Abstract
This study evaluated whether improvements in nicotine withdrawal symptoms (NWS), depression and anxiety are greater for body acupuncture than for sham acupuncture. Smoking volunteers from the public were randomized to receive six sessions of either real or sham acupuncture for 2 weeks. The primary outcome measure was NWS measured by the Minnesota Nicotine Withdrawal Score, and the secondary measures were scores on the Beck Depression Inventory (BDI) and Beck Anxiety Inventory (BAI). Eighty volunteers were randomized into real acupuncture (n = 38) and sham acupuncture (n = 42) groups, of which 46 subjects (22 and 24 in the real and sham acupuncture groups, respectively) completed the treatment and the 2-week follow-up. An intention-to-treat analysis revealed that the NWS did not differ significantly between the real and sham acupuncture groups immediately after the treatment (12.2 ± 9.7 and 12.8 ± 7.7, respectively; mean ± SD) and at the 2-week follow-up (11.7 ± 10.2 and 12.6 ± 7.8). Both groups also showed similar improvements in BDI and BAI scores. These results indicate that the real acupuncture treatment tested in this trial was no more effective than sham acupuncture at reducing NWS, depression and anxiety for smoking cessation.
Keywords: acupuncture, nicotine withdrawal symptoms, smoking cessation, anxiety
Introduction
Smoking kills one in two long-term users, with approximately five million such deaths occurring each year (1). Promoting smoking cessation and treating tobacco dependence can provide both immediate and long-term benefits (2). The most obvious benefits of smoking cessation are improved life expectancy and the reduction of diseases such as cardiovascular disease, cancer and hypertension (3). Smoking imposes a huge economic burden on society, currently representing up to 15% of total health care costs in developed countries. For example, the cost of treating smoking-related diseases in the US and UK is projected to be US$ 97 billion and £1.4 billion, respectively, which includes health care expenditures and lost productivity from deaths and disability (3). Therefore, smoking cessation is expected to also reduce the societal economic burden.
The treatments for smoking cessation include behavioral support, nicotine replacement therapy, bupropion and other drug treatments (4). However, stopping smoking is difficult, mainly due to nicotine withdrawal symptoms (NWS). Complementary therapies are popular and frequently used for tobacco cessation (5), with survey data indicating that hypnosis, relaxation, acupuncture and meditation are the most commonly used (5). This survey also found that 30% of responders were interested in the future use of acupuncture treatment for smoking cessation.
Acupuncture is an important therapeutic modality in traditional Chinese medicine, which involves inserting fine needles into specific points. Acupuncture is now a widely accepted intervention for the treatment of a variety of conditions (6). Several acupuncture techniques have been used to treat smoking cessation, including manual acupuncture, auricular acupuncture and electroacupuncture. The review of Cochrane (7) concluded that there is no consistent evidence that acupuncture is effective for smoking cessation, but methodological problems mean that no firm conclusions can be drawn. Another review (8) also claimed that acupuncture has no therapeutic effects on smoking cessation.
Few clinical trials have directly compared the efficacies of body and sham acupuncture. All previous studies compared body acupuncture as an adjuvant with other acupuncture techniques or other interventions with controls (7). Thus, those trials do not provide direct evidence of the therapeutic effects of body acupuncture on smoking cessation. In the only clinical trial that tested the effects of acupuncture treatments on NWS, White et al. (9) reported that electroauricular acupuncture had no effect on NWS. This indicates the need to assess the evidence for the efficacy of body acupuncture as a smoking cessation treatment, and hence the present study clinically assessed the effectiveness of body acupuncture on NWS, depression and anxiety.
Participants and Methods
Participants
Volunteers who wanted to quit smoking were recruited through local mass media advertising to participate in a 4-week quit-smoking program at the Dunsan Oriental Hospital of Daejeon University in Daejeon, South Korea. Participants were eligible to participate in the program if they: (i) were aged 18–65 years; (ii) smoked ≥10 cigarettes/day for >6 months; (iii) agreed to stop smoking on the quitting date; (iv) had attempted to stop smoking at least once without success; (v) had not received acupuncture for smoking cessation; (vi) had not been diagnosed with psychiatric disease (including alcohol or drug abuse); (vii) were not currently taking medication for chronic obstructive pulmonary disease, hypertension or diabetes mellitus and (h) were not pregnant or attempting to conceive.
Eighty-seven participants screened between August 2006 and December 2006 fulfilled the study criteria, of which 80 signed the consent form. The Institutional Review Board of the University Hospital granted approval for the study before we approached the subjects.
Protocol
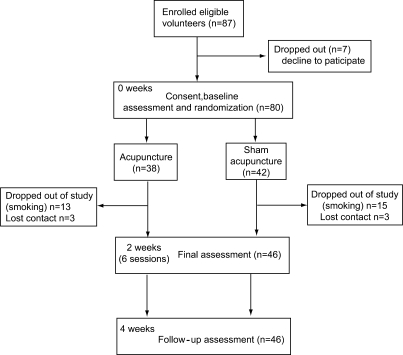
The trial comprised a 2-week intervention and 2-week follow-up (Figure 1). Participants were assessed 1 week before treatment, immediately after treatment (final), and at 2 weeks after the treatment (follow-up).
Figure 1.
Diagram of study design showing the flow of participants.
Randomization and Masking
Following baseline assessment, participants were randomly assigned to receive either real acupuncture (n = 38) or a sham acupuncture control treatment (n = 42). Randomization was performed by the study coordinator according to a computerized list that was stratified using a nicotine-dependence cut-off score on the Fagerstrom Test of 6. The subjects were informed that they would receive one of two types of acupuncture, each of which had the potential to help smoking cessation, but they were no told which treatment they received. Clinical observers assessing the endpoints were blinded to the real and sham acupuncture groups. An independent researcher not involved in eligibility assessment, outcome assessment or treatment kept the concealed assignment scheme in a locked cupboard. Two oriental medical doctors (OMDs), who had worked in Korean traditional medicine for 4 years, were allocated to administer either real or sham acupuncture. They were instructed not to talk with the subjects during any of the treatment sessions.
Intervention
Each patient received six acupuncture sessions. Sessions were scheduled three times weekly for 2 weeks, with each lasting 20 min. All patients were treated in a prone position. Disposable, sterile acupuncture needles (0.3 × 15 mm2, Dongbang Acupuncture Inc., Sungnam-si, South Korea) were used in both the real and sham acupuncture groups.
Traditional Chinese medicine (10) classifies smoking as a heat deficiency related to Kidney and Heart meridians, because the symptoms brought about hot flush, agitation, anxiety, depression and impatient after withdrawal (10). This symptom was treated in the real acupuncture group using the acupuncture points for nourishing yin and tonifying the kidneys, and removing heat from the heart for tranquilization. Therefore, the selected acupuncture points were HT7 (Shenmen, Shu-Stream and Yuan-Primary point of Heart meridian, both), PC7 (Daling, Shu-Stream and Yuan Primary point of Pericardium meridian, both), HT8 (Shaofu, Ying-Spring point of Heart meridian, both), KI3 (Taixi, Shu-Stream and Yuan-Primary point of Kidney meridian, both) and KI6 (Zhaohai, the Eight Confluent point, both), which are all located below the elbow or knee joint and commonly reported as useful for kidney- and heart-related syndromes in textbooks on Acupuncture and Moxibustion (10). Yuan-Primary point is usually selected for tonification or sedation of deficiency or excess of Jang-Fu organs, and Ying-Spring point is usually used for sedating the heat syndromes of related organs (11).
After being inserted into the skin perpendicularly from 0.5 to 1.5 cm depth in each points according to thin or obese, total 10 acupuncture the needles were manipulated in order to produce a needle sensation (De-qi). Manipulations were used as reinforcing and reducing by lifting and thrusting (heavy pressing is reinforcing, while forceful lifting is reducing) or by twirling and rotating 180–360° (the direction of meridian is reinforcing, while against direction is reducing) the needles until participants had experienced the sensation of soreness, numbness or a distending feeling around the point after the needle was inserted to a certain depth. We sedated HT8 and PC7, and tonified HT7, KI3 and KI6 according to the earlier mentioned theory. After arrival of De-qi, the acupuncture needles were retained for a while, and 10 min after the start of treatment, all acupuncture needles were again manipulated by the OMD in the same manner.
In the sham acupuncture control group, participants were treated using non-acupuncture points that were 1 cm away from LI12 (Zhouliao, both), TE11 (Qinglengyuan, both), TE12 (Xiaoluo, both), GB32 (Zhongdu, both) and BL37 (Yinmen, both), which are all located above the elbow or knee joint, and total 10 needles (both side) are inserted under 3 mm perpendicularly into the skin as shallow as possible so as to prevent occurring acupuncture stimulation. The non-acupuncture points used in this study were chosen because they were not related to the condition being treated in the experimental group. Moreover, needling in this group was superficial and exclusively intracutaneous, and the needle sensation (De-qi) was not achieved because there was no use of manipulation technique. The OMD was instructed to avoid any form of manipulation in this group. The therapeutic setting, procedure, and frequency of sessions were similar in both groups except the depth and manipulation technique of the inserted needles. The same acupuncture points were used in all the sessions.
Outcome Measures
Minnesota Nicotine Withdrawal Scale
The Minnesota Nicotine Withdrawal Scale (MNWS) measures certain self-reported tobacco withdrawal symptoms that were validated by Hughes and Hatsukami (12) in 1986. It is used to compare specific withdrawal symptoms and self-reported nicotine withdrawal levels between conditions of acute nicotine deprivation and non-deprivation. The MNWS questionnaire uses a four-point Lickert scale to measure the severity of the following seven withdrawal symptoms: irritability, anxiety, difficulty concentrating, restlessness, insomnia, increased appetite and depressed mood.
Beck Depression Inventory
The Beck Depression Inventory (BDI) is a 21-item self-reported depressive symptoms. Each item consists of four statements, scored from 0 to 3, with a higher score indicating increased symptom severity. Respondents are instructed to respond based on how they have been feeling during the previous week (13,14).
Beck Anxiety Inventory
The Beck Anxiety Inventory (BAI) is a 21-item self-reported inventory designed to assess the severity of the somatic, affective and cognitive components of anxiety in psychiatric populations, with higher scores being indicative of greater anxiety (15,16).
Carbon Monoxide Level
Smoking status was verified using a portable exhaled-CO sensor (Micro Smokerlyzer, Bedfont, Kent, UK), with 8 p.p.m. used as the cut-off to distinguish between current smokers and non-smokers.
Sample Size
We estimated that 22 subjects were required in each group to detect a clinically relevant two-point difference in an MNWS score with a power of 90% and an α-value of 0.05. This magnitude of effect was based on a previous study (9). Assuming a 40% dropout rate, we planned to randomize 37 participants to each group.
Statistical Analysis
The results were statistically analyzed using SAS (Windows version 12). All data satisfied the Kolmogorov–Smirnov normality test. The Wilcoxon rank-sum test and the χ2-test were used to evaluate statistical differences in the demographic data. Two-sample t-tests were used to compare differences between the real and sham acupuncture groups.
Results
Demographic Comparison
The two study groups did not differ significantly at baseline (Table 1). The 2-week program was completed by 46 participants (22 and 24 in the real and sham acupuncture groups, respectively), all of whom remained at the 2-week follow-up. Comparison of the demographic and pre-test data revealed no significant differences between the dropouts and the remaining members of the real and sham acupuncture groups.
Table 1.
Baseline characteristics of the acupuncture (n = 38) and sham acupuncture (n = 42)
| Variable | Acupuncture (n = 38) | Sham acupuncture (n = 42) | P |
|---|---|---|---|
| Gender (M/F) | 36/2 | 39/3 | 0.73 |
| Age, median (IRQ), years | 40.0 (34.0–46.0) | 42.0 (34.0–49.0) | 0.53 |
| Height, median (IRQ), cm | 169.5 (167.0– 175.0) | 168.5 (165.0–172.0) | 0.38 |
| Weight, median (IRQ), kg | 69.0 (61.0–72.0) | 67.5 (62.0–74.0) | 0.86 |
| BMI | 23.2 (21.6– 25.7) | 23.3 (21.8–24.9) | 0.93 |
| Total smoking duration, median (IRQ), years | 20.0 (15.0–28.0) | 22.5 (15.0–30.0) | 0.38 |
| Average smoked amount of cigarette per day, median (IRQ) | 20.0 (20.0–30.0) | 20.0 (20.0–30.0) | 0.88 |
| Previous attempts to stop smoking within 1 year (Yes/No) | 15/23 | 18/24 | 0.36 |
| Advised by physician to stop (Yes/No) | 12/26 | 21/21 | 0.64 |
| Consider smoking antisocial (Yes/No) | 32/6 | 38/4 | 0.80 |
| Concerned about weight gain (Yes/No) | 17/21 | 17/25 | 0.40 |
IRQ, interquartile range.
No Effects on MNWS
The intervention reduced MNWS by 65% and 62% in the real and sham acupuncture groups, respectively, with no significant difference between the two groups (Table 2). MNWS remained significantly lower at follow-up than at baseline in both groups. Similar levels of MNWS were evident in the real (62%) and sham (61%) groups, also with no intergroup differences.
Table 2.
Scores of outcome measures over time according to group allocation using intention to treat analysis
| Mean score (mean ± SD) |
Mean change (mean ± SD) |
Mean difference in change between groups (mean ± SD) | ||||
|---|---|---|---|---|---|---|
| Acupuncture | Sham | Acupuncture | Sham | |||
| MNWS | ||||||
| Baseline | 18.8 ± 8.9 | 20.6 ± 7.3 | − | − | − | |
| Final | 6.6 ± 7.0 | 7.9 ± 7.7 | 12.2 ± 9.7 | 12.8 ± 7.7 | −0.6 ± 9.7 | |
| Follow-up | 7.1 ± 6.8 | 8.1 ± 7.6 | 11.7 ± 10.2 | 12.6 ± 7.8 | −0.9 ± 10.1 | |
| BDI | ||||||
| Baseline | 10.9 ± 7.1 | 9.1 ± 5.1 | − | − | − | |
| Final | 3.8 ± 3.8 | 3.2 ± 4.3 | 7.6 ± 6.2 | 5.8 ± 5.3 | 1.8 ± 6.3 | |
| Follow-up | 3.2 ± 4.4 | 2.3 ± 4.1 | 8.2 ± 7.3 | 6.7 ± 4.8 | 1.5 ± 7.0 | |
| BAI | ||||||
| Baseline | 11.4 ± 8.3 | 9.7 ± 6.6 | − | − | − | |
| Final | 4.5 ± 5.4 | 4.4 ± 3.5 | 5.6 ± 6.1 | 4.6 ± 4.7 | 1.0 ± 6.0 | |
| Follow-up | 3.2 ± 3.0 | 3.6 ± 3.5 | 7.0 ± 7.1 | 5.4 ± 4.4 | 1.6 ± 6.7 | |
MNWS, Minnesota nicotine withdrawal scale; BDI, Beck Depression Inventory; BAI, Beck Anxiety Inventory.
No Effects on Anxiety and Depression
The secondary outcome measures, BDI and BAI scores, also improved significantly compared with baseline in both groups, also with no intergroup differences.
Per-protocol Analysis
When the outcome measures were re-analyzed using only the data from subjects who had completed the trial, MNWS and BDI and BAI scores did not differ between the groups both immediately after the intervention and at the 2-week follow-up.
No Adverse Events
No adverse effects associated with either real or sham acupuncture were reported by the participants.
Discussion
This double-blind (both assessor and patient), placebo-controlled clinical trial investigated the efficacy of body acupuncture on NWS, depression and anxiety during smoking cessation. In our sample of smokers, all of the study measures were improved by both real and sham acupuncture during short-term smoking cessation. However, real acupuncture was no better than sham acupuncture, which is consistent with results obtained for the effects of electroauricular acupuncture on NWS (9). However, the present study is the first randomized clinical trial to produce this result whilst using a sham acupuncture control group. Moreover, our finding of no difference between the groups in NWS, depression and anxiety suggests that the effects of body acupuncture are non-specific.
There are several possible reasons for the absence of a difference between real and sham acupuncture in reducing NWS found in the present study. The first possible reason is the short treatment and follow-up times, since a 6-month follow-up is generally needed to properly judge the success rate of smoking cessation (17). We may also have used very few treatment sessions. Indeed, the lack of information on required doses is a frequently noted limitation of acupuncture research (18,19).
The second possible reason is that the stimulation was insufficient to induce secretion. We used short acupuncture needles (15 mm), in order to reduce depth differences between the sessions. However, this might have evoked insufficient De-qi. For more precise stimulation, future trials should include an electroacupuncture treatment group so as to remove this shortcoming of manual acupuncture.
Third, the protocol applied in the real acupuncture group might not have been suitable for reducing NWS, even though it was selected based on acupuncture textbook. Moreover, White et al. (9) noted that using non-meridian acupuncture points may not be an appropriate control procedure. We used control points away from major acupuncture points because they produced smaller physical effects. A recent review (19) analyzed the dependency of points chosen in auricular acupuncture studies, and suggested that the treatment at correct points probably does not differ from treatment at incorrect (sham) points. There has been no equivalent analysis of the difference between real penetration and fake penetration. It is possible that even minimal penetration of the skin can affect the brain, stimulate neurotransmitters or have a psychological impact. The effects may be psychological or non-specific rather than neuronal, and several studies have found significant differences in electric conductivity between meridian and non-meridian points (20–22).
The fourth possible reason is the absence of testing success of blinding of the treatment. All of the participants had received acupuncture previously, which is a limitation of many studies due to the difficulty of obtaining Koran subjects who have not received acupuncture. We therefore only included subjects who had not received acupuncture for smoking cessation, and hence the patients were not truly blind to the procedure. To account for the placebo effect, it is crucial for the sham procedure to be indistinguishable from the real treatment, and this is virtually impossible in assessments of acupuncture due to possible psychological effects. Therefore, the adequacy of blinding procedures should be assessed in future studies.
The fifth possible reason for the absence of a difference between our study groups is the high dropout rate, which is a common complication of research into substance abuse (18). We used a conservative method to allocate values for missing data in our intention-to-treat analysis, and the effect of the dropouts is unknown. However, when reanalyzing the data on a per-protocol method, similar results were found both immediately after the treatment and at the 2-week follow-up. These results suggest that placebo effects are likely to be maintained once in contact with the OMD has ceased. Moreover, the non-specific effects appeared to be unrelated to interactions between therapists and subjects. However, even in the absence of significant differences between the two groups and with our calculation of the results based on intention to treat, it is still possible that type II errors occurred (18).
Acupuncture is a potentially useful treatment option for smoking cessation, especially NWS, and its possible mechanism of action is of interest. Regular stimulation of appropriate acupuncture points affects the nerve systems that regulate neurotransmitters, including dopamine via GABA, β-endorphin and norepinephrine, and neural activity in the nucleus accumbens (23). It may also directly affect the desire to smoke (24).
In conclusion, our results suggest that improvements in NWS, depression and anxiety during smoking cessation are the same for real and sham acupuncture. However, this study was subject to several limitations, including the short treatment duration and possibilities of inadequate blinding and insufficient stimulation at the acupuncture points. Further randomized studies employing larger samples, measurements after multiple sessions and long-term follow-up are needed to verify the effects of body acupuncture with or without electric stimulation on psychological variables and nicotine-dependence improvement.
Acknowledgements
The authors specially thank Dr Byung-Cheul Shin in Wonkwang University, South Korea for his helpful comments about this study. This study was supported by the Acupuncture, Moxibustion and Meridian Research Project (K06070) of Korea Institute of Oriental Medicine in 2006.
References
- 1.World Health Organization. The Millennium Development Goals and Tobacco Control. Geneva, Switzerland: World Health Organization; 2004. [Google Scholar]
- 2.World Health Organization. Policy Recommendations for Smoking Cessation and Treatment of Tobacco Dependence. Geneva, Switzerland: World Health Organization; 2003. [Google Scholar]
- 3.Parrott S, Godfrey C. Economics of smoking cessation. Br Med J. 2004;328:947–9. doi: 10.1136/bmj.328.7445.947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Srivastava P, Currie GP, Britton J. Smoking cessation. Br Med J. 2006;332:1324–6. doi: 10.1136/bmj.332.7553.1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sood A, Ebbert JO, Sood R, Stevens SR. Complementary treatments for tobacco cessation: a survey. Nicotine Tob Res. 2006;8:767–71. doi: 10.1080/14622200601004109. [DOI] [PubMed] [Google Scholar]
- 6.Ernst E. Acupuncture—a critical analysis. J Intern Med. 2006;259:125–37. doi: 10.1111/j.1365-2796.2005.01584.x. [DOI] [PubMed] [Google Scholar]
- 7.White AR, Rampes H, Campbell JL. Acupuncture and related interventions for smoking cessation. Cochrane Database Syst Rev. 2006 doi: 10.1002/14651858.CD000009.pub2. Art. No.: CD000009. doi: 10.1002/14651858.CD000009.pub2. [DOI] [PubMed] [Google Scholar]
- 8.The Bandolier team. Acupuncture to stop smoking. Bandolier. 2002. p. 72. (available at: http://www.jr2.ox.ac.uk/bandolier/band72/b72-5.html)
- 9.White AR, Resch KL, Ernst E. Randomized trial of acupuncture for nicotine withdrawal symptoms. Arch Intern Med. 1998;158:2251–5. doi: 10.1001/archinte.158.20.2251. [DOI] [PubMed] [Google Scholar]
- 10.Acupuncture and Mixubustion of University Association of Korea. Acupuncture and Mixubustion. Seoul, Korea: Jibmoondang; 1988. pp. 182–205. [Google Scholar]
- 11.Xing C. Chinese Acupuncture and Moxibustion. Beijing, China: Foreign Languages Press; 1987. p. 134. 57, 82–3, 91, 95, 96, 207, 327–29. [Google Scholar]
- 12.Hughes JR, Hatsukami D. Signs and symptoms of tobacco withdrawal. Arch Gen Psychiatry. 1986;43:289–94. doi: 10.1001/archpsyc.1986.01800030107013. [DOI] [PubMed] [Google Scholar]
- 13.Beck AT, Steer RA, Garbin MG. Psychosometric properties of the Beck Depression Inventory: 25 years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- 14.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 15.Beck AT, Brown G, Epstein N, Steer RA. An inventory for measuring anxiety: psychosometric properties. J Consult Clin Psychol. 1988;55:893–7. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 16.Beck AT, Steer RA. Relationship between Beck Anxiety Inventory and the Hamilton Anxiety Rating Scale with anxious outpatients. J Anxiety Disord. 1991;5:142–6. [Google Scholar]
- 17.Kang HC, Shin KK, Kim KK, Youn BB. The effects of the acupuncture treatment for smoking cessation in high school student smokers. Yonsei Med J. 2005;46:206–12. doi: 10.3349/ymj.2005.46.2.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Margolin A. Acupuncture for substance abuse. Curr Psychiatry Rep. 2003;5:333–9. doi: 10.1007/s11920-003-0065-6. [DOI] [PubMed] [Google Scholar]
- 19.White A, Moody R. The effects of auricular acupuncture on smoking cessation may not depend on the point chosen—an exploratory meta-analysis. Acupunct Med. 2006;24:149–56. doi: 10.1136/aim.24.4.149. [DOI] [PubMed] [Google Scholar]
- 20.Chen KG. Electric properties of meridians. IEEE Eng Med Biol Mag. 1996;15:58–63. [Google Scholar]
- 21.Lee MS, Jeong SY, Lee YH, Jeong DM, Eo YG, Ko SB. Differences in electrical conduction properties between meridians and non-meridians. Am J Chin Med. 2005;33:723–8. doi: 10.1142/S0192415X05003405. [DOI] [PubMed] [Google Scholar]
- 22.Lu WA, Tuesi JJ, Chen KG. Preferential direction and symmetry of electric conduction of human meridians. IEEE Eng Med Biol Mag. 1999;18:76–8. doi: 10.1109/51.740987. [DOI] [PubMed] [Google Scholar]
- 23.Yeom MJ, Lee HJ, Shim IS, Park HJ, Hahm DH. Neural mechanism of acupuncture therapy for aiding in smoking cessation. Kor J Meridian Acupoint. 2007;24:13–25. [Google Scholar]
- 24.He D, Medbo JI, Hostmark AT. Effect of acupuncture on smoking cessation or reduction: an 8-month and 5-year follow-up study. Prev Med. 2001;33:364–72. doi: 10.1006/pmed.2001.0901. [DOI] [PubMed] [Google Scholar]