SYNOPSIS
New York City approached the 1918 influenza epidemic by making use of its existing robust public health infrastructure. Health officials worked to prevent the spread of contagion by distancing healthy New Yorkers from those infected, increasing disease surveillance capacities, and mounting a large-scale health education campaign while regulating public spaces such as schools and theaters. Control measures, such as those used for spitting, were implemented through a spectrum of mandatory and voluntary measures. Most of New York City's public health responses to influenza were adapted from its previous campaigns against tuberculosis, suggesting that a city's existing public health infrastructure plays an important role in shaping its practices and policies during an epidemic.
The threat of a high-fatality influenza pandemic looms large on the public health horizon. Driving the concerns of the international public health community is the fear that H1N1 could become as deadly as the 1918 influenza pandemic that killed between 50 and 100 million people worldwide 90 years ago.1 The influenza pandemic that swept the globe in 1918 was the most acute crisis handled by public health officials in modern times.
When compared with other large U.S. cities, especially its two largest neighbors, Boston and Philadelphia, New York City did not fare poorly in its overall mortality burden. During the pandemic, New York City's excess death rate per 1,000 was reportedly 4.7, compared with 6.5 in Boston and 7.3 in Philadelphia.2 New York City emerged from the three waves of the influenza pandemic (September 1918 to February 1919) officially recording approximately 30,000 deaths out of a population of roughly 5.6 million due to influenza or pneumonia, 21,000 of them during the second fall wave (September 14 to November 16).3,4
This article describes and examines the Department of Health's myriad policies and practices used to control the spread of influenza from August through December 1918. New York City's proactive approach to controlling the influenza epidemic was a product of the city's existing public health infrastructure and employed a variety of tactics familiar to public health practice at the turn of the 20th century.
The most notable strategies to control the spread of influenza were changes in legal statutes that mandated staggered business hours to avoid rush-hour crowding and established more than 150 emergency health districts and centers to coordinate home care and case reporting. The sick were cared for and counted in hospitals, at home, and in gymnasia and armories. Even the Municipal Lodging House, Manhattan's first homeless shelter on East 25th Street, was temporarily converted for the duration of the epidemic.5
State health officials used a modified maritime quarantine for New York City-bound ship traffic. In fact, the harbor's maritime quarantine was in place for at least a month before the first confirmed cases of influenza were reported in the city by the press on August 14, 1918. At the ports, traditional maritime quarantine usually carried out by New York state officials was abandoned in favor of a land-based quarantine strategy in part due to considerations for the war effort.
The city increased its capacities for disease surveillance through physician reporting and health inspection, while a massive public health education campaign persuaded New Yorkers to cover their coughs and sneezes and stop spitting. Standard public health techniques were used to limit the exposure of the general population to influenza cases and attempted to distance New Yorkers from one another. These techniques and interventions varied in their level of compulsion: the New York City response relied on a mix of mandatory as well as voluntary measures to curb the spread of the disease. The Department of Health applied this framework to policies regarding schools and theaters, which stayed open throughout the epidemic, though under careful regulation. Anti-spitting measures consisted of health education efforts backed by the threat of misdemeanor fines and watchful police officers.
LEGAL BASIS OF THE PUBLIC HEALTH RESPONSE
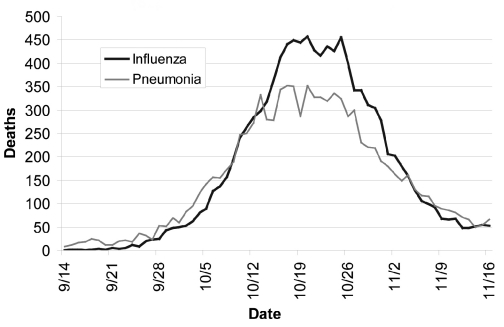
In the middle of September, the Board of Health began making changes to the Sanitary Code. On September 17, it made influenza and pneumonia reportable for the first time in New York City's history and on October 4 officially resolved that an epidemic existed. As reported in the Annual Report of the New York City Department of Health, for the two weeks between October 5 and October 19, influenza deaths mounted until cresting around October 21 (Figure). From October 26 onward, the number of deaths from both influenza and pneumonia quickly declined and by mid-November had returned to levels comparable to the previous year's influenza and pneumonia mortality rates. After November 4, the only item left on the Board of Health's influenza docket was to process the glut of hiring and compensation forms in the wake of a dramatic emergency expansion of the public health workforce.6
Figure.
Reported deaths from influenza and pneumonia in New York City, September to November 1918
Source: Department of Health of the City of New York. Annual report of Department of Health of the City of New York for the calendar year 1918. New York: William Bratler, Inc.; 1919.
The Board of Health mandated a number of compulsory actions to slow the disease's spread. By far, the action most felt by New Yorkers was their Board of Health's decision to establish a timetable to regulate the opening and closing hours of businesses. Passed on October 4, this timetable staggered the hours of business opening and closing with the intention of easing congestion in the public transit system during the morning and afternoon rush. It was hoped that reducing crowding both on subway and elevated train platforms and inside the train cars would slow the spread of influenza.6
Health Commissioner Royal S. Copeland reasoned that more restrictive means, such as ordering all businesses and municipal offices closed, was unwarranted because of the low incidence and concentrated prevalence of the disease.7 Though this order carried with it the full weight of the police powers of the Board of Health, it is not clear the degree to which it was enforced. Media accounts paint a mixed picture of the city's reaction to the timetable. It was initially greeted with confusion and criticism about its ineffectiveness at reducing crowding in the subways during its first week, and it is unclear how many New York businesses complied.7–10
The mandatory timetable codified in the Sanitary Code was created with input from those most affected by it. Before it was enacted, Copeland and other health officials met with representatives of New York City's business community, including large employers such as the Tobacco Products Corporation, to explain the logistics of the order and the reasons it was needed.11
Business interests also had a voice in altering the timetable once it took effect. In fact, Copeland proved very amenable to changing the specifics of the timetable for the sake of businesses and manufacturers. In the wake of the numerous complaints lodged against the Board of Health's orders, Copeland negotiated new opening and closing hours with some large department stores, theaters, and banks and exempted municipal and federal offices from the order the day after it took effect.6,12
Widely disbursed cases, along with an inadequate means of delivering nursing services, led the Department of Health to create a network of emergency health centers. The “clearinghouse plan,” rolled out on October 7, divided the city into sub-units and established about 150 temporary emergency health centers. Copeland described the centers as the clearing house through which all the local activities of the Department of Health will be carried.13
Although some emergency district health centers acted as clinics and kept track of available hospital beds, their main purpose was to act as headquarters for nurses delivering home health care in their districts while operating as a base of operations for the health inspectors who often assisted them. The Department of Health met the shortage of public health inspectors through new hires using emergency appropriations from the Board of Estimate and inspectors reassigned from the Tenement House Department.13 Nursing care was coordinated through the Nurses' Emergency Council, created and chaired by Lillian D. Wald, who also served on the Emergency Advisory Committee created to help Commissioner Copeland manage the epidemic. Nursing, in fact, was a major part of the public health response to the epidemic. City health officials coordinated care with Lillian Wald and others to tend to the ill, survey tenement house districts, and care for those in isolation.
A covenant enacted on October 17 required all people “… to protect their nose or mouth while coughing or sneezing.” Though this policy was not rigorously enforced, this amendment to the Sanitary Code provided the legal basis for any fines or other punitive measures issued by sanitarians and police officers.6
On October 19, the Board of Health overhauled the administrative structure of the Department of Health. Under this new organizational structure, more authority was granted to each borough's sanitary superintendants and assistant superintendants. Under the new plan, the heads of each borough were given the power to regulate, order, and “… remove, abate, suspend, alter or otherwise improve” places that sell, store, or serve food and drink with the same authority as if their orders were issued by the Board of Health. This plan intended to clarify the Department of Health's chain of command and increase each borough's autonomy to regulate local health matters.6
Board of Health regulations were sometimes grim. On October 30, Mayor John F. Hylan ordered 75 men dispatched to the Calvary Cemetery to help it meet a Board of Health deadline for interring unburied bodies that were stored in a two-level shed acting as an overflow area for the cemetery's receiving vault.6,14
New York City did not shape its policies around bacteriological investigations of influenza despite furious attempts by the Department's laboratories to come to conclusive results about its etiology and transmissibility. Rather, the Department of Health built its control plan around its experiences fighting tuberculosis at the beginning of the century. By and large, New York City health officials responded to the influenza with the public health machinery that was the hallmark of 19th-century public health practice.
QUARANTINE AT THE PORT
Various techniques were used to distance influenza victims from the rest of the healthy population. At the beginning of the century, infection-control measures included personal quarantine at home for the sick and their contacts, use of placards to identify places where the sick resided, keeping children at home, and isolations at the request of private physicians. As is the case today, the ill were sometimes forcibly isolated on North Brothers Island in the East River or in other state-run facilities in New York Harbor. Modified sanitary cordons, port closures, and travel restrictions at railway terminals were also identified as forms of quarantine. As other authors have explained, quarantine, even before the influenza epidemic, was a complex concept with multiple meanings and uses.15
Newspaper accounts identified the arrival of influenza in New York's port on August 14, 1918, a full month before influenza was made a reportable disease by the Department of Health. According to the press, eight passengers were isolated by state inspectors at the Norwegian Hospital in Brooklyn after disembarking from a Norwegian steamship on fears they were infected with influenza.16–18 The Norwegians who supposedly brought influenza to New York City's port were identified because New York (state) port officials had increased disease surveillance on inbound ship traffic to actively monitor for influenza since the beginning of July 1918 using modified quarantine measures to do so.19–22
In typical cases of maritime quarantine, New York State port officials would hold ships at a quarantine station in the harbor for inspection and a waiting period before letting them land.15,23 After bacteriological investigation became more prevalent in the late 1890s, cultures were collected from passengers who waited for days in quarantine while labs cultured their specimens. However, this was not the case during the summer of 1918, perhaps due to the unknown etiology of influenza.
Media accounts suggest that port quarantine measures were modified in the summer of 1918 specifically to monitor for “Spanish” influenza coming from Europe. Under the modified system of quarantine at the port, ships were boarded by port health officials, inspected, and then proceeded to immediately dock at port. Once docked, passengers identified as having flu-like symptoms during the inspection were put in ambulances and driven to the hospital where they were isolated. Statements made to the press indicate that isolation, as well as contact tracing, were carried out by the Department of Health once the sick were in quarantine.19,21,24,25 This maritime quarantine may have continued into late September, well after native cases developed.
Although newspapers reported that the first cases of influenza in New York City came via the port on August 14, 1918, the cases from the Norwegian steamship were not the first to reach New York City's shores. Roughly 180 cases of “active” influenza arrived on vessels bound for New York City between July 1 and mid-September. Approximately 305 cases of suspected influenza were reported throughout the voyages of 32 ships' port health officers examined from July through September, including victims who died while at sea or recovered from their illness.26 Health officials did not report any secondary outbreaks of influenza from the index cases that arrived through the harbor before August 14, 1918.
New York State health officials opted for a maritime quarantine in the case of influenza to ensure the uninterrupted movement of goods and supplies to Europe for the war effort. America entered World War I on April 6, 1917, and New York City was the main point of embarkation for American doughboys heading to the European fronts.27 Col. J. M. Kennedy, the army officer in charge of medical affairs for the district of New York, met with local health officials in the summer of 1918 to discuss the possibility of a quarantine measure for influenza and concluded that a typical maritime quarantine for influenza would not be appropriate or practical. As Leland E. Cofer, the State of New York's Health Officer of the Port of New York City, explained:
“Before any of the vessels arrived with influenza on board, the matter of quarantining influenza was considered solely on account of its possible bearing on the military and naval situation… it was more advantageous for the public to face a possible infection with influenza than to hinder the movement of vessels by any quarantine method which would prove effective.”26
VOLUNTARY ISOLATION AND HOME QUARANTINE
Due to practical concerns, isolation measures used during the 1918 epidemic took on a slightly different form than the protocols for quarantine and isolation used at the turn of the century for yellow fever, diphtheria, or smallpox. Under typical public health protocols, a person would either be bound to their home for the duration of their illness and a placard placed on their door, or they would be removed from their home and isolated in a hospital or sanitarium. Given the high number of cases in New York City, placard isolation for influenza was impractical and unenforceable. State Commissioner of Health Herman M. Biggs summarized the dilemma of isolation and quarantine by explaining that such measures “… while theoretically desirable, are not practical in view of the highly contagious character and the widespread extent of the malady and the general susceptibility to it.”28
Copeland's Health Department opted for a two-tiered approach to isolating cases of influenza. As Copland explained to The New York Times on September 19, “When cases develop in private houses or apartments they will be kept in strict quarantine there. When they develop in boarding houses or tenements they will be promptly removed to city hospitals, and held under strict observation and treated there.”29 Influenza cases found in tenement and boarding homes were to be removed to municipal hospitals. All other cases were put under home quarantine without placards.29,30 Placarded quarantine was not used because of the belief that there were no asymptomatic cases of influenza. As Copeland explained in the press:
“The Health Department has not deemed it necessary to quarantine families in which there are cases of influenza because this disease is held not to be communicable by one who has not himself got influenza. It matters not that a person is exposed to the malady unless he himself is stricken with it. The danger of infection lies almost entirely, it is said, in the coughing and sneezing of one who actually has influenza.31
The responsibility for ensuring compliance with the home isolation measure fell on the shoulders of attending physicians. Doctors were required to report if they were assuming responsibility for isolating their patient when they reported cases to the Department of Health.32,33 It seems unlikely that individual doctors were able to ensure their patients complied with their orders to stay home during a time when doctors in New York City's East Side neighborhood were reportedly “mobbed by women demanding their services.”18
Without doctors or sanitarians rigorously enforcing isolation orders, isolation was a de facto voluntary measure. Despite the obligation of physicians to enforce isolation orders and the ubiquitous presence of public health nursing efforts and inspectors, daily enforcement of isolation orders fell on the shoulders of the ill and their families. The Bureau of Public Health Education's annual report contains no evidence that placards were printed for posting on dwellings.
SURVEILLANCE AND HEALTH EDUCATION
On September 28, the city's Board of Estimate approved the first emergency appropriation to the Department of Health to fight influenza. The first and largest use of the appropriation went toward printing health education materials. The second largest appropriation was used to hire nurses and health inspectors who could help the city count its sick. The Board of Estimate's first appropriation is telling: when confronted with the prospect of an influenza epidemic, the city's first move was to increase its health education and surveillance capacities.
Tandem programs of health education and surveillance had been mainstays of the Department of Health's infectious disease control procedures since the late 19th century and were touted as two of the primary means of countering the spread of tuberculosis. Surveillance measures were expanded in the 1890s, most notably through mandates that physicians report cases of tuberculosis to the Department of Health. Health education also took on a prominent role, persuading the tubercular to act in ways that would lessen the risk of transmitting their disease. Educational campaigns, compulsory notification of cases by public institutions and private physicians, and case follow-up were the most important efforts in New York City's tuberculosis control plan.34 In its efforts to control the influenza epidemic, the Health Department heavily relied on these precedents.
As the eyes of the Health Department, physicians were the primary means of collecting health information. The Board of Health's order on September 17 that made influenza and pneumonia reportable also required physicians to report the name, age, sex, and address of their patients. Two weeks later, Copeland expanded the reporting requirements for physicians, requesting that they also report “the sanitary conditions of the home.”33
To better coordinate care and treatment services, inspectors borrowed from the Tenement House Authority undertook a house-to-house canvas in which they attempted to find previously undocumented cases of flu and pneumonia and report on the needs of the families.35
Just as the Department of Health had enlisted laypeople, specifically janitors and landlords, to report tuberculars beginning in 1902, Copeland appealed for help beyond the medical community to count cases of influenza.34 In a move that The New York Times called “rather unusual,” Copeland appealed to Tammany Hall to use its “… party machinery to seek out influenza cases.36 Five days later, the Tammany Hall Executive Committee obliged. According to the Times, “… the entire organization, with its election district captains, was turned over to the Department of Health to aid Commissioner Copeland in the Spanish influenza epidemic.”37
Along with case reporting, the Department of Health used health education to control the influenza epidemic. By September 24, at least 10,000 posters had been placed around the city in railway stations, elevated train platforms, street cars, store windows, police precincts, hotels, and other public places. At least three different health posters were distributed during the epidemic: one instructing people to cover their coughs and sneezes, one not to spit, and the last titled, “Help to Prevent the Return of the ‘Flu’ and Pneumonia!”3,38 Compared to other local health departments, the New York City Department of Health had an unrivaled capacity for creating and disseminating health education materials. Established in 1914, theirs was the first health department to formally incorporate health education into public health practice.
KEEPING SCHOOLS OPEN
In an October 5 New York Times story, Commissioner Copeland outlined the logic behind one of his most controversial decisions during the epidemic: the continued operation of New York's public schools.
“New York is a great cosmopolitan city and in some homes there is careless disregard for modern sanitation… In schools the children are under the constant guardianship of the medical inspectors. This work is part of our system of disease control. If the schools were closed at least 1,000,000 would be sent to their homes and become 1,000,000 possibilities for the disease. Furthermore, there would be nobody to take special notice of their condition.”7
In Copeland's mind, there was no real danger of influenza spreading in schools and during the epidemic, he repeatedly defended his decision not to close them.
Copeland's argument was three-fold. First, he advocated for keeping children in schools where “… educational propaganda against influenza can be kept constantly before them.”39 And it was. At the end of September, the Department of Health distributed nearly one million circulars, one for every pupil in the public and parochial schools to take home.40 Second, Copeland believed that the city could do a better job keeping the students healthy than could their families. Last, Copeland made use of the existing school health and medical surveillance programs already in place in New York City schools, which at the time were perhaps the nation's best.
Copeland reasoned that schools were safer than many homes because in the schools children would be under the watchful eye of their teacher and subject to daily medical inspection. As part of the school health and medical surveillance program, teachers were mandated to inspect their pupils daily and report symptomatic children to school medical authorities. School nurses and medical inspectors were instructed to follow up on teacher inspections and conduct home visits on absentee students to determine whether “… they or members of their family are sick, that physical examinations be carefully made, and that dry sweeping [in their home] be discontinued and ventilation sufficient.”3,41 The Board of Superintendents agreed with Copeland's assumption that most children's homes were unsanitary.42
Numerous parties disagreed with the Department of Health's decision to keep the schools open, including the Red Cross of Long Island and former Health Commissioner Dr. S.S. Goldwater. Goldwater did not criticize the Department of Health's parens patriae argument, but instead took issue with the “almost criminal laxity” the schools used in carrying out pupil inspections and case follow-up, the enforcement of which he described as “lamentably weak.”43,44
THE SHOW MUST GO ON
Theaters presented a paradox for the Department of Health. Theaters of all types were an opportunity to educate the public about ways to prevent the spread of influenza, but they also presented an immense risk for spreading the disease. Throughout the city, theaters were not universally closed and instead were subject to increased regulation and inspection.
On October 11, the Board of Health issued regulations for theaters that included prohibiting children younger than age 12 from entering movies or shows. Regulations also included bans on dry sweeping, overcrowding and, in a move truly ahead of its time, smoking. Theaters were also required to ventilate during off-hours by opening all their windows and doors.6 The Board of Health order was enforced through increased inspection, and non-compliant theaters were shut down. Of the greatest concern to Copeland was not the properly maintained, “well-ventilated, sanitary theatre,” but the “insanitary [sic], hole-in-the-wall theatre … the latter sort which our inspectors found was closed immediately …”45
Despite the danger posed by theaters, these public places provided two potential benefits. First, theaters presented an opportunity to educate the public about how not to transmit influenza. Second, Copeland maintained that keeping sanitary theaters with a low risk of spreading contagion in operation would “… prevent the spread of panic and hysteria, and thus to protect the public from a condition of mind which would predispose it to physical ills.”45
REGULATING “THE FILTHY HABIT”
The Department of Health began its anti-spitting campaign more than 20 years prior to the influenza epidemic in 1918. The anti-spitting campaign waged under former Health Commissioner Herman Biggs was based on education, moral suasion, and police enforcement. Pamphlets, with titles such as “Don't Spit,” were translated into English, Italian, German, and Yiddish and distributed in tenement houses from the turn of the century onward. An extensive anti-spitting placarding campaign was evident in public buildings, rail platforms, and ferryboats at a time when preventing the spread of contagious respiratory disease took on a moral tone.46 Biggs' spitting campaign also included fines and arrests for violation of the Sanitary Code. In writing about the extent and efficacy of the Department of Health's anti-spitting campaign in 1908, Biggs wrote that arrests of spitters by the “sanitary police of the Department” were constant and, as a result, “spitting is much less prevalent than it was a few years ago, although still much remains to be desired.”34
The anti-spitting campaign employed during the 1918 influenza epidemic reinforced the same message and used the same tactics. Placards were posted in railway stations, ferries, and public places. Nongovernmental organizations were involved in the Department of Health's suasion, too. The New York Tribune reported that Boy Scouts handed out cards to people spitting on the sidewalk that read: “You are violating the Sanitary Code.”47
Like the previous spitting campaign, education and persuasive efforts occurred in tandem with enforcement.48 New Yorkers caught spitting were usually rounded up and brought before courts in large numbers and available records suggest that few taken to court escaped without fines. On October 4, 134 men were fined $1 at Jefferson Market Court and another three at the Yorkville Court for spitting on subways, subway platforms, and elevated trains. A few days later on October 7, more than 100 spitters were summoned to court; 128 paid a $1 fine and 11 cases were dropped.41,49 Violating the spitting covenants of the Sanitary Code technically resulted in fines or jail time, although no records exist indicating that violators were punished with the latter.36,49,50
CONCLUSIONS
New York City health officials used a combination of traditional public health practices, such as quarantine, isolation, and health information campaigns, in their attempt to control the influenza epidemic. Along with isolation, quarantine, and regulation of public spaces, modifying personal behavior was essential to halt the disease's spread. At the same time the Health Department was borrowing inspectors from other city agencies to complete block-by-block surveys for influenza cases, they recruited laypeople and nongovernmental organizations to increase their surveillance capacity. When compulsory measures were impractical, Copeland's Department of Health turned to persuasive measures, such as posters and pamphlets, because health education was thought to be an appropriate and effective supplement to public health policies.51
The city's health surveillance capacity increased through physician reporting and an expanded workforce of public health inspectors. Health inspection played an important role in schools, too, as they remained open because of the belief that children would be healthier if kept in schools rather than sent home. Schools were also an effective conduit for distributing health education materials to children and their families. Likewise, theaters were subjected to increased regulation and inspection, but not closed because they were another effective venue for disseminating health educational information.
The mandated system of staggered business hours and theater regulations and the use of public health police powers to fine people caught violating the anti-spitting ordinances of the Sanitary Code were the most frequently used means of enforcing healthy practices. In responding to the influenza epidemic, the Health Department scaled up and adapted the programs and practices that had been developed to address tuberculosis. New York City's mixture of mandatory and voluntary measures was part of a broad continuum of public health activities used to stem disease throughout the 19th and early 20th centuries.
In an interview with The New York Times after the epidemic subsided, Copeland commented that New York City “escaped” with a low mortality rate because of the city's health efforts over the previous 20 years. He referenced the consistent efforts of tuberculosis control to improve sanitary conditions, tenement house reform laws mandating good ventilation, and the constant effort to maintain clean streets and to keep the city clean and sanitary.52
When confronted with the overwhelming task of controlling influenza, the New York City Department of Health turned to a variety of time-tested and adaptable regulatory and voluntary techniques already at its disposal. Certainly, the importance of a robust public health infrastructure is instructive as we confront the possibility of a future influenza epidemic.
Acknowledgments
The author thanks David Rosner, James Colgrove, Maryann Aimone, and three anonymous reviewers for their comments on drafts of this article; and Leonora Gidlund and Beth Spinelli for their assistance with archival materials.
REFERENCES
- 1.Johnson N, Mueller J. Updating the accounts: global mortality of the 1918–1920 ‘Spanish’ influenza pandemic. Bull Hist Med. 2002;76:105–15. doi: 10.1353/bhm.2002.0022. [DOI] [PubMed] [Google Scholar]
- 2.Deaths from influenza and pneumonia in cities: 25 weeks, September 8, 1918 to March 1, 1919. Public Health Rep. 1919;34:505–8. [Google Scholar]
- 3.Department of Health of the City of New York. Annual report of Department of Health of the City of New York for the calendar year 1918. New York: William Bratler, Inc.; 1919. [Google Scholar]
- 4.Department of Health of the City of New York. Annual report of Department of Health of the City of New York for the calendar year 1919. New York: 1920. [publisher unknown] [Google Scholar]
- 5.New York City Police Department. New York Police Department annual report for the year 1918. New York: Bureau of Printing; 1919. [Google Scholar]
- 6.Book 31. New York: Municipal Archives of the City of New York; Minutes of the Board of Health of the City of New York, August 10, 1918, to December 31, 1918. [Google Scholar]
- 7.Drastic steps to fight influenza. New York Times. 1918 Oct;5:1. [Google Scholar]
- 8.Epidemic here checked hints Dr. Copeland. New York Tribune. 1918 Oct;7:16. [Google Scholar]
- 9.Influenza orders bring a flood of inquiries. New York Evening Post. 1918 Oct;5:1. [Google Scholar]
- 10.Cars are crowded despite new rules. New York Evening Post. 1918 Oct;7:6. [Google Scholar]
- 11.Copeland Royal S., Whalen Grover H. Mayoral Correspondence Collection, folder 795, box 072. New York: Municipal Archives of the City of New York; 1918. Oct 25, [Google Scholar]
- 12.Six hospitals here taken in influenza fight. New York Tribune. 1918 Oct;6:18. [Google Scholar]
- 13.Copeland Royal S., Hylan John F. Mayoral Correspondence Collection, folder 795, box 072. New York: Municipal Archives of the City of New York; 1918. Oct 18, [Google Scholar]
- 14.Hylan John F., Copeland Royal S. folder 795, box 072, Mayoral Correspondence Collection. New York: Municipal Archives of the City of New York; 1918. Oct 30, [Google Scholar]
- 15.Centers for Disease Control and Prevention (US) A commentary on the JAMA study's interpretation of the influenza experiences in New York City and Chicago, 1918–19. 2008. Jan 17, [cited 2009 Aug 1]. Available from: URL: http://www.cdc.gov/ncidod/dq/1918_commentary.htm.
- 16.Spanish influenza here, shipmen say. New York Times. 1918 Aug;14:1. [Google Scholar]
- 17.8 Spanish grip suspects here; one victim dead. New York Tribune. 1918 Aug;14:12. [Google Scholar]
- 18.Price GM. Mobilizing social forces against influenza. The Survey. 1918;41:95–6. [Google Scholar]
- 19.Health head calls for influenza inquiry. New York Times. 1918 Aug;16:16. [Google Scholar]
- 20.13 Spanish influenza cases come to port. New York Evening Post. 1918 Sep;16:1. [Google Scholar]
- 21.City has 85 cases of Spanish influenza. New York Evening Post. 1918 Sep;23:1. [Google Scholar]
- 22.Epidemic guard for port. New York Times. 1918 Aug;19:5. [Google Scholar]
- 23.Markel H. Baltimore: Johns Hopkins University Press; 1997. Quarantine! East European Jewish immigrants and the New York City epidemics of 1892. [Google Scholar]
- 24.Spanish influenza found in New York. New York Tribune. 1918 Aug;20:7. [Google Scholar]
- 25.Spanish influenza found in ‘mild form’. New York Times. 1918 Aug;20:20. [Google Scholar]
- 2.Influenza may be old-fashioned grip. New York Evening Post. 1918 Sep 19; [Google Scholar]
- 27.Ellis ER. The epic of New York City: a narrative history. New York: Carroll & Graf Publishers; 2004. [Google Scholar]
- 28.Influenza causes Crowder to cancel Oct. 7–11 draft call. New York Tribune. 1918 Sep;27:6. [Google Scholar]
- 29.New York prepared for influenza siege. New York Times. 1918 Sep;19:11. [Google Scholar]
- 30.Subway spreading influenza here. New York Tribune. 1918 Sep;29:10. [Google Scholar]
- 31.Vaccine for influenza. New York Evening Post. 1918 Oct;12:8. [Google Scholar]
- 32.Copeland Royal S. Mayoral Correspondence Collection, folder 793, box 071. New York: Municipal Archives of the City of New York; 1918. Sep 20, to unnamed New York City doctors. [Google Scholar]
- 33.Copeland Royal S. Mayoral Correspondence Collection, folder 795, box 072. New York: Municipal Archives of the City of New York; 1918. Oct 10, to unnamed New York City doctors. [Google Scholar]
- 34.Biggs HM. Brief history of the campaign against tuberculosis. New York: New York City Department of Health; 1908. [Google Scholar]
- 35.Emergency Advisory Committee. Lillian D. Wald Papers, folder 4.1, box 91. Columbia University, New York: Rare Book and Manuscript Library; 1918. Oct 24, Memo to the executives of the emergency health districts. [Google Scholar]
- 36.Fight stiffens here against influenza. New York Times. 1918 Oct;12:13. [Google Scholar]
- 37.Grip in the Y.M.C.A. checked by vaccine. New York Times. 1918 Oct;17:9. [Google Scholar]
- 38.Find 114 cases of influenza here. New York Times. 1918 Sep;24:9. [Google Scholar]
- 2.142,000 draft men held up by influenza. New York Tribune. 1918 Sep;27:6. [Google Scholar]
- 40.New influenza cases in the city doubled. New York Times. 1918 Sep;28:10. [Google Scholar]
- 41.Has clearing house plan for influenza. New York Times. 1918 Oct;8:11. [Google Scholar]
- 42.Influenza lessens school attendance. New York Evening Post. 1918 Oct;15:2. [Google Scholar]
- 43.Asks experts' aid to check epidemic. New York Times. 1918 Oct;13:18. [Google Scholar]
- 44.Closing of schools will be discussed. New York Evening Post. 1918 Oct;19:1. [Google Scholar]
- 45.Copeland Royal S. Mayoral Correspondence Collection, folder 796, box 072. New York: Municipal Archives of the City of New York; 1918. Dec 17, to National Association of the Motion Picture Industry. [Google Scholar]
- 46.Tomes N. The gospel of germs: men, women, and the microbe in American life. Cambridge (MA): Harvard University Press; 1998. [PubMed] [Google Scholar]
- 47.Anti-influenza serum made in tests here. New York Tribune. 1918 Oct;2:14. [Google Scholar]
- 48.Tells of vaccine to stop influenza. New York Times. 1918 Oct;2:10. [Google Scholar]
- 49.Influenza cases increase. New York Evening Post. 1918 Oct;4:2. [Google Scholar]
- Influenza cases still mounting. New York Evening Post. 1918 Oct;11:2. [Google Scholar]
- 51.Duffy J. A history of public health in New York City, 1866–1966. New York: Russell Sage Foundation; 1974. [Google Scholar]
- 52.Epidemic lessons for next time. New York Times. 1918 Nov;17:42. [Google Scholar]