SYNOPSIS
The Spanish influenza arrived in the United States at a time when new forms of mass transportation, mass media, mass consumption, and mass warfare had vastly expanded the public places in which communicable diseases could spread. Faced with a deadly “crowd” disease, public health authorities tried to implement social-distancing measures at an unprecedented level of intensity. Recent historical work suggests that the early and sustained imposition of gathering bans, school closures, and other social-distancing measures significantly reduced mortality rates during the 1918–1919 epidemics. This finding makes it all the more important to understand the sources of resistance to such measures, especially since social-distancing measures remain a vital tool in managing the current H1N1 influenza pandemic. To that end, this historical analysis revisits the public health lessons learned during the 1918–1919 pandemic and reflects on their relevance for the present.
The influenza pandemic came to the United States, wrote physician George Price in December 1918, in the guise of both “destroyer and teacher.” Like the Black Death had centuries before, he observed, influenza had many lessons to teach, if only people were wise enough to comprehend them. Among the most important of these lessons were the difficulties inherent in controlling a deadly, fast-moving epidemic in communities knit closely together by mass transportation, mass media, mass consumption, and mass warfare. As Price recognized, the 1918–1919 pandemic represented something profoundly new under the public health sun, so to speak. It was the first global pandemic to occur in the era of “mass society,” as the early 20th- century intellectuals were just beginning to term it. As such, the Spanish influenza offered an object lesson in how quickly a disease that was both deadly and easily communicable could cut through “the masses” in spite of public health efforts to prevent its spread.1
Like Price, most public health authorities who lived through the 1918–1919 pandemic looked back on it as a test that they had failed. Despite having discovered—with considerable fanfare—the microorganisms causing many of humankind's worst afflictions, bacteriologists could not identify the microbial agent of influenza. Despite unprecedented efforts at mass education and coercion designed to halt it, the disease spread with lightning speed. After decades of remarkable progress in controlling communicable diseases, the influenza pandemic raised troubling questions about the efficacy of modern public health methods. Perhaps the most important “lesson” taught by the pandemic was the realization that those measures that worked the best to control a highly infectious disease—bans on public gatherings, school closures, and strict quarantine and isolation—were precisely the ones most difficult to implement in a modern mass society. As an article in the July 5, 1919, Literary Digest summed it up, influenza's spread “... was simple to understand, but difficult to control.”2
Revisiting the “lessons learned” about managing the masses during the 1918–1919 influenza pandemic is well worth doing at the present moment, as global public health authorities attempt to manage a novel H1N1 strain of influenza. Such a retrospective is all the more timely in light of recent work suggesting that the early and sustained imposition of gathering bans, school closures, and other social-distancing measures significantly reduced mortality rates during the 1918–1919 epidemic. Those municipalities that were able to quickly minimize the mixing of people in public spaces lost fewer lives to the Spanish influenza.3,4 These findings provide new incentive to investigate the reasons why some communities accepted the necessity for social-distancing measures and others did not. Why and when did the threat of deadly disease succeed or fail to convince public officials and ordinary citizens to alter their behavior?
With that question at the forefront, this article explores how the influenza pandemic created new awareness of the problems of disease prevention in a mass society connected by new forms of public education, transportation, and amusement. It focuses on public health efforts to modify the behavior of the as-yet uninfected “masses” to create a firewall against the pandemic's spread. More specifically, it explores the implementation of social-distancing measures, such as public gathering bans, and the enforcement of personal hygiene measures such as using masks and handkerchiefs to stem the deadly epidemic.
The narrative that follows is organized into a sequence of “before, during, and after” perspectives. The “before” section surveys the dramatic changes in popular understandings of germ diseases that preceded the pandemic. The “during” section explores how problems controlling the public were understood as a function of modern life and the difficulties they posed for mass education and compliance. The “after” section reflects on the great pandemic in the 1920s, especially in relation to the return of epidemic influenza in 1928–1929. Finally, the epilogue offers some thoughts on the pandemic's lessons about managing the masses in our own times.
BEFORE: INFECTIOUS DISEASE CONTROL IN THE PROGRESSIVE ERA
The Spanish influenza arrived in the United States at a time of growing confidence among public health authorities. The late 19th-century acceptance of the germ theory of disease and subsequent development of bacteriological science had produced several decades of remarkable progress. Between 1870 and 1918, researchers using more sophisticated laboratory methods had isolated the causal microorganisms responsible for many of the most feared communicable diseases of the past, including cholera, typhoid, tuberculosis (TB), syphilis, and bubonic plague. These scientific advances undergirded an expansive public health movement. By the 1910s, the Progressive trend toward stronger government had provided city and state public health departments with an array of laws and regulations to manage outbreaks of infectious diseases. When coercion was deemed necessary, public health departments had the statutory power to isolate the ill and punish public health infractions. When voluntary compliance was sought, public health authorities could draw on substantial experience in securing the public's voluntary compliance with preventive measures.5,6
How much that public health arsenal had expanded by 1918 is evident by a look backward at the previous influenza pandemic in 1889–1890. Newspaper coverage of the 1889–1890 “Russian influenza” reveals the still-vague appreciation of the germ theory of disease as it applied to “the grip”. On December 18, 1889, The New York Times carried a quotation from the Medical Record stating that “.. . the disease is undoubtedly due to some microorganism which floats in the air, and which infects the human system, but is generally killed in so doing, for influenza is but slightly if at all contagious.”7 Although well aware, thanks to an already extensive transoceanic telegraph cable system, that the Russian influenza was headed their way, public health departments did little preventive work in advance of its arrival, and once the disease did appear, left its management to private physicians. The latter simply told sick people to stay at home so as to recover more quickly, and warned the aged and infirm to stay away from the ill. More specific instructions for how to avoid contagion were conspicuously absent, probably because the atmosphere was seen as the chief source of the disease.8
Twenty years later, public health authorities had a clear understanding of influenza as a germ disease, albeit a mysterious one. The laboratory methods used so successfully to identify the bacteria responsible for cholera, TB, and many other diseases did not work with influenza. In 1918, the virus was still a little-known branch of the germ family. Researchers could prove the existence of infective particles far smaller than bacteria but could not yet isolate them nor conclusively show their connection to specific diseases. During and after the pandemic, scientists sought in vain to isolate the “x-germ” that caused it. (See John Eyler's “The State of Science, Microbiology, and Vaccines circa 1918,” p. 27–36 in this issue.) Still, so strong was the acceptance of the germ theory of disease that influenza's microbial identity was accepted without question and aggressive measures were used to contain its spread.
Compared to 1889–1890, public health experts faced the 1918–1919 influenza epidemic with a much greater capacity to teach the rules of disease avoidance and to punish those who failed to observe them through the use of fines and other coercive forms of sanitary policing. In 1918, public health authorities recognized influenza as a respiratory infection spread by coughing, sneezing, and spitting. To minimize its spread, they drew on infection-control methods that had been elaborated and tested for decades, in some cases centuries, including quarantine, isolation, disinfection, ventilation, and personal hygiene designed to limit droplet infection. Although some of the ideas still accepted in this era, such as the dust theory of infection or the role of library books and postage stamps in spreading germs, would later be jettisoned, much of what experts and well-informed laypeople assumed to be true in 1918 we still assume to be true. The particulars have been altered, but the basic mechanisms of how microorganisms migrate from the sick to the well were understood.9
The response to pandemic influenza in 1918 drew on elements of disease control used to manage a wide range of communicable diseases. For fast-moving epidemics, there was long experience in quarantine and isolation. City health departments had the legal power to close schools and quarantine homes when epidemics of diphtheria or polio broke out.10,11 They could screen for and demand special precautions be taken by healthy carriers of typhoid.12 Federal law required the medical inspection and quarantine of ships and immigrants arriving in the big port cities.13 On occasion, city health departments even imposed isolation on specific neighborhoods, as in the 1900 bubonic plague outbreak in San Francisco.14
In addition, influenza management drew heavily on the public health campaign against pulmonary TB, the leading cause of death in 1900. At first glance, it may seem strange that TB served as such an important model for managing an influenza epidemic because the diseases differ so greatly in clinical and epidemiological terms. Yet, from a preventive standpoint, they had some important similarities: both pulmonary TB and influenza were infections of the respiratory tract that spread by direct droplet infection and nose/mouth/hand contamination. Precisely because it was so chronic and so widespread, TB had dominated two decades of laboratory and field experience dedicated to mapping out the wide circulation of germs via coughing, sneezing, and spitting. Its ubiquity helped confirm public health belief in fomite infection (transmission of germs via objects such as drinking glasses or books) and dust infection (transmission of dried germs mixed with common house dust and street dirt).9
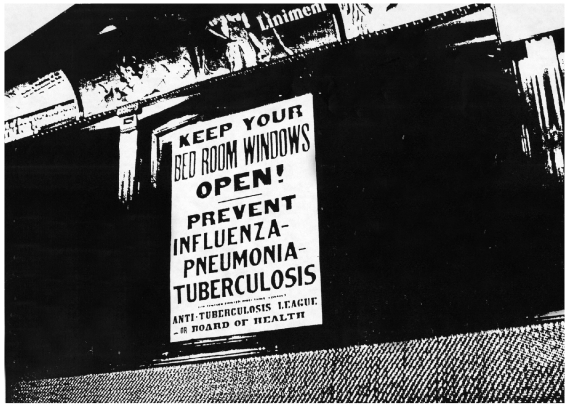
Influenza control also drew on the strong hygienic program popularized by the anti-TB movement at the turn of the century. The first of the modern voluntary health associations, the National Tuberculosis Association (now the American Lung Association) and its state affiliates pioneered the use of modern methods of journalism, advertising, and entertainment to create an effective new style of popular health education. By the eve of the pandemic, the anti-TB crusade had widely publicized the basics of disease transmission and protection against respiratory infections. Laid side by side, the similarities between the standard anti-TB protocol and the anti-influenza measures popularized in the fall of 1918 are strikingly apparent: keep windows open to dilute germs in the air; protect others against one's coughs, sneezes, and spitting; avoid sharing utensils; stay rested and eat nutritious food; and avoid worry and overwork. What worked against TB should work against influenza, or so it was assumed.9
But by 1918, public health experts had already begun to see the difficulties of controlling TB in a “modern” society. Identification and isolation of the ill worked most effectively to stop the chain of TB infection, yet states balked at the expense of building sufficient sanatoria to hold them, and people with TB (understandably) resisted being removed from family and friends. Many consumptives simply could not afford to go for the cure and, hence, continued to live at home and attempt to work, forming an infective risk to those around them. Since “careless consumptives” were presumably everywhere, it became all the more important that everyone practice careful sneezing, coughing, and spitting behaviors. But sanitary disposal of mouth and nose secretions and antiseptic hand washing were not easy tasks in an era before Kleenex®, Dixie® cups, and hand sanitizers.9,15
Although these problems were evident by 1918, so too was the downward trend in TB mortality. Public health authorities had good reason to believe that they were defeating the white plague by getting as many acute cases into isolation as possible, encouraging those who remained at home to be “careful consumptives,” training “the masses” in the rules of good nose/mouth/hand hygiene, and working to elevate living conditions more generally. Despite their imperfect execution, sanitarium treatment and rigorous sanitary policing of the hand/mouth/nose connection seemed to be making a positive difference. In the absence of a reliable cure for TB (which would not be found until the late 1940s), there was every reason to continue to promote these measures.
DURING: THE PROBLEM OF THE CROWD DISEASE
With the luxury of hindsight, it is easy to understand why the public health strategies adopted in 1918 failed. As George A. Soper noted in a 1919 article titled “The Lessons of the Pandemic,” authorities thought “.. . the influenza could be stopped by the employment of methods which it was assumed would stop the other respiratory diseases.” In reality, “this double assumption proved to be a weak reed to lean upon.” Throughout the epidemic, public health authorities found themselves having to explain why the standard “lessons” of disease control were not working to contain the Spanish influenza.16
Due to a vastly expanded mass-media network, this questioning process got played out in a very public way. In the preceding two decades, new forms of communication, print technology, and advertising practice had given rise to a highly competitive news industry that greatly expanded the scope of what was considered “fit to print.” By World War I, newspaper reading in the United States had reached an all-time high.17 Editors had already learned from previous events, such as the rabies vaccine's introduction in 188518 and the cholera pandemic of 1892–1893, that disease stories sold papers.13 In this media-rich context, coverage of the 1918–1919 epidemic unfolded with an unprecedented degree of speed and detail, making the Spanish influenza a truly mass-mediated pandemic. As Edwin O. Jordan remarked in 1927, “Rarely if ever before in the annals of medicine has a manifestation of epidemic disease been studied by numerous observers with so much ardor and reported with so much fullness as was the epidemic. .. of 1918.”19
To be sure, influenza's importance was magnified by its association with the Great War, an event that still dominated the front pages. Yet even as a secondary issue, the pandemic earned an extraordinary amount of newspaper coverage. For months between the spring of 1918 and the winter of 1919, readers were provided a detailed commentary on the unfolding epidemic, including discussions about the nature of the disease, the best methods of containing it, and the growing frustration over managing it. Specialized newspapers such as Variety, a weekly devoted to the entertainment industry, carried extensive coverage of the pandemic. Monthly periodicals and magazines offered additional stories, albeit at a slower rate due to their less frequent publication.
Price's December 1918 article in the Survey, perhaps the most influential social science journal of this era, was a case in point. Writing for a presumably more educated audience, he made no effort to sugarcoat his observations. Despite the great advances of bacteriology, “.. . we are in the dark as to the invisible germ causing the disease,” he wrote, and “.. . might as well admit it and call it the ‘x' germ for want of a better name.” While the exact identity of the x germ was unclear, experts agreed that influenza was “.. . a hand-to-mouth infection which travels by direct contact from person to person. .. spread by droplets diffused by sneezing and coughing.” Hence, the best way to interrupt the chain of infection was to isolate flu victims, or as a Massachusetts physician expressed it more colorfully, “.. . put each diseased person in a diver's suit and provide him with a pair of handcuffs.”1 But what E.O. Jordan later referred to as “perfect” isolation proved no easier to implement in the face of influenza than it had been for either polio or pulmonary TB.19
To explain what made influenza so hard to control, public health commentators found the concept of a “crowd disease” increasingly useful. Of course, the idea that cities, crowding, and epidemics went together was by no means new in the early 1900s; for centuries, observers had noted that where many people packed in together, diseases often followed. Yet in size and complexity, the new industrial cities of the early 20th century posed an extreme challenge. The scale and scope of public gathering places increased dramatically between 1890 and 1918. The second industrial revolution directly or indirectly led to a vastly expanded public school system, huge factories and office buildings, extensive public entertainments (amusement parks, nickelodeons, dance halls), and, last but not least, mass transportation systems that connected all these elements together. By the early 1900s, the interlinking of public spaces created a vast highway along which the deadly germs could quickly travel.6
The influenza pandemic underlined the difficulty of policing those public spaces. Influenza was a “crowd disease” as opposed to a “house disease” (an illness rooted in defective household plumbing or careless housekeeping).20 Although the term “crowd disease” did not become a familiar part of the public health lexicon until publication of Major Greenwood's Epidemics and Crowd Diseases in 1935,21 commentators routinely marked the association between population density and influenza's spread.22 From its outset, the pandemic was linked with crowded places, from troop ships to movie theaters. Although isolation of the sick was essential, quarantine measures had to be accompanied by broader measures aimed at regulating the congestion of public spaces.
The influenza pandemic heightened a contrast between the safe home and the dangerous public space that had already become a familiar theme in the late 19th century. The anti-TB movement had long warned that one could have the most sanitary home imaginable and still incur mortal danger by virtue of taking the subway or going to a movie where “careless consumptives” might have left their germs behind. The emphasis on exacting individual precautions concerning coughs, sneezes, and spitting reflected the belief that modern health citizenship required eternal vigilance about such behaviors when in public places.9
Social-distancing measures
While few of the individual measures deployed during the influenza pandemic were entirely new to public health practice, the scale and scope of their enactment was without precedent. Tactics formerly focused on specific groups, such as children or immigrants, were expanded to cover the entire urban population. Instead of closing schools and banning children from theaters, as had been done in epidemics from the late 1800s through the 1916 polio epidemic, state and local boards of health now enacted bans on public gatherings for all age groups. Cities across the country contemplated sweeping measures. In Seattle, Variety reported, it was the “first time this city has ever been closed tight,” while in Pennsylvania the epidemic prompted “the most drastic health order ever issued in this commonwealth.”23
In the face of a deadly crowd disease, municipal authorities had difficult choices to make. They could impose city-wide bans on public gatherings, which typically included closing schools, saloons, theaters, and more rarely stores. A less drastic approach allowed public places to stay open but required additional preventive measures, such as staggered opening times, strict observance of sanitation rules, and mask wearing. Many factors played into the path a particular city followed, not the least of them timing. In the two principal cities where influenza first broke out, Boston and Philadelphia, the illness and death rates rose so steeply and quickly that the municipal authorities felt they had no choice but to impose sweeping public-gathering bans. Yet their decision to close schools, theaters, and other gathering places came too late to prevent the wide spread of the disease. The leaders of other cities, blessed with a little more time to prepare, had to decide what strategies to adopt.24
By 1918, the United States had 10 cities with more than a half million in population, the largest of which was New York City, with five and a half million residents. Implementing social-distancing measures in these big cities presented a massive public health challenge. They had complex economies dependent on both industry and commerce that could easily be damaged by quarantines and closures. As had happened in earlier epidemics, businessmen resisted the idea of mass closures of transportation and businesses that would cause economic distress both to owners and workers.25 (At least one employee filed a lawsuit to recover lost wages due to such a closure.) Big cities also had large public school systems, flourishing commercial entertainment districts, and extensive systems of mass transit, all of which formed fertile ground for the spread of influenza. Closing schools left parents with children to provide for during the day. Shutting down saloons and theaters meant not only lost revenue for owners but also lost pleasures for their customers. To inflict such economic damage on a city's economy required a public health emergency without precedent.24
New York City represented a particularly formidable public health challenge, due to its size and economic importance. The newly appointed Health Commissioner, Royal Copeland, decided not to impose a full-scale public-gathering ban. Instead, he urged businesses and theaters to stagger their opening and closing times so that the crowds in streets and on subway lines would be minimized. He had influenza and pneumonia added to the list of reportable diseases so that private physicians had to notify the department of health of their cases. (Copeland, who was a homeopath, became especially exasperated by the behavior of the city's physicians and druggists.) He demanded and got more rigorous inspection of schoolchildren to allow early detection of the sick. Finally, he concentrated on expanding hospital beds and recruiting skilled nurses for home care of influenza victims.24,26
Concern about panicking a large urban population shaped Copeland's strategy in New York. As The New York Times reported in a November 1918 article titled “Epidemic Lessons Against Next Time,” Copeland explained that “my aim was to prevent panic, hysteria, mental disturbance, and thus to protect the public from the condition of mind that in itself predisposes to physical ills.”27 Physicians in other cities sounded a similar note. For example, at a meeting of the Detroit medical association, speakers suggested that “.. . a lot of people are being affected more by fright than by Spanish Influenza.” Doctors' offices were filled with people “.. . afflicted with nothing more than a slight cold and a great fright.” At the same meeting, Detroit Health Commissioner J.W. Inches expressed his belief that it was unnecessary for the governor to ban all public gatherings and reassured the public that the situation was well in hand.28
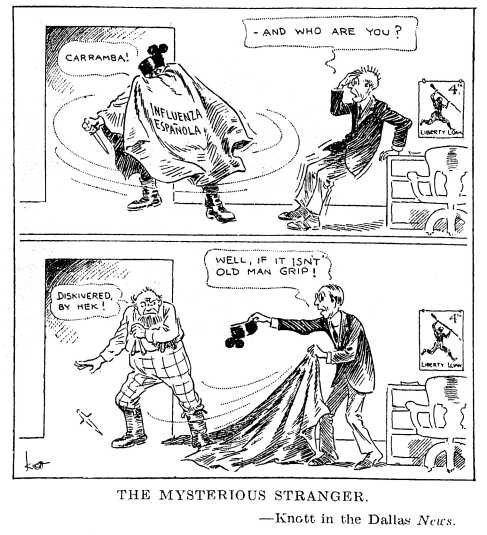
Copeland's reluctance to impose more sweeping closures of schools and businesses reflected the awareness that identifying those in need of quarantine was no easy matter. In its very earliest stages, the symptoms of the deadly flu could mimic those of the milder strain of influenza and even the common cold. Moreover, those familiar with the publicity surrounding the famous Typhoid Mary knew that some diseases could be spread by healthy carriers.12 The impracticality of sending everyone with symptoms of a head cold into quarantine seemed obvious. The Literary Digest for October 12, 1918, carried a cartoon from the Dallas News that suggested the uncertainty surrounding the degree of threat posed by influenza (Figure 1). In the first frame, the “Influenza Espanola” appeared as a caped stranger, carrying a knife, before which an older man quakes in fear. But in the second frame, the quaking man has found the courage to remove the stranger's cape and hat, and discovers “old man grip,” a far less menacing character.29
Figure 1.
“The Mysterious Stranger”: a cartoon in the Dallas News during the 1918–1919 influenza pandemic
Source: How to fight Spanish influenza. Literary Digest 1918 Oct 12;59:13. The cartoon is attributed to Knott of the Dallas News.
Thus, while some public health authorities worried that the public was insufficiently impressed by the influenza threat, others warned against the dangers of overreacting. References to “panic” and “hysteria” reinforced a longstanding tendency to identify crowds and masses with delusional thinking and dangerous behavior.30 Faced with a city full of very nervous people, it made sense to urge them to stay calm and not interpret every cold symptom as incipient influenza. Yet this “don't panic” message surely contributed to public confusion about exactly how scared people should be.
Unlike New York City, many cities did pass more sweeping public-gathering bans for at least a short period during the 1918–1919 pandemic.24 While in retrospect it may seem obvious that these bans were both necessary and justified, they met with considerable opposition. Significantly, as Alan Kraut's article in this issue shows (See “Immigration, Ethnicity, and the Pandemic,” p. 123–33, in this issue), this resistance did not come from specific ethnic or racial groups being made scapegoats for the outbreak, as had happened in previous epidemics. The Spanish influenza moved so quickly and so indiscriminately among the population that it could not easily be blamed on immigrants or the poor.31 Instead, the divisions revealed by the pandemic were of a different sort; the lines of resistance reflected divisions both within the public health community and between the public health departments and the communities they served.
One fault line emerged within the public health movement. In the previous 30 years, both local and state boards of public health had gained enormous authority. The influenza pandemic quickly revealed the limits of their coordination and cooperation. City health boards complained that state boards, which were often dominated by small town and rural representatives, did not recognize the peculiar problems of urban public health. In Pennsylvania, Indiana, and Illinois, the state boards of health imposed strict public-gathering bans that local departments opposed and even circumvented. For example, Chicago's Health Commissioner, John Robertson Dill, initially allowed the city's theaters to stay open on the condition that they maintained good ventilation systems. But in what Variety described as a victory for the “downstate villagers,” Illinois authorities issued a state-wide closure order that included theaters.32
Public-gathering bans also exposed tensions about what constituted essential vs. unessential activities. Those forced to close their facilities complained about those allowed to stay open. For example, in New Orleans, municipal public health authorities closed churches but not stores, prompting a protest from one of the city's Roman Catholic priests. If churches had to be closed, Father Bandeaux argued, then the “.. . big business establishments, which are crowded from early morning until closing hours in the evening, [should] be also required to close.” Because the board of health was doing such a poor job of stopping the disease's spread, the priest suggested, people had all the more reason to go to church to ask for divine help. Finally, he pointed out that in all the yellow fever epidemics that New Orleans endured, this was the first time its churches had been closed.33
Theater owners often voiced the “why us and not them” argument. In many cities they were the first, and sometimes the only, businesses to be shut down. By mid October, Variety reported that more than 90% of American theaters, including motion picture houses as well as live performances, were on “the dark list.” Theater owners faced a difficult problem: they did not want to appear irresponsible in the face of a public health emergency, yet they resented being singled out for closures. In Providence, theaters were closed while “.. . saloons [were] wide open.” In Philadelphia, theater owners “.. . smarted under the injustice” that department stores and restaurants could open whereas they could not. In St. Louis, “.. . a delegation of 15 theatrical and picture” men called on the mayor “.. . objecting to the epidemic's closing order” issued by the health board and “.. . asked that the order be extended to department stores, 10-cent stores, elevated and street cars.” Trying to emulate what had been done in New York City, the managers “.. . offered to provide posters advertising the dangers and methods of combating the epidemic and to give full aid in publishing health department propaganda on the screens when reopening.” But the mayor did not relent, and the theaters lost an estimated $150,000 a week.23
The pandemic revealed how economically important public amusements had become to local economies. Variety estimated that theater owners lost close to $50 million during the influenza pandemic. Vowing to lift his statewide theater ban as soon as public safety allowed, Benjamin Franklin Royer, Pennsylvania's state health commissioner, remarked, “Nobody knows better than I do the material loss in dollars and cents of such an order.”23 The influenza pandemic also exposed the growing psychological and emotional dependence on public amusements. As an editorial about theater closings in the Boston Evening Record noted, “Dwellers in big cities are deprived of the social life that comes from living in smaller communities.” For “Mr. Bigcitizen,” the theater, motion picture house, and concert hall had taken up that function.34 Public health authorities often expressed their reluctance to impose theater bans because of the intense attachment that modern urban dwellers had to their amusements. As the Philadelphia health commissioner stated, he was “a firm believer in amusement.”35
Personal hygiene measures
Even in cities that passed sweeping bans on public gatherings, people could not live in total isolation. Due to the necessity of working and eating, most urban residents had to venture out of their homes into the germ-ridden realm of public spaces. Hence, it was critical that health authorities remind individuals about the rules of safe coughing, sneezing, and spitting and to encourage business establishments to do their part to minimize the spread of infection.
At the time of the 1918–1919 pandemic, all large American cities had sanitary regulations in place to control other diseases, in particular TB. These regulations could be, and often were, adapted to influenza control. These regulations included bans on public spitting and the use of the common cup, requirements for cleaning and disinfecting public spaces, and regulations governing sanitary food service. During the influenza epidemic, cities increased their enforcement of sanitary laws that had not been vigorously enforced in the past. For example, as the epidemic spread in Philadelphia in late September, 25 men were arrested for spitting.36 A New York City magistrate sentenced 14 men reported by the sanitary inspectors for using dirty glasses in their establishments, scolding them, “Don't you men know that the Board of Health is trying to prevent deaths from Spanish influenza, which is spread by uncleanliness?”37 In New Orleans, public health officials harried proprietors of ice cream shops as part of their toughening stance against sanitary infractions.24
Greater enforcement of existing anti-spitting laws and vigilance among individuals and businesses were frequently associated with the relaxation of public-gathering bans. Copeland made this tradeoff clear in his handling of the New York City epidemic. Mass transit could not be closed down, he argued, because “.. . you might as well try to cut off the main artery of the body as to close the subway.”26 But trolley cars and subways could be made safer by warning riders to be careful and setting police to catch the careless (Figure 2). When Copeland met on September 18 with representatives from New York City street car companies, theaters, and movie houses, he found them more than eager to help publicize influenza-control measures as a way to head off potentially profit-killing closures. At Copeland's suggestion, the railroad companies “.. . offered to co-operate in placing prominent posters and other forms of advertising cards in cars requesting that all persons feeling a tendency to sneeze, cough, or expectorate, do so with a handkerchief close to their mouths.” Theater owners agreed to print the same rule in their programs, and to have ushers “.. . keep a careful watch on theatre patrons” and “.. . ask persons who do not heed this rule to depart from the house.” Motion picture operators offered to show slides with the health rules before and after the feature film and to enforce them. Patrons were also instructed to wash their hands after coming in contact with anyone coughing or sneezing in public. By following these “simple” rules, an article on Copeland's meeting reported, “a large part of the danger of infecting the atmosphere with influenza germs will be obviated.”38 Another New York Times article quoted Copeland's statement that “.. . if every one observes this warning the disease will not become epidemic.”39
Figure 2.
Trolley car poster, Cincinnati, Ohio, 1918
Source: Center for Photographic Images of Medicine and Health Care, Media Services, Health Sciences Center, Stony Brook University, Stony Brook, New York.
In retrospect, some of the preventive measures practiced during the pandemic seem painfully ineffective. For example, so strong was the belief in the infective power of street dust and dirt that cities all over the country, including Los Angeles, Philadelphia, Fall River, Indianapolis, and Nashville, invested considerable time and money in daily street washing.24 In Boston, draft boards required special precautions to prevent the spread of “grippe germs” on the paper questionnaires submitted by registrants.40
In contrast, the efforts to police coughing, sneezing, and spitting are much more in line with modern influenza-control practices. As of 1918, anti-spitting laws had been in force for at least a decade; they simply needed to be enforced. Coughing and sneezing were a different story: although the anti-TB movement had long cited these behaviors as potentially dangerous, there were no existing laws against coughing or sneezing. The influenza epidemic greatly heightened anxiety about these common behaviors. As the Boston commissioner of health put it, it was wise “.. . to keep out of spray range” to avoid infection.41 Putting the onus on individual sneezers, spitters, and coughers also worked to supplement or in some cases forestall more sweeping measures such as closing schools, businesses, and theaters. Theater owners in New York and Indianapolis, for example, took the initiative by having ushers ask coughing patrons to leave the premises.38,42
The use of gauze masks offered one solution to the droplet infection threat.19 While common in hospital operating rooms by World War I, mask wearing by lay people was among the most novel public health practices introduced in the 1918 pandemic. Public health authorities promoted mask use as a measure that would allow cities to function while minimizing the spread of influenza. When cities lifted public-gathering bans, they often did so with the proviso that people wear masks when attending theaters. Mask wearing gained considerable popularity as an emblem of public spiritedness and discipline. Newspapers carried instructions on how to make and launder them; women volunteers already accustomed to rolling bandages and knitting socks for the soldiers added making gauze masks to their list of good deeds. Fashionable women made theirs of chiffon, while volunteer health workers donned them when venturing into homes to carry educational information about the epidemic.24,43
Still, gauze masks had their detractors within the public health community. One notable critic was the Detroit health commissioner, Dr. J.W. Inches, who declared “.. . these masks are worthless.” They were so porous that not only “.. . a mosquito could jump through them,” he remarked, but, “I have sprinkled granulated sugar through them,” telling proof that a microbe could get through the mask's defenses. Inches thought masks might have some utility for doctors and nurses treating flu victims, but for the ordinary citizen, the use of an ordinary paper napkin that could be destroyed after each use was far more advisable. (Dr. Inches was ahead of his time, anticipating the rise of disposable paper handkerchiefs in the 1920s.)28,44
During the pandemic, another, more common alternative, namely the cloth handkerchief, came to fill a similar function. Although the gauze mask received the greater degree of publicity, the handkerchief got an equally big boost from public health authorities. Starting in September 1918, public health officials urged the public to use their hankies as cloth shields when coughing or sneezing. This message appeared in the first influenza precautions issued by Surgeon General Rupert Blue and was repeated by local health departments throughout the remainder of the epidemic.45 The City of Chicago even passed a law making people who coughed or sneezed without using a handkerchief liable to arrest.46 Likely one big reason for the emphasis on handkerchief use was its ease of practice. Compared with gauze masks, which were expensive to buy and uncomfortable to wear, the cheap, easily washed handkerchief was a good substitute. But for very poor Americans, even a handkerchief, much less a frequently washed one, represented a luxury.
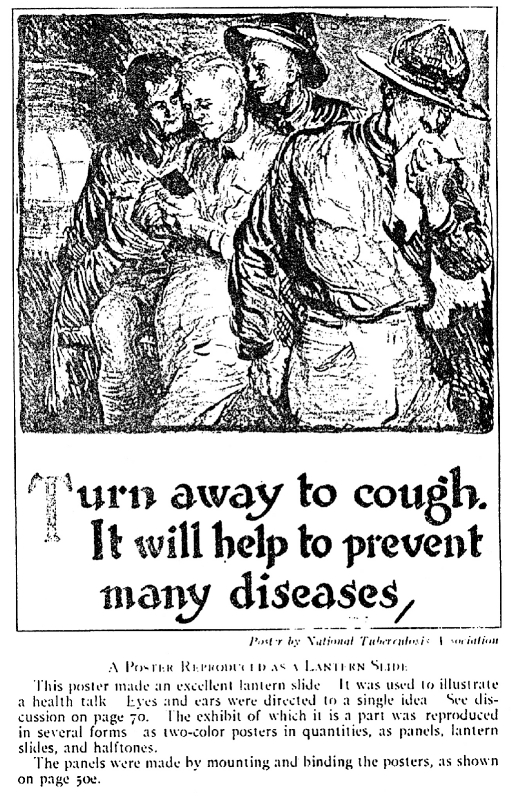
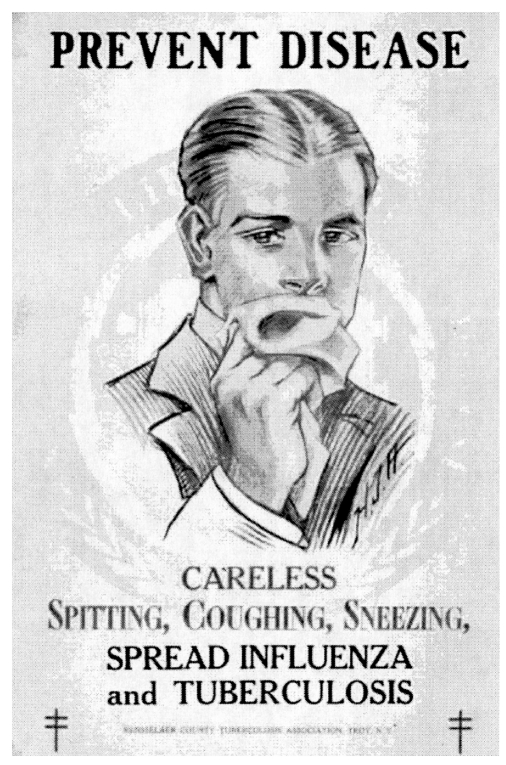
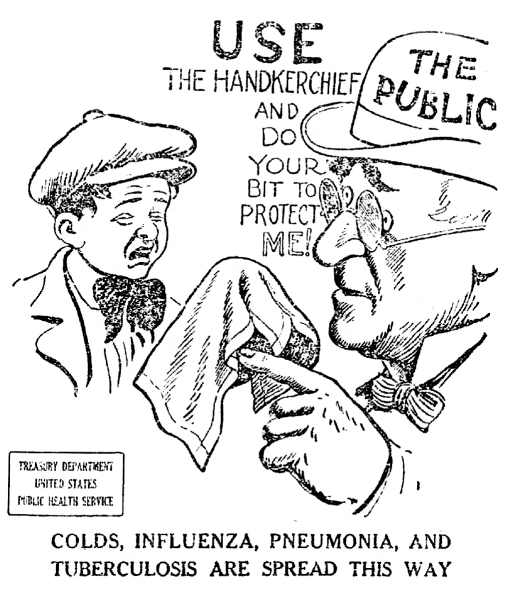
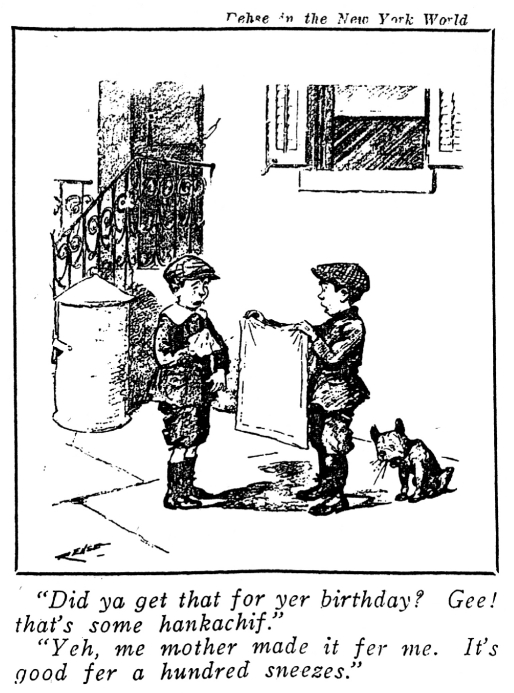
Although women as well as men made up the Progressive-era “masses,” the public health villains blamed for careless coughing, spitting, and sneezing during the influenza pandemic were frequently represented, at least visually, as men behaving badly. The posters, cartoons, and advertisements promoting handkerchief use during the pandemic featured only boys and men. For example, the National Tuberculosis Association distributed a poster showing a soldier considerately turning away from his comrades to cough into his handkerchief and thus protecting them against infection (Figure 3). A civilian version of the same concept showed a handsome young man, nicely dressed, hair well groomed, also using his handkerchief, with the same warning about spreading disease through careless habits (Figure 4). A U.S. Public Health Service poster featured a cartoon showing an older man labeled “the public” thrusting a hankie at a sneezing boy, asking that he “do your bit to protect me!” (Figure 5). In a lighter-hearted vein, a cartoon accompanying an article on “Spanish Influenza and Its Control” in the Survey for October 12, 1918 (Figure 6), showed a boy showing off the handkerchief “good fer a hundred sneezes” that he had received as a birthday present from his mother.
Figure 3.
Poster distributed by National Tuberculosis Association, 1918
Source: Reproduced in: Routzahn E, Routzahn MS. The ABCs of exhibit planning. New York: Russell Sage Foundation; 1916. p. 68b.
Figure 4.
Poster distributed by Rennsselaer County Tuberculosis Association, Troy, New York, 1918
Source: National Library of Medicine. Images from the history of medicine cited 2010 Feb 24]. Available from: URL: http://ihm.nlm.nih.gov/luna/servlet/detail/NLMNLM˜1˜1˜101449540˜157889:Prevent-disease?qvq=q:influenza;lc:NLMNLM˜1˜1&mi=55&trs=59
Figure 5.
Poster distributed by U.S. Public Health Service, 1918
Source: Public Health Service (US) [cited 2010 Feb 24]. Available from: URL: http://1918.pandemicflu.gov/pics/cartoons/Cartoon_from_1918.jpg
Figure 6.
Cartoon attributed to George Rehse of the New York World
Source: Reprinted in: Spanish influenza and its control. Survey 1918 Oct 12;41:45.
Perhaps the masculine slant of public health circulars reflected the wartime context of the pandemic. Influenza was a military problem first and a civilian problem second. As one 1918 commentary put it, wartime was associated with “unsanitary herding of men” that frequently gave rise to epidemics.47 In this still somewhat prudish era, there may have been unspoken conventions about what bodily functions could be represented in pictorial form; showing women sneezing might have been considered “indelicate.”
Perhaps, too, the pandemic gave public health leaders an opportunity to advance a more manly style of health education. As evident in the writings of Charles Chapin and H.W. Hill, some in the public health field felt that older forms of public outreach were too old-fashioned to reach the modern men and boys who now posed a special weakness in the chain of infection control.48,49 The influenza pandemic offered a teaching moment in which masculine resistance to hygiene rules associated with mothers, school marms, and Sunday school teachers could be replaced with a more modern, manly form of public health, steeped in discipline, patriotism, and personal responsibility.50
Public health authorities pushed personal hygiene measures such as masks and handkerchiefs in spite of questions about their effectiveness as disease-control measures. Herein lays the irony of public health education during the pandemic: pushing the “gospel of germs” was not likely to stop the epidemic, but it had to be done. George Soper summed up this position beautifully in his 1919 Lessons of the Pandemic: “.. . if doubt arises as to the probable efficacy of measures which seem so lacking in specificity it must be remembered that it is better for the public morale to be doing something than nothing and the general health will not suffer for the additional care which is given it.” To do otherwise would constitute an unacceptable passivity in the face of a deadly disease.16
AFTER: LESSONS LEARNED IN DEFEAT
The 1918–1919 influenza pandemic taught public health experts a complex and contradictory set of lessons. On the positive side, the pandemic seems to have diminished the appeal of atmospheric theories of infection. Although some commentators continued to mention weather conditions as a variable in the disease's spread, the Spanish influenza confirmed the importance of droplet and contact infection. As William Osler was credited with observing, the flu never traveled faster than modern transportation, confirming that it was human bodies and not some ethereal atmospheric force that spread it.45 Natural experiments, such as the flu's introduction into San Quentin prison, enabled a clearer understanding of the contingent nature of infection; at the prison, the peaks of the illness followed nights that the inmates had gathered to watch a movie (and likely without benefit of handkerchiefs).19
Even though post-war experimental efforts to spread it failed, public health experts still had no doubt that the influenza spread by a combination of droplet infection and mouth/nose/hand contamination. Yet they also learned from the 1918–1919 pandemic that it was exceedingly difficult to get an urban population to stay at home. People needed to work so they could eat; parents wanted their children to go to school; businesses dependent on customers, whether department stores or movie theater operators, did not want to close down. Hence, the most practical strategy was not unlike that arrived at for TB control: move quickly to isolate the acutely ill in hospital wards or at home, under the care of professional nurses or Red Cross-trained volunteers well schooled in infection control; and direct an intensive public education effort about personal hygiene to everyone else.
In the years immediately following the pandemic, commentators would continue to reflect on the difficulty of controlling the urban “masses” during a public health emergency. In 1922, a Survey article quoted the English newspaper the Guardian, expressing this sense of futility in relation to influenza: “But of what use is it to advise a modern urban population to avoid traveling on trains or trams, to ask the rising generation to abandon the pictures, or to warn the unemployed to take plenty of nourishing good and avoid worry?”51 Nor was it easy to get the public to practice the rules of modern nose/mouth/hand hygiene. Even at the height of the pandemic, people who should have known better broke the rules. For example, in San Francisco the mayor let his face mask dangle while watching the Armistice Day Parade, and the Commissioner of Health was fined for not wearing his mask at a boxing match.24 Nor did post-pandemic behavior seem any more careful. Anticipating what would become a perennial lament, Dr. Ennion Williams noted in a 1927 address to a group of nurses that health-care professionals set the public a bad example, citing the case of a TB expert with a head cold who coughed into his hand (where was his handkerchief?) while reading a paper at the National Tuberculosis Association's annual meeting.52
In a 1925 article in the American Journal of Public Health, one of several retrospective essays on the 1918–1919 outbreak, Edwin O. Jordan summed up the “.. . simple to understand, but difficult to control” theme so frequently sounded in retrospective accounts of the pandemic. “This is incomparably the worst catastrophe of the sort that has visited the human race since the Black Death of the Middle Ages,” he wrote, and therefore it was important that experts study it carefully. “Perhaps the most demonstrably useful methods of protection are certain forms of quarantine and isolation,” but, he added, “.. . under conditions of modern life these are not readily applicable.” Yet Jordan concluded, “Difficult to apply and uncertain of success as it may be, the minimizing of contact seems at present to offer the best chance we have of controlling the ravages of influenza.”53
The public health response to the next wave of pandemic influenza, which came in 1928–1929, confirmed those lessons. Although nowhere as frightening in its virulence as the previous pandemic, the 1928 outbreak gave public health authorities a chance to demonstrate the ability of strict quarantine and isolation to contain its spread. One important testing ground was American colleges: by the 1920s, college health programs were fast emerging as demonstration stations for more enlightened health approaches.54 In this regard, the quick action by colleges and universities in 1928 to isolate flu sufferers was widely cited as proof of isolation's virtues. For example, by acting quickly, college authorities at the University of Oregon limited the spread of influenza to less than 15% of the student body.55
This odd combination of futility and certainty would continue to characterize summaries of the “lessons learned” from the great pandemic. Writing in the American Journal of Public Health in 1930, after the 1928–29 influenza season had passed without catastrophe, Jordan observed again that “.. . in the field of prevention little real progress has been made.” He continued, “It seems justifiable to increase the emphasis already placed on the influenza patient as a definite focus of infection and to adopt reasonable measures to reduce crowding and direct contact to a minimum during a period of epidemic prevalence.” In future epidemics, this “.. . stricter isolation of influenza patients will probably some day be put into effect,” he suggested, referring to the Oregon case as an example. Jordan concluded with advice that could well have been lifted from a 1915 anti-TB circular: “The opportunities for self protection by individuals lie along the same line: avoidance of crowds and of direct contact with influenza patients and with all people suffering from colds; rigorous abstention from the use of common drinking glasses, common towels and the like; and scrupulous hand washing before eating. While measures of personal hygiene designed to promote physical vigor and well-being are assuredly not to be decried, it is not clear that such measures are efficacious in preventing influenza infection during an epidemic period.”55
Here again was the irony of public health commentaries on the pandemic: few believed that practicing the gospel of germs had worked to control the outbreak, yet they continued to promote its value. In the aftermath of the 1918 pandemic, interwar health educators and commercial advertisers embraced the gospel of germs with great enthusiasm. Post-1919, public schools passed on the techniques of safe coughing and sneezing to children born after the epidemic. In the graded health curriculums introduced in the 1920s, the use of the hankie was first introduced in kindergarten, and elementary schoolchildren learned different versions of the “handkerchief drill,” in which they sneezed into their hankies with military-style precision.
Also in the interwar period, boys and men continued to be seen as weak links in hygienic discipline. Consider, for example, a health talk published by Cincinnati's health commissioner in 1927, titled the “Story of a ‘Common Cold.'” Its main character was a boy named Willie, running amuck in his neighborhood without a handkerchief, indulged by an ignorant mother, and guilty of spreading pneumonia to Mrs. Smith's baby.56 Twenty years later, the 1949 film The Handkerchief Drill treated the same subject with a blend of comedy and contempt, portraying a recalcitrant man whose wife finally left him because he was such a careless sneezer.57
With even greater zeal, interwar advertisers carried on the work of promoting personal hygiene by invoking the fear of influenza. Timed to run during cold and flu season, advertising promotions of mouthwash, cough drops, and tonics reminded their readers that “a cold may be something far more dangerous.”58 For example, the 1929 ads for Listerine® alerted readers to the dangers of “street car colds,” using illustrations of men sneezing while using public transportation.59 When in the late 1920s, consumers began to use paper tissues—originally marketed to remove cold cream—as disposable handkerchiefs, advertisers quickly began to promote this usage of the product. Ads for disposable tissues in the 1940s and 1950s featured mothers training their sons to manage their “man sized sneezes.”60
While the pandemic helped entrench some habits in the repertoire of health educators and advertisers, it spelled the end of other aspects of late 19th-century disease control, such as the focus on “house diseases.” The Spanish influenza showed the inadequacy of untrained nursing in the face of a deadly epidemic. The average homemaker would no longer be trained to minimize the spread of infection by hanging sheets soaked with disinfectant around her loved one's sickbeds. Instead, women were encouraged to learn the early warning signs of contagious disease so as to get their families quickly under a physician's expert care. In addition, they served the cause of public health by reinforcing the lessons of careful coughing and sneezing with husbands and children.9,61
EPILOGUE
Even now, nearly 100 years later, the image of the influenza pandemic as “destroyer and teacher” remains a compelling one. For all the greater knowledge we now possess about its genetic makeup and natural history, the influenza virus still retains the capacity to remind us how difficult disease prevention and control remain in modern societies. Do we have any better chance of controlling a “crowd disease” such as influenza in the early 21st century, compared to 1919?
In some important ways, the answer is probably yes. To begin with, we have a new line of defense that was missing in 1918–1919, in the form of antivirals such as Tamiflu® and the capacity to produce effective flu vaccines. These measures play an essential role in the modern approach to influenza pandemics. Yet they have their limitations: stockpiles of Tamiflu can be quickly used up by physicians seeking to calm panicky patients, and the manufacture of flu vaccine depends on a complicated and in some ways antiquated system of production. Thus, the discovery of flu wonder drugs and vaccines has by no means diminished the need for nonpharmaceutical interventions. As the Centers for Disease Control and Prevention guidelines for pandemic control make evident, they have an essential role to play in slowing down influenza's spread long enough for these measures to be perfected and distributed.62
It may also be easier for people to understand the rationale for social-distancing measures now than it was in 1918. First, the proliferation of fictional and journalistic portrayals of killer epidemics has created a popular apprehension of pandemics in general and influenza in particular that did not exist in 1918. Inventive film makers and novelists have spun dramatic scenarios, some entirely hypothetical, some loosely based on real diseases, about the dangers of rapidly spreading plagues. Books and films, among them Michael Crichton's Andromeda Strain, Stephen King's The Stand, Richard Preston's The Hot Zone, Terry Giliam's Twelve Monkeys, and Francis Lawrence's I Am Legend, to name only a few, have taught successive generations of movie and TV watchers to fear the microbe. Real-life pandemics, including HIV/AIDS and SARS, have taught their own lessons about the difficulties of disease prevention in modern mass societies. Along with climate change, pandemic disease has become part of an apocalyptic set of worries far beyond what E. O. Jordan's generation could have imagined.63
Yet despite our renewed fear of the germ, the implementation of social-distancing measures still faces many challenges today. Public-gathering bans, school closures, and transportation restrictions are difficult to enforce for the same reasons they encountered resistance in 1918–1919. Nor are we any more likely than our World War I forbears to be able to sustain an exacting hygiene of nose/mouth/hand prevention. Consider, for example, the many studies that show the difficulties of getting health-care professionals to practice proper hand-washing protocols, a problem that has helped make hospital-based infections such as methicillin-resistant staphylococcus aureas so common. Like the mayor who let his face mask dangle and the TB expert who coughed into his hand, even people who should know better forget to be careful. Health-care professionals still have to be reminded to wash their hands frequently.64 Studies have also found that men tend to be more careless about hygiene protocols than women, suggesting that the man/boy problem has yet to be solved.65
Perhaps fortunately for us, the resources of late modern industrial culture will conceivably make it easier for us to tolerate staying sequestered at home at least on a short-term basis. Compared to troop ships and railroads, air travel is easier to regulate from a public health perspective, especially since the terrorist precautions enacted in 2001. With the expansion of the modern welfare state, local and state governments can order employees to stay at home and assure them they will be paid. Businesses serving health-conscious customers may be slightly more willing to conform to public health directives. Our capacities to stockpile food and entertain ourselves at home with cable television, computer games, and the Internet (so long as the electricity holds out) have grown enormously since 1918. We have become far more familiar with sneezing into tissues and wearing face masks while mowing the lawn or using aerosol sprays.
Still, should pandemic influenza return in its guise as “destroyer and teacher” we would no doubt have many humbling lessons to learn. Nearly 100 years after the great pandemic, we have no program of national health insurance. Enormous racial and class disparities in health status and access to health care persist. Despite a far greater degree of scientific sophistication, we have been unable to stop the spread of HIV/AIDs, which has generated its own bitter lessons. We still have many reasons to study the great influenza pandemic. To conclude with George Soper's still-relevant observation from 1919: “.. . This may all seem very discouraging but it need not depress anybody. .. To rightly measure a difficulty is often the first step toward overcoming it.”16
REFERENCES
- 1.Price GM. Influenza-destroyer and teacher: a general confession by the public health authorities. Survey. 1918;41:367–9. [Google Scholar]
- 2.How infection travels. Literary Digest. 1919;62:88–91. [Google Scholar]
- 3.Markel HM, Lipman HB, Navarro JA, Sloan A, Michalsen JR, Stern AM, et al. Nonpharmaceutical interventions implemented by US cities during the 1918–1919 influenza pandemic. JAMA. 2007;298:644–54. doi: 10.1001/jama.298.6.644. [DOI] [PubMed] [Google Scholar]
- 4.Hatchett RJ, Mecher CE, Lipsitch M. Public health interventions and epidemic intensity during the 1918 influenza pandemic. Proc Natl Acad Sci USA. 2007;104:7582–7. doi: 10.1073/pnas.0610941104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rosenkrantz B. Public health and the state. Cambridge (MA): Harvard University Press; 1972. [Google Scholar]
- 6.Rosner D, editor. Hives of sickness. New Brunswick (NJ): Rutgers University Press; 1991. [Google Scholar]
- 7.Epidemic influenza. New York Times. 1889. Dec 18, p. 4.
- 8.An official warning. New York Times. 1890. Jan 1, p. 1.
- 9.Tomes N. The gospel of germs: men, women and the microbe in American life. Cambridge (MA): Harvard University Press; 1998. [PubMed] [Google Scholar]
- 10.Hammonds EM. Childhood's deadly scourge: the campaign to control diphtheria in New York City, 1880–1930. Baltimore: Johns Hopkins University Press; 1999. [Google Scholar]
- 11.Rogers N. Dirt and disease: polio before FDR. New Brunswick (NJ): Rutgers University Press; 1992. [Google Scholar]
- 12.Leavitt JL. Typhoid Mary: captive to the public's health. Boston: Beacon Press; 1996. [Google Scholar]
- 13.Markel H. East European Jewish immigrants and the New York City epidemics of 1892. Baltimore: Johns Hopkins University Press; 1997. Quarantine! [Google Scholar]
- 14.Shah N. Contagious divides: epidemics and race in San Francisco's Chinatown. Berkeley (CA): University of California Press; 2001. [PubMed] [Google Scholar]
- 15.Ott K. Fevered lives: tuberculosis in American culture since 1870. Cambridge (MA): Harvard University Press; 1999. [Google Scholar]
- 16.Soper GA. The lessons of the pandemic. Science. 1919;49:501–6. doi: 10.1126/science.49.1274.501. [DOI] [PubMed] [Google Scholar]
- 17.Starr P. The creation of the media: political origins of modern communication. New York: Basic Books; 2005. [Google Scholar]
- 18.Hansen B. America's first medical breakthrough: how popular excitement about a French rabies cure in 1885 raised new expectations for medical progress. Am Hist Rev. 1998;103:373–418. [PubMed] [Google Scholar]
- 19.Jordan EO. Epidemic influenza: a survey. Chicago: University of Chicago Press; 1927. [Google Scholar]
- 20.Tomes N. The private side of public health: sanitary science, domestic hygiene, and the germ theory. Bull Hist Med. 1990;64:498–539. [PubMed] [Google Scholar]
- 21.Greenwood M. Epidemics and crowd diseases: an introduction to the study of epidemiology. London: Williams and Norgate; 1935. [Google Scholar]
- 22.Carlen A. Plague's progress: a social history of man and disease. London: Victor Gollancz; 1995. [Google Scholar]
- 23.Epidemic shows no signs of immediate abatement. Variety. 1918. Oct 11, p. 1.
- 24.Markel H, Stern AM, editors. The American influenza epidemic of 1918: a digital encyclopedia. Ann Arbor (MI): Center for the History of Medicine; [cited 2010 Mar 30]. Forthcoming 2012. Available from: URL: http://www.influenzaarchive.org. [Google Scholar]
- 25.Ackerknecht E. Anticontagionism between 1821 and 1867. Bull Hist Med. 1948;22:562–93. [PubMed] [Google Scholar]
- 26.Robins N. Copeland's cure. New York: Knopf; 2005. [Google Scholar]
- 27.Epidemic lessons against next time. New York Times. 1918. Nov 17, p. 42.
- 28.Teachers will fight the epidemic. Detroit News. 1918. Oct 22, p. 1.
- 29.How to fight Spanish influenza. Literary Digest. 1918. Oct 12, pp. 13–4.
- 30.Zimmerman DA. Markets, crises, and crowds in American fiction. Chapel Hill (NC): University of North Carolina Press; 2006. Panic! [Google Scholar]
- 31.Jones EW. Cooperation is all human endeavor. Can Bull Med Hist. 2005;22:57–82. doi: 10.3138/cbmh.22.1.57. [DOI] [PubMed] [Google Scholar]
- 32.Chicago shut. Variety. 1918. Oct 18, p. 7.
- 33.Priests oppose church closing. New Orleans States. 1918. Oct, p. 7.
- 34.Editorial. Variety. 1918. Nov 1, p. 11.
- 35.Philadelphia in doubt. Variety. 1918. Oct 10, p. 7.
- 36.Spitters fined. Philadelphia Evening Bulletin. 1918. Oct 16, p. 2.
- 37.For strict reports on new grip cases. New York Times. 1918. Oct 29, p. 10.
- 38.F.D. Roosevelt Spanish grip victim. New York Times. 1918. Sep 20, p. 14.
- 39.New influenza cases in the city doubled. New York Times. 1918. Sep 28, p. 10.
- 40.Influenza losing ground in Boston. Boston Daily Globe. 1918. Sep 20, p. 14.
- 41.Italians can aid the advisory board. Boston Daily Globe. 1919. Oct 14, p. 14.
- 42.Precautions urged to stay influenza. Indianapolis Star. 1918. Sep 29, pp. 1–2.
- 43.Masked men to front voters. Los Angeles Times. 1918. Nov 5, p. 4.
- 44.How the ‘flu' mask traps the germ. Literary Digest. 1918. Dec 21, p. 59.
- 45.Measures for the prevention of the introduction of epidemic influenza. Public Health Rep. 1918;33:1540–4. [Google Scholar]
- 46.Drastic rule in Chicago. New York Times. 1918. Oct 4, p. 24.
- 47.Spanish influenza much like grippe. New York Times. 1918. Sep 22, p. 37.
- 48.Chapin CV. The sources and modes of infection. New York: Wiley; 1910. [Google Scholar]
- 49.Hill HH. The new public health. Minneapolis: Press of the Journal Lancet; 1913. [Google Scholar]
- 50.Bristow NK. Making men moral: social engineering during the Great War. New York: New York University Press; 1996. [Google Scholar]
- 51.Immunity from influenza. Survey. 1922. Apr 1, p. 48.
- 52.Williams EG. Practicing health habits. Am J Nurs. 1927;27:349–51. [Google Scholar]
- 53.Jordan EO. The present status of the influenza problem. Am J Public Health. 1925;15:943–947. doi: 10.2105/ajph.15.11.943-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Prescott HM. Student bodies: the impact of student health on American society and medicine. Ann Arbor (MI): University of Michigan Press; 2007. [Google Scholar]
- 55.Jordan EO. What we know of influenza and how we may add to our knowledge. Am J Public Health. 1930;20:130–6. doi: 10.2105/ajph.20.2.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.The story of a ‘common cold’. Public Health Rep. 1927;42:331–2. [Google Scholar]
- 57.The handkerchief drill, 1949. Plot synopsis on Internet Movie Database. [cited 2010 Feb 23]. Available from: URL: http://www.imdb.com/title/tt0913389.
- 58.Tomes N. Epidemic entertainments. American Literary History. 2002;14:625–52. [Google Scholar]
- 59.John W. Hartman Center for Sales, Advertising & Marketing History; Rare Book, Manuscript, and Special Collections Library, Duke University, Durham, NC. Street car colds! Listerine advertisement, 1929. Medicine and Madison Avenue On-Line Project—Ad #MM0608. [cited 2010 Feb 23]. Available from: URL: http://library.duke.edu/digitalcollections/mma.
- 60.John W. Hartman Center for Sales, Advertising & Marketing History; Rare Book, Manuscript, and Special Collections Library, Duke University, Durham, NC. “Man sized sneezes don't tear it”. Medicine and Madison Avenue On-Line Project—Ad #MM0580. [cited 2010 Feb 23]. Available from: URL: http://library.duke.edu/digitalcollections/mma.
- 61.Apple RD. Perfect motherhood: science and childrearing in America. New Brunswick (NJ): Rutgers University Press; 2006. [Google Scholar]
- 62.Centers for Disease Control and Prevention (US) Interim pre-pandemic planning guidance: community strategy for pandemic influenza mitigation. Atlanta: CDC; 2007. [Google Scholar]
- 63.Tomes N. The making of a germ panic, then and now. Am J Public Health. 2000;90:191–8. doi: 10.2105/ajph.90.2.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gawande A. Better: a surgeon's notes on performance. New York: Henry Holt and Co.; 2007. [Google Scholar]
- 65.Kleenex unveils new research that analyzes sneezing and nose blowing behavior. press release 2007 Dec 12. [cited 2010 Feb 19]. Available from: URL: http://www.businesswire.com.