Abstract
This study examined predictors of psychiatric hospitalization among children with autism spectrum disorders (ASD). Data were collected from 760 caregivers of children with ASD. Cox regression was used to determine factors associated with hospitalization. Almost 11% were hospitalized. Youth in single parent homes were more likely to be hospitalized (OR = 2.54), as were youth diagnosed at a later age (OR = 1.10). Engaging in self-injurious behavior (OR = 2.14), aggressive behavior (OR = 4.83), and being diagnosed with depression (OR = 2.48) or obsessive compulsive disorder (OR = 2.35) increased the odds of hospitalization. Risk for hospitalization increased with age and over time. The results suggest early diagnosis and community-based interventions for aggressive and self-injurious behaviors may reduce hospitalizations.
Keywords: Autistic disorder, Hospitalization, Health services
Introduction
The goal of this study was to examine the frequency of psychiatric hospitalization among children with autism spectrum disorders (ASD) and the risk of hospitalization associated with their clinical and demographic characteristics. Children with ASD or other developmental disabilities may be at greater risk for psychiatric hospitalization than children with other disorders (Gallaher et al. 2002; Romansky et al. 2003; Saeed et al. 2003; Walsh et al. 1997). Studies have found that a quarter of children with ASD served in community mental health settings have been psychiatrically hospitalized (Mandell et al. 2005) and that children with ASD have five times the Medicaid-reimbursed expenditures for inpatient psychiatric care of children with mental retardation and 20 times that of children with other psychiatric diagnoses (Croen et al. 2006; Mandell et al. 2006).
Aggressive and self-injurious behaviors, often present in children with ASD (Holden and Gitlesen 2006; McCracken et al. 2004; Volkmar et al. 2004), may increase the risk of hospitalization, as may a lack of appropriate community services. Clinicians often are unfamiliar with relevant interventions (Heidgerken et al. 2005), there often are long waiting lists for treatment programs (Levy et al. 2003), and education services, which comprise the bulk of interventions delivered to children with ASD, vary in quality and intensity (Lord et al. 2005; Stahmer 2006). In addition, private insurance companies often exclude autism as a covered diagnosis or limit coverage of related services (Birenbaum et al. 1990; Krauss et al. 2003), which may ultimately lead to the need for more intensive and restrictive care. Given this latter set of factors and the fact that few localities have decision rules governing care for children with ASD (Stahmer and Mandell 2006), risk for hospitalization may vary depending on the resources families bring to bear on the process of negotiating for services (Mandell et al. 2005).
While hospitalization may be warranted in some cases (Green et al. 2001; Leichtman et al. 2001), its use may represent a failure to provide appropriate community-based care. Examining factors associated with hospitalization may identify potential points of intervention that could decrease the need for children with ASD to be hospitalized. As a first step in investigating this issue, we examined characteristics associated with the risk for psychiatric hospitalization among a large sample of children diagnosed with ASD.
Methods
Data Collection
The University of Pennsylvania Institutional Review Board approved this study. Survey data were collected from June 21 through September 30, 2004 as part of a state-sponsored effort to improve the quality of care for individuals with ASD in Pennsylvania. Participants were recruited through mailings to 273 caregivers of individuals with autism who had indicated their willingness to participate in this research; those receiving direct mailings were asked to share information about how to obtain a copy of the survey with other caregivers. Autism provider organizations (n = 137) were identified through state directories and were requested to distribute a letter asking families to participate by contacting the research team for a copy of the survey. The invitation letter described the project and provided a web address for completing the survey over the Internet and a toll-free number to call to receive a paper copy, which was mailed out accompanied by a postage-paid return envelope. Both the Internet and paper versions of the survey again described the project and explained that all responses would be confidential. Participants were asked to complete the survey for their oldest child with ASD. Participants were given the opportunity to enter a drawing in which 40 people won cash prizes of $50 each.
Survey Description
The survey included 92 questions designed to measure the quality and quantity of services from the time concerns about development were first noted up to the present. It took an average of 45 min to complete, depending on the age of the child. Questions about clinical and socio-demographic characteristics also were included. The survey was developed through seven focus groups with parents of children with ASD; it was pilot tested with 10 parents of children with ASD ages 9–38 years, and subsequently altered for comprehensibility and content.
Sample
For this study the sample was limited to all 760 children between the ages of 5 and 21 years with a diagnosis of autistic disorder, Asperger’s disorder or pervasive developmental delay-not otherwise specified (PDD-NOS) for whom a survey was completed by parents. There were 1,027 returned surveys, 713 of which were obtained through the Internet; nine Internet surveys contained little data and were deleted from the sample. Twenty percent of the survey subjects were below 5 years and 4% were above 21 years of age. Children under 5 years were excluded because of their low risk of hospitalization. Another 3% were diagnosed with Rett’s disorder or childhood disintegrative disorder and were not included. Of the remaining sample, mothers of children with ASD comprised 86%, fathers 7% and legal guardians 7% of survey respondents. To determine the sample representativeness, their race and ethnicity was compared with those of the 5,200 children ages 5–21 in Pennsylvania who received autism-related special education services in 2003. The two groups deviated by no more than 1% in any ethnic category. Because children with ASD in Pennsylvania are eligible for Medicaid-reimbursed services regardless of family income, the service use of the sample was compared to Medicaid-reimbursed claims for ASD in Pennsylvania (data not shown). Eleven percent of the sample experienced a psychiatric inpatient episode compared with 10% of Medicaid-eligible youth of comparable ages; 46% had used a psychotropic medication compared with 44% in the claims.
Analyses
Frequencies and means with standard deviations as appropriate were calculated for all variables, stratified on the presence of a psychiatric hospitalization. Because of the large number of possible covariates, only those whose bivariate association with hospitalization was significant at <0.25 were included in the adjusted model (Hosmer and Lemeshow 2001). Cox proportional hazards models were used to determine the effect of covariates on hospitalization. This method compared the risk of first hospitalization among subjects of the same age, using time until first hospitalization as the outcome variable (Cox and Oakes 1984). This method treats the study as a cohort study, with subjects contributing as much “time” to the analysis as they are old. If they did not experience a hospitalization but were younger than 21 years when the survey was completed, then they were “censored,” since it is only known that they did not experience a hospitalization up to that point.
Adding age as a separate covariate, similar to adding year of birth, allowed for the determination of birth cohort effects. Kaplan-Meier curves were used to determine unadjusted differences in hospitalization risk among birth cohorts stratified based whether they were above or below the sample’s sample age (10.2 years).
Results
Of the sample, 10.8% were hospitalized (8.7% if children less than 5 years of age are included in the denominator). Table 1 displays the sample characteristics. Hospitalized youth were, on average, older, more likely to be African American, and more likely to be adopted than non-hospitalized youth. Caregivers of hospitalized youth were less likely to be living with a partner, more likely to make less than $40,000 a year, and less likely to have graduated college. Hospitalized youth were more likely than their peers to be diagnosed with autistic or Asperger’s disorders and less likely to be diagnosed with PDD-NOS. They were more likely to display self-injurious or aggressive behaviors, and less likely to display stereotypies. Hospitalized youth were also more likely than non-hospitalized youth to have been diagnosed with a number of other disorders, including ADHD (despite the fact that ASD precludes a diagnosis of ADHD), depression, mental retardation and obsessive-compulsive disorder.
Table 1.
Characteristics of children ages 2–21 years diagnosed with autism spectrum disorders (n = 939)
| Had hospitalization (n = 82) | No hospitalization (n = 678) | Sig. | ||
|---|---|---|---|---|
| Demographics | ||||
| Age [years (SD)] | 13.6 (3.7) | 8.8 (4.1) | <0.001 | |
| Male | 85% | 84% | 0.875 | |
| African American | 17% | 8% | 0.003 | |
| White | 74% | 84% | ||
| Other | 9% | 7% | ||
| Adopted | 15% | 4% | <0.001 | |
| Live in a rural area | 23% | 21% | 0.759 | |
| Live in a suburban area | 55% | 59% | ||
| Live in an urban area | 22% | 20% | ||
| Respondent not married/cohabitating | 44% | 17% | <0.001 | |
| Household income | < $40,000/year | 45% | 26% | <0.001 |
| $40,000–$79,000/year | 27% | 40% | ||
| > $80,000/year | 28% | 34% | ||
| Respondent education | No high school diploma | 6% | 2% | 0.028 |
| High school graduate | 45% | 38% | ||
| College graduate | 49% | 60% | ||
| Clinical characteristics | ||||
| Diagnosis | Autistic disorder | 43% | 40% | 0.017 |
| Asperger’s disorder | 35% | 21% | ||
| PDD-NOS | 22% | 39% | ||
| Symptoms | Self-injurious behavior | 68% | 38% | <0.001 |
| Aggressive to others | 79% | 46% | <0.001 | |
| Severe language deficits | 55% | 69% | 0.008 | |
| Sleep problems | 57% | 54% | 0.315 | |
| Stereotypies | 52% | 64% | 0.029 | |
| Other diagnoses received | Attention deficit | 56% | 33% | <0.001 |
| Depression | 27% | 5% | <0.001 | |
| Mental retardation | 42% | 19% | <0.001 | |
| Obsessive compulsive | 40% | 12% | <0.001 | |
| Seizures | 11% | 8% | 0.411 | |
| Service experiences | ||||
| Age of first expressed concern [years (SD)] | 2.0 (1.9) | 2.0 (1.6) | 0.918 | |
| Age of diagnosis [years, (SD)] | 6.2 (3.7) | 4.2 (2.8) | <0.001 | |
| Diagnosing clinician provided service information | 43% | 55% | 0.031 | |
| Ever used psychotropic medications | 73% | 36% | <0.001 | |
| Ever used applied behavior analysis | 46% | 52% | 0.355 | |
| Ever used early intervention services | 67% | 87% | <0.001 | |
There was no difference between the groups regarding the age at which caregivers first expressed concerns to a clinician; however, hospitalized youth received an ASD diagnosis an average of 1.6 years later than non-hospitalized youth. Hospitalized youth were more likely to use psychotropic medications and less likely to have used early intervention services.
Table 2 provides the result of the Cox regression predicting first hospitalization. Each year of age was associated with a decrease in hospitalization risk (odds ratio [OR] = 0.81), which should be interpreted as a decrease in the risk for hospitalization over time, rather than a decrease in risk associated with older age. Youth living in single parent homes were more likely to be hospitalized (OR = 2.54), as were youth who were diagnosed at a later age (OR = 1.10). Youths diagnosed with PDD-NOS had less than half the odds (OR = 0.46) of being hospitalized relative to youth with autistic disorder. Engaging in self-injurious behavior (OR = 2.14), aggressive behavior (OR = 4.83), being diagnosed with depression (OR = 2.48) or obsessive compulsive disorder (OR = 2.35), or taking psychotropic medications (OR = 2.08) all increased the odds of hospitalization.
Table 2.
Cox regression predicting psychiatric hospitalization among children with autism spectrum disorders ages 5–21 years (n = 760)
| Odds ratio | 95% Confidence interval | |
|---|---|---|
| Age (years) | 0.81 | 0.73–0.90 |
| Nonwhite | 1.41 | 0.74–2.70 |
| Adopted | 1.85 | 0.85–4.02 |
| Not married or cohabitating | 2.54 | 1.32–4.88 |
| Income $40,000–$79,000 | 0.93 | 0.46–1.87 |
| Income ≥ $80,000 | 1.29 | 0.60–2.76 |
| Asperger’s disorder | 1.08 | 0.46–2.53 |
| PDD-NOS | 0.46 | 0.23–0.93 |
| Age of diagnosis (years) | 1.10 | 1.00–1.21 |
| Self-injurious behavior | 2.14 | 1.18–3.88 |
| Aggressive towards others | 4.83 | 2.24–10.42 |
| Severe language deficits | 0.92 | 0.45–1.90 |
| Stereotypies | 0.68 | 0.39–1.18 |
| ADHD | 1.03 | 0.59–1.80 |
| Depression | 2.48 | 1.33–4.63 |
| Mental retardation | 1.93 | 0.95–3.93 |
| Obsessive compulsive disorder | 2.35 | 1.39–3.96 |
| Diagnosing clinician provided information | 1.24 | 0.72–2.12 |
| Ever used psychotropic medications | 2.08 | 1.11–3.90 |
| Ever used early intervention services | 1.08 | 0.51–2.27 |
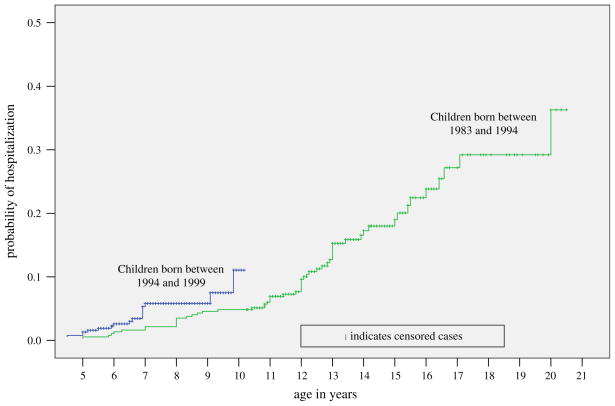
Figure 1 displays the Kaplan-Meier plot of risk of hospitalization, stratified by the median split in age. Children in the younger birth cohort (born between 1994 and 1999) had a greater risk of hospitalization than children in the older cohort (1983–1994) at the same age. For example, 10-year olds in the younger birth cohort had an 11% probability of first hospitalization, compared with 5% among 10-year olds in the older birth cohort. Unadjusted risk of first hospitalization reached 37% among 21-year olds.
Fig. 1.
Kaplan-Meier curve showing the cumulative risk of hospitalization among children with autism spectrum disorders (n = 939)
Discussion
In this community sample of children with ASD, 10.8% had at least one lifetime psychiatric hospitalization. Self-injurious and aggressive behaviors independently predicted hospitalization, as did having a diagnosis of depression or obsessive-compulsive disorder, or using a psychotropic medication. These characteristics suggest a high level of clinical complexity that may be difficult to address in the community, or conversely that the level of care in the community is not able to address a disorder that is complex in its own right and often is associated with co-morbidity. The fact that the later children were diagnosed, the more likely they were to be hospitalized, could reflect the negative impact of lack of intervention on child behavior and on parent skills for addressing behavior problems, since most early intervention programs include both a child component and a parent training program to promote generalization of the program to the home (Stahmer 2006; Stahmer and Ingersoll 2004). It could also indicate that families with fewer resources to obtain appropriate care have fewer resources to cope with the burden of care (Mandell et al. 2005).
Children of single parents were at increased risk for hospitalization, perhaps because these families have fewer resources to obtain appropriate services for their children. For these families, attending appointments or implementing home-based activities may come at the sacrifice of a day’s pay. Alternatively, hospitalization may act as respite for highly distressed families (Dossetor et al. 1993). In general, the demographic characteristics of the hospitalized children and the fact that they were less likely to receive early intervention paint a picture of the traditionally underserved families with fewer resources. The fact that being a single parent remained significant in the adjusted model, while other socio-demographic characteristics did not suggests the particular burden associated with this family arrangement and provides evidence for the idea of hospitalization as respite for families when other supports are not available.
An alarming finding is that the risk of hospitalization increased over time. Despite considerable efforts over the past 20 years to reduce the use of psychiatric hospitalization because of the associated costs and the value of keeping children in their communities (Center for Mental Health Services 1999; Knitzer and Olson 1982), some groups of children may be increasingly hospitalized. For example, while Harpaz-Rotem et al. found that while the percentage of privately insured children who were psychiatrically hospitalized dropped from 0.36% in 1995 to 0.23% in 2000, the percentage of children with some diagnoses who were hospitalized went up (Harpaz-Rotem et al. 2005). Changing diagnostic practices could account for these differences. It also could be that as an increasing number of children are diagnosed with ASD, the communities in which they are served are unprepared to meet their needs (Mandell and Palmer 2005). A backlog in the availability of community-based services may result in more children being hospitalized.
A number of study limitations should be considered. Perhaps primary among them is the validity of ASD diagnoses and reporting of related symptoms. All respondents indicated that the diagnosis was made by a physician or psychologist. Studies have found good to excellent reliability associated with the diagnosis of ASD by healthcare professionals (Fombonne et al. 2004; Hill et al. 2001; Mahoney et al. 1998). A related limitation is that data were collected only on some symptoms associated with ASD. Our goal was to focus on those symptoms that might differentiate subtypes of children with ASD. In the process, we may have missed symptoms that are associated with hospitalization such as specific stereotypies, socialization or communication deficits. A third limitation is the potential bias in survey respondents, especially given the sampling method. Despite the similarities between the experiences and ethnicity of survey respondents and children with ASD in Pennsylvania described in the methods section, families motivated to complete this survey may have characteristics and experiences different from those of non-responders. A fourth limitation is that caregivers were asked to recall events that may have happened much earlier. Differential recall about, for example, age of diagnosis or age of hospitalization may have biased the results. Finally, we did not collect information on repeat hospitalizations, duration of hospital stays, placement in residential facilities, which means that our outcome of interest can only be treated as dichotomous. In addition, we collected no information on insurance, which may greatly affect the risk of hospitalization.
Despite these limitations, there are important implications related to these findings. The results suggest some potential points for intervention to reduce psychiatric hospitalization among children with ASD. For example, especially for younger children, behavioral interventions may reduce the aggressive and self-injurious behaviors that lead to hospitalization (Bodfish, 2004; Volkmar et al. 1999). Pharmacological treatments also have been developed to address these behaviors (Hollander et al. 2003), but there are many concerns about long-term consequences, especially in young children (Volkmar 2001).
There is a particular need for crisis intervention strategies that divert children with ASD from hospitalization, similar to those that have been developed for children with other psychiatric disorders (Henggeler et al. 2003). These regular (Jacobson and Mulick 2000) and crisis (Sheidow et al. 2004) interventions are expensive and many communities have little infrastructure to deliver them at the required intensity (Heidgerken et al. 2005; Stahmer 2006; Stahmer and Mandell 2006). Increased investment in these services, however, has the potential to significantly reduce the need for more costly inpatient services.
The profile of hospitalized children and their families suggests the need for careful discharge planning that includes a thorough family—as well as child—assessment to determine the root causes. Interventions limited to addressing children’s clinical needs may not be as effective as those that address family needs as well. Families with fewer resources, especially single-parent families, require respite care, which reduces caregiver stress and improve family functioning (Botuck and Winsberg 1991; Cowen and Reed 2002). Respite care often is in short supply (McConkey and Adams 2000), however, and ironically, aggressive and self-injurious behaviors often disqualify children from its use (McGill et al. 2006).
The finding that earlier diagnosis was associated with decreased hospitalization risk, combined with the bivariate finding that hospitalized children were less likely to use early intervention services, raises the possibility that early treatment may decrease the need for later, more costly services. The association of hospitalization and age of diagnosis bordered on marginal significance, and therefore bears replication before deriving too many implications from it; however; an increasing number of studies suggest that earlier intervention results in better outcomes (Lord and McGee 2001) and that gains in functioning associated with early treatment will result in cost savings to the family and the systems in which children with ASD are served (Jacobson and Mulick 2000; Jacobson et al. 1998; Jarbrink and Knapp 2001).
Addressing issues related to hospitalization takes on particular urgency in light of the finding that the risk of hospitalization is increasing over time. Future research should examine the role of supportive healthcare services and supports, as well as insurance coverage for these services, in reducing the risk of hospitalization among children with ASD.
Acknowledgments
Support for this study was provided by a grant from the Pennsylvania Department of Health (ME02271) and a mentored scientist career development award from the National Institute of Mental Health (MH067628).
References
- Birenbaum A, Guyot D, Cohen H. Health care financing for severe developmental disabilities. Monographs of the American Association on Mental Retardation. 1990;14:1–150. [PubMed] [Google Scholar]
- Bodfish J. Treating the core features of autism: Are we there yet? Mental Retardation and Developmental Disabilities Research Reviews. 2004;10(4):318–324. doi: 10.1002/mrdd.20045. [DOI] [PubMed] [Google Scholar]
- Botuck S, Winsberg B. Effects of respite on mothers of school-age and adult children with severe disabilities. Mental Retardation. 1991;29(1):43–47. [PubMed] [Google Scholar]
- CMHS. Annual report to congress on the evaluation of the comprehensive community mental health services for children and their families program. Atlanta: ORC Macro; 1999. [Google Scholar]
- Cowen P, Reed D. Effects of respite care for children with developmental disabilities: Evaluation of an intervention for at risk families. Public Health Nursing. 2002;19(4):272–283. doi: 10.1046/j.1525-1446.2002.19407.x. [DOI] [PubMed] [Google Scholar]
- Cox D, Oakes D. Analysis of survival data. London: Chapman & Hall; 1984. [Google Scholar]
- Croen L, Najjar D, Ray T, Lotspeich L, Bernal P. A comparison of health care utilization and costs of children with and without autism spectrum disorders in a large group-model health plan. Pediatrics. 2006;118(4):e1203–e1211. doi: 10.1542/peds.2006-0127. [DOI] [PubMed] [Google Scholar]
- Dossetor D, Nicol A, Stretch D. Hostel-based respite care for adolescents with developmental retardation: The need for “normalized” respite resources. Journal of Child Psychology & Psychiatry & Allied Disciplines. 1993;34(3):391–412. doi: 10.1111/j.1469-7610.1993.tb01000.x. [DOI] [PubMed] [Google Scholar]
- Fombonne E, Heavey L, Smeeth L, Rodrigues L, Cook C, Smith P, et al. Validation of the diagnosis of autism in general practitioner records. BMC Public Health. 2004;4 doi: 10.1186/1471-2458-4-5. (Article 5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallaher M, Christakis D, Connell F. Health care use by children diagnosed as having developmental delay. Archives of Pediatrics & Adolescent Medicine. 2002;156(3):246–251. doi: 10.1001/archpedi.156.3.246. [DOI] [PubMed] [Google Scholar]
- Green J, Kroll L, Imrie D, Frances F, Begum K, Harrison L, et al. Health gain and outcome predictors during inpatient and related day treatment in child and adolescent psychiatry. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(3):325–332. doi: 10.1097/00004583-200103000-00012. [DOI] [PubMed] [Google Scholar]
- Harpaz-Rotem I, Leslie D, Martin A, Rosenheck R. Changes in child and adolescent inpatient psychiatric admission diagnoses between 1995 and 2000. Social Psychiatry & Psychiatric Epidemiology. 2005;40(8):642–647. doi: 10.1007/s00127-005-0923-0. [DOI] [PubMed] [Google Scholar]
- Heidgerken A, Geffken G, Modi A, Frakey L. A survey of autism knowledge in a health care setting. Journal of Autism & Developmental Disorders. 2005;3:323–330. doi: 10.1007/s10803-005-3298-x. [DOI] [PubMed] [Google Scholar]
- Henggeler S, Rowland M, Halliday-Boykins C, Sheidow A, Ward D, Randall J, et al. One-year follow-up of multisystemic therapy as an alternative to the hospitalization of youths in psychiatric crisis. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42(5):543–551. doi: 10.1097/01.CHI.0000046834.09750.5F. [DOI] [PubMed] [Google Scholar]
- Hill A, Bolte S, Petrova G, Beltcheva D, Tacheva S, Poustka F. Stability and interpersonal agreement of the interview-based diagnosis of autism. Psychopathology. 2001;34(4):187–191. doi: 10.1159/000049305. [DOI] [PubMed] [Google Scholar]
- Holden B, Gitlesen J. A total population study of challenging behaviour in the county of Hedmark, Norway: Prevalence, and risk markers. Research in Developmental Disabilities. 2006;27(4):456–465. doi: 10.1016/j.ridd.2005.06.001. [DOI] [PubMed] [Google Scholar]
- Hollander E, Phillips A, Yeh C. Targeted treatments for symptom domains in child and adolescent autism. Lancet. 2003;362(9385):732–734. doi: 10.1016/S0140-6736(03)14236-5. [DOI] [PubMed] [Google Scholar]
- Hosmer D, Lemeshow S. Applied logistic regression, textbook and solutions manual. 2. Hoboken: Wiley-Interscience; 2001. [Google Scholar]
- Jacobson J, Mulick J. System and cost research issues in treatments for people with autistic disorders. Journal of Autism & Developmental Disorders. 2000;30(6):585–593. doi: 10.1023/a:1005691411255. [DOI] [PubMed] [Google Scholar]
- Jacobson J, Mulick J, Green G. Cost-benefit estimates for early intensive behavioral intervention for young children with autism-general model and single state case. Behavioral Interventions. 1998;13:201–226. [Google Scholar]
- Jarbrink K, Knapp M. The economic impact of autism in Britain. Autism. 2001;5(1):7–22. doi: 10.1177/1362361301005001002. [DOI] [PubMed] [Google Scholar]
- Knitzer J, Olson L. Unclaimed children: The failure of public responsibility to children and adolescents in need of mental health services. Washington: Children’s Defense Fund; 1982. [Google Scholar]
- Krauss M, Gulley S, Sciegaj M, Wells N. Access to specialty medical care for children with mental retardation, autism and other special health care needs. Mental Retardation. 2003;41(5):329–339. doi: 10.1352/0047-6765(2003)41<329:ATSMCF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Leichtman M, Leichtman M, Barber C, Neese D. Effectiveness of intensive short-term residential treatment with severely disturbed adolescents. American Journal of Orthopsychiatry. 2001;71(2):227–235. doi: 10.1037/0002-9432.71.2.227. [DOI] [PubMed] [Google Scholar]
- Levy SE, Mandell DS, Merhar S, Ittenbach RF, Pinto-Martin JA. Use of complementary and alternative medicine among children recently diagnosed with autistic spectrum disorder. Journal of Developmental and Behavioral Pediatrics. 2003;24(6):418–423. doi: 10.1097/00004703-200312000-00003. [DOI] [PubMed] [Google Scholar]
- Lord C, McGee J, editors. Educating children with autism. Washington: National Academy Press; 2001. [Google Scholar]
- Lord C, Wagner A, Rogers S, Szatmari P, Aman M, Charman T, et al. Challenges in evaluating psychosocial interventions for Autistic Spectrum Disorders. Journal of Autism & Developmental Disorders. 2005;35(6):695–708. doi: 10.1007/s10803-005-0017-6. [DOI] [PubMed] [Google Scholar]
- Mahoney W, Szatmari P, MacLean J, Bryson S, Bartolucci G, Walter S, et al. Reliability and accuracy of differentiating pervasive developmental disorder subtypes. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37(3):278–285. doi: 10.1097/00004583-199803000-00012. [DOI] [PubMed] [Google Scholar]
- Mandell D, Novak M, Zubritsky C. Factors associated with the age of diagnosis among children with autism spectrum disorders. Pediatrics. 2005;116(6):1480–1486. doi: 10.1542/peds.2005-0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandell D, Palmer R. Differences among states in the identification of autistic spectrum disorders. Archives of Pediatrics & Adolescent Medicine. 2005;159(3):266–269. doi: 10.1001/archpedi.159.3.266. [DOI] [PubMed] [Google Scholar]
- Mandell D, Walrath C, Manteuffel B, Sgro G, Pinto-Martin J. Characteristics of children with autistic spectrum disorders served in comprehensive community-based mental health settings. Journal of Autism and Developmental Disorders. 2005;35(3):113–121. doi: 10.1007/s10803-005-3296-z. [DOI] [PubMed] [Google Scholar]
- Mandell DS, Cao J, Ittenbach R, Pinto-Martin J. Medicaid expenditures for children with autistic spectrum disorders: 1994 to 1999. Journal Of Autism And Developmental Disorders. 2006;36(4):475–485. doi: 10.1007/s10803-006-0088-z. [DOI] [PubMed] [Google Scholar]
- McConkey R, Adams L. Matching short break services for children with learning disabilities to family needs and preferences. Child: Care, Health & Development. 2000;26(5):429–444. doi: 10.1046/j.1365-2214.2000.00163.x. [DOI] [PubMed] [Google Scholar]
- McCracken J, McGough J, Shah B, Cronin P, Hong D, Aman M, et al. Risperidone in children with autism and serious behavior problems. New England Journal of Medicine. 2004;347(5):314–321. doi: 10.1056/NEJMoa013171. [DOI] [PubMed] [Google Scholar]
- McGill P, Papachristoforou E, Cooper V. Support for family carers of children and young people with developmental disabilities and challenging behaviour. Child: Care, Health & Development. 2006;32(2):159–165. doi: 10.1111/j.1365-2214.2006.00600.x. [DOI] [PubMed] [Google Scholar]
- Romansky J, Lyons J, Lehner R, West C. Factors related to psychiatric hospital readmission among children and adolescents in state custody. Psychiatric Services. 2003;54(3):356–362. doi: 10.1176/appi.ps.54.3.356. [DOI] [PubMed] [Google Scholar]
- Saeed H, Ouellette-Kuntz H, Stuart H, Burge P. Length of stay for psychiatric inpatient services: A comparison of admissions of people with and without developmental disabilities. Journal of Behavioral Health Services & Research. 2003;30(4):406–417. doi: 10.1007/BF02287428. [DOI] [PubMed] [Google Scholar]
- Sheidow A, Bradford W, Henggeler S, Rowland M, Halliday-Boykins C, Schoenwald S, et al. Treatment costs for youths receiving multisystemic therapy or hospitalization after a psychiatric crisis. Psychiatric Services. 2004;55(5):548–554. doi: 10.1176/appi.ps.55.5.548. [DOI] [PubMed] [Google Scholar]
- Stahmer A. The Basic Structure of Community Early Intervention Programs for Children with Autism: Provider Descriptions. Journal of Autism & Developmental Disorders. 2006 doi: 10.1007/s10803-006-0284-x. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahmer A, Ingersoll B. Inclusive programming for toddlers autism spectrum disorders: Outcomes from the Children’s Toddler School. Journal of Positive Behavior Interventions. 2004;6(2):67–82. [Google Scholar]
- Stahmer A, Mandell D. State infant/toddler program policies for eligibility and services provision for young children with autism. Mental Health Services Research. 2006 doi: 10.1007/s10488-006-0060-4. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkmar F. Pharmacological interventions in autism: Theoretical and practical issues. Journal of Clinical Child Psychology. 2001;30(1):80–87. doi: 10.1207/S15374424JCCP3001_9. [DOI] [PubMed] [Google Scholar]
- Volkmar F, Cook E, Pomeroy J, Realmuto G, Tanguay P. Practice parameters for the assessment and treatment of children, adolescents and adults with autism and other pervasive developmental disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38(12 Suppl):32S–54S. doi: 10.1016/s0890-8567(99)80003-3. [DOI] [PubMed] [Google Scholar]
- Volkmar F, Lord C, Bailey A, Schultz R, Klin A. Autism and pervasive developmental disorders. Journal of Child Psychology & Psychiatry & Allied Disciplines. 2004;45(1):135–155. doi: 10.1046/j.0021-9630.2003.00317.x. [DOI] [PubMed] [Google Scholar]
- Walsh K, Kastner T, Criscione T. Characteristics of hospitalizations for people with developmental disabilities: utilization, costs, and impact of care coordination. American Journal of Mental Retardation. 1997;101(5):505–520. [PubMed] [Google Scholar]