Cardiac arrest occurs only about once in every 30 000 late pregnancies, but survival from such an event is exceptional. Most deaths are from acute causes, with many mothers receiving some form of resuscitation. However, the number of indirect deaths—that is, deaths from medical conditions exacerbated by pregnancy—is greater than that of deaths from conditions that arise from pregnancy itself. The use of national guidelines can decrease mortality, as shown by the reduction in the number of deaths from pulmonary embolus and sepsis after caesarean section. To try to reduce mortality from amniotic fluid embolism, a national database for suspected cases has been established.
Table 1.
Physiological changes in late pregnancy affecting cardiopulmonary resuscitation
| Respiratory |
| • Increased ventilation |
| • Increased oxygen demand |
| • Reduced chest compliance |
| • Reduced functional residual capacity |
| Cardiovascular |
| • Incompetent gastroesophageal (cardiac) sphincter |
| • Increased intragastric pressure |
| • Increased risk of regurgitation |
Factors peculiar to pregnancy that weigh the balance against survival include anatomical changes that make it difficult to maintain a clear airway and perform intubation, pathological changes such as laryngeal oedema, physiological factors such as increased oxygen consumption, and an increased likelihood of pulmonary aspiration. In the third trimester the most important factor is compression of the inferior vena cava and impairment of venous return by the gravid uterus when the woman lies supine. These difficulties may be exaggerated by obesity. All staff directly or indirectly concerned with obstetric care need to be trained in resuscitation.
A speedy response is essential. Once respiratory or cardiac arrest has been diagnosed, the patient must be positioned appropriately and basic life support started immediately. This must be continued while venous access is secured, any obvious causal factors are corrected (for example, hypovolaemia), and the necessary equipment, drugs, and staff are assembled.
Table 2.
Specific difficulties in pregnant patients
| Airway |
| Patient needs to be inclined laterally for: |
| • Suction or aspiration |
| • Removing dentures or foreign bodies |
| • Inserting airways |
| Breathing |
| • Greater oxygen requirement |
| • Reduced chest compliance |
| • More difficult to see rise and fall of chest |
| • More risk of regurgitation and aspiration |
| Circulation |
| External chest compression difficult because: |
| • Ribs flared |
| • Diaphragm raised |
| • Patient obese |
| • Breasts hypertrophied |
| • Supine position causes inferior vena cava compression by the gravid uterus |
Basic life support
Airway
A clear airway must be quickly established with the head tilt-jaw thrust or head tilt-chin lift manoeuvre and then maintained. Suction should be used to aspirate vomit. Badly fitting dentures and other foreign bodies should be removed from the mouth, and an airway should be inserted. These procedures should be performed with the patient inclined laterally or supine and the uterus displaced as described below.
Breathing
If the patient is not breathing adequately, intermittent positive pressure ventilation should be started once the airway has been cleared; mouth to mouth, mouth to nose, or mouth to airway ventilation should be carried out until a self inflating bag and mask are available. Ventilation should then be continued with 100% oxygen and a reservoir bag. Because of the increased risk of regurgitation and pulmonary aspiration of gastric contents in late pregnancy, cricoid pressure should be applied until the airway has been protected by a cuffed tracheal tube.
Figure 1.

Patient inclined laterally by using Cardiff wedge
Ventilation is made more difficult by the increased oxygen requirements and reduced chest compliance in pregnancy. The reduced compliance is due to rib flaring and splinting of the diaphragm by the abdominal contents. Observing the rise and fall of the chest in pregnant patients is also more difficult.
This article is adapted from the 5th edition of the ABC of Resuscitation, which will be published by BMJ Books in December (www.bmjbooks.com)
Circulation
Circulatory arrest is diagnosed by the absence of a palpable pulse in a large artery (carotid or femoral). Chest compressions are given at the standard rate and ratio of 15:2. Chest compression on a pregnant woman is made difficult by flared ribs, raised diaphragm, obesity, and breast hypertrophy. Because the diaphragm is pushed upwards by the abdominal contents, the hand position for chest compressions should similarly be moved up the sternum, although currently no guidelines suggest exactly how far.
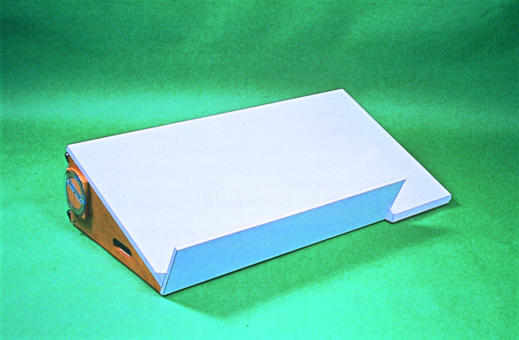
Figure 2.
Manual displacement of uterus
In the supine position an additional factor is compression of the inferior vena cava by the gravid uterus, which impairs venous return and reduces cardiac output; all attempts at resuscitation will be futile unless the compression is relieved. This is achieved either by placing the patient in an inclined lateral position by using a wedge or by displacing the uterus manually. Raising the patient's legs will improve venous return.
Lateral displacement of the uterus
Effective forces for chest compression can be generated with patients inclined at angles of up to 30°, but pregnant women tend to roll into a full lateral position when inclined at angles greater than this, making chest compression difficult. The Cardiff resuscitation wedge is not commercially available, so other techniques need to be used. One technique is the “human wedge,” in which the patient is tilted on to a rescuer's knees to provide a stable position for basic life support. Alternatively, the patient can be tilted on to the back of an upturned chair. Purpose-made wedges are available in maternity units, but any cushion or pillow can be used to wedge the patient into the left inclined position. An assistant should, however, move the uterus further off the inferior vena cava by lifting it with two hands to the left and towards the patient's head.
Figure 3.
Use of an upturned chair as wedge
Advanced life support
Intubation
Tracheal intubation should be carried out as soon as facilities and skill are available. Difficulty in tracheal intubation is more common in pregnant women, and specialised equipment for advanced airway management may be required. A short obese neck and full breasts due to pregnancy may make it difficult to insert the laryngoscope into the mouth. The use of a short handled laryngoscope or one with its blade mounted at more than 90° (polio or adjustable blade) or demounting the blade from the handle during insertion into the mouth may help.
Figure 4.
Cardiff wedge
Mouth to mouth or bag and mask ventilation is best done without pillows under the head and with the head and neck fully extended. The position for intubation, however, requires at least one pillow to flex the neck and extend the head. Any pillow removed to facilitate initial ventilation must, therefore, be kept at hand for intubation.
In the event of failure to intubate the trachea or ventilate the patient's lungs with a bag and mask, insertion of a laryngeal mask airway should be attempted. Cricoid pressure must be temporarily removed in order to place the laryngeal mask airway successfully. Once the airway is in place, cricoid pressure should be reapplied.
Table 3.
Anatomical features relevant to difficult intubation or ventilation
| • Full dentition |
| • Large breasts |
| • Oedema or obesity of neck |
| • Supraglottic oedema |
| • Flared ribcage |
| • Raised diaphragm |
Defibrillation and drugs
Defibrillation and drug administration is in accordance with advanced life support recommendations. On a practical note, it is difficult to apply an apical defibrillator paddle with the patient inclined laterally, and great care must be taken to ensure that the dependent breast does not come into contact with the hand holding the paddle. This problem is avoided if adhesive electrodes are used.
Increasingly, magnesium sulphate is used to treat and prevent eclampsia. If a high serum magnesium concentration has contributed to the cardiac arrest, consider giving calcium chloride. Tachyarrhythmias due to toxicity of the anaesthetic drug bupivacaine are probably best treated by electrical cardioversion or with bretylium rather than lidocaine (lignocaine).
Caesarean section
This is not merely a last ditch attempt to save the life of the fetus; it plays an important part in the resuscitation of the mother. Many successful resuscitations have occurred after prompt surgical intervention. The probable mechanism for the favourable outcome is that occlusion of the inferior vena cava is relieved completely by emptying the uterus, whereas it is only partially relieved by manual uterine displacement or an inclined position. Delivery also improves thoracic compliance, which will improve the efficacy of chest compressions and the ability to ventilate the lungs.
Figure 5.
Paramedics are often the primary responders in obstetric emergency calls and so must be aware of the problems associated with resuscitation in pregnancy
After cardiac arrest, non-pregnant adults suffer irreversible brain damage from anoxia within three to four minutes, but pregnant women become hypoxic more quickly. Although evidence shows that the fetus can tolerate prolonged periods of hypoxia, the outlook for the neonate is optimised by immediate caesarean section.
If maternal cardiac arrest occurs in the labour ward, operating theatre, or accident and emergency department, and basic and advanced life support are not successful within five minutes, the uterus should be emptied by surgical intervention. Given the time taken to prepare theatre packs, this procedure is probably best carried out with just a scalpel. Time passes very quickly in such a high pressure situation, and it is advisable to practise this scenario, particularly in the accident and emergency department.
Cardiopulmonary resuscitation must be continued throughout the operation and afterwards because this improves the prognosis for mother and child. If necessary, transabdominal open cardiac massage can be performed. After successful delivery both mother and infant should be transferred to their appropriate intensive care units as soon as clinical conditions permit. The key factor for successful resuscitation in late pregnancy is that all midwifery, nursing, and medical staff concerned with obstetric care should be trained in cardiopulmonary resuscitation.
Training
Retention of cardiopulmonary resuscitation skills is poor, particularly in midwives and obstetricians who have little opportunity to practise them. Regular short periods of practice on a manikin are therefore essential.
Members of the public and the ambulance service should be aware of the additional problems associated with resuscitation in late pregnancy. The training of ambulance staff is particularly important as paramedics are likely to be the primary responders to community obstetric emergency calls.
The timing of caesarean section and the speed with which surgical delivery is carried out is critical in determining the outcome for mother and fetus. Most of the children and mothers who survive emergency caesarean deliveries are delivered within five minutes of maternal cardiac arrest
Stephen Morris and Mark Stacey are consultant obstetric anaesthetists at Cardiff and Valie NHS Trust, South Glamorgan
The ABC of Resuscitation was edited by Michael Colquhoun, senior lecturer in prehospital care, Wales Heart Research Institute, Universtiy of Wales College of Medicine, Cardiff (colquhoun@bishopsfrome.u-net.com), Anthony J Handley, senior research fellow, Prehospital Emergency Research Unit, University of Wales College of Medicine, and Tom Evans, consultant cardiologist, Royal Free Hospital, London
Competing interests: None declared.
Further reading and resources
- • Department of Health. Report on the confidential enquiry into maternal deaths in the United Kingdom, 1997-1999. London: Stationery Office, 2001.
- • European Resuscitation Council. Part 8: Advanced challenges in resuscitation. Section 3: Special challenges in ECC.3F: Cardiac arrest associated with pregnancy. Resuscitation 200:46: 293-5 [PubMed] [Google Scholar]
- • Goodwin AP, Pearce AJ. The human wedge: a manoeuvre to relieve aortocaval compression in resuscitation during late pregnancy. Anaesthesia 1992;47: 433-4 [DOI] [PubMed] [Google Scholar]
- • Page-Rodriguez A, Gonzalez-Sanchez JA. Perimortem cesarean section of twin pregnancy: case report and review of the literature. Acad Emerg Med 1999;6: 1072-4 [DOI] [PubMed] [Google Scholar]
- • Whitten M, Irvine LM. Postmortem and perimorten cesarean section: what are the indications? J R Soc Med 2000;93: 6-9 [DOI] [PMC free article] [PubMed] [Google Scholar]