Abstract
Stroke is one of the most life-altering syndromes affecting the world population. Rehabilitation for people experiencing stroke is focused almost exclusively on self-care activities and being able to return home and has little to no focus on work rehabilitation or community reintegration. The Cognitive Rehabilitation Research Group (CRRG) at the Washington University School of Medicine in St. Louis was formed with the vision of improving everyday life for people after stroke by translating knowledge from neuroscience into treatment programs for productive living. Descriptive analysis of the intake assessment from the CRRG Clinical Core (N = 7,740) revealed three important findings: The age at stroke is decreasing, most strokes are neurologically mild to moderate in nature, and discharge placement decisions are being made largely on the basis of measures of impairment. The changes in the stroke population require occupational therapy to expand rehabilitation beyond the acute management of stroke to address full participation in work, family, and community life.
Keywords: occupational therapy, patient care management, rehabilitation, stroke
Stroke is one of the most expensive and life-altering syndromes affecting the ability of people to participate fully in their lives. The American Heart Association (2004) has estimated that approximately 700,000 people experience new or recurrent stroke in the United States each year; 4.8 million stroke survivors are alive today. The direct and indirect cost of stroke in the United States was approximately $53.6 billion, with a mean lifetime cost estimated at $140,048 (American Heart Association, 2004). Recent 30-year projections show that these numbers will drastically increase in the forthcoming years, outpacing overall population growth (Elkins & Johnston, 2003). Current literature has indicated that occupational therapy has been overly focused on rehabilitating functional activities of everyday living and independence in the home with people after stroke (Bendz, 2000, 2003; Medin, Barajas, & Ekberg, 2006). Although functional activities are important, occupational therapists’ focus on functional activities fails to address how stroke survivors will be able to complete activities within the complex social context of everyday life. Although rehabilitation has been successful in helping people return home, it has not been sufficient to help them return to work and to integrate back into the community (Low, Kersen, Ashburn, George, & McLellan, 2003).
The profession of occupational therapy was founded on the principles of occupation and participation, and these principles have now become central concepts in the definition of health (Baum, 2003). Much of the research and clinical work in occupational therapy is aimed at the activity level, as defined by the International Classification of Functioning, Disability and Health (ICF; World Health Organization, 2001), yet society expects occupational therapy to help people live meaningful lives—lives that go beyond the scope of self-care activities to include activities that allow people to manage themselves and others; to engage in work, leisure, and fitness activities; and to be a part of social groups, including families. Scholars have been very directive in asking occupational therapists to focus on a top-down approach to both measurement and treatment (Fisher, 1998; Trombly, 1992), appreciating people's needs in their environmental and cultural context. However, because the profession has been socialized in and responsive to the medical model, practitioners often find themselves practicing from a bottom-up approach, focusing instead on impairment. The impairment-based approach to measurement and treatment has required assessment during the execution of a task or action (ICF definition of activity) assuming that activity participation is simply a by-product of the impairment. Although this approach is a valid way to assess impairment, it neglects a direct assessment of participation; current occupational therapy practice mandates assessment using a top-down approach (Baum & Law, 1997; Fisher, 1998; Mathiowetz & Haugen, 1995; Trombly, 1992).
Participation is defined by the ICF as “involvement in a life situation.” By assessing a person's involvement in a life situation, the therapist captures comprehensive information about how a person is able to use his or her skills and abilities in everyday life. Focusing assessment and intervention on participation will likely identify and treat problems that often go unnoticed in bottom-up assessment. For example, in the stroke population, recent literature has reported that current stroke scales that solely measure impairments can only partially explain the level of disability, including disability related to work outcome (de Haan, Aaronson, Limburg, Hewer, & van Crevel, 1993; Kelly-Hayes et al., 1998). Therefore, it is imperative for the occupational therapy profession to investigate new assessment and intervention protocols aimed at a participation level to address the needs of the stroke population.
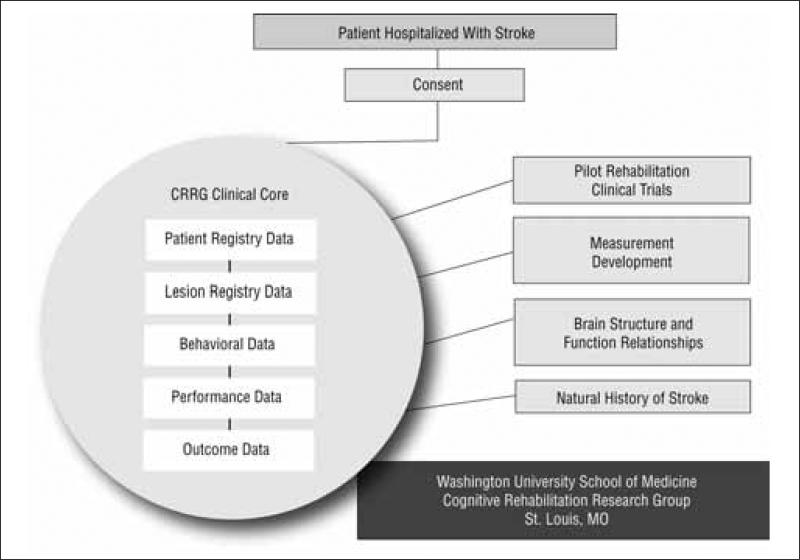
Our research group is a multidisciplinary research effort offering a unique opportunity to address these questions. The Cognitive Rehabilitation Research Group (CRRG) at Washington University School of Medicine in St. Louis was formed in 1996 with the vision of improving everyday life for people with brain injury (primarily stroke) by translating neuroscience into treatment programs for productive living. The CRRG includes a multidisciplinary team of biomedical, social, occupational, and clinical scientists interested both in how neuroscientific knowledge can be applied to improve the function and everyday lives of people with brain injury and in how knowledge of the relationships among structural, cognitive, behavioral, and functional constructs can enhance understanding of brain function. In essence, CRRG's focus is to examine the relationships among brain, behavior, and performance, leading to a greater understanding of outcomes in everyday life. One of CRRG's main efforts has been to build a “clinical core” (Figure 1). At present, the clinical core includes data from neurological examinations, neuroimaging studies, neuropsychological evaluations, performance-based testing, and functional and participation assessments of home and community life of nearly 8,000 people admitted to the Barnes–Jewish Hospital stroke service. The focus of this report is to present the preliminary findings from this cohort of people after stroke to demonstrate how the health care community's understanding of stroke is changing. Specifically, we present data from the CRRG clinical core that show that the age at stroke is decreasing, the majority of strokes are neurologically mild to moderate, and discharge placement decisions should not be made solely on measures of impairment.
Figure 1.
Cognitive Rehabilitation Research Group (CRRG) clinical core.
Method
The clinical core data have been contributed by a prospective cohort of all of the patients hospitalized and served by the neurology service at Barnes–Jewish Hospital in St. Louis (1999–Spring 2008). The Institutional Review Board reviewed and approved this study. Participants (N = 7,740) gave informed consent for testing and consent to have their data placed in the clinical core database. In addition, participants were asked to give consent to be contacted for future follow-up assessments. Testing was administered at Barnes–Jewish Hospital and at the Washington University School of Medicine Program in Occupational Therapy. Data collected included demographic information, the National Institutes of Health Stroke Scale (NIHSS; a measure of neurologic impairment resulting from stroke [Brott et al., 1989]), premorbid functional status, medical history, and discharge dispensation information.
Results
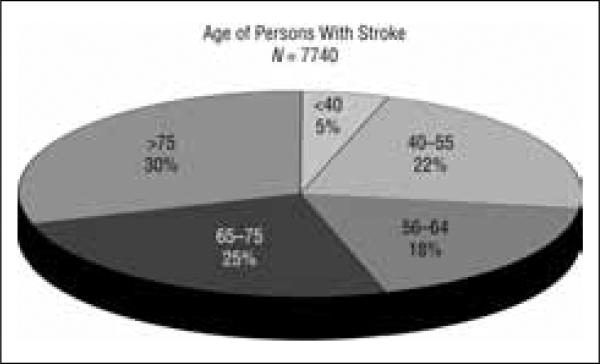
Descriptive analysis of the intake assessment from the CRRG clinical core revealed three important findings. First, analysis revealed that of the cohort of 7,740 people after stroke, 45% of the patients were <65 years old, and nearly 27% were <55 years old (Figure 2). Second, of all the patients who had sustained strokes, 49.3% had a mild stroke, defined as a NIHSS score <6. This score indicates that the person likely had no significant aphasia or unilateral spatial neglect, no major motor problems, was able to manage all of his or her activities of daily living (ADLs), had enough mobility to get in and out of bed, and was able to transfer to a toilet. Of this sample, 32.8% had a moderate stroke and an NIHSS score of 6–16, those typically seen for rehabilitation services. Finally, 17.9% of the sample had a severe stroke, and 6% died. Nearly half had mild neurological impairment, which results in changes that although not visible, have a devastating impact on the person's daily performance and the people in their social networks. Third, of those who had mild to moderate stroke, 71% were discharged directly home, discharged with home services only, or discharged with outpatient services only; these services have limited focus on work rehabilitation and community reintegration. On the basis of CRRG follow-up assessment, although people with mild or moderate stroke may have received occupational therapy services, they were not successful in reintegrating back into their everyday lives. Specifically, of 288 people with mild stroke who reported that they had returned to work, 46% reported working slower, 42% reported not being able to do the job as well, 31% reported not being able to keep organized, and 52% reported not being able to concentrate.
Figure 2.
Decreasing age at first stroke.
Discussion
The data collected by the CRRG clinical core and reported here demonstrate that critical changes are taking place in the stroke population that underscore the need to change rehabilitation practice, particularly occupational therapy practice. The demographic shift to younger people having stroke, the increase in survival with relatively modest neurological impairment coupled with the significant impact that stroke has on the daily lives of people, and the importance of discharge placement decisions require the attention of occupational therapy.
Age of Stroke Is Decreasing
Nearly half of all people who have had stroke are <65 years old, and a large percentage are <55 years old. The rehabilitation services offered to these people are largely based on self-care. The needs of the younger person with stroke go far beyond self-care and include family issues, work, driving, marriage responsibilities, and community participation. U.S. rehabilitation programs are not organized to serve these needs. In fact, this study demonstrated that many of these people get minimal or no services after stroke. Not addressing these broader issues has a dramatic impact on the person and also on society at large. For example, stroke rehabilitation largely overlooks employment. Beyond the financial implications implicit in the need to return to work, the ability to successfully reenter the competitive work force has more far-reaching implications that are instrumental in the recovery of the person after stroke. Return to work contributes significantly to life satisfaction, well-being, self-worth, and social identity after stroke (Banks & Pearson, 2003; Koch, Egbert, Coeling, & Ayers, 2005; Stuart, 2004; Vestling, Tufvesson, & Iwarsson, 2003).
In addition, inability to return to work has a significant financial impact on society. Multiple factors are responsible for the rising cost of stroke; however, lack of productivity after stroke has now become one of the most costly factors associated with stroke because of the increasing percentage of people having strokes who are of working age. In a recent Canadian study of people employed full-time before their stroke, only 9% returned to work full-time after discharge from treatment (Teasell, McRae, & Finestone, 2000). Lack of productivity, namely the inability to return to work, has now been estimated to be responsible for up to 25% of all costs (direct and indirect) of stroke and as much as 58% of the indirect cost of stroke (Saeki, 2000; Terent et al., 1994). Despite these statistics, current stroke rehabilitation efforts are dramatically overlooking work rehabilitation (Bendz, 2000, 2003). Therefore, future studies need to focus on the development of assessment and intervention strategies that target these broader rehabilitation needs of people with stroke, including but not limited to work rehabilitation and community reintegration.
Majority of Strokes Are Neurologically Mild to Moderate in Nature
According to currently accepted impairment-based stroke scales that measure the neurologic severity of stroke, the majority of strokes are classified as being mild to moderate in nature; however, as previously mentioned, current stroke scales that measure only impairments can only partially explain the concomitant disability (de Haan et al., 1993; Kelly-Hayes et al., 1998). Therefore, the designation of having had a mild to moderate stroke based on the NIHSS does not reflect the participation deficits the person will demonstrate after returning home; it simply demonstrates that the stroke scale does not focus on the constructs that map onto limitations in participating in everyday activities. Although people may not demonstrate outward signs of impairment after stroke, people with mild to moderate neurologic impairment are reporting and demonstrating deficits when they return to the lives they were living before stroke. As demonstrated by CRRG clinical core data, these people have deficits that have an impact on performance in complex everyday activities. As a profession, occupational therapy needs to evaluate the assessment tools used to establish patients’ previous level of function and, consequently, their needs for rehabilitation services.
Discharge Placement Decisions Should Not Be Made Solely on the Basis of Measures of Impairment
In the current medical climate, 71% of people who have had mild to moderate stroke are discharged with minimal or no services, in large part because stroke scales do not identify all of the deficits that affect participation after stroke. The person does not have significant aphasia or neglect, does not have major motor problems, can manage all of his or her ADLs, has enough mobility to get in and out of bed, and can transfer to a toilet. Therefore, the person is told that he or she does not need rehabilitation. This study has demonstrated that in our current environment, the person who has had a stroke is likely to be younger and engaged in more complex activities beyond ADLs; his or her deficits are exhibited in cognitively demanding activities like employment. The stroke scales used by neurologists to make discharge placement decisions do not provide the health care provider with sufficient information to determine whether the person will have difficulty with these more complex occupations. Therefore, the occupational therapy profession needs to be persistent in implementing performance-based measures and occupational histories as part of routine acute care for people who have had a stroke. Future studies need to focus on developing a more comprehensive assessment of people who have had a stroke; this comprehensive assessment will be used in discharge determination.
Conclusion
These changes—age, stroke severity, and discharge placement—present important challenges to the profession of occupational therapy. The focus of rehabilitation needs to expand beyond the acute management of stroke to address full participation in work, family, and community life. It opens opportunities for new initiatives in return to work, focusing on cognitive behavioral strategies; requires programs such as driving assessment and training; and demands prevention strategies such as self-management and fitness because stroke is no longer considered an acute episode but rather a chronic condition that requires behavioral and health changes. Right now, while we as a profession are in the midst of working toward our Centennial Vision (American Occupational Therapy Association, 2007), occupational therapy needs to emphasize meeting societal needs for health and well-being. This report has demonstrated that people who have had a stroke need occupational therapy to meet this need. ▲
Acknowledgments
We acknowledge the James S. McDonnell Foundation (Grant 220020087, Carolyn Baum, PI) for the support of this study. In addition, we would like to thank the faculty, staff, and students in the Cognitive Rehabilitation Research Group at Washington University in St. Louis School of Medicine.
Contributor Information
Timothy J. Wolf, Instructor of Occupational Therapy and Neurology and Investigator, Cognitive Rehabilitation Research Group, Washington University School of Medicine, 4444 Forest Park Avenue, Campus Box 8505, St. Louis, MO 63108; wolft@wustl.edu.
Carolyn Baum, Professor of Occupational Therapy and Neurology, Elias Michael Director of Program in Occupational Therapy, and Principal Investigator, Cognitive Rehabilitation Research Group, Washington University School of Medicine, St. Louis, MO..
Lisa Tabor Connor, Assistant Professor of Occupational Therapy, Radiology, and Neurology and Principal Investigator, Clinical Core, Cognitive Rehabilitation Research Group, Washington University School of Medicine, St. Louis, MO..
References
- American Heart Association . Heart disease and stroke statistics—2004 update. American Heart Association; Dallas, TX: 2004. [Google Scholar]
- American Occupational Therapy Association AOTA's Centennial Vision and executive summary. American Journal of Occupational Therapy. 2007;61:613–614. doi: 10.5014/ajot.61.6.622. [DOI] [PubMed] [Google Scholar]
- Banks P, Pearson C. Improving services for younger stroke survivors and their families. University of Glasgow, Strathclyde Centre for Disability Research; Glasgow, Scotland: 2003. Retrieved from www.chss.org.uk/pdf/research/Young_stroke_study_2003.pdf. [Google Scholar]
- Baum CM. Participation: Its relationship to occupation and health. OTJR: Occupation, Participation and Health. 2003;23(2):46–47. [Google Scholar]
- Baum CM, Law M. Occupational therapy practice: Focusing on occupational performance. American Journal of Occupational Therapy. 1997;51:277–288. doi: 10.5014/ajot.51.4.277. [DOI] [PubMed] [Google Scholar]
- Bendz M. Rules of relevance after a stroke. Social Science and Medicine. 2000;51:713–723. doi: 10.1016/s0277-9536(99)00486-4. [DOI] [PubMed] [Google Scholar]
- Bendz M. The first year of rehabilitation after a stroke-from two perspectives. Scandinavian Journal of Caring Sciences. 2003;17(3):215–222. doi: 10.1046/j.1471-6712.2003.00217.x. [DOI] [PubMed] [Google Scholar]
- Brott T, Adams HP, Jr., Olinger CP, Marler JR, Barsan WG, Biller J, et al. Measurements of acute cerebral infarction: A clinical examination scale. Stroke. 1989;20(7):864–870. doi: 10.1161/01.str.20.7.864. [DOI] [PubMed] [Google Scholar]
- de Haan R, Aaronson N, Limburg M, Hewer RL, van Crevel H. Measuring quality of life in stroke. Stroke. 1993;24(2):320–327. doi: 10.1161/01.str.24.2.320. [DOI] [PubMed] [Google Scholar]
- Elkins JS, Johnston SC. Thirty-year projections for deaths from ischemic stroke in the United States. Stroke. 2003;34(9):2109–2112. doi: 10.1161/01.STR.0000085829.60324.DE. [DOI] [PubMed] [Google Scholar]
- Fisher AG. Uniting practice and theory in an occupational framework. American Journal of Occupational Therapy. 1998;52:509–521. doi: 10.5014/ajot.52.7.509. [DOI] [PubMed] [Google Scholar]
- Kelly-Hayes M, Robertson JT, Broderick JP, Duncan PW, Hershey LA, Roth EJ, et al. The American Heart Association Stroke Outcome Classification: Executive summary. Circulation. 1998;97(24):2474–2478. doi: 10.1161/01.cir.97.24.2474. [DOI] [PubMed] [Google Scholar]
- Koch L, Egbert N, Coeling H, Ayers D. Returning to work after the onset of illness: Experiences of right hemisphere stroke survivors. Rehabilitation Counseling Bulletin. 2005;48(4):209–218. [Google Scholar]
- Low J, Kersen P, Ashburn A, George S, McLellan D. A study to evaluate the met and unmet needs of members belonging to young stroke groups affiliated with the stroke associations. Disability and Rehabilitation. 2003;25(18):1052–1056. doi: 10.1080/0963828031000069753. [DOI] [PubMed] [Google Scholar]
- Mathiowetz V, Haugen JB. Evaluation of motor behavior: Traditional and contemporary views. In: Trombly CA, editor. Occupational therapy for physical dysfunction. Williams & Wilkins; Baltimore: 1995. pp. 157–185. [Google Scholar]
- Medin J, Barajas J, Ekberg K. Stroke patients’ experiences of return to work. Disability and Rehabilitation. 2006;28(17):1051–1060. doi: 10.1080/09638280500494819. [DOI] [PubMed] [Google Scholar]
- Saeki S. Disability management after stroke: Its medical aspects for workplace accommodation. Disability and Rehabilitation. 2000;22(13–14):578–582. doi: 10.1080/09638280050138241. [DOI] [PubMed] [Google Scholar]
- Stuart H. Stigma and work. Healthcare Papers. 2004;5(2):100–111. doi: 10.12927/hcpap..16829. [DOI] [PubMed] [Google Scholar]
- Teasell R, McRae M, Finestone H. Social issues in the rehabilitation of younger stroke patients. Archives of Physical Medicine and Rehabilitation. 2000;81:205–209. doi: 10.1016/s0003-9993(00)90142-4. [DOI] [PubMed] [Google Scholar]
- Terent A, Marke LA, Asplund K, Norrving B, Jonsson E, Wester PO. Costs of stroke in Sweden: A national perspective. Stroke. 1994;25(12):2363–2369. doi: 10.1161/01.str.25.12.2363. [DOI] [PubMed] [Google Scholar]
- Trombly CA. Deficits of reaching in subjects with left hemiparesis: A pilot study. American Journal of Occupational Therapy. 1992;46:887–897. doi: 10.5014/ajot.46.10.887. [DOI] [PubMed] [Google Scholar]
- Vestling M, Tufvesson B, Iwarsson S. Indicators for return to work after stroke and the importance of work for subjective well-being and life satisfaction. Journal of Rehabilitation Medicine. 2003;35(3):127–131. doi: 10.1080/16501970310010475. [DOI] [PubMed] [Google Scholar]
- World Health Organization . International classification of functioning, disability and health. Author; Geneva: 2001. [Google Scholar]