Abstract
Background
Although many studies have been focused on interventions designed to promote mammography screening among ethnic minority women, few summaries of the effectiveness of the interventions are available.
Objective
The aim of this study was to determine the effectiveness of the interventions for improving mammography screening among asymptomatic ethnic minority women.
Methods
A meta-analysis was performed on intervention studies designed to promote mammography use in samples of ethnic minority women. Random-effects estimates were calculated for interventions by measuring differences in intervention and control group screening rates postintervention.
Results
The overall mean weighted effect size for the 23 studies was 0.078 (Z = 4.414, p < .001), indicating that the interventions were effective in improving mammography use among ethnic minority women. For mammography intervention types, access-enhancing strategies had the biggest mean weighted effect size of 0.155 (Z = 4.488, p < .001), followed by 0.099 (Z = 6.552, p < .001) for individually directed approaches such as individual counseling or education. Tailored, theory-based interventions resulted in a bigger effect size compared with nontailored interventions (effect sizes = 0.101 vs. 0.076, respectively; p < .05 for all models). Of cultural strategies, ethnically matched intervention deliveries and offering culturally matched intervention materials had effect sizes of 0.067 (Z = 2.516, p = .012) and 0.051 (Z = 2.365, p = .018), respectively.
Discussion
Uniform improvement in mammography screening is a goal to address breast cancer disparities in ethnic minority communities in this country. The results of this meta-analysis suggest a need for increased use of a theory-based, tailored approach with enhancement of access.
Keywords: ethnic minority women, mammography, meta-analysis
Despite considerable progress in breast cancer control in the United States over the past 20 years, ethnic minority women continue to face an unequal burden of cancer (Chu, Miller, & Springfield, 2007; Lantz et al., 2006). For example, African American and Hispanic women are more likely to be diagnosed at an advanced stage of breast cancer (American Cancer Society, 2008; Lantz et al., 2006) and have worse stage-for-stage survival than do White women (Carey et al., 2006; Shavers, Harlan, & Stevens, 2003). Traditionally, Asian American women have had lower breast cancer incidence rates than White women had (American Cancer Society, 2008). Over the past decade, however, the incidence of breast cancer in Asian women has been increasing at a much higher rate than that of White women (annual increase of 6.3% vs. <1.5%; Deapen, Liu, Perkins, Bernstein, & Ross, 2002). In addition, similar to Black and Hispanic women, Asian American women are significantly more likely than White women to discover breast cancer at a later stage (Miller, Hankey, & Thomas, 2002).
Researchers have ascribed a large portion of this disparity in the late-stage diagnosis and poor survival of breast cancer to racial and ethnic differences in the utilization of mammography screening, which is a critical strategy in early detection and timely treatment of breast cancer (Smith-Bindman et al., 2006). The U.S. Preventive Services Task Force (2002) recommends that women have a mammogram every 1–2 years beginning at age 40 years. Although differences in mammography rates between White and African American women have narrowed during the past decade (Smigal et al., 2006), ethnic differences in screening do persist in some groups. The American Cancer Society’s most recent annual report of cancer statistics revealed that regular use of mammography was especially low among Hispanic and Asian women relative to the national level (Cokkinides, Bandi, Siegel, Ward, & Thun, 2007). According to a recent report on national surveys (Town, Wholey, Feldman, & Burns, 2007), ethnic minority women are less likely than their White counterparts to have health insurance (69.7% vs. 87%). Minority women who lack health insurance or have lived in the United States for less than 10 years have been found particularly vulnerable to insufficient mammography screening (Cokkinides et al., 2007; Purc-Stephenson & Gorey, 2008; Rakowski et al., 2006).
Many studies have been focused on promoting mammography screening among ethnic minority women using a variety of intervention strategies. For example, promotora (lay health advisor) interventions have been generally well received by ethnic minority women, positively affecting their use of preventive health services, including mammography (Erwin et al., 2003; Mock et al., 2007; Navarro et al., 1998; Taylor et al., 2002). Without a sufficient amount of monitoring, support, and opportunities for advancement, however, the utility of the promotora approach is uncertain because the content and frequency of interactions between the promotora and the study participant may change by the discretion of the promotora (Suarez et al., 1997; Wasserman, Bender, & Lee, 2007). Well-validated theories can be used to guide an intervention effectively by specifying the ingredients and correct implementation of the intervention, making replication of the intervention easier (Sidani & Braden, 1998). Theory-guided tailored interventions (i.e., providing intervention materials adjusted to the characteristics of an individual) have been effective in promoting various forms of health behavior such as healthy diet (Park et al., 2008; Resnicow et al., 2008) and smoking cessation (Schumann et al., 2008). Likewise, recent strategies to promote breast cancer screening include theory-based tailored interventions (Allen & Bazargan-Hejazi, 2005; Champion et al., 2006, 2007; Jibaja-Weiss, Volk, Kingery, Smith, & Holcomb, 2003), although no systematic evaluation of this intervention approach across studies has been done.
The purpose of this meta-analysis was to determine the effects of intervention programs on mammography screening among ethnic minority women. Identification of the determinants of mammography use can facilitate more effective strategies to reduce barriers to breast cancer screening. Meta-analyses of mammography interventions (Denhaerynck et al., 2003; Edwards et al., 2006; Legler et al., 2002; Sohl & Moyer, 2007; Yabroff & Mandelblatt, 1999) found that combined approaches enhancing access—in addition to individual strategies such as reminder letters, telephone calls, or personal contact—can increase mammography use. Specifically, in the Legler et al. (2002) meta-analysis, access-enhancing strategies were the strongest intervention approach, resulting in an increase in mammography use by 18.9% (95% confidence interval [CI] = 10.4–27.4), followed by individually directed interventions in a healthcare setting (17.6%; 95% CI = 11.6–24.0). Yabroff and Mandelblatt (1999) included two studies that used access-enhancing strategies (financial incentives) in their meta-analysis but did not perform meta-analysis with two interventions. They found that patient-targeted behavioral interventions improved mammography utilization by 13.2% (95% CI = 4.7–21.2). Effect sizes of interventions using social networks were revealed to be in the range of 5.8% (Legler et al., 2002) to 12.6% (Yabroff & Mandelblatt, 1999).
However, most previous meta-analyses have not been focused specifically on ethnic minority women, nor have culturally tailored or recent intervention approaches most effective for these groups of women with traditionally lower use of mammography been discussed. The goal of this study was to fill this gap by conducting analyses on more recent studies (published since September 2000, where the review by Legler et al., 2002, left off) that were targeted specifically to ethnic minority women. Specifically, the objective of the meta-analysis was to describe mammography intervention approaches used for ethnic minority (Asian American, African American, and Hispanic) women in the United States.
Methods
Study Selection
Literature for this review was identified using electronic searches of databases and hand searches from reference collections. The literature search was limited to articles published in the English language from 2000 onwards. Two authors independently searched Medline, CINAHL, PsycINFO, and Web of Science using combinations of the key word phrases Asian, African American, Hispanic or Latino, breast cancer screening, mammography, experimental studies, interventions, and intervention studies.
The electronic and hand searches generated a combined total of 749 titles and abstracts for assessment. Screening of relevant studies for inclusion was conducted using titles and abstracts based on the following criteria: (a) the study aimed to increase use of mammography screening among asymptomatic women, either exclusively or in addition to other health behaviors; (b) the study included more than 40% of women with ethnic minority background (i.e., Asian American, Black, or Hispanic) in the sample; (c) outcomes were based on a woman’s adherence to mammography screening, documented either by self-report or in a clinical database or medical record; (d) an experimental or quasi-experimental design was used in the study; and (e) the study was reported between September 2000 and August 2008. Not included were international studies because the focus was on intervention strategies to improve breast cancer screening among ethnic minority women in the United States.
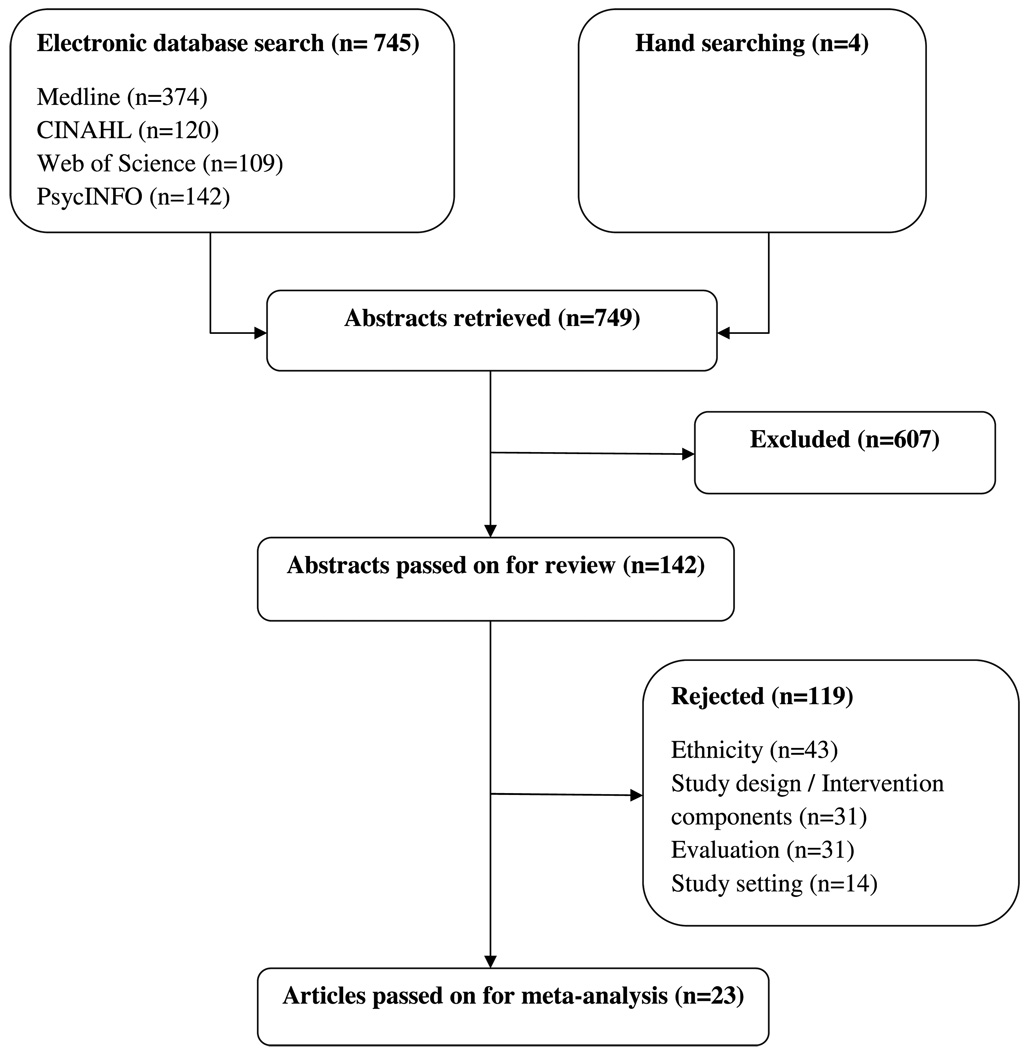
The titles and abstracts of all identified studies were reviewed by two study team members. Of these 749 studies, 607 were excluded. A total of 142 full-text articles were reviewed systematically to confirm eligibility for this study. Of the 142 articles examined, 43 did not include more than 40% of ethnic minority women, or ethnicity was unclear; 23 did not have a control group; 2 were only system directed; and 6 did not specify an intervention component clearly. In addition, 13 did not include enough information to calculate an effect size; 18 did not include a woman’s adherence to mammography screening as an outcome; and 14 had an international study setting or reported on the same sample as another that was already included. As a result, a total of 23 studies were included in the meta-analysis (Figure 1).
FIGURE 1.
Summary of the study selection process.
Study Coding
The specific outcome of interest in this analysis was the difference in the proportion of mammography screening in the intervention group versus the control group. A number of variables were selected for inclusion in the database of articles. The following were coded: first author, year, study design, setting, sample (percentage of ethnic minority women), unit of assignment, type of intervention, intervention period, time to outcome measure (months), method of outcome ascertainment, number of participants in the study groups, mean age of the study sample, proportion of mammography screening for the treatment and control groups, theory, control group (no intervention, minimal intervention or usual care, or other non-breast-cancer intervention), any cultural strategies used, and study quality. Following the typology used in previous reviews (Legler et al., 2002; Rimer, 1994), interventions were categorized as follows: (a) individual directed (e.g., one-on-one counseling, tailored and nontailored letters and reminders, and telephone counseling), (b) system directed (e.g., provider prompts), (c) access enhancing (e.g., mobile vans and reduced-cost mammograms), (d) social network (e.g., peer educators and lay health advisors), (e) community education, (f) mass media, and (g) multiple strategies (combinations of the intervention approaches listed above). As in a prior review (Legler et al., 2002), in five studies comparing two or more intervention groups to one control group, the intervention with the most components (i.e., highest dose group) was considered. To rate study quality, four items were used from relevant literature (Jadad et al., 1996; Soeken, Lee, Bausell, Agelli, & Berman, 2002). The range of total quality scores was 0 to 4 (Table 1). For the purpose of this analysis, studies with scores of 1–2 were considered to be low quality and those with scores of 3–4 were considered to be high quality. Using Microsoft Excel, two raters independently coded the variables. Every discrepancy was identified and resolved by discussion among team members. The average κ for coding agreement was sufficient, 0.86.
TABLE 1.
Study Quality Ratings
| Items | Scores |
|---|---|
| Study design | 0 = Nonrandomized prospective experiment |
| 1 = Randomized experiment | |
| Outcome measure | 0 = Subjective measure of mammogram receipt (self-reports) |
| 1 = Objective measure of mammogram receipt (claims data, chart review) |
|
| Clarity of outcome definition |
0 = No definition of study outcome (mammogram adherence) |
| 1 = Clearly defined mammogram adherence | |
| Information on withdrawal |
0 = Not clearly discussed |
| 1 = The number and the reasons for withdrawals in each group are stated |
Analysis
Stata (StataCorp LP, College Station, TX) was used to conduct the data analysis. An effect size (d) was calculated for each study using the difference in the postintervention adherence rates between the intervention and control groups (pi and pc, respectively). An overall mean weighted effect size (MWES) for the 23 studies was computed using the meta command in Stata, which weights d by the inverse of the estimated study variance in fixed-effects models. For the effect size of d = pi – pc, the study variance was defined to be pi (1 – pi) / ni + pc (1 – pc) / nc, where ni and nc are the number of participants in the intervention and control groups, respectively (DerSimonian & Laird, 1986). A test for heterogeneity of the intervention effects was performed using the DerSimonian and Laird (1986) Q statistic. When significant, a random-effects model was used to accommodate this heterogeneity (DerSimonian & Laird, 1986). This process was repeated to calculate MWES for various subgroups of the 23 studies. In addition, 95% CIs were estimated for each MWES.
The sensitivity analyses consisted of refitting the meta-analysis for the overall MWES to determine whether the results varied by potentially influential studies (i.e., extreme effect size, large sample size) or study quality. A leave-one-out approach was taken and the overall MWES was reestimated by removing the influential studies one at a time. Also conducted were meta-analyses restricted to high- and low-quality studies to compare to the overall MWES. Finally, additional analyses using funnel plot and fail-safe N were performed to examine publication bias. In the absence of publication bias, the plot should be symmetric, resembling an inverted funnel (Light & Pillemer, 1984). Because visual inspection of the funnel plot involves subjective interpretation, Rosenthal’s (1984) fail-safe N was calculated also. This calculation is an estimate of the number of studies having no effect (i.e., zero effect size) that is needed to reduce the overall effect size in the meta-analysis from significant to nonsignificant. If the estimated fail-safe N is greater than a cutoff value (formula = 5k + 10, where k is the number of studies in the meta-analysis; Rosenthal, 1984), it is suggested that there is no evidence of publication bias.
Results
Study Characteristics
Of the 23 studies, 6 studies included predominantly African Americans; 2 studies, Hispanics; 5 studies, Asians; and 10 studies, combined ethnic samples. Randomized experimental study design (61%), group-level assignment (57%), and community setting (83%) were common features of the studies. Sample sizes varied; smaller studies included <100 participants in the sample, whereas the biggest study was done on >5,000 women, totaling 22,849 women. (See Table, Supplemental Digital Content 1, which summarizes the characteristics of studies included in this meta-analysis, http://links.lww.com/A1244 ) This table is also included on the Editor’s Web site at http://www.nursing-research-editor.com.
The studies used single or multiple intervention strategies, with individually directed print materials being the most frequently used approach, followed by peer or lay health worker education or support and telephone counseling. Access-enhancing strategies such as low- or no-cost mammograms, making appointments, mobile vans, or vouchers were included in 6 studies. For the comparison group, 15 studies (65%) provided no intervention or usual care; 6 studies, minimal intervention; and 2 studies, other active nonbreast intervention (e.g., education on cholesterol or physical activity). Self-report rather than medical records was more frequently used as a method of outcome measurement (74% vs. 26%). The Health Belief Model was the most popular theory and was used in 6 studies alone or in combination with other theories such as Transtheoretical Model of Change and Social Learning theory, although in 9 studies, the theoretical approach was unspecified. These theories offered a basis for targets of individualized tailoring (e.g., providing intervention materials attuned to the characteristics of a person) in 4 studies. Most interventions involved some form of cultural strategies except for 2 (both conducted in a healthcare setting). Culturally matched intervention materials and ethnically matched intervention deliveries were equally common, whereas 5 studies indicated participation of members of the target ethnic community as a way of increasing cultural sensitivity of their intervention. Nine (39%) of the studies received a high quality rating, whereas 14 (61%) were rated as low quality.
Pooled Results
The estimated intervention effect and 95% CI for each study are presented in Table 2. As shown in Table 2, the overall MWES for the 23 studies was 0.078 (Z = 4.414, p < .001) with a 95% CI of 0.043 to 0.113, indicating that the interventions were effective in improving mammography screening among ethnic minority women. This effect size was computed using a random-effects model to account for significant heterogeneity among interventions as indicated by a significant Q statistic (Q = 92.95, df = 22, p < .001).
TABLE 2.
Estimated Effect Sizes With 95% Confidence Intervals (CIs)
| Element | Category | No. of Studies | Effect Size (95% CI) |
|---|---|---|---|
| Overall | 23 | 0.078 (0.043 to 0.113) | |
| Intervention typea, b | Individual directed | 19 | 0.099 (0.073 to 0.110) |
| Access enhancing | 6 | 0.155 (0.087 to 0.223) | |
| Social network | 6 | −0.023 (−0.078 to 0.032) | |
| Community education | 4 | 0.013 (−0.067 to 0.094) | |
| Mass media | 4 | 0.065 (−0.007 to 0.138) | |
| Theory | Theory based | 14 | 0.090 (0.042 to 0.137) |
| Nontheory based | 9 | 0.062 (0.009 to 0.116) | |
| Tailored | Yesc | 4 | 0.101 (0.057 to 0.145) |
| No | 19 | 0.076 (0.035 to 0.116) | |
| Cultural strategiesb | Involved target community members | 5 | 0.074 (−0.055 to 0.203) |
| Culturally matched materials | 15 | 0.051 (0.009 to 0.092) | |
| Matched intervention deliveries | 14 | 0.067 (0.015 to 0.120) | |
| Setting | Healthcarec | 4 | 0.113 (0.081 to 0.114) |
| Community | 19 | 0.067 (0.027 to 0.107) | |
| Ethnic groupsd | African American | 9 | 0.098 (0.023 to 0.174) |
| Asian Pacific Islanders | 5 | 0.094 (0.000 to 0.189) | |
| Hispanic | 5 | 0.036 (−0.034 to 0.106) | |
| Quality | High (3 or 4)c | 9 | 0.099 (0.076 to 0.122) |
| Low (1 or 2) | 14 | 0.061 (0.008 to 0.114) |
Type of intervention: individual directed = counseling (in person, telephone), letters, reminders; access enhancing = facilitated scheduling, mobile vans, vouchers, reduced-cost or free mammograms; social network = peer leaders or lay health advisors; community education = community workshops, seminars.
Studies may be classified as using more than one type of intervention or cultural strategies.
Fitted with a fixed-effects model (p for Q statistic > .05).
Included studies with samples >40% of specified ethnic groups.
Subgroup Analyses
Also shown in Table 2 is the effectiveness of the different intervention methods. Access-enhancing interventions had the biggest MWES of 0.155 (n = 6, Z = 4.488, p < .001), followed by individually directed interventions (n = 19, MWES = 0.099, Z = 6.552, p < .001). Estimated effect sizes for other intervention approaches involving mass media (n = 4, MWES = 0.065, Z = 1.759, p = .079), community education (n = 4, MWES = 0.013, Z = 0.324, p = .746), or social networks (n = 6, MWES = −0.023, Z = −0.817, p = .414) were not statistically significant.
Tailoring an intervention according to the individual’s characteristics based on valid behavioral theory was more effective than not doing so, with the MWES being 0.101 (n = 4, Z = 4.476, p < .001) and 0.076 (n = 19, Z = 3.677, p < .001), respectively. Theory-based interventions (n = 14) resulted in a bigger effect size compared with nontheory-based interventions (n = 9; effect sizes = 0.090 vs. 0.062, respectively; p < .05 for all tests). Of cultural strategies, eth nically matched intervention deliveries (n = 14, MWES = 0.067, Z = 2.516, p = .012) and culturally matched intervention materials (n = 15, MWES = 0.051, Z = 2.365, p = .018) significantly improved mammography screening. Interventions involving members of the target community were a cultural strategy, with the biggest effect size of 0.074 (n = 5, Z = 1.124, p = .261), but the result was not significant. Interventions delivered in healthcare settings (n = 4) were associated with a bigger effect size compared with interventions done in community settings (n = 19; MWES = 0.113 vs. 0.067; p < .01 for all models). When combined intervention effects were examined for each ethnic group (included studies with samples >40% of specified ethnic groups), the estimated intervention effect was significant for African American women with a MWES of 0.098 (n = 9, Z = 2.550, p = .011). Studies with other ethnic minority women yielded no significant findings with a MWES of 0.094 for Asian and Pacific Islanders (n = 5, Z = 1.955, p = .051) and 0.036 for Hispanic women (n = 5, Z = 1.004, p = .315).
Sensitivity Analyses
Sensitivity analyses were conducted using potentially influential studies such as Kim and Sarna (2004), Sauaia et al. (2007), and Welsh, Sauaia, Jacobellis, Min, and Byers (2005) to gauge the impact on the variability of effect sizes. When the Kim and Sarna study was removed, the MWES for remaining studies was 0.069 (Z = 4.153, p < .001). Removing Sauaia et al. resulted in a MWES of 0.082 (Z = 4.292, p < .001) for the remaining studies. Without Welsh et al., the MWES for the other 22 studies was 0.085 (Z = 5.198, p < .001). Also performed were analyses with studies of high versus low quality ratings (quality rating 3–4 vs. 1–2). The MWES for the high-quality studies (n = 9) was 0.099 (Z = 8.452, p < .001), whereas the MWES for the low-quality studies (n = 14) was 0.061 (Z = 2.239, p = .025).
Publication Bias
The likelihood of publication bias was examined by first plotting the standard error by the natural logarithm of the logged odds ratio for the estimated effect sizes. The funnel plot appeared slightly asymmetrical. The fail-safe N, however, indicated that 411 nonsignificant studies would be necessary (cutoff = 125) to show that these interventions used to promote mammography screening among traditionally nonadherent ethnic minority women have no effect on mammography adherence, making the aggregate result from this analysis fairly robust.
Discussion
The results indicate that there was an average of 7.8% increase in the rate of mammography use for minority women in the treatment groups receiving a variety of interventions. Access-enhancing interventions yielded the biggest increase in mammography use (15.5%), followed by individually directed interventions (9.9%). Even though the result cannot be compared directly with those of other meta-analyses due to different study selection criteria and intervention typology, this finding is similar to that of Legler et al. (2002) and Yabroff and Mandelblatt (1999).
Interventions using social networks such as promotoras or lay health advisors were associated with a small and negative effect size (i.e., reduced mammography screening rates after intervention). The finding of the negative effect size associated with promotora interventions might have been a result of study design. Specifically, the six promotora interventions included in the meta-analysis (Earp et al., 2002; Fernandez-Esquer, Espinoza, Torres, Ramirez, & McAlister, 2003; Nguyen, Vo, McPhee, & Jenkins, 2001; Powell et al., 2005; Sauaia et al., 2007; Welsh et al., 2005) were all nonrandomized, community-based trials with mostly large sample sizes (mean sample size = about 2,299) and low quality ratings; five studies received a quality rating of 2 and one study received a quality rating of 1. Our finding indicates that promotora interventions may be better suited for smaller community applications. When a large-scale community-based intervention trial is planned, interventions using promotoras may need to be considered as an alternative with well-prepared promotora training and a rigorous monitoring plan.
In analyzing effect sizes by the use of theory, the results indicated that theory-based interventions were more effective than nontheory-based interventions. Tailored interventions guided by theory also resulted in a greater effect size than did nontailored interventions. Indeed, tailored interventions included in this meta-analysis used single or multiple theories to structure the content of the intervention messages. Considering the few tailored interventions with larger improvement in mammography screening, more tailored intervention studies based on valid theories are warranted.
Interventions involving target community members as a way to enhance cultural sensitivity yielded a bigger effect size as compared with interventions using other cultural strategies (e.g., providing culturally matched materials or matching intervention deliveries), although the random-effects model for testing of its effect was not statistically significant. We cannot compare the result with those of other meta-analyses because no previous meta-analyses specifically examined cultural strategies as part of intervention typology. The nonsignificance might be attributable to the small number of studies in this category (n = 5). Although the finding offers some implications in designing mammography-enhancing interventions for ethnic minority women, future meta-analysis is needed as more empirical evidence becomes available.
Consistent with previous meta-analysis (Legler et al., 2002), it was found that the intervention effect was bigger for studies conducted in a healthcare setting (e.g., health maintenance organizations and community health centers) than for the community-based studies. Healthcare settings naturally offer increased contact with medical providers. It is likely that women in the healthcare setting might have had fewer barriers to screening, with more support for obtaining mammograms through individualized letters or counseling (Champion et al., 2007; Young, Waller, & Smitherman, 2002), scheduling of screening appointments (Beach et al., 2007), or case management (Beach et al., 2007; Dietrich et al., 2006). As Legler et al. (2002) pointed out, additional support or cues are necessary to facilitate mammography use even when access may no longer be a problem.
Effect sizes for studies including more than 40% African American and more than 40% Asian or Pacific Islander women were similar (9.8% and 9.4%, respectively), although the effect size for Asian or Pacific Islander women was marginally significant (p = .051); however, the MWES (3.6%) was not statistically significant for comparisons consisting of more than 40% Hispanic women. The estimated effect for intervention groups with more than 40% African American women in the Legler et al. (2002) meta-analysis was 11.6% (95% CI = 6.4–16.7), slightly bigger than that in this study. Although no published analysis of intervention effects for Asian or Pacific Islanders or Hispanic women were found, the nonsignificant result might have been due, in part, to the small number of studies available for these subgroup analyses (five studies each for Asian or Pacific Islander and Hispanic women). A careful examination of the characteristics of each individual study included in the ethnic subgroup analyses also revealed some design issues—particularly for studies involving Hispanic women—that are worth pointing out: three out of five studies with more than 40% Hispanic women (Fernandez-Esquer et al., 2003; Sauaia et al., 2007; Welsh et al., 2005) used a nonrandomized experimental design with a large sample size (N > 5,000 for Sauaia et al., 2007, and Welsh et al., 2005). A large-scale community trial is likely to put researchers in a less controlled situation. Diffusion might occur between groups or control communities may receive interventions with substantial amount through other mechanisms (e.g., the Breast and Cervical Cancer Program for free mammograms). A traditional randomized controlled trial could pose ethical and logistical dilemmas in community research because control groups do not benefit from study participation, which is often perceived as unfair (Learmonth, 2000). Nevertheless, this analysis suggests that more tightly controlled trials may be necessary to improve mammography screening among minority groups, particularly Hispanic women. Researchers may need to consider and engage more actively in alternative research designs (e.g., waiting list design and attention control design) to ensure that the benefits of the research are made available to all ethnic minority communities (Corbie-Smith et al., 2003).
Several limitations of this meta-analysis should be noted. One limitation is the reliance of this review on published sources in Medline, CINAHL, PsycINFO, and Web of Science databases. This might have led to an overestimation or underestimation of effect sizes by excluding unpublished sources (e.g., dissertations) or government documents that might not be readily available, although researchers have found no differences related to inclusion or exclusion of unpublished literature (Conn, Valentine, Cooper, & Rantz, 2003). Second, due to the focus of interest in ethnic minority women in the United States who face unique cultural and linguistic challenges, this review was limited to articles of samples in the United States; thus, the findings may not be generalizable to studies that have been conducted in other countries. Third, as is common in meta-analyses, the uneven quality and quantity of studies are also limitations. An attempt was made to address this issue by offering estimates for high- versus low-quality studies. Several analyses included only four to six studies with nonsignificant MWES. Findings from the analyses with only a small number of studies should be considered as preliminary evidence and not definitive estimates of the effectiveness of the studies. It will be important to conduct additional analyses when results from more studies become available. Finally, most studies included in this meta-analysis used multiple intervention components. One problem in interventions with multiple components is that it is difficult to tease out the effect of each individual component. Some researchers suggest conducting factorial design studies to address this issue (Legler et al., 2002), although the cost to conduct such studies would likely be higher.
In conclusion, uniform improvement in cancer screening is a national goal to address cancer disparities among ethnic minority communities in the United States. The results of this meta-analysis suggest important directions for the design of future interventions to promote mammography screening among ethnic minority women. Access-enhancing strategies are an important intervention component for minority women who are likely to lack the resources to obtain mammography screening readily. Also highlighted in this analysis is a need for increased use of a theory-based, tailored approach. More active engagement of community partners in the research process should be considered also to improve screening outcomes. Finally, based on the pooled MWES estimated in this meta-analysis, well-controlled studies are needed to improve the effectiveness of mammography intervention programs among ethnic minority women, particularly among Hispanic women. Consistent use of the rate difference of mammography screening as an outcome measure is important for additional meta-analyses and promotion of further knowledge development in this important area.
Acknowledgments
This study was supported by a grant from the National Cancer Institute (R01 CA129060). Editorial support was provided by the Johns Hopkins University School of Nursing Center for Collaborative Intervention Research. Funding for the Center is provided by the National Institute of Nursing Research (P30 NRO 8995). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.nursingresearchonline.com)
Contributor Information
Hae-Ra Han, Associate Professor, School of Nursing, The Johns Hopkins University, Baltimore, Maryland.
Jong-Eun Lee, Postdoctoral Fellow, School of Nursing, The Johns Hopkins University, Baltimore, Maryland.
Jiyun Kim, Postdoctoral Fellow, School of Nursing, The Johns Hopkins University, Baltimore, Maryland.
Haley K. Hedlin, Doctoral Student, Bloomberg School of Public Health, The Johns Hopkins University, Baltimore, Maryland.
Heejung Song, Research Associate, Bloomberg School of Public Health, The Johns Hopkins University, Baltimore, Maryland.
Miyong T. Kim, Professor, School of Nursing, Bloomberg School of Public Health, and School of Medicine, The Johns Hopkins University, Baltimore, Maryland.
References
- Allen B, Jr, Bazargan-Hejazi S. Evaluating a tailored intervention to increase screening mammography in an urban area. Journal of the National Medical Association. 2005;97(10):1350–1360. [PMC free article] [PubMed] [Google Scholar]
- American Cancer Society. Cancer facts and figures 2008. Atlanta, GA: Author; 2008. [Google Scholar]
- Avis NE, Smith KW, Link CL, Goldman MB. Increasing mammography screening among women over age 50 with a videotape intervention. Preventive Medicine. 2004;39(3):498–506. doi: 10.1016/j.ypmed.2004.05.024. [DOI] [PubMed] [Google Scholar]
- Beach ML, Flood AB, Robinson CM, Cassells AN, Tobin JN, Greene MA, et al. Can language-concordant prevention care managers improve cancer screening rates? Cancer Epidemiology, Biomarkers & Prevention. 2007;16(10):2058–2064. doi: 10.1158/1055-9965.EPI-07-0373. [DOI] [PubMed] [Google Scholar]
- Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, Conway K, et al. Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA. 2006;295(21):2492–2502. doi: 10.1001/jama.295.21.2492. [DOI] [PubMed] [Google Scholar]
- Champion VL, Springston JK, Zollinger TW, Saywell RM, Jr, Monahan PO, Zhao Q, et al. Comparison of three interventions to increase mammography screening in low income African American women. Cancer Detection and Prevention. 2006;30(6):535–544. doi: 10.1016/j.cdp.2006.10.003. [DOI] [PubMed] [Google Scholar]
- Champion V, Skinner CS, Hui S, Monahan P, Juliar B, Daggy J, et al. The effect of telephone versus print tailoring for mammography adherence. Patient Education and Counseling. 2007;65(3):416–423. doi: 10.1016/j.pec.2006.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu KC, Miller BA, Springfield SA. Measures of racial/ethnic health disparities in cancer mortality rates and the influence of socioeconomic status. Journal of the National Medical Association. 2007;99(10):1092–1100. 1102–1104. [PMC free article] [PubMed] [Google Scholar]
- Cokkinides V, Bandi P, Siegel R, Ward EM, Thun MJ. Cancer prevention & early detection facts & figures 2008. Atlanta, GA: American Cancer Society; 2007. [Google Scholar]
- Conn VS, Valentine JC, Cooper HM, Rantz MJ. Grey literature in meta-analyses. Nursing Research. 2003;52(4):256–261. doi: 10.1097/00006199-200307000-00008. [DOI] [PubMed] [Google Scholar]
- Corbie-Smith G, Ammerman AS, Katz ML, St. George DM, Blumenthal C, Washington C, et al. Trust, benefit, satisfaction, and burden: A randomized controlled trial to reduce cancer risk through African-American churches. Journal of General Internal Medicine. 2003;18(7):531–541. doi: 10.1046/j.1525-1497.2003.21061.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danigelis NL, Worden JK, Flynn BS, Skelly JM, Vacek PM. Increasing mammography screening among low-income African American women with limited access to health information. Preventive Medicine. 2005;40(6):880–887. doi: 10.1016/j.ypmed.2004.10.004. [DOI] [PubMed] [Google Scholar]
- Deapen D, Liu L, Perkins C, Bernstein L, Ross RK. Rapidly rising breast cancer incidence rates among Asian-American women. International Journal of Cancer. 2002;99(5):747–750. doi: 10.1002/ijc.10415. [DOI] [PubMed] [Google Scholar]
- Denhaerynck K, Lesaffre E, Baele J, Cortebeeck K, Van Overstraete E, Buntinx F. Mammography screening attendance: Meta-analysis of the effect of direct-contact invitation. American Journal of Preventive Medicine. 2003;25(3):195–203. doi: 10.1016/s0749-3797(03)00201-0. [DOI] [PubMed] [Google Scholar]
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clinical Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- Dietrich AJ, Tobin JN, Cassells A, Robinson CM, Greene MA, Sox CH, et al. Telephone care management to improve cancer screening among low-income women: A randomized, controlled trial. Annals of Internal Medicine. 2006;144(8):563–571. doi: 10.7326/0003-4819-144-8-200604180-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan N, Fox SA, Derose KP, Carson S. Maintaining mammography adherence through telephone counseling in a church-based trial. American Journal of Public Health. 2000;90(9):1468–1471. doi: 10.2105/ajph.90.9.1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earp JA, Eng E, O’Malley MS, Altpeter M, Rauscher G, Mayne L, et al. Increasing use of mammography among older, rural African American women: Results from a community trial. American Journal of Public Health. 2002;92(4):646–654. doi: 10.2105/ajph.92.4.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards AG, Evans R, Dundon J, Haigh S, Hood K, Elwyn GJ. Personalised risk communication for informed decision making about taking screening tests. Cochrane Database of Systematic Reviews. 2006;(4) doi: 10.1002/14651858.CD001865.pub2. CD001865. [DOI] [PubMed] [Google Scholar]
- Erwin DO, Ivory J, Stayton C, Willis M, Jandorf L, Thompson H, et al. Replication and dissemination of a cancer education model for African American women. Cancer Control. 2003;10(5 Suppl):13–21. doi: 10.1177/107327480301005s03. [DOI] [PubMed] [Google Scholar]
- Fernandez-Esquer ME, Espinoza P, Torres I, Ramirez AG, McAlister AL. A su salud: A quasi-experimental study among Mexican American women. American Journal of Health Behavior. 2003;27(5):536–545. doi: 10.5993/ajhb.27.5.5. [DOI] [PubMed] [Google Scholar]
- Husaini BA, Sherkat DE, Levine R, Bragg R, Van CA, Emerson JS, et al. The effect of a church-based breast cancer screening education program on mammography rates among African-American women. Journal of the National Medical Association. 2002;94(2):100–106. [PMC free article] [PubMed] [Google Scholar]
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Controlled Clinical Trials. 1996;17(1):1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- Jibaja-Weiss ML, Volk RJ, Kingery P, Smith QW, Holcomb JD. Tailored messages for breast and cervical cancer screening of low-income and minority women using medical records data. Patient Education and Counseling. 2003;50(2):123–132. doi: 10.1016/s0738-3991(02)00119-2. [DOI] [PubMed] [Google Scholar]
- Kim YH, Sarna L. An intervention to increase mammography use by Korean American women. Oncology Nursing Forum. 2004;31(1):105–110. doi: 10.1188/04.ONF.105-110. [DOI] [PubMed] [Google Scholar]
- Lantz PM, Mujahid M, Schwartz K, Janz NK, Fagerlin A, Salem B, et al. The influence of race, ethnicity, and individual socioeconomic factors on breast cancer stage at diagnosis. American Journal of Public Health. 2006;96(12):2173–2178. doi: 10.2105/AJPH.2005.072132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Learmonth AM. Utilizing research in practice and generating evidence from practice. Health Education Research. 2000;15(6):743–756. doi: 10.1093/her/15.6.743. [DOI] [PubMed] [Google Scholar]
- Legler J, Meissner HI, Coyne C, Breen N, Chollette V, Rimer BK. The effectiveness of interventions to promote mammography among women with historically lower rates of screening. Cancer Epidemiology, Biomarkers & Prevention. 2002;11(1):59–71. [PubMed] [Google Scholar]
- Light RJ, Pillemer DB. Summing up: The science of reviewing research. Cambridge, MA: Harvard University Press; 1984. [Google Scholar]
- Maxwell AE, Bastani R, Vida P, Warda US. Results of a randomized trial to increase breast and cervical cancer screening among Filipino American women. Preventive Medicine. 2003;37(2):102–109. doi: 10.1016/s0091-7435(03)00088-4. [DOI] [PubMed] [Google Scholar]
- Miller BA, Hankey BF, Thomas TL. Impact of sociodemographic factors, hormone receptor status, and tumor grade on ethnic differences in tumor stage and size for breast cancer in US women. American Journal of Epidemiology. 2002;155(6):534–545. doi: 10.1093/aje/155.6.534. [DOI] [PubMed] [Google Scholar]
- Mishra SI, Bastani R, Crespi CM, Chang LC, Luce PH, Baquet CR. Results of a randomized trial to increase mammogram usage among Samoan women. Cancer Epidemiology, Biomarkers & Prevention. 2007;16(12):2594–2604. doi: 10.1158/1055-9965.EPI-07-0148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mock J, McPhee SJ, Nguyen T, Wong C, Doan H, Lai KQ, et al. Effective lay health worker outreach and media-based education for promoting cervical cancer screening among Vietnamese American women. American Journal of Public Health. 2007;97(9):1693–1700. doi: 10.2105/AJPH.2006.086470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moskowitz JM, Kazinets G, Wong JM, Tager IB. “Health is strength”: A community health education program to improve breast and cervical cancer screening among Korean American women in Alameda County, California. Cancer Detection and Prevention. 2007;31(2):173–183. doi: 10.1016/j.cdp.2007.02.002. [DOI] [PubMed] [Google Scholar]
- Navarro AM, Senn KL, McNicholas LJ, Kaplan RM, Roppe B, Campo MC. Por La Vida model intervention enhances use of cancer screening tests among Latinas. American Journal of Preventive Medicine. 1998;15(1):32–41. doi: 10.1016/s0749-3797(98)00023-3. [DOI] [PubMed] [Google Scholar]
- Nguyen T, Vo PH, McPhee SJ, Jenkins CN. Promoting early detection of breast cancer among Vietnamese-American women. Results of a controlled trial. Cancer. 2001;91(1 Suppl):267–273. doi: 10.1002/1097-0142(20010101)91:1+<267::aid-cncr17>3.3.co;2-0. [DOI] [PubMed] [Google Scholar]
- Park A, Nitzke S, Kritsch K, Kattelmann K, White A, Boeckner L, et al. Internet-based interventions have potential to affect short-term mediators and indicators of dietary behavior of young adults. Journal of Nutrition Education and Behavior. 2008;40(5):288–297. doi: 10.1016/j.jneb.2008.02.001. [DOI] [PubMed] [Google Scholar]
- Powell ME, Carter V, Bonsi E, Johnson G, Williams L, Taylor-Smith L, et al. Increasing mammography screening among African American women in rural areas. Journal of Health Care for the Poor and Underserved. 2005;16(4 Suppl. A):11–21. doi: 10.1353/hpu.2005.0129. [DOI] [PubMed] [Google Scholar]
- Purc-Stephenson RJ, Gorey KM. Lower adherence to screening mammography guidelines among ethnic minority women in America: A meta-analytic review. Preventive Medicine. 2008;46(6):479–488. doi: 10.1016/j.ypmed.2008.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rakowski W, Meissner H, Vernon SW, Breen N, Rimer B, Clark MA. Correlates of repeat and recent mammography for women ages 45 to 75 in the 2002 to 2003 Health Information National Trends Survey (HINTS 2003) Cancer Epidemiology, Biomarkers & Prevention. 2006;15(11):2093–2101. doi: 10.1158/1055-9965.EPI-06-0301. [DOI] [PubMed] [Google Scholar]
- Resnicow K, Davis RE, Zhang G, Konkel J, Strecher VJ, Shaikh AR, et al. Tailoring a fruit and vegetable intervention on novel motivational constructs: Results of a randomized study. Annals of Behavioral Medicine. 2008;35(2):159–169. doi: 10.1007/s12160-008-9028-9. [DOI] [PubMed] [Google Scholar]
- Reuben DB, Bassett LW, Hirsch SH, Jackson CA, Bastani R. A randomized clinical trial to assess the benefit of offering on-site mobile mammography in addition to health education for older women. American Journal of Roentgenology. 2002;179(6):1509–1514. doi: 10.2214/ajr.179.6.1791509. [DOI] [PubMed] [Google Scholar]
- Rimer BK. Mammography use in the U.S.: Trends and the impact of interventions. Annals of Behavioral Medicine. 1994;16(4):317–326. [Google Scholar]
- Rosenthal R. Meta-analysis procedures for social research. Beverly Hills, CA: Sage; 1984. [Google Scholar]
- Sauaia A, Min SJ, Lack D, Apodaca C, Osuna D, Stowe A, et al. Church-based breast cancer screening education: Impact of two approaches on Latinas enrolled in public and private health insurance plans. Preventing Chronic Disease. 2007;4(4):A99. [PMC free article] [PubMed] [Google Scholar]
- Schumann A, John U, Ulbricht S, Ruge J, Bischof G, Meyer C. Computer-generated tailored feedback letters for smoking cessation: Theoretical and empirical variability of tailoring. International Journal of Medical Informatics. 2008;77(11):715–722. doi: 10.1016/j.ijmedinf.2008.03.001. [DOI] [PubMed] [Google Scholar]
- Shavers VL, Harlan LC, Stevens JL. Racial/ethnic variation in clinical presentation, treatment, and survival among breast cancer patients under age 35. Cancer. 2003;97(1):134–147. doi: 10.1002/cncr.11051. [DOI] [PubMed] [Google Scholar]
- Sidani S, Braden CJ. Evaluating nursing interventions: A theory-driven approach. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- Smigal C, Jemal A, Ward E, Cokkinides V, Smith R, Howe HL, et al. Trends in breast cancer by race and ethnicity: Update 2006. CA: A Cancer Journal for Clinicians. 2006;56(3):168–183. doi: 10.3322/canjclin.56.3.168. [DOI] [PubMed] [Google Scholar]
- Smith-Bindman R, Miglioretti DL, Lurie N, Abraham L, Barbash RB, Strzelczyk J, et al. Does utilization of screening mammography explain racial and ethnic differences in breast cancer? Annals of Internal Medicine. 2006;144(8):541–553. doi: 10.7326/0003-4819-144-8-200604180-00004. [DOI] [PubMed] [Google Scholar]
- Soeken KL, Lee WL, Bausell RB, Agelli M, Berman BM. Safety and efficacy of S-adenosylmethionine (SAMe) for osteoarthritis. Journal of Family Practice. 2002;51(5):425–430. [PubMed] [Google Scholar]
- Sohl SJ, Moyer A. Tailored interventions to promote mammography screening: A meta-analytic review. Preventive Medicine. 2007;45(4):252–261. doi: 10.1016/j.ypmed.2007.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. Stata statistical software: Release 9. College Station, TX: Author; 2005. [Google Scholar]
- Suarez L, Roche RA, Pulley LV, Weiss NS, Goldman D, Simpson DM. Why a peer intervention program for Mexican-American women failed to modify the secular trend in cancer screening. American Journal of Preventive Medicine. 1997;13(6):411–417. [PubMed] [Google Scholar]
- Taylor VM, Jackson JC, Yasui Y, Kuniyuki A, Acorda E, Marchand A, et al. Evaluation of an outreach intervention to promote cervical cancer screening among Cambodian American women. Cancer Detection and Prevention. 2002;26(4):320–327. doi: 10.1016/s0361-090x(02)00055-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Town RJ, Wholey DR, Feldman RD, Burns LR. Hospital consolidation and racial/income disparities in health insurance coverage. Health Affairs. 2007;26(4):1170–1180. doi: 10.1377/hlthaff.26.4.1170. [DOI] [PubMed] [Google Scholar]
- U.S. Preventive Services Task Force. Screening for breast cancer: Recommendations and rationale. 2002 Retrieved May 8, 2008, from http://www.ahcpr.gov/clinic/3rduspstf/breastcancer/brcanrr.htm.
- Wasserman M, Bender D, Lee SY. Use of preventive maternal and child health services by Latina women: A review of published intervention studies. Medical Care Research and Review. 2007;64(1):4–45. doi: 10.1177/1077558706296238. [DOI] [PubMed] [Google Scholar]
- Welsh AL, Sauaia A, Jacobellis J, Min SJ, Byers T. The effect of two church-based interventions on breast cancer screening rates among Medicaid-insured Latinas. Preventing Chronic Disease. 2005;2(4):A07. [PMC free article] [PubMed] [Google Scholar]
- Wood RY, Duffy ME. Video breast health kits: Testing a cancer education innovation in older high-risk populations. Journal of Cancer Education. 2004;19(2):98–104. doi: 10.1207/s15430154jce1902_10. [DOI] [PubMed] [Google Scholar]
- Yabroff KR, Mandelblatt JS. Interventions targeted toward patients to increase mammography use. Cancer Epidemiology, Biomarkers & Prevention. 1999;8(9):749–757. [PubMed] [Google Scholar]
- Young RF, Waller JB, Jr, Smitherman H. A breast cancer education and on-site screening intervention for unscreened African American women. Journal of Cancer Education. 2002;17(4):231–236. doi: 10.1080/08858190209528844. *Indicates studies included in this meta-analysis. [DOI] [PubMed] [Google Scholar]