Abstract
The interpersonal model of binge eating disorder proposes that social problems lead to negative affect which, in turn, precipitates binge eating episodes. However, no study to date has examined this model among youth who report loss of control (LOC) eating. Participants were 219 non-treatment seeking children and adolescent volunteers, age 8–17 years (13.1 ± 2.8y; 50% female). Children’s social problems were assessed by parent report. Youth completed self-report questionnaires of negative affect that assessed depressive symptoms and anxiety. Participants were interviewed to determine the presence or absence of LOC eating in the month prior to assessment. Structural equation modeling analyses found that social problems were positively related to LOC eating presence (p = 0.02). Negative affect mediated the relationship between social problems and LOC eating (95% CI Product = .00247, .01336). These preliminary results suggest that the interpersonal model of binge eating may describe one possible pathway for the development of LOC eating among non-treatment seeking youth.
Keywords: Interpersonal model, binge eating disorder, loss of control eating, children, adolescents
Binge eating is defined as the consumption of an objectively large amount of food while experiencing a sense of loss of control (LOC) over eating. Binge eating disorder (BED), a putative diagnostic category in the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders Text Revision (DSM-IV-TR), is characterized by recurrent binge eating episodes during which marked distress is experienced with regard to the binge eating (American Psychiatric Association, 2000). Among adults, BED is associated with distress about shape and weight, poor social functioning, and low self-esteem (Wilfley, Wilson, & Agras, 2003). Individuals with BED are also more likely to have co-morbid mood and anxiety disorders in comparison to both overweight and non-overweight adults without BED (Wilfley et al., 2003).
Several of the theories proposed to describe the development and maintenance of BED suggest that binge eating serves as a maladaptive mechanism for coping with negative affect (Heatherton & Baumeister, 1991; Stice, 1994). Bolstering such theories is evidence that adults with BED often experience binge episodes in response to adverse mood states (Agras & Telch, 1998). Furthermore, adults with BED are more likely to eat in response to negative emotions compared to overweight and obese adults without BED (Eldredge & Agras, 1996; Masheb & Grilo, 2006).
The interpersonal theory of BED (Wilfley, MacKenzie, Welch, Ayres, & Weissman, 2000) was originally developed from research in the depression literature (Klerman, Weissman, Rounsaville, & Chevron, 1984), and thus places considerable emphasis on the role of affect in the development and maintenance of binge eating. Interpersonal theory proposes that individual interpersonal patterns either foster self-esteem or result in hopelessness, anxiety and psychopathology (Sullivan, 1953). The interpersonal theory of BED proposes that difficulties with social functioning precipitate low self-esteem and negative affect, which trigger binge eating behaviors in an attempt to cope with negative feelings (Wilfley, Pike, & Striegel-Moore, 1997). The success of interpersonal psychotherapy for the treatment of BED in adults supports this underlying theoretical model (Wilfley et al., 2002; Wilson, Wilfley, Agras, & Bryson, In press).
Although the diagnosis of BED during youth is rare, studies indicate that the experience of LOC, regardless of the amount of food consumed, is common, with prevalence rates ranging from 9.4% to 29.5% in non-treatment-seeking samples (Tanofsky-Kraff, 2008). LOC appears to be a salient marker of disordered eating behavior during youth, as it is associated with disordered eating attitudes, symptoms of depression and anxiety, and parent-reported problem behaviors (Tanofsky-Kraff, 2008). LOC eating is also associated with being overweight (Tanofsky-Kraff et al., 2004) and is predictive of excess weight gain over time (Tanofsky-Kraff, Yanovski et al., 2009). Therefore, understanding the mechanisms that underlie LOC eating in youth is important for understanding and potentially reducing risk for obesity and eating disorders.
To our knowledge, no study has examined whether the interpersonal model for BED might also describe the manifestation of LOC eating in youth. However, it has been proposed that similar to adults with BED, youth who experience LOC may use food as a maladaptive way to cope with negative feelings that result from difficulties in the social milieu (Tanofsky-Kraff, Wilfley et al., 2007). Indeed, cross-sectional data show that youth with LOC have difficulty regulating negative emotions (Czaja, Rief, & Hilbert, 2009) and are more likely to eat in response to adverse emotion when compared to youth without LOC (Tanofsky-Kraff, Theim et al., 2007). Additionally, in a multi-site study of children and adolescents, both boys and girls reported that negative emotion commonly preceded LOC eating episodes (Tanofsky-Kraff, Goossens et al., 2007).
Although no studies have tested the interpersonal model of LOC in youth, research on peer teasing during childhood and adolescence has shown cross-sectional (Hayden-Wade et al., 2005) and prospective (Gardner, Stark, Friedman, & Jackson, 2000) associations with binge eating. Further, in longitudinal studies of adolescent girls, both negative affect and low perceived social support were related to binge eating onset (Stice, Presnell, & Spangler, 2002; Van Strien, Engels, Van Leeuwe, & Snoek, 2005). Similarly, in a cross-sectional study (Schutz & Paxton, 2007), adolescent girls’ social anxiety, social insecurity, and negative friendship characteristics (e.g. conflict and isolation) were associated with a cluster of disordered eating patterns that included binge eating. Consistent with the interpersonal model, the association between social factors and disordered eating in this study was attenuated in analyses controlling for depressive symptoms, suggesting that negative affect may have partly explained the relationship between perceived social difficulties and disordered eating (Schutz & Paxton, 2007).
Despite evidence for significant relationships among social difficulties, negative affect, and disordered eating in youth, no study has tested the interpersonal model of LOC eating in children or adolescents. We therefore conducted a cross-sectional investigation of the interpersonal model of LOC by examining the relationships among social problems, negative affect, and LOC in a non-treatment-seeking sample of youth. We hypothesized that social problems and negative affect would be positively related to each other and that each of these factors would also be related to the presence of LOC eating. Further, based on the interpersonal model, we expected negative affect to mediate the relationship between social problems and LOC eating.
Method
Participants were a convenience sample of non-treatment seeking youth ages 8–17 years who volunteered for a study of eating behaviors. Recruitment, inclusion, and exclusion criteria, and assent/consent procedures are described elsewhere (Tanofsky-Kraff, McDuffie et al., 2009). All children were in good general health and understood that they would not receive treatment as part of the study, but would be financially compensated for their participation. Body composition and disordered eating data from 188 youth in this cohort have been published previously in an investigation of energy intake among youth with and without LOC (Tanofsky-Kraff, McDuffie et al., 2009).
As part of their baseline assessment, participants’ height and weight were measured, as previously described (Tanofsky-Kraff et al., 2004), to determine body mass index (BMI, kg/m2). Pubertal development was assessed by a pediatric endocrinologist or trained pediatric or family nurse practitioner. For girls, breast development was assigned according to the five stages of Tanner (Marshall & Tanner, 1969, 1970) and for boys, testicular volumes were measured according to Prader (Tanner, 1981). For the purposes of the current study, participants were classified as pre/early puberty (girls’ breast Tanner stage = 1–2, boys’ testicular volume = 1–6 cc) or middle/late puberty (girls’ breast Tanner stage = 3–5, boys’ testicular volume = 8–20 cc). Youth completed an interview assessment of disordered eating pathology and questionnaires assessing symptoms of general psychopathology. Additionally, parents of youth completed a questionnaire assessing their children’s socio-emotional and behavioral adjustment.
Social Problems
Children’s interpersonal difficulties were assessed with parent report on the Child Behavior Checklist (CBCL) (Achenbach & Edelbrock, 1991) for children 4–18 years of age. The CBCL measures parents’ perceptions of the child’s behavior, school performance, and social adjustment. For this study, the Social Problems scale was examined as a measure of problem social behaviors, such as being teased or acting lonely. The CBCL is extensively used and has excellent psychometric properties (McConaughy, 1993).
Negative Affect
Negative affect was assessed using two self-report measures. First, children completed the Children’s Depression Inventory (CDI) (Kovacs, 1995), a 27-item self-report questionnaire designed to assess depressive symptoms in children and adolescents. The CDI generates a total score comprised of five subscale scores (negative mood, interpersonal problems, ineffectiveness, anhedonia, and negative self-esteem). Only the total score was examined in this study. The CDI has good psychometric properties (Kovacs, 1995). Second, children’s anxiety symptoms were assessed by self-report on the State-Trait Anxiety Inventory for Children (STAI-C) – Trait Version (Spielberger, Edwards, Lushene, Montuori, & Platzek, 1973), a 20-item measure of trait anxiety for children. The STAI-C has high internal consistency and adequate validity (Spielberger, Gorsuch, & Lushene, 1970).
Interview Assessment of LOC Eating
The Eating Disorder Examination version 12OD/C.2 (Fairburn & Cooper, 1993) (EDE) or the EDE adapted for children (Bryant-Waugh, Cooper, Taylor, & Lask, 1996) (ChEDE) was administered to each participant as described previously (Tanofsky-Kraff et al., 2004) to determine the presence or absence of LOC eating in the month prior to assessment. The child version differs from the adult EDE only in that its script has been edited to make it more accessible to children ages 8–14 years. The EDE’s interview-based, interactive nature allows for questions to be explained so that they are understood by each individual. Further, during the ChEDE, special care is taken, and examples are provided, to explain difficult concepts such as “loss of control,” or the sense of being unable to stop eating once started. For example, when a child does not readily understand the concept of loss of control, one of the standardized descriptions used is that the experience is “like a ball rolling down a hill, going faster and faster.” Based on their responses to the EDE, participants were categorized as engaging in objective binge episodes (overeating with LOC), subjective binge episodes (LOC without objective overeating as assessed by the interviewer, but viewed as excessive by the interviewee), objective overeating (overeating without LOC) or no episode (a meal involving neither LOC nor overeating) over the 28 days prior to assessment. For the purposes of the current study, participants reporting at least one instance of an objective or a subjective binge episode in the past month were categorized as those with LOC eating. Children with objective overeating or no episodes over the month prior to assessment were categorized as those without LOC eating. EDE training, administration, and psychometrics are described elsewhere (Tanofsky-Kraff et al., 2004).
Data Analysis Plan
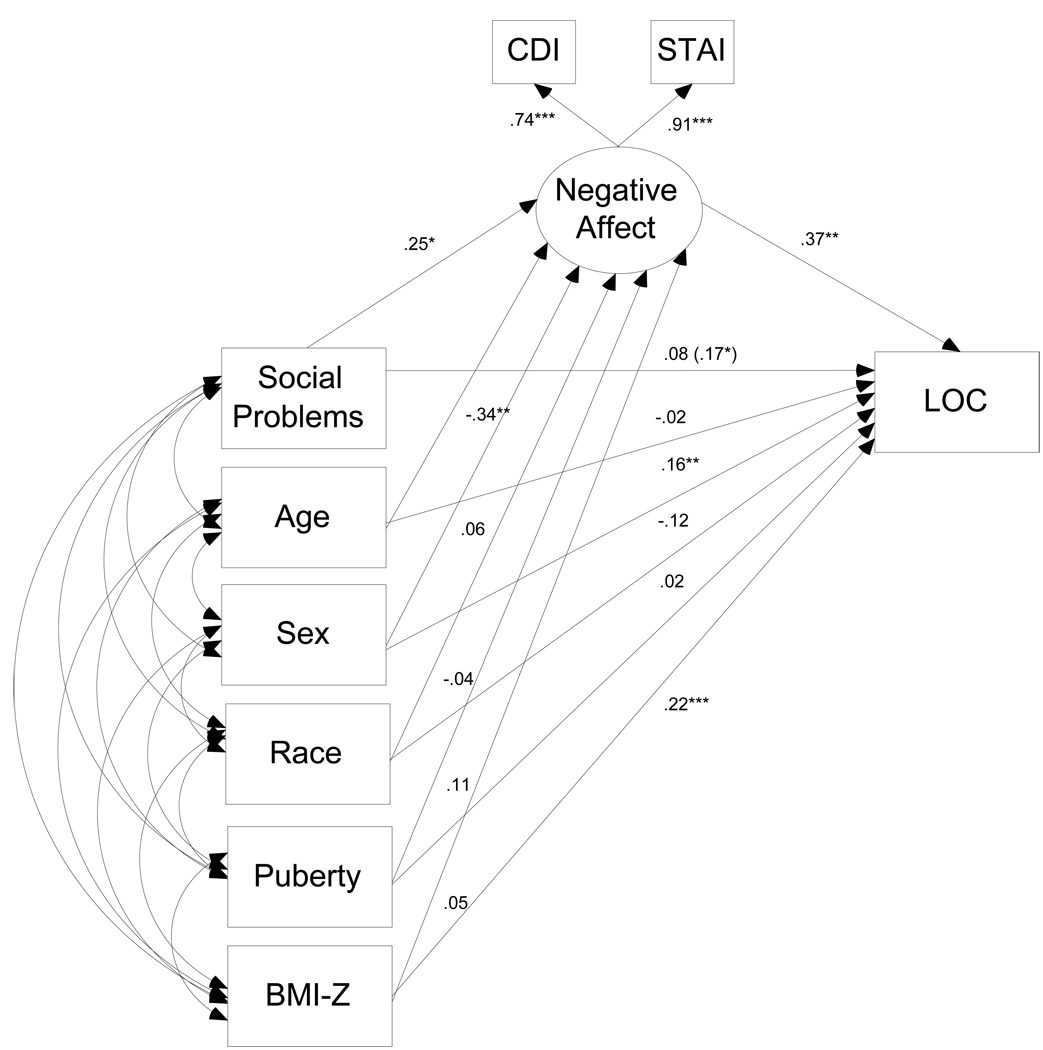
Data were examined to determine that all variables were normally distributed (Behrens, 1977). Outliers were adjusted to fall 1.5 times the interquartile range below the 25th percentile or above the 75th percentile (i.e., to the whiskers in Tukey’s boxplot (Tukey, 1977). All scores had acceptable levels of skew and kurtosis. Descriptive analyses were generated on all study variables and Pearson correlations were used to examine the bivariate intercorrelations among CBCL social problems, CDI score, STAI-C score, age, sex, race, BMI z-score, and pubertal status. To examine the hypothesized model, structural equation modeling (SEM) based on full information maximum likelihood estimation was conducted using AMOS 16.0 (SPSS, Chicago, IL) (Arbuckle, 2003). SEM was used to model negative affect as a latent variable comprised of two indicators (CDI total score depressive symptoms and STAI-C trait anxiety symptoms) (Kline, 2005; Nelson, Aylward, & Steele, 2008). SEM allows minimization of Type I error by reducing the number of analyses run (Kline, 2005). Because model chi-square (χ2M) is highly sensitive to sample size, Bentler comparative fit index (CFI) was examined as an additional fit index; a value equal or greater than .90 is considered indicative of a reasonably good fitting model (Kline, 2005). First, we tested the relationship between social problems and negative affect, as well as the relationship between negative affect and LOC eating. Then, we examined a model in which negative affect mediated the relationships between social problems and LOC eating, accounting for the effects of age, sex, race, BMI z-score, and pubertal status on negative affect and LOC eating (Figure 1). We then removed negative affect from the model and examined a model in which social problems were associated with LOC eating presence, to ensure the role of negative affect as a mediator. A distribution-of-products approach was used to test for mediation because this approach has better statistical power and less likelihood of Type I errors than traditional methods (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002; MacKinnon, Lockwood, & Williams, 2004). A confidence interval for the indirect effect of social problems on LOC eating through negative affect was derived based on the asymmetric distribution of the product of two coefficients: a) α, the effect of the independent variable (social problems) on the mediator (negative affect), and b) β, the effect of the mediator (negative affect) on the dependent variable (LOC eating).
Figure 1.
Model of negative affect as a mediator of social problems and loss of control (LOC) eating, accounting for age, sex, race, puberty, and BMI-z. *p<.05, **p<.01, ***p<.001. Note: When negative affect was removed from the model, social problems were significantly related to LOC eating (path = 17, p = .02).
Results
Two-hundred-nineteen children and adolescents (mean ± SD, age 13.1 ± 2.8y) participated in the present study (Table 1). Sixty-two children (28.4%) had experienced at least one episode of LOC in the month prior to assessment. Children with LOC and those without LOC did not differ significantly in age, race, socioeconomic strata, or pubertal status (Table 1). As expected (Tanofsky-Kraff, McDuffie et al., 2009), LOC was more prevalent in girls than boys (p = .01), and mean BMI z-score was higher in youth with LOC compared to youth with no LOC (p < .001). Parent-reported CBCL social problem scores were higher among the LOC compared to the no LOC group (t = −3.73, p < .001). The LOC group also had higher CDI depressive symptoms scores (t = −4.91, p < .001) and STAI-C anxiety symptoms scores (t = −6.14, p < .001) relative to youth without LOC.
Table 1.
Group Demographics (N = 219)
| No LOC | LOC | p-value | |
|---|---|---|---|
| (n = 157) | (n = 62) | ||
| Age (y) | 13.2 ± 2.8 | 12.9 ± 2.8 | .50 |
| Sex (% female) | 43.9 | 64.5 | .01 |
| Race/Ethnicity (%) | .53 | ||
| Caucasian | 56.7 | 59.7 | |
| Black | 33.8 | 29.0 | |
| Asian | 3.1 | 3.2 | |
| Other | 1.3 | 4.8 | |
| Unknown | 5.1 | 3.2 | |
| Median Socieconomic Satusa | 2 | 2 | .63 |
| Pubertal Stage (% middle/late puberty)b | 52.0 | 50.8 | .88 |
| BMI z-score | 0.76 ± 1.14 | 1.42 ± 1.04 | <0.001 |
| CDI Total | 4.6 ± 4.1 | 7.9 ± 5.3 | <0.001 |
| STAI-C Trait | 28.9 ± 6.2 | 34.7 ± 6.4 | <0.001 |
| CBCL Social Problems | 52.9 ± 5.0 | 56.1 ± 6.8 | <0.001 |
Note: For socioeconomic status, higher numbers are indicative of lower social status (range: 1–5).
Pubertal stage was coded according to the stages of Tanner (range 1–5) as pre/early puberty (girls’ breast Tanner stage = 1–2, boys’ testicular volume = 1–6 cc) or middle/late puberty (girls’ breast Tanner stage = 3–5, boys’ testicular volume = 8–20 cc).
CDI = Children’s Depression Inventory, STAI-C = State-Trait Anxiety Inventory for Children, CBCL = Child Behavior Checklist
As depicted in Figure 1, the model provided an adequate fit to the data, χ2 (df = 6, N = 219) = 18.01, p = .006, CFI = .97. Social problems were associated with negative affect (path = .25, p = .002), and in turn, negative affect was associated with LOC eating (path = .37, p < .001). Furthermore, negative affect served as a significant mediator of social problems and LOC eating. There was evidence for an indirect effect of social problems on LOC eating through negative affect, (95% CI Product = .00247, .01336). Consistent with its role as a mediator, when negative affect was removed from the model (keeping all the same covariates in the model), social problems became significantly, positively associated with LOC eating presence (path = .17, p = .02). We conducted a follow-up, multiple-group analysis to test whether weight status (overweight ≥ 85th percentile, non-overweight < 85th percentile) moderated the observed associations among social problems, negative affect, and LOC eating. The fit of the model in which the paths among these variables were constrained to be equal did not significantly differ from the fit of model in which these paths were unconstrained, χ2diff (dfdiff = 3) = 5.68, p = .13, indicating that weight status did not act as a significant moderator of the relationships among social problems, negative affect, and LOC eating.
Discussion
In this preliminary investigation of the interpersonal model of LOC eating among non-treatment seeking children and adolescents, we found that social problems, negative affect, and LOC eating were all positively interrelated. As hypothesized, the association between children’s social problems and LOC eating was consistent with a role for children’s negative affect as a mediator, providing initial support for the application of the interpersonal model to youth with LOC.
Previous studies have documented similarities between youth with LOC and adults with BED, including elevated symptoms of general psychopathology, a greater likelihood of being overweight, and a propensity to eat in response to adverse feelings (Tanofsky-Kraff, Goossens et al., 2007; Wilfley et al., 2003). In the present study, the finding that youth with LOC experienced elevated rates of negative affect is in concert with such previous literature (Tanofsky-Kraff, Goossens et al., 2007; Tanofsky-Kraff, Theim et al., 2007). This study also builds upon a growing body of literature linking interpersonal difficulties to LOC eating behaviors during youth (Libbey, Story, Neumark-Sztainer, & Boutelle, 2008; Schutz & Paxton, 2007). This finding holds particular relevance as peer interactions become increasingly salient throughout childhood (Furman & Buhrmester, 1992) and are prospectively related to the progression of disordered eating behaviors (Stice et al., 2002) and excess weight gain with age (Lemeshow et al., 2008). These results further suggest that affective theories that have been proposed as explanations for adult binge eating may also apply to LOC experienced during childhood and adolescence. Consistent with the interpersonal model for BED (Wilfley et al., 2000), this study provides provisional evidence that social difficulties may be one pathway leading to the greater negative affect observed among youth with LOC eating (Tanofsky-Kraff, Goossens et al., 2007; Tanofsky-Kraff, Theim et al., 2007).
Strengths of the study include use of interview methodology to assess for the presence of LOC eating and multiple indicators of negative affect. This investigation included both boys and girls and represented a variety of races/ethnicities and ages, which allow for greater generalizability of our findings. However, in the current study, we relied on parents’ reports of their children’s social problems. Although the expected, theory-driven relationships were observed among social problems, negative affect, and LOC eating, since some data suggest that parent report of children’s problems differ from child self-report (Edelbrock, Costello, Dulcan, Conover, & Kala, 1986), future studies should incorporate assessment of social problems from youths’ own perspective, as well. Prior research suggests that children with depressive symptoms also have more negative perceptions of their social abilities (McGrath & Repetti, 2002) which may be observable by their parents, and there is evidence that adults who binge eat may be particularly sensitive to negative social interactions (Steiger, Gauvin, Jabalpurwala, Sequin, & Stotland, 1999). It is therefore possible that the social difficulties observed among youth with LOC may emerge and intensify out of pre-existing tendencies to view circumstances in a negative light. Alternatively, social problems and negative affect may interact cyclically to exacerbate each other. The cross-sectional nature of the study design limits our ability to draw conclusions about the temporal development of these variables. Longitudinal and ecological momentary assessment studies are required to elucidate whether social and interpersonal difficulties are etiologically related to the development of negative affect and subsequent LOC eating behaviors, or rather serve to maintain maladaptive eating patterns once they have begun.
In conclusion, this study provides initial evidence that social problems during youth are related to negative affect, and in turn, LOC eating, thus providing preliminary support for the application of the interpersonal model of BED to LOC eating in youth. In light of the success of interpersonal psychotherapy in decreasing binge eating (Wilfley et al., 2002; Wilson et al., In press), it has been suggested that improving the quality of youth’s social relationships may serve to improve mood and therefore decrease LOC eating behaviors. Such efforts may prevent the progression of disordered eating patterns and further weight gain over time (Tanofsky-Kraff, Wilfley et al., 2007). The results from this study provide preliminary support for such theory and create a foundation for future prospective research in this area.
Acknowledgments
Research support: Intramural Research Program, NIH, grant Z01-HD-00641 (to J. Yanovski) from the NICHD, supplemental funding from NCMHD (to J. Yanovski), NIDDK grant 1R01DK080906-01A1 (to M. Tanofsky-Kraff) and USUHS grant R072IC (to M. Tanofsky-Kraff).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors report no competing interests. J. Yanovski is a commissioned officer in the U.S. Public Health Service, DHHS.
Disclaimer: The opinions and assertions expressed herein are those of the authors and are not to be construed as reflecting the views of USUHS or the U.S. Department of Defense.
References
- Achenbach TM, Edelbrock C. Manual for the Child Behavior Checklist and the Revised Child Behavior Profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- Agras WS, Telch CF. The effects of caloric deprivation and negative affect on binge eating in binge-eating disordered women. Behavior Therapy. 1998;29(3):491–503. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. 4th ed. Washington, D.C.: American Psychiatric Association; 2000. [Google Scholar]
- Arbuckle JL. Amos 5.0 User's Guide. Chicago: SPSS, Inc.; 2003. [Google Scholar]
- Behrens JT. Principles and procedures of exploratory data analysis. Psychological Methods. 1977;2(2):131–160. [Google Scholar]
- Bryant-Waugh R, Cooper P, Taylor C, Lask B. The use of the Eating Disorder Examination with children: A pilot study. International Journal of Eating Disorders. 1996;19(4):391–397. doi: 10.1002/(SICI)1098-108X(199605)19:4<391::AID-EAT6>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- Czaja J, Rief W, Hilbert A. Emotion regulation and binge eating in children. International Journal of Eating Disorders. 2009;42(4):356–362. doi: 10.1002/eat.20630. [DOI] [PubMed] [Google Scholar]
- Edelbrock C, Costello AJ, Dulcan MK, Conover NC, Kala R. Parent-child agreement on child psychiatric symptoms assessed via structured interview. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 1986;31(3):427–436. [PubMed] [Google Scholar]
- Eldredge KL, Agras S. Weight and shape overconcern and emotional eating in binge eating disorder. International Journal of Eating Disorders. 1996;19(1):73–82. doi: 10.1002/(SICI)1098-108X(199601)19:1<73::AID-EAT9>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. The Eating Disorder Examination (12th ed.) In: F CG, W GT, editors. Binge eating, nature, assessment and treatment. New York: Guilford: 1993. pp. 317–360. [Google Scholar]
- Furman W, Buhrmester D. Age and sex differences in the perceptions of networks of personal relationships. Child Development. 1992;63(1):103–115. doi: 10.1111/j.1467-8624.1992.tb03599.x. [DOI] [PubMed] [Google Scholar]
- Gardner RM, Stark K, Friedman BN, Jackson NA. Predictors of eating disorder scores in children ages 6 through 14: A longitudinal study. Journal of Psychosomatic Research. 2000;49(3):199–205. doi: 10.1016/s0022-3999(00)00172-0. [DOI] [PubMed] [Google Scholar]
- Hayden-Wade HA, Stein RI, Ghaderi A, Saelens BE, Zabinski MF, Wilfley DE. Prevalence, characteristics, and correlates of teasing experiences among overweight children vs. non-overweight peers. Obesity Research. 2005;13(8):1381–1392. doi: 10.1038/oby.2005.167. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Baumeister RF. Binge eating as an escape from self-awareness. Psychological Bulletin. 1991;110(1):86–108. doi: 10.1037/0033-2909.110.1.86. [DOI] [PubMed] [Google Scholar]
- Klerman GL, Weissman MM, Rounsaville BJ, Chevron ES. Interpersonal Psychotherapy of Depression. New York: Basic Books; 1984. [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 2nd ed. New York: Guilford Press; 2005. [Google Scholar]
- Kovacs M. The Children’s Depression Inventory (CDI) Psychopharmacology Bulletin. 1995;21:995–998. [PubMed] [Google Scholar]
- Lemeshow AR, Fisher L, Goodman E, Kawachi I, Berkey CS, Colditz GA. Subjective social status in the school and change in adiposity in female adolescents. Archives of Pediatrics and Adolescent Medicine. 2008;162(1):23–28. doi: 10.1001/archpediatrics.2007.11. [DOI] [PubMed] [Google Scholar]
- Libbey HP, Story MT, Neumark-Sztainer D, Boutelle K. Teasing, disordered eating behaviors, and psychological morbidities among overweight adolescents. Obesity. 2008;16(2):S24–S29. doi: 10.1038/oby.2008.455. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7(1):83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39(1):99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall WA, Tanner JM. Variations in pattern of pubertal changes in girls. Archives of Disorders of Childhood. 1969;44(235):291–303. doi: 10.1136/adc.44.235.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall WA, Tanner JM. Variations in pattern of pubertal changes in boys. Archives of Disorders of Childhood. 1970;45(239):13–23. doi: 10.1136/adc.45.239.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masheb RM, Grilo CM. Emotional overeating and its associations with eating disorder psychopathology among overweight patients with binge eating disorder. International Journal of Eating Disorders. 2006;39(2):141–146. doi: 10.1002/eat.20221. [DOI] [PubMed] [Google Scholar]
- McConaughy SH. Advances in empirically based assessment of children's behavioral and emotional problems. School Psychology Review. 1993;22(2):285–307. [Google Scholar]
- McGrath EP, Repetti RL. A longitudinal study of children's depressive symptoms, self-perceptions, and cognitive distortions about the self. Journal of Abnormal Psychology. 2002;111(1):77–87. doi: 10.1037//0021-843x.111.1.77. [DOI] [PubMed] [Google Scholar]
- Nelson TD, Aylward BS, Steele RG. Structural equation modeling in pediatric psychology: Overview and review of applications. Journal of Pediatric Psychology. 2008;33(7):679–687. doi: 10.1093/jpepsy/jsm107. [DOI] [PubMed] [Google Scholar]
- Schutz HK, Paxton SJ. Friendship quality, body dissatisfaction, dieting, and disordered eating in adolescent girls. British Journal of Clinical Psychology. 2007;46(1):67–83. doi: 10.1348/014466506x115993. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Edwards CD, Lushene RE, Montuori J, Platzek D. STAIC Preliminary Manual. Palo Alto, CA: Consulting Psychologists Press; 1973. [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene RE. STAI Manual for the State-Trait Anxiety Inventory ("Self-Evaluation Questionnaire") Palo Alto, CA: Consulting Psychologists Press; 1970. [Google Scholar]
- Steiger H, Gauvin L, Jabalpurwala JR, Sequin JR, Stotland S. Hypersensitivity to social interactions in bulimic syndromes: Relationship to binge eating. Journal of Consulting and Clinical Psychology. 1999;67(5):765–775. doi: 10.1037//0022-006x.67.5.765. [DOI] [PubMed] [Google Scholar]
- Stice E. Review of the evidence of a sociocultural model of bulimia nervosa and an explanation of the mechanisms of action. Clinical Psychology Review. 1994;14(7):633–661. [Google Scholar]
- Stice E, Presnell K, Spangler D. Risk factors for binge eating onset in adolescent girls: A 2-year prospective investigation. Health Psychology. 2002;21(2):131–138. [PubMed] [Google Scholar]
- Sullivan H. The Interpersonal Theory of Psychiatry. New York: W.W. Norton; 1953. [Google Scholar]
- Tanner JM. Growth and maturation during adolescence. Nutrition Reviews. 1981;39(2):43–55. doi: 10.1111/j.1753-4887.1981.tb06734.x. [DOI] [PubMed] [Google Scholar]
- Tanofsky-Kraff M. Binge Eating Among Children and Adolescents. In: Jelalian E, Steele RG, editors. Handbook of Childhood and Adolescent Obesity. Springer US: 2008. [Google Scholar]
- Tanofsky-Kraff M, Goossens L, Eddy KT, Ringham R, Goldschmidt A, Yanovski SZ, et al. A multisite investigation of binge eating behaviors in children and adolescents. Journal of Consulting and Clinical Psychology. 2007;75(6):901–913. doi: 10.1037/0022-006X.75.6.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, McDuffie JR, Yanovski SZ, Kozlosky M, Schvey N, Shomaker LB, et al. Laboratory assessment of the food intake of children and adolescents with loss of control eating. The American Journal of Clinical Nutrition. 2009;89(3):738–745. doi: 10.3945/ajcn.2008.26886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Theim KR, Yanovski SZ, Bassett AM, Burns NP, Ranzenhofer LM, et al. Validation of the Emotional Eating Scale adapted for use in children and adolescents (EES-C) International Journal of Eating Disorders. 2007;40(3):232–240. doi: 10.1002/eat.20362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Wilfley D, Young JF, Mufson L, Yanovski SZ, Glasofer DR, et al. Preventing excessive weight gain in adolescents: Interpersonal psychotherapy for binge eating. Obesity. 2007;15(6):1345–1355. doi: 10.1038/oby.2007.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Yanovski SZ, Schvey NA, Olsen CH, Gustafson J, Yanovski JA. A prospective study of loss of control eating for body weight gain in children at high risk for adult obesity. International Journal of Eating Disorders. 2009;42(1):26–30. doi: 10.1002/eat.20580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Yanovski SZ, Wilfley DE, Marmarosh C, Morgan CM, Yanovski JA. Eating disordered behaviors, body fat, and psychopathology in overweight and normal-weight children. Journal of Counseling and Clinical Psychology. 2004;72(1):53–61. doi: 10.1037/0022-006X.72.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tukey JW. Exploratory Data Analysis. Reading: Addison-Wesley; 1977. [Google Scholar]
- Van Strien T, Engels RC, Van Leeuwe J, Snoek HM. The Stice model of overeating: Tests in clinical and non-clinical samples. Appetite. 2005;45(3):205–213. doi: 10.1016/j.appet.2005.08.004. [DOI] [PubMed] [Google Scholar]
- Wilfley DE, MacKenzie KR, Welch RR, Ayres VE, Weissman MM. Interpersonal Psychotherapy for Group. New York: Basic Books; 2000. [Google Scholar]
- Wilfley DE, Pike KM, Striegel-Moore RH. Towards an integrated model of risk for binge eating disorder. Journal of Gender, Culture, and Health. 1997;2:1–3. [Google Scholar]
- Wilfley DE, Welch RR, Stein RI, Spurrell EB, Cohen LR, Saelens BE, et al. A randomized comparison of group cognitive-behavioral therapy and group interpersonal psychotherapy for the treatment of overweight individuals with binge-eating disorder. Archives of General Psychiatry. 2002;59(8):713–721. doi: 10.1001/archpsyc.59.8.713. [DOI] [PubMed] [Google Scholar]
- Wilfley DE, Wilson GT, Agras WS. The clinical significance of binge eating disorder. International Journal of Eating Disorders. 2003;34 Suppl. 1:S96–S106. doi: 10.1002/eat.10209. [DOI] [PubMed] [Google Scholar]
- Wilson GT, Wilfley DE, Agras WS, Bryson SW. Psychological treatments of binge eating disorder. Archives of General Psychiatry. doi: 10.1001/archgenpsychiatry.2009.170. (In press) [DOI] [PMC free article] [PubMed] [Google Scholar]