Abstract
Frequent consumption of simple carbohydrates, primarily in the form of dietary sugars is significantly associated with increased dental caries risk. Malnutrition (under or over nutrition) in children is often a consequence of inappropriate infant and childhood feeding practices and dietary behaviors associated with limited access to fresh, nutrient dense foods substituting instead, high-energy low cost and nutrient poor sugary and fatty foods. Lack of availability of quality food stores in rural and poor neighborhoods, food insecurity, and changing dietary beliefs resulting from acculturation including changes in traditional ethnic eating behaviors, can further deter healthful eating and increase risk for Early Childhood Caries and obesity.
America is witnessing substantial increases in children and ethnic minorities living in poverty, widening the gap in oral health disparities noted in the Surgeon General's Report, Oral Health in America. Dental and other care providers can educate and counsel pregnant women, parents and families to promote healthy eating behaviors and should advocate for governmental policies and programs that decrease parental financial and educational barriers to achieving healthy diets. For families living in poverty, however, greater efforts are needed to facilitate access to affordable healthy foods, particularly in urban and rural neighborhoods in order to effect positive changes in children's diets and advance the oral components of general health.
Keywords: Diet and pediatric caries
The prevalence of dental caries in primary teeth, early childhood caries (ECC), increased from approximately 40 percent in children aged 2–11 years in the 1988–1994 National Health and Nutrition Examination Survey (NHANES) to 42 percent in the 1999–2004 survey.1 For children 2–5 years of age the rate increase was greater, rising from 24 percent to 28 percent. Increases were identified specifically among non-Hispanic white males and children living in households with incomes at or below the Federal Poverty Level (FPL).2 Changing and increasing numbers of ethnic minorities, cultural and dietary practices, and children living in poverty have widened the chasm of disparity.3 Understanding the role of diet, eating behaviors, demographics and environmental factors in contributing to increased caries rates in children is essential in order to improve the oral component of general health.4 In particular, an established relationship has been reported linking malnutrition in children, inappropriate infant feeding practices and excessive intakes of sugar to ECC.4,5
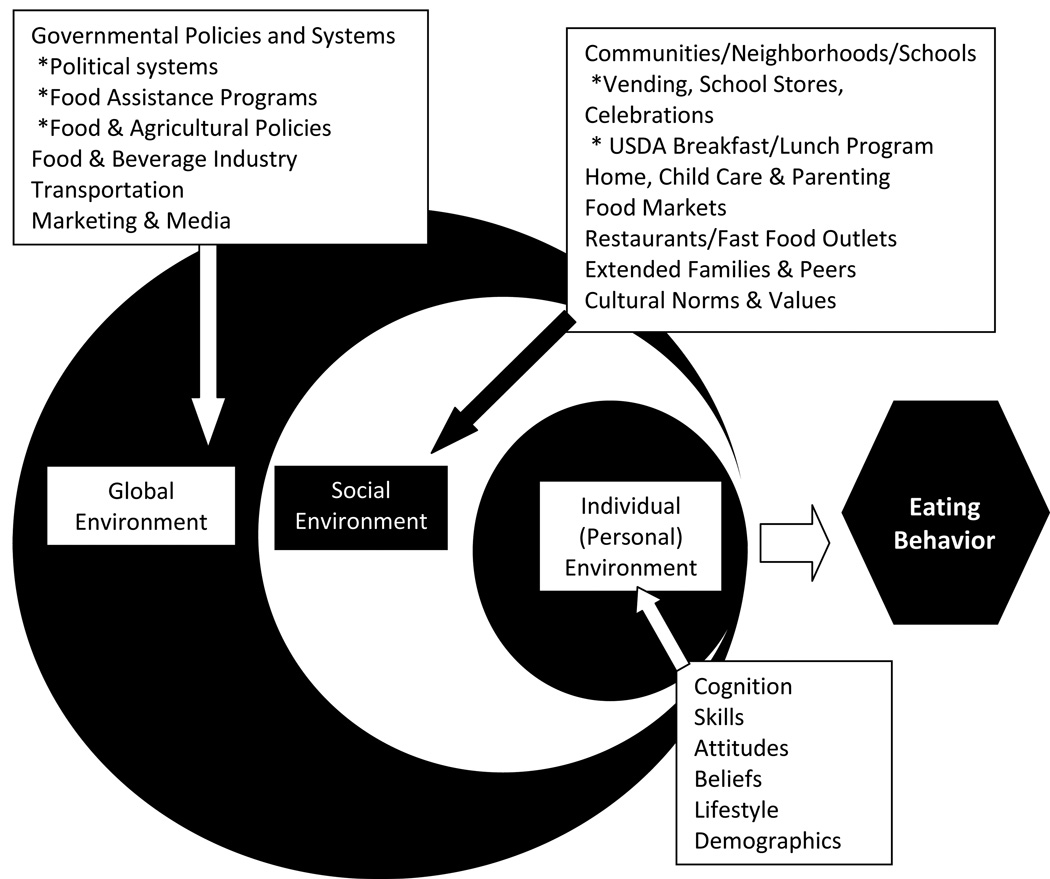
The association of dental caries to excessive sugar intake has been affirmed by an Expert Panel of the World Health Organization (WHO), whose members reviewed the strength of evidence linking dietary factors to caries in 2003. The Panel reported an increased risk of caries associated with frequent and total intake of free, simple sugars.6 Reports in the US noted total and individual intakes of free, simple sugars were not associated with caries experience in young Iowa children suggesting that current simple sugar intakes exceeds the caries threshold or that caries is influenced more by frequency and other factors.7 The WHO Expert Panel also reported a decreased risk of caries related to consumption of specifically hard cheeses and use of sugar-free chewing gum. Evidence was insufficient to support associations with intake of dried or whole fresh fruit, milk, dietary fiber, xylitol, or cooked or raw starches.6 However, the paucity of longitudinal studies to support the role of nutrient and food components in caries risk or progression noted by the panel as a limitation in determining the specific role of a spectrum of foods and nutrients remains unchanged.8 Additionally, there is no significant published data linking diet to disparities in caries, a diet-dependent infectious disease. Dietary factors and food choices are determinants of a number of chronic diseases, including dental caries.9,10 Multiple influential environmental, social and personal factors associated with eating behaviors are listed in Figure 1.11,12 A spectrum of dynamic, synergistic conditions in the global environment including political and industry systems and policies interact with regional and community programs and cultures to create environments that determine availability and access to food choices. In this context and based on knowledge and individual experiences, beliefs and skills personal eating behaviors are determined. This review examines dimensions of this social-ecological model relevant to ECC.
Figure 1.
An Ecological Model Identifying Factors Influencing Eating Behaviors
Malnutrition and Food Insecurity
Malnutrition results from adverse changes in dietary intake, digestive and metabolic malfunctions, or the excretion of essential metabolically required nutrients.13 Undernutrition -an insufficient intake of nutrients, overnutrition --an intake beyond required needs, and nutrient imbalances--are all forms of malnutrition.13 Overnutrition is commonly associated with the substitution of low-cost, low nutrient-dense foods such as snacks that contain excessive quantities of sugar, salt, and fat for lower energy, high nutrient-dense foods such as fruits.14 Analysis of data from NHANES III (1988–1994) indicates that 8- to 18-year old Americans who reported consuming excessive numbers of low nutrient-dense foods are more likely to report less than estimated average daily requirements of nutrients essential for optimum health.15 Dietary quality data expressed in the Healthy Eating Index (HEI) from the same source for 2 to 5 year old children indicates those with the best dietary practices are 44% less likely to exhibit severe ECC compared to children with the worst practices.16 Increased consumption of sugar sweetened beverages, candy, chips, and cookies provides excessive calories to the child, increases the risk of caries, and when combined with inadequate intake of fruits and vegetables, deprives the child of nutrients essential to growth and development.17 Thus, low nutrient-dense food problem is ubiquitous and largely responsible for many chronic health problems in both developing nations and developed parts of the world experiencing increasing immigration.14,18
Food insecurity, defined as a lack of adequate quantities of safe foods to meet nutritional requirements at some time during the year, is increasingly recognized as an environmental link between hunger, lack of adequate food resources, patient behaviors, including compliance, and disease risk. Food insecurity is pronounced in both rural and urban communities, among the poor and in female-headed households19 and is associated with developmental risk. In Ohio 20.6 percent of participants in supplemental Nutrition Programs for Women, Infants, and Children (WIC) lived in food insecure households. Young children in Mexican immigrant families in the US are also reported to be at high risk for hunger and household food insecurity.20
Dietary Guidance and Food Assistance Programs
Since 1977 the federal government has established and has periodically reviewed and updated United States Dietary Guidelines supporting nutrition and health and physiological requirements for maintaining an adequate nutritional status. The current 2005 version including toolkits and the HEI dietary assessment tool are accessible on government websites for all health professionals to aid in diet planning and counseling in clinical, community, and private practice settings.21 Frequency of intake is not addressed in these resources, however, and should be included in interventions designed to address total dietary intake and advance oral health. Food assistance programs such as WIC, Head Start Programs, and the United States Department of Agriculture (USDA) Food and Nutrition Services that include School Meals Programs (lunch, breakfast and after-school) are designed to improve access to healthy food and beverage options for infants and children. Dental providers in collaboration with other health professionals and organizations, including the American Dietetic Association, serve as advisers to Head Start and other childcare programs to influence policies and to provide nutritional guidance.22 Participation in these programs is available to children and families at no cost based on family income.
Schools are an important source of food in children’s diets. For example, fruit and vegetable consumption among school children has been correlated with the availability of these foods in school lunch programs.23 A 2008 study of the quality of diets of children participating in school lunch programs reported the diets to be nutritious, but cautioned policy makers about the increased prevalence of high sodium, high saturated fat intakes among some low income participants.24 Many after-school programs receive food aid because they serve disadvantaged and minority youth. The U.S. government supports these programs through the After School Snack Program and the Summer Food Service.25 However, little is known about the quality of these programs and what impact they may have on oral health disparities related to diet.
Global Influences on Dietary Choices
What people eat is affected by many complex variables including socioeconomic status, the cost of food, the industrialization of agriculture, the location of food outlets, and the effects of advertising and marketing. Industrialization of agriculture has impacted food markets and led to an increased availability of more processed, shelf-stable foods throughout the country. The use of high fructose corn syrup (HFCS) and other starch by-products (e.g., maltodextrin, modified starches) has resulted in an increased availability and consumption of sweetened beverages and a variety of dessert type snacks.26 Individual packaging and increased market outlets ensure that cariogenic foods and beverages are readily available at most children’s venues – the ballpark, playgrounds, movies, and school. The poor and the disadvantaged have been described as being disproportionately affected by diet-related diseases, such as caries, and advocates suggest they could benefit from government intervention to decrease availability of sweetened beverages by imposing a tax on such foods.26 Unfortunately, this would not by itself address the need for diet and nutrition education to choose and access healthful, affordable and appropriate foods that could be substituted for sweetened beverages and would support health, including oral health.27
Food cost has a strong influence on food purchases. When women of low and high incomes were given additional funds to purchase foods, women of low income added healthier choices and those with high incomes added less healthy choices.29 Education addressing strategies to improve nutrient quality while managing food cost is needed.
Aggressive food marketing on television, radio, and the Internet contributes to health and caries disparities. In-school product marketing and sales promotion of high-fat snacks and carbonated, sweetened beverages have been a growing concern.30 Child-and youth-targeted media publish ads for candy, snacks, sugared cereals, and fast food.31 Children and youth were reported to have received approximately one-third or more of their calories from foods purchased outside of the home, at restaurants and quick serve restaurants that contain higher fat content than food consumed at home.31 Government policies in the form of sugar and corn subsidies may help to reduce costs of some of these foods making such snacks more affordable. However, there is no documented evidence to suggest that inexpensive low-nutrient dense food production is overtly supported by government subsidized commodity foods.32
Experts believe the snack ads will soon extend to messages on cell phones, instant messaging, and video games. Parents may be largely unaware of the extent of this advertising or its impact. While some countries ban television advertising of certain products from periods when children are most likely to view these items, they permit ads for foods that are most associated with oral health disparities.33 For example, they may avoid promoting high-fat snacks associated with risk for obesity replacing them with low-fat, high sugary snack food ads that promote caries risk. Promoting sweetened fruit drinks at home, school, and in the market by simply using 100 percent juice in small portion controlled boxes as a replacement does not change the potential caries risk.34
Parenting Practices
The first years of life mark a time of rapid development and dietary change, as children transition from an exclusive milk diet to a modified adult diet. Human milk has been identified as the ideal food for infants and is recommended throughout the first year of life. And while human milk contains sugar, an analysis of a subset of children between 2 and 5 years of age from the NHANES 1999–2004 survey concluded that there was no evidence that breastfeeding or its duration per se were independently associated with an increased risk for ECC. However, children living in poverty, Mexican American children and those exposed to maternal smoking behaviors were at increased risk for poor oral health in the early years.35 Other investigators have confirmed these findings, and have identified milk-bottle feeding at night (in which the sweetened liquid remains in contact with the developing dentition) as the most significant determinant of ECC.36,37
During the transition to solid foods, parents are the major influence on what children eat and like, the quality of their diet, and weight status.38 The strongest factors associated with healthy eating behaviors at home are availability and accessibility of nutritious food.39 As role models, parents can encourage eating fruits and vegetables by regularly serving them at meals and eating them themselves. On the other hand, parents can also encourage the habitual consumption of cheap, highly palatable, energy dense foods, such as sweetened beverages and snacks, leading to caries, overeating and weight gain. To counter these patterns, parents need guidance regarding food choices and relative cost to nutrient ratio.38 Structured meal and snacking patterns, allowing for one to three daily snacks, are desirable as opposed to free access to 100 percent juice, other sugared beverages and snacks over the course of the day. Such behaviors favor the intake of nutrient-poor foods and increase the risk of obesity and dental caries.40,41 The American Academy of Pediatric Dentistry’s policy on dietary recommendations to decrease caries risk for infants, children and adolescents supports the adoption of a diverse and balanced diet based on US Dietary Guidelines.42
Cultural and Socioeconomic Norms
Within families, traditional cultural norms as well as socioeconomic (SES) status help to shape attitudes towards body weight and eating behaviors associated with ECC. A survey of female adolescents found girls of higher SES were more aware of America’s idealizing of slimness and had more family and friends trying to lose weight. They also defined a lower body mass index as “fat” than did low SES adolescents and differed in their food choices.43 In terms of food selection, Barker and colleagues found that lower educational attainment was associated with less fruit and vegetable consumption compared to high fat sugary foods that are often associated with caries risk.44 Other studies have shown that many low-income mothers viewed an infant who is large for his/her age as healthy, in contrast to health professionals who found that same infant to be overweight.45,46 To increase an infant’s weight, low-income mothers may add cereal to formula or feed the baby more frequently, establishing future eating patterns. Mothers may also misinterpret signs of distress as signs of hunger. Food and beverages provided on a regular, frequent and continuous basis, increase risk of both ECC and obesity.6,44 Marshall et al. reported that caries and obesity coexist in young children of low SES, and that both mother’s education- and soda intake were closely associated with caries experience.47
Carnell and colleagues found that across all income levels, parents of 3-to 5-year-old children generally show poor awareness of their child’s weight status and often fail to recognize overweight.48 Lack of awareness and corollary eating behaviors likely contributes to unhealthy pressure to eat more frequently, sustaining oral bacterial caries promoting activity. High intake of unhealthy snack foods and low intake of fruits and vegetables have both been linked to high parental pressure to eat. This parenting style is commonly observed among male, non-white parents and parents of younger children.49 In contrast, covert control of children’s diets (keeping unhealthy foods out of the home and avoiding fast food restaurants) is associated with healthy child nutrition practices associated with appropriate growth, development and decreased caries risk. Such covert control of a child’s diet is positively associated with parental level of education.49 Some parental control methods, such as using foods as a reward or tightly restricting sweets, may backfire, however, creating the unintended consequence of children eating more unhealthful sweets.50 Parents can increase children’s acceptance of new and appropriate foods by providing frequent exposure to them in the home.51 This may require eight or more presentations of a new healthy food (such as sweet red pepper or tofu) to increase children’s acceptance.
Ethnicity is associated with differences in food-related beliefs, preferences, and behaviors. The interaction between ethnicity and environments with lower than average neighborhood availability of healthful foods and higher than average availability of fast food restaurants, along with exposure to ethnically targeted food marketing may contribute to reliance on high calorie, low-nutrient dense foods and beverages.52 Ethnic differences in food choices and inappropriate child feeding practices may increase risks of malnutrition during gestation, infancy, childhood and adolescence and manifest nutrient deficiencies in altered tooth morphology and eruption patterns.18 Alternatively, ethnic food choices may include increased access to desirable diets rich in fruit and vegetables. Acculturation may be negatively affecting the dietary quality of Latinos from Latin American who come to the US. They are disproportionately affected by disparities including low educational attainment, poverty, food insecurity, increased health risk (i.e. ECC) and neighborhoods with major barriers preventing healthful practices including proper nutrition.53
The Neighborhood
Where people live influences their ability to acquire adequate supplies of healthy foods, and may present particular problems for low SES and ethnic populations. In both rural and urban communities, convenience stores offering high energy, low nutrient dense foods are more common than full supermarkets offering a wide variety of fruits and vegetables and other healthy foods.54,55,56 In one rural South Carolina county of 91,582 people covering 1,106 square miles, there were 1.1 supermarkets, 0.7 grocery stores and 5.2 convenience stores per 100 square miles.54 Greater access to convenience stores would suggest inadequate access to a variety of foods. In the entire state, 52 percent of children in the third grade had experienced caries and 33 percent went untreated, compared to national data of fifty and twenty-six percent, respectively.57 An association between access to markets, rural disparities and the oral health components of general health is supported by these data.
Dependence on reliable cars and the price of gas may also limit access to supermarkets and larger grocery stores for individuals living in rural communities. Within inner cities, the type of food store available also differs by racial groups. In predominantly African American census blocks in East Harlem there were no supermarkets or grocery stores, while Latino census blocks had more specialty food and convenience stores than racially mixed census blocks.55
Community-based organizations have attempted to provide access to healthy foods through advocacy campaigns and policy changes. The Pennsylvania Fresh Food Financing Initiative, the nation’s first statewide program to increase supermarket development in underserved areas, is one example of grass root attempts to provide the underserved and those with limited incomes access to affordable fresh food from retailers who offer greater variety that potentially contributes to a nutritionally balanced diet.58
Countervailing Forces
Two forces increasingly evident in American society are working to change America’s dietary habits. One is the widespread recognition of the epidemic of obesity that is affecting children and adolescents as well as adults.14 Americans have come to realize that fast food chains are major contributors to excessive calories and in response the chains themselves are moderating selections to include more healthy choices. Also of significance is a growing emphasis on the role of nutrition and diet in health promotion and disease prevention. Availability of unprocessed fresh foods, fortified processed foods, and the management of the food supply system require health literacy messages that address the significance of food and dietary practices in general and oral health. How these trends will play out and whether or not they will have an effect in all neighborhoods is unknown, but deserves attention in meeting the needs of children.
Recommendations
Addressing the role of dietary factors in decreasing caries disparity in children requires a comprehensive perspective and consideration of the multiple, constantly changing variables that affect eating behaviors and health status. (See Fig. 1.) Closing the gap among racial, ethnic and demographic minorities who experience higher rates of diseases compared with those who have access to education and health care can begin with education but will require government and community action as well. The measures needed require the actions of multiple partners: health care providers (pediatricians, other physicians, dentists, dietitians and allied health professionals), local community leaders, legislators, government agencies, educators, the media, industry, and other concerned individuals and organizations. Necessary elements in programs to improve children’s oral and general health include:
1. Dietary Counsel
Health professionals and others as appropriate need to counsel parents, other caretakers and children to moderate sugar, salt and fat intake to achieve adequate growth and development and adhere to high-quality diets, following dietary guidelines using MyPyramid resources provided by USDA.21,40 Counsel should include the role of frequency of consumption of sugary food and beverage and why frequency can increase caries risk. Support for inclusion of nutrition education and skill development in health literacy for future dental professionals and continuing education for practicing dentists can enhance practices in this area.22 Registered dietitians can guide practices and provide consultation to health professionals and the public and develop skills in addressing the oral components of general health.
2. Advocacy
Health professionals and allies should organize, lead and work with local community, state and national organizations to improve access necessary for a healthful diet, including, for example, the promotion of legislation to provide incentives for establishing well-stocked supermarkets and grocery stores in poor neighborhoods. Support for changes in dental professionals’ academic training and continuing education requirements should include skill development in diet promotion and counseling in support of oral components of general health. Representation of local, regional and state boards involved in improving environments that support healthy communities, schools and families should be sought and leadership should be achieved.
3. Advice to Mothers
Educational protocols need to be established to advise pregnant women on diets and provide guidance on infant feeding, emphasizing the value of breast feeding and the necessity of restricting night-time bottle feeding to decrease caries risk. Acknowledgment of ethnic/cultural practices that reflect appropriate eating behaviors in support of oral components of general health should include tailored messages to address unique neighborhood environments.
4. Guidance on Home Eating Patterns
Parents should be advised that they are role models able to set eating behaviors at home by providing high-quality meals and having fruits and vegetables and other healthy foods available as snacks. Advice should include discouraging frequent consumption of high-fat, high-sugar foods and the realization that acceptance of new foods may require repeated presentations of the food. Community resources to assist families in developing skills in purchasing, and preparing healthy food and meals should be included in dental patient education.
5. Cultural/ethnic Sensitivity
Family demographics, cultural/ethnic practices and food-related environmental issues should be routinely taken into consideration in order to tailor education and counseling to the unique needs of a family.
6. Skilled Health Care Providers
Multidisciplinary teams including dental professionals, pediatricians, nurses, registered dietitians, family practice physicians and other allied health care professionals should be educated and trained to screen, educate, and counsel children and families to access care and seek medical and dental homes with active health promotion programs that include diet, nutrition and dental education resources. Awareness of the obesity and caries association among primary care providers can lead to early interventions and improved health status for all children.
Contributor Information
Connie Mobley, Professor of Nutrition & Associate Dean of Research University of Nevada Las Vegas School of Dental Medicine 1001 Shadow Lane, MS 7410 Las Vegas, NV 89106-4124
Teresa A. Marshall, University of Iowa College of Dentistry Department of Preventive and Community Dentistry 329 DSB N Iowa City, IA 522242-1010
Peter Milgrom, Northwest/Alaska Center to Reduce Oral Health Disparities Box 357475, University of Washington, Seattle, WA 98195-7475.
Susan E. Coldwell, Department of Dental Public Health Sciences Box 357475, University of Washington, Seattle, WA 98195-7475.
References
- 1.US Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General--Executive Summary. Rockville, MD: US Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000. [Google Scholar]
- 2.Dye BA, Tan S, Smith V, Lewis BG, Barker LK, Thoronton-Evans G, et al. Trends in oral health status: United States, 1988–1994 and 1999–2004. National Center for Health Statistics. Vital Health Statistics. 2007;11:248. [PubMed] [Google Scholar]
- 3.Tomar S, Reeves AF. Changes in the state of oral health of U.S. children and adolescents since the release of the Surgeon General’s Report on Oral Health. Academic Pediatrics. 2009;9(6) doi: 10.1016/j.acap.2009.09.018. XX. [DOI] [PubMed] [Google Scholar]
- 4.Roberts MW. Dental health of children: where we are today and remaining challenges. J Clin Pediatr Dent. 2008;32(3):231–234. doi: 10.17796/jcpd.32.3.d5180888m8gmm282. [DOI] [PubMed] [Google Scholar]
- 5.Patrick DL, Lee RSY, Nuci M, Grembowski D, Jolles CZ, Milgrom P. Reducing oral health disparities: a focus on social and cultural determinants. [Accessed on June 22 2009];BMC Oral Health. 2006 6(Suppl 1) doi: 10.1186/1472-6831-6-S1-S4. Available at http://creativecommons.org/licenses/by/2.0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The World Health Organization. The World Oral Health Report 2003. Geneva: World Health Organization; 2003. [Google Scholar]
- 7.Marshall TA, Eichenberger-Gilmore JM, Larson MA, Warren JJ, Levy SM. Comparison of the intakes of sugars in young children with and without dental caries experience. J Am Dent Assoc. 2007;138:39–46. doi: 10.14219/jada.archive.2007.0019. [DOI] [PubMed] [Google Scholar]
- 8.Moynihan P, Petersen PE. Diet, nutrition and the prevention of dental diseases. Public Health Nutr. 2003;7:201–226. doi: 10.1079/phn2003589. [DOI] [PubMed] [Google Scholar]
- 9.Cappelli DP, Mobley CC. Prevention in clinical oral health care. St. Louis, MO: Mosby Elsevier; 2008. [Google Scholar]
- 10.Kant AK, Graubard BI, Schatzkin A. Dietary patterns predict mortality in a national cohort: the National Health Interview Surveys, 1987 and 1992. J Nutr. 2004;134:1793–1799. doi: 10.1093/jn/134.7.1793. [DOI] [PubMed] [Google Scholar]
- 11.Beydoun MA, Wang Y. How do socio-economic status, perceived economic barriers, and nutritional benefits affect quality of dietary intake among US adults? Eur J Clin Nutr. 2008;62:303–313. doi: 10.1038/sj.ejcn.1602700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sheiham A. Oral health, general health and quality of life. Bull World Health Organ. 2005;83(9):644–645. [PMC free article] [PubMed] [Google Scholar]
- 13.Shils ME, Shike M, Ross AC, et al. Modern nutrition in health and disease. 10th Edition. Philadelphia, PA: Lippincott, Williams & Wilkins; 2006. [Google Scholar]
- 14.Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public health crisis, common sense cure. Lancet. 2002;360:473–482. doi: 10.1016/S0140-6736(02)09678-2. [DOI] [PubMed] [Google Scholar]
- 15.Kant AK. Reported consumption of low-nutrient-density foods by American children and adolescents. Arch Pediatr Adolesc Med. 2003;157:789–796. doi: 10.1001/archpedi.157.8.789. [DOI] [PubMed] [Google Scholar]
- 16.Nunn ME, Braunstein NS, Krall KEA, Dietrich T, Gracia RI, Henshaw MM. Healthy eating index is a predictor of early childhood caries. J Dent Res. 2009;88(4):361–366. doi: 10.1177/0022034509334043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ballew C, Kuester S, Gillespie C. Beverage choices affect adequacy of children’s nutrient intakes. Arch Pediatr Adolesc Med. 2000;154:1148–1152. doi: 10.1001/archpedi.154.11.1148. [DOI] [PubMed] [Google Scholar]
- 18.Oliveira AFB, Chaves AMB, Rosenblatt A. The influence of enamel defects on the development of early childhood caries in a population with low socioeconomic status: a longitudinal study. Caries Res. 2006;40:296–302. doi: 10.1159/000093188. [DOI] [PubMed] [Google Scholar]
- 19.Kropf ML, Holben DH, Holcomb JP, Anderson H. Food security status and produce intake and behaviors of Special Supplemental nutrition Program for Women, Infants, and Children and Farmers’market Nutrition program participants. J Am Diet Assoc. 2007;107:1903–1908. doi: 10.1016/j.jada.2007.08.014. [DOI] [PubMed] [Google Scholar]
- 20.Kersey M, Geppert J, Cutts DB. Hunger in young children of Mexican immigrant families. Public Health Nutr. 2007;10(4):390–395. doi: 10.1017/S1368980007334071. [DOI] [PubMed] [Google Scholar]
- 21.U.S. Department of Health and Human Services and U.S. Department of Agriculture. [Accessed on June 15, 2009];Washington, DC: U.S. Government Priniting Office; Dietary Guidelines for Americans, 2005. (6th Edition). 2005 January; Available at http://www.health.gov/DietaryGuidelines/.
- 22.Touger-Decker R, Mobley CC. Position paper of the American Dietetic Association: Oral health and nutrition. J Am Diet Assoc. 2007;103:615–625. doi: 10.1053/jada.2003.50130. [DOI] [PubMed] [Google Scholar]
- 23.Glanz K, Sallis JF, Saelens BE, Frank LD. Healthy nutrition environments: concepts and measures. Am J Health Promot. 2005;19(5):330–333. doi: 10.4278/0890-1171-19.5.330. [DOI] [PubMed] [Google Scholar]
- 24.USDA Food and Nutrition Service. Diet quality of American school aged children by school lunch participation status. Data from the national nutrition and health examination survey. 2008 July [Google Scholar]
- 25. [Accessed on June 22, 2009];National School Meals Programs. 2009 Available at http://www.fns.usda.gov/cnd/.
- 26. [Accessed on August 28, 2008];High Fructose Corn Syrup Usage May be Leveling Off. AmberWaves. 2008 Feb; Available at: http://www.ers.usda.gov/AmberWaves/February08/Findings/HighFructose.htm.
- 27.Brownell KD, Frieden TR. Ounces of prevention-the public policy case for taxes of sugared beverages. N Engl J Med. 2009;18:1805–1808. doi: 10.1056/NEJMp0902392. [DOI] [PubMed] [Google Scholar]
- 28.Inglis V, Ball K, Crawford D. Does modifying the household food budget predict changes in the healthfulness of purchasing choices among low- and high-income women. Appetite. 2009;52(2):273–279. doi: 10.1016/j.appet.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 29.Drewnowski A, Darmon N. Food choices and diet costs: an economic analysis. J of Nutr. 2005;135:900–904. doi: 10.1093/jn/135.4.900. [DOI] [PubMed] [Google Scholar]
- 30.French SA, Story M, Fulkerson JA, Geriach AF. Food environment in secondary schools: a la carte, vending machines, and food policies and practices. Am J of Public Health. 2003;93(7):1161–1167. doi: 10.2105/ajph.93.7.1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McGinnis JM, Gootman JA, Kraak VI, editors. Food Marketing to Children and Youth: Threat or Opportunity? Washington DC: National Academies Press, Institute of Medicine; 2006. [Google Scholar]
- 32.Miller JC, Coble K. Cheap food policy: fact or rhetoric? Food Policy. 2007;32:98–111. [Google Scholar]
- 33.Hawkes C. Marketing food to children: the global regulatory environment. Geneva: World Health Organization; 2004. [Google Scholar]
- 34.Rodd HD, Patel V. Content analysis of children’s television advertising in relation to dental health. Br Dent J. 2005;199(11):710–712. doi: 10.1038/sj.bdj.4812967. [DOI] [PubMed] [Google Scholar]
- 35.Hiroko I, Auinger P, Billings RJ, Weitzman M. Association between infant breastfeeding and early childhood caries in the United States. Pediatrics. 2007;120:e944–e952. doi: 10.1542/peds.2006-0124. [DOI] [PubMed] [Google Scholar]
- 36.Mohebbi SZ, Virtanen JI, Vahid-Golpayegani M, Vehkalahti MM. Feeding habits as determinants of early childhood caries in a population where prolonged breastfeeding is the norm. Community Dent Oral Epidemiol. 2008;36:363–369. doi: 10.1111/j.1600-0528.2007.00408.x. [DOI] [PubMed] [Google Scholar]
- 37.Kramer MS, Vanilovich L, Matush L, Bogdanovich N, Zhang X, Shishko G, Muller-Bolla M, Platt RW. The effect of prolonged and exclusive breast-feeding on dental caries in early school-age children. Caries Res. 2007;41:484–488. doi: 10.1159/000108596. [DOI] [PubMed] [Google Scholar]
- 38.Savage JS, Fisher JO, Birch LL. Parental influence on eating behavior: conception to adolescence. J of Law, Medicine & Ethics. 2007;35(1):22–34. doi: 10.1111/j.1748-720X.2007.00111.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cullen KW, Baranowski T, Owens E, Marsh T, Rittenberry L, et al. Availability, accessibility, and preferences for fruit, 100% fruit juice, and vegetables influence children’s dietary behavior. Health Educ Behav. 2003;30(5):615–626. doi: 10.1177/1090198103257254. [DOI] [PubMed] [Google Scholar]
- 40.Marshall TA, Broffitt B, Eichenberger-Gilmore JM, Warren JJ, Cunningham MA, Levy SM. The roles of meal, snack and daily total food and beverage exposures on caries experience in young children. J Pub Health Dent. 2005;65(3):166–173. doi: 10.1111/j.1752-7325.2005.tb02807.x. [DOI] [PubMed] [Google Scholar]
- 41.Dubois L, Girard M, Ptovin KM, Farmer A, Tatone-tokida F. Breakfast skipping is associated with differences in meal patterns, macronutrient intakes and overweight among preschool children. Public Health Nutr. 2008;18:1–10. doi: 10.1017/S1368980008001894. [DOI] [PubMed] [Google Scholar]
- 42.Clinical Affairs Committee. Policy on Dietary Recommndatrions for Infants, Children and Adolescents. American Academy of Pediatrics. 2008 [Google Scholar]
- 43.Wardle J, Robb KA, Johnson F, Griffith J, Brunner E, Power C, Tovee M. Socioeconomic variation in attitudes to eating and weight in female adolescents. Health Psychol. 2004;23(3):275–282. doi: 10.1037/0278-6133.23.3.275. [DOI] [PubMed] [Google Scholar]
- 44.Barker M, Lawrence W, Woadden J, et al. Women of lower educational attainment have lower food involvement and eat less fruit and vegetables. Appetite. 2008;50:464–468. doi: 10.1016/j.appet.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 45.Baughcum AE, Burklow KA, Deeks CM, et al. Maternal feeding practices and childhood obesity: A focus group study of low-income mothers. Arch Pediatr Adolesc Med. 1998;152(10):1010–1014. doi: 10.1001/archpedi.152.10.1010. [DOI] [PubMed] [Google Scholar]
- 46.Bentley M, Gavin L, Black MM, et al. Infant feeding practices of low-income, African-American adolescent mothers: an ecological, multigenerational perspective. Soc Sci Med. 1999;49:1085–1100. doi: 10.1016/s0277-9536(99)00198-7. [DOI] [PubMed] [Google Scholar]
- 47.Marshall TA, Eichenberger-Gilmore JM, Broffitt B, Warren JJ, Levy SM. Dental caries and childhood obesity: roles of diet and socio-economic status. Community Dent Oral Epidemiol. 2007;35:449–458. doi: 10.1111/j.1600-0528.2006.00353.x. [DOI] [PubMed] [Google Scholar]
- 48.Carnell S, Edwards C, Croker H, et al. Parental perceptions of overweight in 3–5 y olds. Int J Obes. 2005;29(4):353–355. doi: 10.1038/sj.ijo.0802889. [DOI] [PubMed] [Google Scholar]
- 49.Brown KA, Ogden J, Vogele C, et al. The role of parental control practices in explaining children’s diet and BMI. Appetite. 2007;50:252–259. doi: 10.1016/j.appet.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 50.Birch L. Development of food preferences. Annu Rev Nutr. 1999;19:41–62. doi: 10.1146/annurev.nutr.19.1.41. [DOI] [PubMed] [Google Scholar]
- 51.Cooke L. The importance of exposure for healthy eating in childhood: a review. J Hum Nutr Diet. 2008;2:294–301. doi: 10.1111/j.1365-277X.2007.00804.x. [DOI] [PubMed] [Google Scholar]
- 52.Kumanyika SK. Environmental influences on childhood obesity: ethnic and cultural influencs in context. Physiol Behav. 2007;94(1):61–70. doi: 10.1016/j.physbeh.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 53.Perez-Escamilla R. Dietary quality among Latinos: is acculturation making us sick? J Am Diet Assoc. 2009;109(6):988–991. doi: 10.1016/j.jada.2009.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liese AD, Weis KE, Pluto D, Smith E, Lawson A. Food store types, availability, and cost of foods in a rural environment. J Am Diet Assoc. 2007;107(11):1916–1923. doi: 10.1016/j.jada.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 55.Galvez MP, Morland K, Raines C, Kobil J, Siskind J, Godbold J, Brenner B. Race and food store availability in an inner city neighbourhood. Public Health Nutr. 2008;11(6):624–631. doi: 10.1017/S1368980007001097. [DOI] [PubMed] [Google Scholar]
- 56.Sharkey JR, Horel S. Neighborhood socioeconomic deprivation and minority composition are associated with better potential spatial access to the grounded food environment in a large rural area. J Nutr. 2008;138(3):620–627. doi: 10.1093/jn/138.3.620. [DOI] [PubMed] [Google Scholar]
- 57.Carlson V, Veschucio . The Burden of Oral Diseases in South Carolina. Columbia, SC: South Carolina Department of Health and environmental Control; 2006. [Google Scholar]
- 58.Giang T, Karpyn A, Laurison HB, Hillier A, Perry RD. Closing the grocery gap in underserved communities: the creation of the Pennsylvania Fresh Food Financing Initiative. J Public Health Manag Pract. 2008;14(3):272–279. doi: 10.1097/01.PHH.0000316486.57512.bf. [DOI] [PubMed] [Google Scholar]