Abstract
The usefulness of acupuncture (AP) as a complementary and/or alternative therapy in animals is well established but more research is needed on its clinical efficacy relative to conventional therapy, and on the underlying mechanisms of the effects of AP. Cardiac magnetic resonance imaging (CMRI), an important tool in monitoring cardiovascular diseases, provides a reliable method to monitor the effects of AP on the cardiovascular system. This controlled experiment monitored the effect electro-acupuncture (EA) at bilateral acupoint Neiguan (PC6) on recovery time after ketamine/xylazine cocktail anesthesia in healthy cats. The CMRI data established the basic feline cardiac function index (CFI), including cardiac output and major vessel velocity. To evaluate the effect of EA on the functions of the autonomic nervous and cardiovascular systems, heart rate, respiration rate, electrocardiogram and pulse rate were also measured. Ketamine/xylazine cocktail anesthesia caused a transient hypertension in the cats; EA inhibited this anesthetic-induced hypertension and shortened the post-anesthesia recovery time. Our data support existing knowledge on the cardiovascular benefits of EA at PC6, and also provide strong evidence for the combination of anesthesia and EA to shorten post-anesthesia recovery time and counter the negative effects of anesthetics on cardiac physiology.
Keywords: acupoint, anesthesia, cats, CFI, CMRI, electro-acupuncture (EA), Neiguan, PC6
Introduction
Acupuncture (AP) is being used more frequently as a complementary and/or alternative medicine in clinical medicine in humans (1) and animals (2–4). Used to cure or prevent many ailments, especially pain, in animals and humans, AP has been shown to be effective in neurological and cardiovascular disorders also (5–6). Ancient texts on traditional Chinese medicine (TCM) mention the importance of AP and other modalities to enhance cardiac function (7–8). Modern research has studied extensively the beneficial effect of AP on cardiovascular system (9–10). Research suggests that AP at specific acupoints has antihypertensive effects and can prevent cardiac muscle hypertrophy (11–12). Acupoint Neiguan (PC6) is effective in manipulating cardiac functions (13–16). Apart from clinical outcomes, the relative unavailability of high-tech instruments to monitor cardio-physiology has led to much speculation as to the mechanisms of AP that cause those beneficial effects on heart functions. However, the advent of new technologies, like magnetic resonance imaging (MRI), has made it easier to monitor cardiac functional parameters (17–18).
Aside from being non-invasive, cardiac magnetic resonance imaging (CMRI) has the intrinsic benefit of providing a spatially defined three-dimensional dataset with a high degree of accuracy and reproducibility (19,20). In cats, clinical cardiac examination is tricky because environmental effects influence blood pressure and heart rate (21–22). Limited availability of data on heart rate variability in pet cats (23) also is a good reason to research the cardiovascular functional index (CFI) of cats. As is the case in other species, anesthetic administration to cats may compromise normal cardiovascular function (24–25). AP analgesia has been used extensively in animal surgery to replace or minimize the doses of anesthetic needed, thereby, to minimize associated complications (26–27). In ancient literatures of TCM, the heart function could be modulated by acupuncture stimulation on acupoint PC6. Recently, accumulating scientific evidence showed that stimulation on acupoint PC6 could modulate the cardiovascular functions, possibly through the activation of rostro-ventrolateral medulla area (12,28–29). Accordingly, we chose PC6 as the target acupoint in this study.
Materials and Methods
Cats
Twelve cats (8 male and 4 female, 3.5 (range 2.5–7 year) were included in this study. All had a veterinary health check and were found to be healthy. The cats were housed under standard university conditions in the experimental animal house of the National Taiwan University (NTU) Animal Hospital.
Animal Preparation before Scanning
The 12 cats were initially treated with atropine sulfate (0.05 mg kg−1 body weight, subcutaneously) and then anesthetized with a ketamine/xylazine cocktail (10–25 mg kg−1 body weight; ketamine hydrochloride: 2.5 mg kg−1 xylazine hydrochloride, both injected intramuscularly). A quadrature surface RF coil was placed above the area of the cat pleural cavity. The cardiac images and other parameters were observed 15 min after the cats were anesthetized. Then, a HANS Electro-acupuncture (EA) instrument was used to give EA stimulation at bilateral PC6. A stainless steel AP needle (30 gauge, 1.0 inch long) was inserted to a depth of about 20 mm at each PC6 (proximal to the carpus, on the medial face of the forearm, between the tendons of palmaris longus and flexor carpi radialis muscles). Two electrical leads from the HANS EA meter were connected to the two inserted needles and the instrument turned on at an output of 3 mA, and frequency 2/100 Hz (Six seconds as a cycle, the first 3 s belong to 100 Hz and the last 3 s belong to 2 Hz.) for 20 min. The second data set of cardiac images and other parameters were recorded again after that. The rationale of using 2/100 Hz, alternatively, was to avoid nerve tolerance induced by continuous nerve stimulation by a fixed frequency, while optimal current was determined by the observation of slight repetitive palm flexion during electrical stimulation.
Blood Pressure Measurement
This measurement aimed to find how systolic and diastolic pressures responded 30, 60, 90 and 120 min after anesthesia in normal healthy cats and also to record those pressure changes 30, 60, 90 and 120 min after EA applying for 20 min at bilateral PC6. Systolic and diastolic blood pressures of the 12 cats were measured electronically (Model CAS740 Monitor; MAXNIBP™) after anesthetic administration and EA applied to bilateral PC6. First, we place the cats in a comfortable position. Depending on the circumference of the antebrachium, select the correct size cuff for the cat. The cuff was wrapped around the middle part of the antebrachium. Then connect the cuff to the end of the monitor's inflation tubing. Finally, connect the inflation tubing to the NIBP connector, located on the left side of the monitor. Press the START pushbutton to begin the measurement. During BP measurements, the antebrachium was maintained at the level of the heart.
Cardiac Magnetic Resonance (CMR) Data Acquisition Protocol
Cardiac imaging was preformed on a 3 Tesla SIEMENS MRI machine connected by a cardiac phase-array synergy coil. Flowing survey scan, true fast imaging with steady-state precession (FISP) cine MR imaging sequence in the axial, coronal, sagittal, two-chamber, and four-chamber plane were acquired to allow planning of the short-axis orientation. The data set of cardiac parameters covering the left ventricle (LV) in 10–14 short axis slices from apex to base were then recorded on a conventional electrocardiogram (ECG)-triggered (repetition time, TR 18.7 ms; echo time, TE 1.87 ms, flip angle of 60°, spatial resolution 208 × 256 matrix, 4-mm slice-thickness, field of vision (FOV) 179 × 220 mm, 10–15 heart phase/image over 10–15 heart beats).
Data Analysis
Using commercially available analysis software (Matlab Set Software®), image analysis was performed off-line. For volume measurements, endocardial contours were traced manually at end-diastole and end-systole. As imaging was triggered on the R-wave in the sequence, the first phase of each slice was taken as end-diastole. End-systole was defined as the phase with the smallest total LV volume. The LV end-diastolic volume (EDV) and LV end-systolic volume (ESV) were computed using Simpson's method by multiplying the measured areas with the sum of slice thickness and inter-slice gaps. Ejection fraction (EF) was determined as {[(EDV − ESV)/EDV] × 100%}. For measurements of LV mass, the epicardial borders were traced in end-diastole and the LV mass was calculated as 1.05 × (epicardial volume − endocardial volume).The data of CFI were collected 5–10 min and 60 min after anesthesia in normal healthy cats and those changes were also recorded just after EA applying for 20 and 40 min after EA applying for 20 min at bilateral PC6.
Statistical Analysis
For testing the effect of time, we used two-way analysis of variance (two-way ANOVA) with cats as block, and using Scheffe post-hoc test to compare the mean difference between pairwise of time-points (30, 60, 90 and 120 min) by treatments (Anesthesia and EA) on pulse, systolic pressure (Sys), diastolic pressure (Dia) and mean arterial pressure(Map) responses. For testing the treatment effect, we used paired t-test to compare the mean difference between anesthesia and EA treatment group at time-points of 30 and 90 min on Pulse, Sys, Dia and Map responses. The 30 min was the first observation time-point after treatment, and the time-point of 90 min was the significant differentially changed time-point within both treatment groups on Pulse, Sys, Dia, and Map responses exception for the Dia of anesthesia though Scheffe post-hoc test. At the part of EDV, ESV, EF, LVPER, LVPFR, nPER and nPFR responses, we used paired t-test to compare the mean difference between pairwise of time-points (5–10/20/60 min) by treatment. We also used paired t-test to compare the mean difference between anesthesia and EA treatment group at 60 min after anesthesia. The data processing was completed with the computer program of SAS (Statistical Analysis System, version 9.1).
Results
Changes in Blood Pressure
Mean Levels of Pulse, Systolic Pressure, Diastolic Pressure and Mean Arterial Pressure
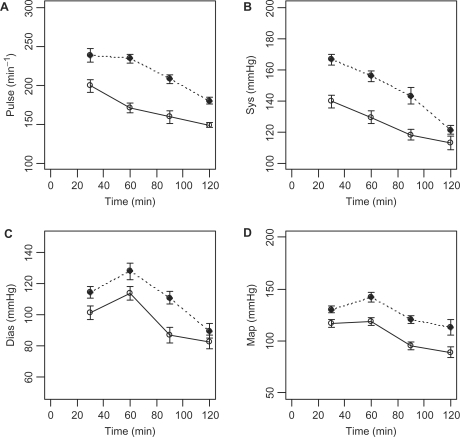
Within the anesthesia treatment group, the mean levels of pulse and systolic pressure at time-points after 90 min were significant by lower than that of 30 min. Within the EA treatment group, the mean levels of pulse and systolic pressure at time-points after 60 min were significantly lower than that of 30 min. Within the anesthesia treatment group, the mean levels of diastolic pressure and mean arterial pressure at time-point 90 min and 30 min were insignificant. Within the EA treatment group, the mean levels of diastolic pressure and mean arterial pressure at time-point after 90 min were significantly lower than that of 30 min (Table 1). No matter anesthesia or EA treatment group, the sample mean levels of pulse and systolic pressure showed monotone decreasing trend with the increasing of time (Table 1 and Fig. 1 (A)–(B)). Although the highest sample mean levels of diastolic pressure and mean arterial pressure were found at the 60 min, the Scheffe post-hoc test showed that the mean levels of diastolic pressure and mean arterial pressure were not significant between 30 and 60 min (Table 1 and Figs 1 (C)–(D)).
Table 1.
Time effect analysis of pulse, systolic pressure (Sys), diastolic pressure (Dia), and mean arterial pressure (Map) by treatment
| Variable | Treatment | Time point | Mean | Scheffe groupinga | Minimum significant difference of Scheffe test at 5% significance level |
|---|---|---|---|---|---|
| Pulse | Anesthesia | 30 | 238.4 | A | 21.3 |
| 60 | 234.1 | A | |||
| 90 | 208.3 | B | |||
| 120 | 179.8 | C | |||
| EA | 30 | 199.3 | A | 21.1 | |
| 60 | 170.9 | B | |||
| 90 | 159.3 | BC | |||
| 120 | 148.9 | C | |||
| Sys | Anesthesia | 30 | 166.6 | A | 14.6 |
| 60 | 155.9 | AB | |||
| 90 | 143.3 | B | |||
| 120 | 121.3 | C | |||
| EA | 30 | 139.6 | A | 9.2 | |
| 60 | 129.3 | B | |||
| 90 | 118.3 | C | |||
| 120 | 113.1 | C | |||
| Dia | Anesthesia | 30 | 114.6 | A | 17.4 |
| 60 | 128.1 | A | |||
| 90 | 111.1 | A | |||
| 120 | 89.8 | B | |||
| EA | 30 | 101.5 | A | 14.1 | |
| 60 | 113.8 | A | |||
| 90 | 87.0 | B | |||
| 120 | 82.8 | B | |||
| Map | Anesthesia | 30 | 130.3 | AB | 21.3 |
| 60 | 142.2 | A | |||
| 90 | 120.3 | B | |||
| 120 | 112.9 | B | |||
| EA | 30 | 116.9 | A | 15.7 | |
| 60 | 118.8 | A | |||
| 90 | 95.3 | B | |||
| 120 | 89.1 | B |
aThe time effects are non-significant at 5% level with the same alphabet; while they are significant at 5% level with different alphabet.
Figure 1.
Time curve by treatment group of mean responses on (A) Pulse, (B) Systolic pressure, (C) Diastolic pressure, and (D) Mean arterial pressure. Dot line: Anesthesia; Solid line: EA; Error bar represent the SEM.
Mean Difference between Anesthesia and EA Treatment
The mean difference between anesthesia and EA treatment of pulse, systolic pressure, diastolic pressure and mean arterial pressure at 30 and 90 were all significantly different (P < 0.05). For example, the pulse values of anesthesia and EA treatment were 238.4 and 199.3 (Mean) at 30 min, and the mean difference between anesthesia and EA treatment was 39.1. It is significant at P = 0.013 by the paired t-test. The mean pulse difference increased to 49.0 between anesthesia and EA treatment at 90 min with P < 0.001. The other three response variables showed similar tendency and are reported in Table 2.
Table 2.
Treatment effect analysis of pulse, systolic pressure (Sys), diastolic pressure (Dia) and mean arterial pressure (Map) at 30 and 90 min
| Time point (min) | Variable | Treatment | Mean | Mean difference | SEM of difference | Paired t-test P-value |
|---|---|---|---|---|---|---|
| 30 | Pulse | Anesthesia | 238.4 | 39.1 | 13.2 | 0.013 |
| EA | 199.3 | |||||
| Sys | Anesthesia | 166.6 | 27.0 | 3.9 | <0.001 | |
| EA | 139.6 | |||||
| Dia | Anesthesia | 114.6 | 13.1 | 5.3 | 0.032 | |
| EA | 101.5 | |||||
| Map | Anesthesia | 130.3 | 13.3 | 2.9 | 0.001 | |
| EA | 116.9 | |||||
| 90 | Pulse | Anesthesia | 208.3 | 49.0 | 9.3 | <0.001 |
| EA | 159.3 | |||||
| Sys | Anesthesia | 143.3 | 25.0 | 4.5 | <0.001 | |
| EA | 118.3 | |||||
| Dia | Anesthesia | 111.1 | 24.1 | 4.1 | <0.001 | |
| EA | 87.0 | |||||
| Map | Anesthesia | 120.3 | 24.9 | 3.2 | <0.001 | |
| EA | 95.3 |
Cardiac Imaging
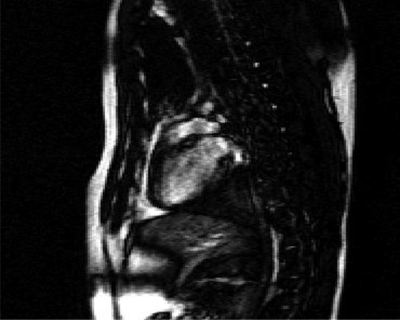
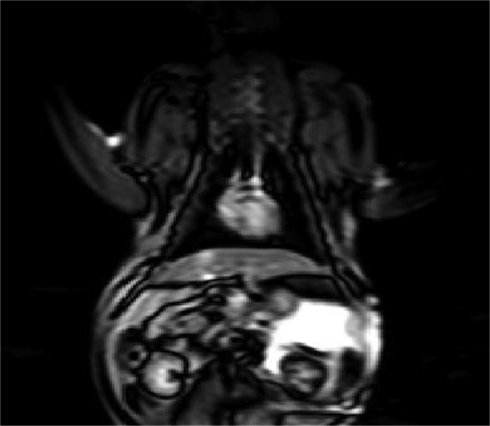
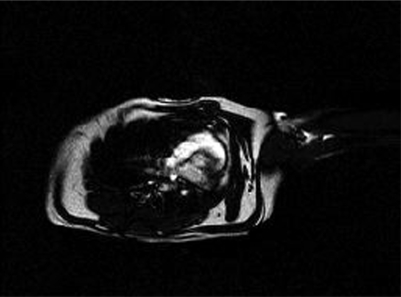
CMRI allows for non-invasive visualization of the heart with high spatial and temporal resolution. The MR parameters for cardiac functional MRI were: True FISP cine MR imaging with field view of 179 × 220 mm2 and 208 × 256 data matrix; TE = 1.87 ms, image TR = 18.7 ms. The sagittal, coronal, and axial section of the cardiac MRI is as shown in Figs 2, 3, and 4.
Figure 2.
Sagittal section MRI of the feline heart.
Figure 3.
Coronal section MRI of the feline heart.
Figure 4.
Axial section MRI of the feline heart.
Changes in CFI
On the responses of EDV, ESV, EF, LVPER, LVPFR, nPER and nPFR, anesthesia group showed significant decreasing of mean levels from 5–10 to 60 min (P < 0.05). Within the EA group, the responses of EDV, ESV, LVPER, LVPFR, and nPER showed significantly decreasing of mean levels from 20 to 60 min (P < 0.05). However, within the EA group, the responses of EF and nPFR showed non-significant mean levels between 20 and 60 min (Table 3). On the responses of EDV, ESV, LVPER, LVPFR and nPER, anesthesia and EA group showed significantly different mean levels at 60 min (P < 0.05). However, the responses of EF and nPFR showed non-significant difference of mean levels at 60 min (Table 4).
Table 3.
Time effect analysis of EDV, ESV, EF, LVPER, LVPFR, nPER, and nPFR by treatment
| Variable | Treatment | Time | Mean | Mean difference | SEM of difference | Paired t-test P-value |
|---|---|---|---|---|---|---|
| EDV | Anesthesia | 5–10 | 4.26 | 1.56 | 0.20 | <0.001 |
| 60 | 2.70 | |||||
| EA | 20 | 2.69 | 0.74 | 0.14 | <0.001 | |
| 60 | 1.94 | |||||
| ESV | Anesthesia | 5–10 | 1.75 | 0.93 | 0.14 | <0.001 |
| 60 | 0.82 | |||||
| EA | 20 | 0.81 | 0.31 | 0.04 | <0.001 | |
| 60 | 0.49 | |||||
| EF | Anesthesia | 5–10 | 0.56 | −0.17 | 0.03 | <0.001 |
| 60 | 0.73 | |||||
| EA | 20 | 0.71 | −0.05 | 0.03 | 0.139 | |
| 60 | 0.76 | |||||
| LVPER | Anesthesia | 5–10 | −30.22 | −4.16 | 0.98 | 0.001 |
| 60 | −26.06 | |||||
| EA | 20 | −25.19 | −2.89 | 1.06 | 0.020 | |
| 60 | −22.30 | |||||
| LVPFR | Anesthesia | 5–10 | 44.55 | 11.30 | 1.80 | <0.001 |
| 60 | 33.25 | |||||
| EA | 20 | 32.33 | 5.66 | 1.40 | 0.002 | |
| 60 | 26.67 | |||||
| nPER | Anesthesia | 5–10 | −7.26 | 2.68 | 0.36 | <0.001 |
| 60 | −9.94 | |||||
| EA | 20 | −9.83 | 1.72 | 0.49 | 0.005 | |
| 60 | −11.55 | |||||
| nPFR | Anesthesia | 5–10 | 10.89 | −2.30 | 0.34 | <0.001 |
| 60 | 13.19 | |||||
| EA | 20 | 12.24 | −1.56 | 0.73 | 0.057 | |
| 60 | 13.80 |
Table 4.
Treatment effect analysis of EDV, ESV, EF, LVPER, LVPFR, nPER, and nPFR at 60 min
| Variable | Treatment | Mean | Mean difference | SEM of difference | Paired t-test P-value |
|---|---|---|---|---|---|
| EDV | Anesthesia | 2.70 | 0.76 | 0.12 | <0.001 |
| EA | 1.94 | ||||
| ESV | Anesthesia | 0.82 | 0.32 | 0.05 | <0.001 |
| EA | 0.49 | ||||
| EF | Anesthesia | 0.73 | −0.04 | 0.03 | 0.233 |
| EA | 0.76 | ||||
| LVPER | Anesthesia | −26.06 | −3.76 | 1.00 | 0.003 |
| EA | −22.30 | ||||
| LVPFR | Anesthesia | 33.25 | 6.59 | 1.76 | 0.003 |
| EA | 26.67 | ||||
| nPER | Anesthesia | −9.94 | 1.61 | 0.50 | 0.008 |
| EA | −11.55 | ||||
| nPFR | Anesthesia | 13.19 | −0.61 | 0.77 | 0.445 |
| EA | 13.80 |
Temporal Parameters with respect to Anesthesia and EA
In healthy cats, all the seven heart functional parameters shortly after anesthetics and 1 h later showed highly significant differences (P < 0.01) (Table 3). Using EA for 20 and 40 min after EA applying for 20 min, except for the functional parameters of EF and nPFR, they all showed highly significant differences (P < 0.01) (Table 3). The data showed that the mean parameters of 60 min after anesthesia were much the same as EA that had been applied for 20 min (Table 3) and meant EA at PC6 could shortened post-anesthesia recovery time to normal. No statistical differences were found between 60 min after anesthesia and 40 min after EA application for 20 min in EF and nPFR, but statistically significant differences were obtained from the other five parameters (P < 0.01) (Table 4).
Discussion
MRI is based on the principle of nuclear magnetic resonance and has intrinsic attributes well suited for cardiac imaging (18). Simpson's algorithm from three-dimensional data as a series of thin slices with no geometric assumptions enables CMRI to obtain actual myocardial mass and volumes. This experiment adopted this modern technique to evaluate the beneficial role of EA at PC6. EA was applied as an important tool in this experiment and has been widely used to build a research model for better understanding of how it affects on different organs or systems, such as to objectify the amount of acupuncture stimulation on an experimental animal model of collagen-induced arthritis (30) and to be an effective alternative or complementary therapy in the relief of pain during labor (31). Some researchers also believed stimulation of real acupuncture points with EA elicited significant activation over the hypothalamus, primary somatosensory motor cortex and rostral anterior cingulated cortex (32).
The Neiguan point (PC6), well known in the West, is the precise cutaneous point for treatment of various ailments by stimulation through neurogenic mechanisms. Several studies showed the beneficial effects of EA at Neiguan point on the cardiovascular variables in different animals (12–16). In the Zhou's study (12), he found that 30 min of low-current, low-frequency (0.3–0.5 mA, 2 Hz), EA, at Jianshi-Neiguan (PC5–6), significantly decreased reflex pressor responses by 40% in rats. Kong Suming (13) reported that EA of Neiguan could stabilize cardiovascular parameters disturbed by asphyxia in rats. During the period of asphyxia, overshoot of LVP (left ventricular pressure) decreased from 55.4 ± 4.7 mmHg of the control to 22.9 ± 11.0 mmHg (P < 0.05) for 10-min period of acupuncture and 20.9 ± 8.8 mmHg (P < 0.02) for 15-min period. The onset of heart rate decrease was postponed from 29.3 ± 3.6 s of the control to 33.3 ± 3.9 s (P < 0.02) and the period of the heart rate decrease was shortened from 29.5 ± 3.5 s to 19.6 ± 4.4 s (P < 0.02) for 10-min of acupuncture. According to Jin's experience (14), 68% of the 28 NST (nucleus of solitary tract) neurions had decreasing discharge frequencies after bilaterally EA at Neiguan in rabbits and suggesting that EA may affect the cardiovascular reflex activities. Syuu (15) had demonstrated that Neiguan EA at 40 Hz increase mean arterial pressure, end-diastolic volume, heart rate, and end-systolic pressure by 10–15%, especially end- systolic elastance by 40% (P < 0.05) over 15 to 60 min. in anesthetized open-chest dogs. Tsou's research (16) on rats showed that there were significant reductions in cardiac enzymes (CPK, CK-MB), the duration of arrhythmia and mortality rate that were either pre-conditioned or treated with EA on PC6, compared with those that did not undergo EA on PC6 (P < 0.05). Demonstrating that EA on PC6 (Neiguan) possesses not only treatment effects, but also preventive effects against myocardial I/R injury.
The CMRI data provide an accurate and reproducible measurement of ejection fraction, ventricular volumes, and ventricular function in cats after anesthesia and EA. Excellent animal restraint is essential but difficult when using machines that refute complete immobilization. Therefore, all cats in this experiment were monitored under general anesthesia and we could not record CMRI data from non-anesthetized cats for comparative purposes. Anesthesia using a ketamine/xylazine cocktail had some effect on cardiovascular physiology (25). Our data confirmed that anesthesia caused a transient hypertension in cats; blood pressure increased initially and then subsided slowly after 30 min. Few data regarding heart rate variability in pet cats are available (23,33). The sensitive nature of cats to changes in heart rate and rhythm, even under minor change of external environments (34), demand the establishment of reliable reference indices of cardiac function. Thus, we recorded CFI for our cats, immediately after anesthesia, and 1 h later. However, the result obtained was not significantly different. This suggests the need for more research with sensitive instruments to monitor changes and establish reference values.
This research used CMRI to monitor the blood pressure and CFI changes in response to EA at PC6. The data show that EA significantly shortened the post-anesthesia recovery time to that of control condition. The beneficial effect of EA at PC6 on cardiovascular function and the reduced post-anesthesia recovery time are most likely due to improved cardiac functional parameters. However, Li (35) reported no hypotensive effect of EA in anesthetized dogs, whereas we found a highly significant (P < 0.01) hypotensive effect in anesthetized cats. This may be due to a species difference, or differences in experimental technique and/or the nature of the anesthetics used.
PC6 is located close to the median nerve, which contains both myelinated and unmyelinated fibers that have been postulated to affect cardiovascular physiology by various mechanisms. The hypotensive (antihypertensive) effect of EA in cats is probably due to inhibition of arterial chemoreceptor pressure reflexes, rather than to activation of baroreceptor reflexes (36). Li, 2002 (35), explained the neural pathway of EA activation through nucleus arcautus (ARC) in the hypothalamus that, in turn, sends excitatory projections to the ventral periaqueduct gray (vPAG), and finally to the nucleus raphe obscurus (NRO). The beneficial effect of EA at PC6 on hypertension, cardiac ischemia, and arrhythmias is achieved by reduced sympathetic outflow, due to excitation of NRO neurons that inhibit cardiovascular neurons in the rostral ventrolateral medulla (rVLM) that activates the opioid, GABA, and 5-HT receptors. The role of opioid release from the central nervous system (37) and cardiovascular reflex changes (14) are assumed to have physiological roles in achieving the effect of EA on PC6. However, as in other AP research, conclusions from the studies of AP in cardiac physiology also are inconsistent and the mechanisms are not fully understood (10). Nevertheless, our data show that the CFI of anesthetized cats treated with EA were better than that of anesthetized cats alone.
Our data support existing knowledge on the cardiovascular benefits of EA at PC6, and also provide strong evidence for the combination of anesthesia and EA to shorten post-anesthesia recovery time and counter the negative effects of anesthetics on cardiac physiology. Also, the data show that the improvement in the CFI due to EA at PC6 was the underlying mechanism to shorten post-anesthetic recovery time and inhibit post-anesthetic hypertension in cats. We also suggest that EA at PC6 may help to improve cardiac functional parameters in conditions of heart disease, as several published clinical reports indicate. However, more research in cats under various conditions is needed before we can draw definite conclusions on the effect of EA at PC6 on cardiovascular physiology and the exact mechanisms involved.
Acknowledgements
The work was accomplished with the funding by the National Science Council, Republic of China, through research grant (NSC93-2313-B-002-020). The authors would also like to acknowledge the International Veterinary Acupuncture Society (IVAS) for allowing us to republish part of the manuscript that was presented at the 30th annual IVAS Congress, Oostende, Belgium, 2004. We also thank Professor Ming-lai Shen for the assiatance in statistics analysis.
References
- 1.Ernst E. Prevalence of use of complementary/alternative medicine: a systemic review. Bull World Health Org. 2000;78:252–57. [Google Scholar]
- 2.Lin JH, Kaphle K, Wu LS, Yang NYJ, Lu G, Yu C, et al. Sustainable veterinary medicine for new era. Rev Sci Tech Off Int Epiz. 2003;22:949–64. doi: 10.20506/rst.22.3.1451. [DOI] [PubMed] [Google Scholar]
- 3.Looney AL. Using acupuncture in veterinary practice. Vet Med. 2000;95:615–29. [Google Scholar]
- 4.Chan WW, Chen KY, Liu H, Wu LS, Lin JH. Acupuncture for general veterinary practice. J Vet Med Sci. 2001;63:1057–62. doi: 10.1292/jvms.63.1057. [DOI] [PubMed] [Google Scholar]
- 5.Schoen AM. Veterinary Acupuncture: Ancient Art to Modern Medicine. St. Louis, Missouri, U.S.A: Mosby, Inc.; 2001. pp. 19–23. 127–48. [Google Scholar]
- 6.Tang ZL. Assessment of acupuncture in the prevention of sudden death from coronary heart disease. J Trad Chin Med. 1987;7:143–46. [PubMed] [Google Scholar]
- 7.Tam KC, Yiu HH. The effect of acupuncture on essential hypertension. Am J Chin Med. 1975;3:369–75. doi: 10.1142/s0192415x7500044x. [DOI] [PubMed] [Google Scholar]
- 8.Richter A, Herlitx J, Hjalmarson A. Effect of acupuncture in patients with angina pectoris. Eur Heart J. 1991;12:175–78. doi: 10.1093/oxfordjournals.eurheartj.a059865. [DOI] [PubMed] [Google Scholar]
- 9.Liu RT, Lang M. Effect of electrical needling “Neiguan” point on the promotion of the recovery of acute myocardial ischemia in cats: analysis of afferent pathways. Acupunct Res. 1986;11:229–33. [PubMed] [Google Scholar]
- 10.Middlekauff HR. Acupuncture in the treatment of heart failure. Cardiol Rev. 2004;12:171–73. doi: 10.1097/01.crd.0000103650.71735.f0. [DOI] [PubMed] [Google Scholar]
- 11.Wu HC, Lin JG, Chu CH, Chang YH, Chang CG, Hsieh CL, et al. The effects of acupuncture on cardiac muscle cells and blood pressure in spontaneous hypertensive rats. Acupunct Electrother Res. 2004;29:83–95. doi: 10.3727/036012904815901515. [DOI] [PubMed] [Google Scholar]
- 12.Zhou W, Fu LW, Loi SCT, Li P, Longhurst C. Afferent mechanism underlying stimulation-modality related modulation of acupuncture-related cardiovascular response. J Appl Physiol. 2005;98:872–80. doi: 10.1152/japplphysiol.01079.2004. [DOI] [PubMed] [Google Scholar]
- 13.Kong SM. Heart rate power spectral analysis during homeostatic action of Neiguan acupoint-role played by cardial vagus nerve. J Trad Chin Med. 1988;8:271–76. [PubMed] [Google Scholar]
- 14.Jin Y, Cao Q, Zhuang D. Function of nucleus of solitary tract in the correlation between heart and acupoint Neiguan. J Trad Chin Med. 1988;8:61–68. [PubMed] [Google Scholar]
- 15.Syuu Y, Matsubara H, Kiyooka T, Hosogi S, Mohri S, Araki J, et al. Cardiovascular beneficial effects of electroacupuncture at Neiguan (PC-6) acupoint in anesthetized open-chest dog. Jpn J Physiol. 2001;51:231–38. doi: 10.2170/jjphysiol.51.231. [DOI] [PubMed] [Google Scholar]
- 16.Tsou MT, Huang CH, Chiu JH. Electrocupuncture on PC-6 (Neiguan) attenuates ischemia/reperfusion injury in rat hearts. Am J Chin Med. 2004;32:951–65. doi: 10.1142/S0192415X04002557. [DOI] [PubMed] [Google Scholar]
- 17.Mongelvang J, Stubgaard M, Thomsen C, Henriksen O. Evaluation of right ventricle volume measured by magnetic resonance imaging. Eur Heart J. 1988;9:529–33. doi: 10.1093/oxfordjournals.eurheartj.a062539. [DOI] [PubMed] [Google Scholar]
- 18.Constantine G, Shan K, Flamm SC, Siva Nathan MU. Role of MRI in clinical cardiology. Lancet. 2004;363:2162–71. doi: 10.1016/S0140-6736(04)16509-4. [DOI] [PubMed] [Google Scholar]
- 19.Lorenz CH. The range of normal values of cardiovascular structures in infants, Children, and adolescents measured by magnetic resonance imaging. Pediatr Cardiol. 2000;21:37–46. doi: 10.1007/s002469910006. [DOI] [PubMed] [Google Scholar]
- 20.Lima JAC, Desai MY. Cardiovascular magnetic resonance imaging: current and emerging application. J Am Coll Cardiol. 2004;44:1164–71. doi: 10.1016/j.jacc.2004.06.033. [DOI] [PubMed] [Google Scholar]
- 21.Belew AM, Barlett T, Brown SA. Evaluation of the white-coat effect in cats. J Vet Int Med. 1999;13:134–42. doi: 10.1892/0891-6640(1999)013<0134:eotwce>2.3.co;2. [DOI] [PubMed] [Google Scholar]
- 22.Massimini M, Porta A, Mariotti M, Malliani A, Montano N. Hear rate variability is encoded in the spontaneous discharge of thalamic somatosensory neurons in cat. J Physiol (London) 2000;526:387–96. doi: 10.1111/j.1469-7793.2000.t01-1-00387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ware WA. Twenty-four-hour ambulatory electrocardiography in normal cats. J Vet Int Med. 1999;13:175–80. doi: 10.1892/0891-6640(1999)013<0175:tfhaei>2.3.co;2. [DOI] [PubMed] [Google Scholar]
- 24.Robinson EP. Anesthesia for geriatric dogs and cats. Vet Technician. 1995;16:156–99. [Google Scholar]
- 25.Dobromylskyj P. Cardiovascular changes associated with anesthesia induced by medetomidine combined with ketamine in cats. J Small Anim Prac. 1996;37:169–72. doi: 10.1111/j.1748-5827.1996.tb01953.x. [DOI] [PubMed] [Google Scholar]
- 26.Janssens L, Altman S, Rogers PAM. Respiratory and cardiac arrest under general anesthesia; treatment by acupuncture of the nasal philtrum. Vet Rec. 1979;105:273–76. doi: 10.1136/vr.105.12.273. [DOI] [PubMed] [Google Scholar]
- 27.Mok YP. Medical acupuncture applications in surgical anesthesia. AAMA Review. 1993;1:20–24. [Google Scholar]
- 28.Li P, Tjen-A-Looi SC, Longhurst JC. Excitatory projections from arcuate nucleus to ventrolateral periaqueductal gray in electroacupuncture inhibition of cardiovascular reflexes. Am J Physiol Heart Circ Physiol. 2006;290:H2535–42. doi: 10.1152/ajpheart.00972.2005. [DOI] [PubMed] [Google Scholar]
- 29.Tsou MT, Ho JY, Lin CH, Chiu JH. Proteomic analysis finds different myocardial protective mechanisms for median nerve stimulation by electroacupuncture and by local somatothermal stimulation. Int J Mol Med. 2004;14:553–63. [PubMed] [Google Scholar]
- 30.Yun-Kyoung Yim, Hyun Lee, Kwon-Eui Hong, Young-Il Kim, Byung-Ryul Lee, Chang-Gue Son, et al. Electro-acupuncture at acupoint ST36 reduces inflammation and regulates immune activity in Collagen-Induced arthritic mice. eCAM. 2007;4:51–57. doi: 10.1093/ecam/nel054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fan Qu, Jue Zhou. Electro-Acupuncture in Relieving Labor Pain. eCAM. 2007;4:125–30. doi: 10.1093/ecam/nel053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lewith GT, White PJ, Pariente J. Investigating acupuncture using brain imaging techniques: the current state of play. eCAM. 2005;2:315–19. doi: 10.1093/ecam/neh110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hamlin RL, Buffington CA. Nutrition and the heart. Vet Clin North Am Small Anim Pract. 1989;19:527–38. doi: 10.1016/s0195-5616(89)50059-7. [DOI] [PubMed] [Google Scholar]
- 34.Abbott JA. Heart rate and heart rate variability of healthy cats in home and hospital Environments. J Feline Med Surg. 2005;7:195–202. doi: 10.1016/j.jfms.2004.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li P. Neural mechanism of the effect of acupuncture on cardiovascular diseases. In: Sato A, editor. Acupuncture-is there a Physiological Basis? Amsterdam: Elsevier Science, B.V.; 2002. pp. 71–77. [Google Scholar]
- 36.Li P, Pitsillides KF, Rendig SV, Pan HL, Longhurst JC. Reversal of reflex-induced myocardial ischemia by median nerve stimulation: a feline model of electropuncture. Circulation. 1998;97:1186–94. doi: 10.1161/01.cir.97.12.1186. [DOI] [PubMed] [Google Scholar]
- 37.Holaday JW. Cardiovascular effects of endogenous opiate systems. Am J Physiol. 1983;276:2127–34. doi: 10.1146/annurev.pa.23.040183.002545. [DOI] [PubMed] [Google Scholar]