Abstract
Anxiety is a common co-occurring problem among young people with autism spectrum disorders (ASD). Characterized by deficits in social interaction, communication problems, and stereotyped behavior and restricted interests, this group of disorders is more prevalent than previously realized. When present, anxiety may compound the social deficits of young people with ASD. Given the additional disability and common co-occurrence of anxiety in ASD, we developed a manual-based cognitive-behavioral treatment program to target anxiety symptoms as well as social skill deficits in adolescents with ASD [Multimodal Anxiety and Social Skills Intervention: MASSI]. In this paper, we describe the foundation, content, and development of MASSI. We also summarize data on treatment feasibility based on a pilot study that implemented the intervention.
Keywords: Autism, Anxiety, Social skills, Adolescence, Intervention, Therapy
Introduction
Autistic Disorder, Asperger’s Disorder, and Pervasive Developmental Disorder-Not Otherwise Specified (PDD-NOS) represent a heterogeneous group of neurodevelopmental conditions that share a common underlying deficit in social competence. In the last decade, scientific interest in treatment approaches for Autism Spectrum Disorders (ASD) has risen considerably, due largely to heightened public awareness and increased rates of identification (US CDC 2007). The need for advances in the development of effective psychosocial treatments for ASD has been identified (Smith et al. 2007). When present, problems with anxiety may intensify the social and functional impairment experienced by adolescents with ASD (see Myles et al. 2001). No available treatment programs, however, target both the core social deficits and associated problems with anxiety that frequently occur in adolescents with ASD.
Background
Anxiety and Social Deficits in ASD
Poor social interaction skills represent the primary source of impairment in ASD, regardless of the individual’s intelligence or language ability (Carter et al. 2005). The social disability that characterizes this group of disorders does not diminish during childhood and adolescence. For higher functioning individuals, in fact, the social disability may be felt more acutely in adolescence (Tse et al. 2007). In recent years, increasing attention has been given to concomitant psychiatric conditions in people with ASD. In clinic samples, anxiety-related concerns are among the most common presenting problems for school-age children and adolescents with ASD (Ghaziuddin 2002). Although large-scale epidemiological data on the prevalence of co-occurring anxiety disorders are not available, a recent comprehensive review found estimates of impairing anxiety in children with ASD ranging from 11 to 84% (White et al. 2009b). On closer examination, most of the reviewed studies reported comorbidity estimates between 40 and 45% (Bellini 2004; Bradley et al. 2004; Simonoff et al. 2008; Sukhodolsky et al. 2008). As such, we conceptualize clinical anxiety as a separate comorbid condition from the ASD itself.
Adolescence may represent a time of heightened risk for the development or exacerbation of problems with anxiety in people with ASD. From a developmental perspective, impairment and distress may increase during adolescence as the social milieu becomes more complex and the teen grows more aware of his social disability (Klin and Volkmar 2000; Tantam 2003 Sukhodolsky et al. 2008). Growing self-awareness, an increasingly complex social world, and a desire to form peer relationships without the necessary skills to successfully do so may contribute to the development of secondary mood and anxiety problems (Myles 2003; Myles et al. 2001; Tantam 2003), especially for higher functioning individuals with ASD who have the capacity for greater insight and awareness. Among neurotypical (non-ASD) people with diagnoses of Social Phobia, most report symptom onset before adolescence, at around 12.5 years (DeWit et al. 1999; Grant et al. 2005). For youngsters with ASD, problems with anxiety—particularly social anxiety, may emerge somewhat later in adolescence (Weisbrot et al. 2005; White et al. 2009b). Based on available phenomenological research, there is evidence that certain types of anxiety (e.g., social and evaluative anxiety, panic disorder) often emerge during adolescence in people with ASD (Bellini 2004; Kuusikko et al. 2008). However, this is based largely on cross-sectional and anecdotal evidence; longitudinal studies on the emergence of problems with anxiety in ASD are needed.
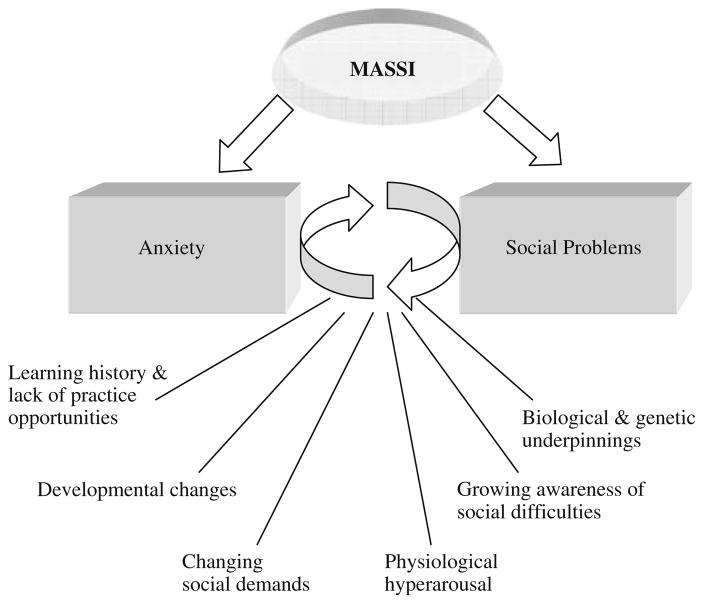
There is emerging evidence for an association between social impairment and anxiety in people with ASD, although the nature of this relationship is not entirely clear. Physiological hyperarousal and social deficits may interact to predict the development of social anxiety in children with ASD (Bellini 2006a), implicating possible biological as well as psychosocial underpinnings in the relationship between anxiety and ASD-related social deficits. Social anxiety can lead to a lack of opportunities in which to practice social skills, if the teen avoids peers because of past social difficulties, and also prevent the successful execution of well-learned skills (e.g., Myles et al. 2001).
Although there are many unanswered questions about the nature of anxiety in young people with ASD, it can be concluded that (1) anxiety is a frequently reported problem in children and adolescents with ASD; (2) anxiety, when present, augments social impairment and poor social functioning may contribute to anxiety; and (3) anxiety may become more prominent as children develop into adolescence, especially for higher functioning individuals. The bi-directional and possibly cyclic relationship between anxiety and social deficits in young people with ASD, in which the core social deficit contributes to the experience of anxiety, which then serves to intensify the teen’s social problems, calls for intervention that addresses both concerns simultaneously. Treatment that promotes anxiety reduction and social skill development could reduce the overall disability of adolescents with ASD. A model of the hypothesized bi-directional relationship between anxiety and social difficulties in adolescents with ASD as conceptualized in MASSI, with contributing influences and targets of treatment, is presented in Fig. 1.
Fig. 1.
MASSI Conceptual Model
Despite ongoing debate about the clinical utility of manual-based interventions (Ollendick et al. 2006), the importance of developing and testing psychosocial intervention manuals was noted by a recent National Institute of Mental Health working group for ASD (Smith et al. 2007). To date, few treatment manuals for people with ASD have been developed (e.g., Bellini 2006b; Johnson et al. 2007; McAfee 2001; RUPP 2007) and fewer still have been systematically evaluated. Treatment manuals are essential for empirical evaluation of an intervention (e.g., via randomized clinical trials) as well as later replication and dissemination of the intervention to practitioners. This paper describes the rationale and development of a novel treatment program to address both social skill deficits and anxiety in cognitively higher functioning (i.e., assessed full scale IQ above 70) adolescents with ASD.
Treatment of Anxiety and Social Deficits in ASD
The primary, non-pharmacological treatment of choice for mood and anxiety disorders in children and adolescents is cognitive-behavioral therapy (CBT; Ollendick et al. 2006; Walkup et al. 2008). To date, however, only a handful of clinical studies have examined the efficacy of non-medical, psychosocial treatments for anxiety in young people with ASD (Chalfant et al. 2007; Lehmkuhl et al. 2008; Reaven and Hepburn 2003; Reaven et al. 2009; Sofronoff et al. 2005; Sze and Wood 2007; Wood et al. 2009). One recent study by Beaumont and Sofrononoff (2008) examined potential indirect improvement in anxiety, via improved emotion regulation, following intensive social skills intervention. This study reported that children with Asperger’s Disorder, ages seven to 11, demonstrated improved knowledge of anxiety- and anger-management strategies following treatment, although anxiety symptoms were not explicitly assessed in the children or targeted in treatment.
In most of these studies, adaptations have been made to traditional CBT approaches for children with ASD, including increased structure and predictability in delivery of treatment components, incorporation of visual aids, increased parental involvement, and consideration of the child’s special needs and interests. Collectively, these studies indicate that modified CBT may be a promising treatment approach for anxiety in children with higher functioning forms of ASD (White et al. 2009b). Interventions in these studies have targeted a range of problems associated with anxiety, including co-occurring Obsessive–Compulsive Disorder (Reaven and Hepburn 2003; Lehmkuhl et al. 2008), symptoms of multiple anxiety disorders (Chalfant et al. 2007), and symptoms of anxiety without formal diagnoses (Sofronoff et al. 2005).
Reaven et al. (2009) evaluated an original, group-delivered CBT intervention program for high-functioning children with ASD, ages seven to 14 (n = 33). They found that parent-reported anxiety symptoms declined following the intervention, but not child-report symptoms. Independent (i.e., blinded) symptom reports were not collected, and participants were not randomly assigned to treatment or control condition. Only three randomized, controlled clinical trials (RCT) of psychosocial treatment for anxiety in children with ASD could be identified. Wood et al. (2009) conducted an RCT of a CBT program with children ages seven to 11 (n = 40). A family-based intervention program (Wood and McLeod 2008) was adapted for use with children with ASD. Of 14 children who completed the intervention, 13 were considered treatment responders and only two of 22 children assigned to the wait-list control group were considered responders (defined as a rating of 1, 2, or 3 by an independent evaluator on the Clinical Global Impression—Improvement Scale). Group differences were also found on independent evaluations of diagnostic status (of anxiety disorders) and parent-reported anxiety symptoms. No group differences were seen in child-reported anxiety (Wood et al. 2009). Chalfant et al. (2007) conducted an RCT with 47 children, ages eight to 13, with ASD. Participants were assigned to either CBT or wait-list. The intervention, adapted from the “Cool Kids” anxiety treatment program (Lyneham et al. 2003), was a 12-week, group-based program. Children in the CBT group showed a decrease in anxiety symptoms based on parent-, teacher-, and child self-reports, and many of the children in the treatment group (71.4%) no longer met criteria for an anxiety disorder, whereas none of the control group children showed change in diagnostic status. Finally, Sofronoff et al. (2005) randomly assigned children with Asperger’s Disorder (ages 10–12, n = 71) to one of three conditions—child-based intervention, combined child and parent intervention, or a wait-list group. Parents of children in the combined (parent and child) intervention reported the greatest decrease in children’s symptoms of anxiety, and children in both treatment groups identified more coping strategies than did the control children. No independent (blinded) ratings of anxiety were gathered.
Collectively, these studies indicate that cognitive-behavioral intervention is promising as a treatment for anxiety in children with ASD. Few studies, however, have implemented individual therapy with the youngster—an important consideration given the heterogeneity seen in ASD symptom expression or utilized independent outcome evaluation. To our knowledge, only two studies have targeted both social skill development and anxiety reduction (Sze and Wood 2007; Wood et al. 2009). Moreover, the above cited studies included children from 7 to 14 years of age, with the majority of participants falling in the younger end of this age range; there have been no treatment trials that have addressed anxiety specifically in adolescents with ASD. This is problematic given that anxiety likely becomes a more acute problem during adolescence for many with ASD. Thus, a gap exists in empirically based treatment approaches for adolescents with ASD and co-occurring anxiety.
Development of the Treatment Program
Rationale and ‘Essential Elements’ of Treatment
Multimodal Anxiety and Social Skills Intervention (MASSI) is based on the principles of CBT, addressing an individual’s thoughts, feelings, and actions, as well as the interactions among these three domains, to bring about desired changes. With a focus on the present, CBT is action-oriented and tends to be a relatively time-limited intervention (i.e., typically 12–16 sessions). The intervention is didactic in nature; the therapist and adolescent work collaboratively to explore how cognitions contribute to anxious feelings and avoidance behaviors and, in turn, how these feelings and behaviors contribute to faulty cognitions. Interpersonal relationships with family and peers are also important considerations in treatment planning, and social skills development is often one goal of a cognitive-behavioral intervention (Kendall et al. 2003). Considerable empirical evidence supports the efficacy of CBT for treating childhood anxiety (Kendall et al. 2003; Ollendick and King 1998; Walkup et al. 2008). As noted above, there is emerging evidence for the utility of CBT in youth with ASD with secondary anxiety problems (Sofronoff et al. 2005; Reaven and Hepburn 2003) and mood disorders (Attwood 2004).
MASSI also draws from the principles of applied behavior analysis (ABA), which assumes that behaviors have a function or purpose. Intervention is targeted at teaching appropriate behaviors to meet an individual’s goals (needs, preferences, etc.), or replacing undesirable behaviors with more acceptable behaviors that will have the same function. ABA has a strong research record of effectiveness with people with ASD (Foxx 2008; Green 1996; Schreibman 2000). Although behaviorally based social skills instruction for youth with ASD is not currently considered an ‘empirically supported treatment,’ behaviorally based strategies delivered in a group format appear promising for these youth (White et al. 2007). Older children and teenagers with ASD, especially those who are cognitively higher functioning, live in a complex and dynamic social milieu. Fluid use of appropriate social skills in this milieu requires naturalistic training, intensive teaching and feedback, and multiple practice opportunities with peers.
In developing a treatment program specifically for people with ASD, we have attempted to address the unique challenges and strengths often associated with ASD. As such, several ‘essential elements’ believed to be particularly relevant to working with youth who have ASD are included in the treatment. These essential elements are embedded into the curriculum across the three treatment components (parental involvement, individual therapy, and group treatment). The first element is a focus on parent and family involvement. Regardless of whether the diagnosis was made early in the child’s life or not until adolescence, parents have had to struggle alongside their child. They have had to accept the diagnosis and come to an understanding that, as opposed to most other psychiatric disorders of childhood, there is no cure for autism and related conditions and the prognosis is often poor (e.g., Howlin et al. 2004; Engstrom et al. 2003). People with ASD often lack non-familial support systems that develop naturally for most people, further heightening the importance of family supports. Finally, adolescents are encouraged to practice new skills at home with siblings and parents, and relationships with family members are often a focus of the intervention. For these reasons, it is critical to include the individual’s primary caretaker(s), usually the parent, in the treatment. In a randomized trial of CBT for anxiety reduction with children, ages 10–12, with Asperger’s Disorder, Sofronoff et al. (2005) found that CBT that included parent involvement was superior to child-only treatment in reducing anxiety symptoms in the children as well as helping the parents feel more competent and empowered.
MASSI involves regular practice. Parents and clinicians often lament that skills learned in one context do not easily generalize to the child’s daily life. This may be due to problems with retrieval of previously learned skills and knowledge (e.g., Minshew et al. 1997) and to problems with context-dependent learning. Learning and repeated practice of new skills in contexts that approximate, as closely as possible, the situations and environments in which the child needs to use the skill is a strategy often recommended to address this concern (Bellini and Akullian 2007; Bellini et al. 2007). Unfortunately, intervening directly with the child in his or her classroom while peers are present, albeit the target environment for many children, is intrusive and usually not feasible. Offering ample practice opportunities during treatment to ensure a high enough ‘dosage’ was an important consideration in MASSI’s development. In the individual therapy sessions, there is practice of newly learned skills via role-play and exposure exercises. The group therapy component offers the opportunity to practice social skills in a relatively naturalistic yet highly supportive environment. Parents are involved in the therapy on a weekly basis and are asked to practice the skills and exercises with the teens at home and in the community. Thus, practice occurs in multiple environments and with different people and situations, with the goal of promoting generalization of treatment gains and flexibility of skill use. The skills should be learned and practiced in situations and environments that approximate, as closely as possible, those situations and environments in which the child is expected to actually use the skills.
MASSI therapists focus on immediate, direct, and specific feedback on performance and effort. The therapist and the individual’s parents provide direct feedback to the adolescent on implementation of new skills. One characteristic typical of people with ASD is a failure to pick up on subtle cues or reminders. Immediate, direct, ‘in the moment’ feedback—as opposed to general feedback that is delayed— is most effective. Common problems in youth with ASD, including difficulties with sustained attention and difficulties distinguishing essential from irrelevant details (e.g., Klin et al. 2003), underscore the importance of immediate and specific feedback as well as directive teaching. Providing age-appropriate explanations for why a given behavior is good (or not) in a given situation can be very helpful, as it gives the logic or rationale of a given (re)action. Frequently, in both individual and group therapy, the teens are shown clips of their own social behaviors (from previously recorded group sessions) to demonstrate specific skills or skill deficits and given feedback about those behaviors.
Yet another essential element embedded throughout the program is an emphasis on corrective, positive social learning experiences. By the time they reach adolescence, many individuals with ASD have experienced considerable social failure and rejection. Exclusion by peers, including explicit rejection and physical and emotional victimization, is not uncommon. One of the foci of the treatment, therefore, is to provide a corrective, positive social learning experience. Peer acceptance is highly valued during adolescence. For many teens in this program, the group experience will be their first time meeting other people with ASD and experiencing social acceptance in a peer group. Feeling safe to try new skills in such a supportive environment is critical to mastery of the material. Dedicated time for building group cohesion and establishing group ‘rules’ agreed upon by all participants helps to instill a sense of safety and comfort in the group environment.
Modeling new skills is important in the program given that many higher functioning individuals with ASD do not respond appropriately in social situations because they do not know how to respond or what to say despite having an awareness of the need to do something (Loveland and Tunali-Kotoski 2005). Modeling demonstrates what should be done in a given situation and increases the likelihood that the adolescent will learn the skill. MASSI employs a great deal of modeling (e.g., by the therapist in individual therapy, by peer tutors in the group component). In the program, the model attempts to explicitly state what they are feeling and doing during the modeled skill (e.g., “even though I feel nervous about how she will respond, I will smile and say ‘hello’ because that is how I should greet someone”).
Psychoeducation and explicit teaching about ASD and anxiety occur in every module and across all treatment modalities. Difficulties with attention and with monitoring and evaluating one’s own behavior necessitate direct, explicit teaching and feedback. Likewise, deficits in Theory of Mind skills (e.g., Baron-Cohen 1995; Colle et al. 2007) make recognizing and accurately interpreting the emotions, intentions, and behaviors of others difficult. Neuropsychological deficits in social cognition, such as inferring someone’s affect from their facial expression and judging someone’s trustworthiness, have indeed been documented in autism (Losh et al. 2009). An adolescent with ASD, for example, might not recognize that he has accidentally offended someone. Afterward he may perceive that peers are excluding him, but not understand why. Honest, candid explanation of how the teen’s behavior (appearance, statements, etc.) affects how other people treat him can be quite powerful. This type of teaching is done in individual and group therapy, and parents are educated on relevant aspects of ASD and anxiety as well. Explanations in MASSI are straightforward and, whenever possible, use analogies and examples drawing from the client’s special area(s) of interest.
Although modules do not have ‘scripts’ for the therapist to follow verbatim, MASSI is delivered in a structured way. Each session follows the same structured agenda and the manual provides examples about how to deliver the content of each module. The aim of the manual is to promote flexible implementation of the treatment, while maintaining consistency across therapists and clients. Other interventions (e.g., Johnson et al. 2007; Chorpita 2007) have developed this type of ‘flexible delivery,’ providing therapist guidance and key objectives/material to be delivered without set scripts to follow. Deficits in executive functioning, including the ability to plan ahead, stay on-task, and shift between tasks purposefully, are often reported in people with ASD (Ozonoff 1997; Ozonoff and Jensen 1999). The same sequence of activities in each session helps participants know what to expect and shift between activities, which may reduce anxiety related to unpredictability in the session.
Therapeutic rapport is instrumental in the success of most therapeutic interventions with children (Karver et al. 2006; Shirk and Karver 2003), including manual-based CBT programs (Shirk et al. 2008). This may be especially difficult to achieve in youth with ASD. In MASSI, the therapist is encouraged to take time at the onset of each session, especially in the initial meetings, to get to know the individual and his or her family and to help the teen feel comfortable with the therapy process. The tasks asked of the youth in the program (i.e., facing anxiety-provoking stimuli and practicing new social skills) are challenging and demanding and require active involvement and engagement. To promote successful outcomes, the adolescent must be willing to take risks to confront anxiety-provoking situations. Therapeutic rapport is likely enhanced when there is a spirit of collaboration between client and therapist and when the adolescent trusts the therapist (e.g., Chu et al. 2004).
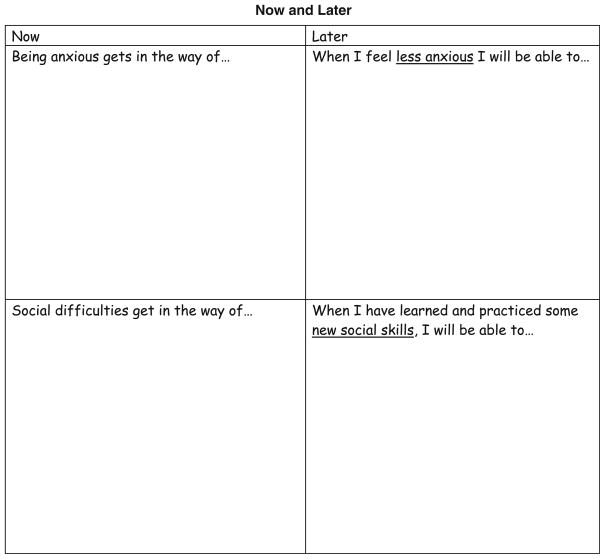
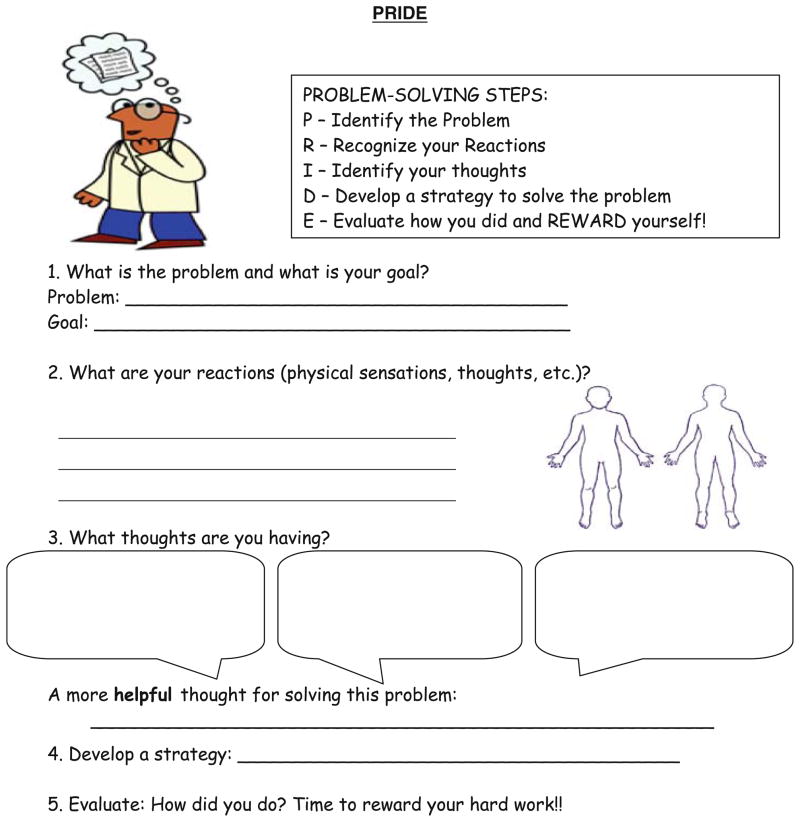
Finally, MASSI emphasizes the integration of creative, alternative, and varied teaching strategies. In addition to traditional verbal explanation and examples, the curriculum includes visual supports, writing and drawing activities, and other approaches (e.g., drama, tactile reminders) to teach concepts and skills (see Figs. 2 and 3 for examples of curriculum handouts). The therapist is encouraged to be imaginative and develop teaching aides and examples that incorporate individuals’ special interests. Many people with ASD struggle with recall of previously learned material out of context, but do quite well when given specific cues or reminders (Tsatsanis 2004). For clients with stronger visual-spatial than verbal abilities, for instance, extra time may be taken to develop imagery (e.g., a cartoon character or symbol) that cues the client to utilize a learned relaxation technique or coping strategy. On the other hand, if the client relies on language to reason and understand new concepts, the therapist and client may identify shared terms, or even create new words, to describe certain emotions and responses. Allowing for individualization of the intervention promotes learning of therapeutic concepts and acquisition of skills. Exploration of possible sensory issues (e.g., aversions), restricted interests, and needs for sameness or rituals that may directly or indirectly contribute to anxiety and appropriate social skill use is encouraged. Finally, the therapist must keep an eye on the various ways that anxiety might be expressed. An increase in oppositional behavior toward parents or in stereotypies or rituals, for example, may signal heightened anxiety.
Fig. 2.
Example of handout from curriculum
Fig. 3.
Example of handout from curriculum
These essential elements are integrated throughout the curriculum. Drawn from available research on psychosocial treatments for ASD and clinical experience with this population, these elements have not yet been empirically evaluated. They are, however, based on research on the cognitive and learning styles of people with ASD and theoretical explanations of ASD-social deficits. At this time, they are only hypothesized to be important to treatment outcome. Further inquiry is needed to evaluate whether this package of therapeutic elements is feasible and effective.
Content of the Program
Development of a structured psychosocial intervention can be conceptualized as a stepwise process. The first step, or stage, includes manual writing, development of therapist training procedures, initial pilot testing, and identification of measures to track adherence to the protocol (Carroll and Nuro 2002). Subsequently, the treatment is evaluated for efficacy via controlled clinical trials (Stage II) and then evaluated in effectiveness studies (Stage III) to determine its applicability in real-world clinical settings (i.e., transportability). The work presented in this paper is representative of Stage I—manual development.
The alpha version of the treatment program used in this pilot study was also the product of an iterative process that involved consultation with experts in the fields of autism and anxiety and clinical researchers with expertise in treatment development, integration of relevant research, clinical feedback, and ongoing revision. Following a thorough review of the scientific and applied literature on social competence deficits in autism, treatment approaches for higher functioning individuals with ASD, evidence-based approaches for the treatment of childhood anxiety, and the phenomenology of anxiety in individuals with ASD, a broad conceptual framework for the treatment was developed.
In the resulting intervention program, MASSI, anxiety and social interaction deficits are conceptualized as reciprocal influences. For example, some teens with ASD may develop anxiety about peer interactions based on recurrent negative social experiences. These negative experiences can often be attributed to the social skill deficits inherent to ASD. For other youngsters, anxiety may be connected with their restricted interests. For example, a fear of tornadoes may develop in a child with an intense interest in the weather. The anxiety then becomes a further hindrance to social-emotional development and effective social interactions. As these examples demonstrate, in this conceptualization anxiety may be regarded as separate from ASD, but closely connected to the social deficits that are fundamental to the diagnosis. It is probable that, for some youngsters with ASD, co-occurring problems with anxiety serve to limit the effectiveness of interventions targeting social skill development. Indeed, the clinical impact and generalizability of social skills training for people with ASD has been questioned (e.g., Rao et al. 2008; White et al. 2007). We speculate that it may be necessary to intervene with the anxiety problem as well as focus on social competence, when anxiety is present, to reap maximum benefit and promote skill use outside of the clinical setting.
In most cases, because of the pervasive nature of social skill deficits in ASD and the often more acutely distressing nature of anxiety, MASSI addresses the anxiety symptoms initially before proceeding to social skill development. Socialization problems represent a longstanding and persistent concern for youth with ASD, whereas problems with anxiety often arise secondarily and tend to be viewed by the client and family as more problematic and acute (Fig. 1). In addition, anxiety reduction may be a more readily observable outcome—attainment of which can contribute to greater self-efficacy and increased motivation to work on ‘core’ social deficits. Moreover, some aspects of effective social functioning (e.g., emotional regulation) can also be enhanced directly by reducing anxiety. This is, of course, variable across clients. In some adolescents, for instance, specific social skill deficits may need to be addressed therapeutically in order for them to be able to carry out effective social exposure exercises to combat their anxiety.
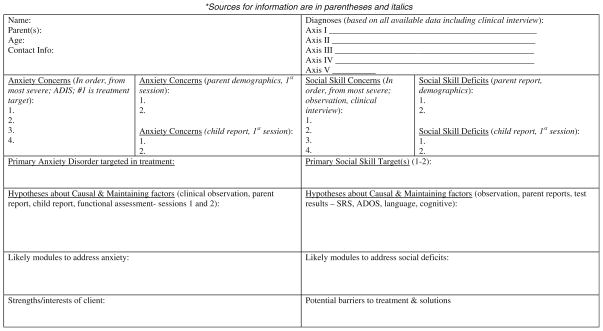
When beginning MASSI, an individual adolescent’s clinical presentation is carefully considered. The therapist formulates hypotheses about the nature of the anxiety and the factors contributing to social deficits based on data drawn from clinical assessments and observations, as well as information provided by the adolescent and her parents. Based on this Case Conceptualization (see Fig. 4), a treatment plan is designed and implemented. Ongoing data collection informs how the program should be tailored as treatment progresses. A modular approach to treatment delivery was selected to allow for maximum individualization of the treatment across participants, while adhering to the theoretical model underlying the program (Chorpita 2007). Selection of treatment modules is based on the participant’s Case Conceptualization, a ‘living’ document modified as needed throughout treatment. In the Case Conceptualization, the therapist forms hypotheses about problems and targets for intervention (i.e., causal and maintaining factors); based on feedback from the participant and parents, as well as direct observation, the conceptualization is dynamic and modified as needed. Principal targets for intervention and the treatment goals identified by the adolescent and his or her parent help determine what treatment modules are selected specifically to address anxiety (e.g., Coping with Worry, Exposure) and social skill deficits (e.g., Initiating with Peers, Conversational Skills). Typically, the MASSI therapist selects at least two modules for each area—anxiety and social skill deficits. At least midway through treatment, the therapist evaluates the progress being made toward treatment goals and revises the Conceptualization. Based on the adolescent’s progress and how well they have learned and applied the content of treatment, other modules may be delivered or modules may be repeated as needed.
Fig. 4.
Case Conceptualization
Structure of the Program
The three treatment modalities of the curriculum are (1) individual therapy for the adolescent, (2) group treatment (social skills training and practice), and (3) parent education and involvement. Any one of these three treatment modalities, if used alone, has potential limitations such as poor generalization of treatment gains to peer interactions (with individual therapy alone), lack of individualization of the treatment (with group treatment alone), and difficulty with controlling treatment dosage fidelity, and assessing impact using traditional parent-report measures (with parent training/education alone). Alternatively, multimodal intervention that cuts across domains in the youngster’s life provides more opportunities to practice specific skills in different contexts, which presumably increases the likelihood of successful generalization.
Social interaction is a highly variable, fluid skill—exactly the type of skill that tends to be most difficult for people with ASD, who often do better in predictable contexts that call for rule-bound behavior. Knowing the right things to say and do in a given social exchange depends on context, including who you are with (e.g., teacher versus classmate), what else is happening (e.g., free time in class versus a review activity right before a big exam), the immediate environment (e.g., study hall versus basketball game), and a host of other factors. Many adolescents with ASD have a desire to improve their social skills and make friends (Bauminger and Kasari 2000), yet have great difficulty knowing when and where to use acquired skills in real world settings. Thus, the rationale for this multi-modal program is to maximize therapeutic gain in an efficient way that promotes skill generalization and maintenance over time. The three treatment modalities of the MASSI Program are described in the next paragraph.
Individual Therapy
In individual therapy, empirically supported strategies for treatment of childhood anxiety (e.g., exposure, cognitive challenges, education) are integrated with empirically supported strategies for teaching appropriate social skills (e.g., modeling, feedback, social reinforcement, role-play practice). By providing therapy in a one-on-one format, the therapist is able to individualize the program to meet the unique needs of the client. Both behavioral aspects (e.g., discrete social skills, addressing competing or interfering behaviors) and cognitive influences (e.g., attribution style, mood regulation) of anxiety and social deficits are addressed.
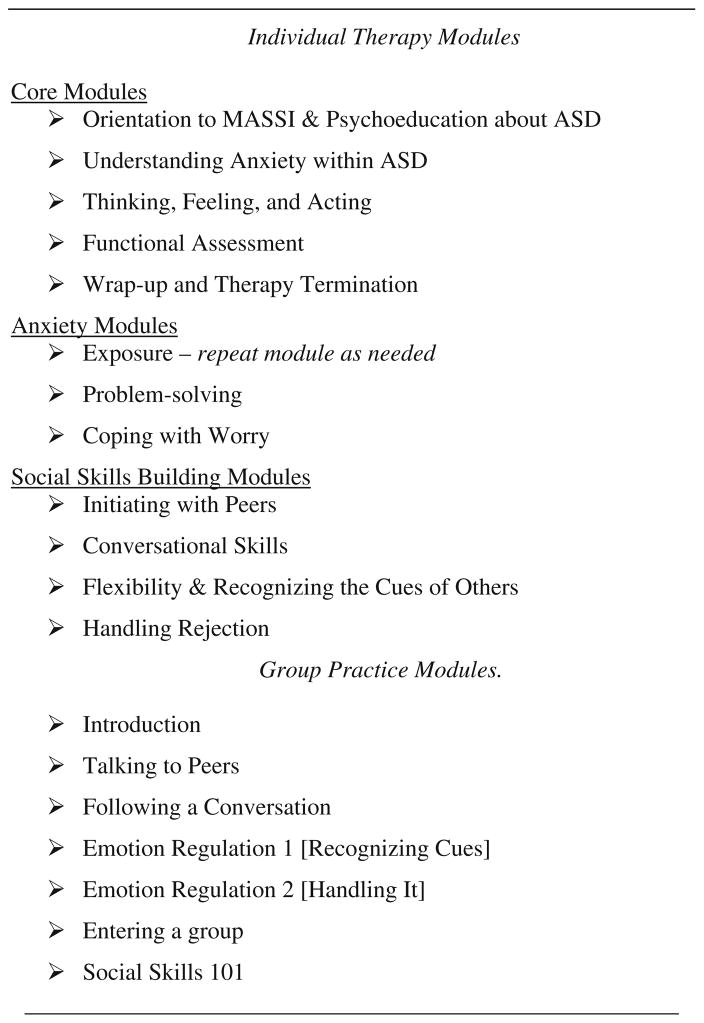
The manual comprises 12 individual therapy modules. The first four individual therapy modules are considered ‘core’ and are delivered sequentially for every participant as their intent is to provide the requisite knowledge for understanding material presented later in the program (see Fig. 5). These ‘core’ modules address orientation to the therapy and homework assignments, explanation of the relationships among thoughts, feelings, and behaviors, psychoeducation about anxiety and ASD, and how to recognize internal states (both feelings and thoughts). A fifth core module is delivered in the final session and serves as a review and wrap-up. Beyond this core, the other treatment modules selected for inclusion are based on the specific needs and skill deficits of the individual. Treatment sessions last approximately 50–75 min, and each is devoted to one module. Given its format, clients may not receive the same selection of modules and modules are repeated as necessary with a client within the maximum number of 13 total sessions. The fact that ASD expresses itself uniquely across individuals necessitates a therapeutic approach that is also individualized.
Fig. 5.
MASSI Modules
Group Therapy
The group therapy is designed to supplement the individual CBT, providing an opportunity for participants to practice specific social skills and anxiety management strategies with peers in a relatively naturalistic but low-stress setting. This treatment modality begins approximately 3 weeks after the beginning of individual therapy and continues concurrently throughout the remainder of the individual therapy. Five, 60-minute group therapy sessions, occurring approximately every other week, cover skills such as talking to peers, entering groups, and emotional regulation. All participants in MASSI are invited to attend all the group sessions.
Information processing weaknesses associated with ASD necessitate repeated practice opportunities and contribute to problems with generalization and skill maintenance. To address these concerns, the group component emphasizes behavioral practice within a supportive environment. The group component is intended to provide a positive social learning experience with peers, which can further motivate adolescents to continue to develop their skills and to work on making friends. A positive group experience can also reduce the inclination to escape social situations.
Parent Involvement
Parents are actively involved in the program, acting as ‘coaches’ for exposure exercises during the week, assisting with other between-session homework activities, and making environmental adaptations as needed. They might, for instance, encourage and reinforce their teen’s implementation of desired target behaviors or set up situations allowing the adolescent to interact with peers in a one-on-one setting. Parent involvement is sought in order to promote skill generalization and to gather parents’ feedback about progress during the program. Parents join the individual therapy sessions for the last 10–20 min, at which time the adolescent is charged with summarizing the session for the parent, including what was learned and what the homework assignment is. Parents receive regular communication and support from the therapist, describing the skills their child is working on and offering suggestions as to how they might continue working on the particular skill(s) at home.
The adolescent is encouraged to summarize the content of the individual therapy session for their parent for two primary reasons. First, it helps the adolescent consolidate what she has learned by summarizing the content in their own words and it gives the therapist an opportunity to correct any misunderstandings. Second, it puts the adolescent more in control of what is shared with the parent, promoting a confidential therapist-adolescent relationship.
Treatment Feasibility
MASSI is designed for the treatment of adolescents (ages 12 through 17) with ASD and co-occurring anxiety disorders. Due to the verbal and learning demands of the treatment program and to ensure some similarity to peers in the group therapy component, participants must have sufficient language skills and adequate intellectual abilities, as determined by clinical interview and observation and by objective assessments. The program is deemed to be appropriate for co-occurring Social Phobia, Generalized Anxiety Disorder, Specific Phobia(s), or Separation Anxiety Disorder. Anxiety disorders not addressed in MASSI are Obsessive–Compulsive Disorder, Panic Disorder, and Post-Traumatic Stress Disorder, as these disorders frequently require specific types of treatment not included in the curriculum (Ollendick et al. 2006). Finally, MASSI has a targeted focus on social development and anxiety reduction; as such, it should not be used for the treatment of youth with co-occurring problems requiring more intensive and immediate treatment such as psychosis or severe, untreated clinical depression.
In an initial trial of MASSI to demonstrate the feasibility of the approach and explore possible efficacy (White et al. 2009a), four participants (ages 12–14, 2 males) completed the program using the alpha version of the treatment manual. Three participants were diagnosed with Asperger’s Disorder and one with PDD-NOS, based on a clinical interview and supported by the Autism Diagnostic Interview-Revised (ADI-R; Lord et al. 1994) and the Autism Diagnostic Observation Schedule (ADOS; Lord et al. 2000). All four participants met criteria for at least one anxiety disorder based on the Anxiety Disorders Interview Schedule for Children—Child/Parent versions (ADIS-C/P; Silverman and Albano 1996). One primary anxiety disorder was identified for each participant as the focus of treatment: two participants had Social Phobia, another had a Specific Phobia (Blood-Injection-Injury: BII), and the remaining one had Generalized Anxiety Disorder. All but one participant met criteria for multiple anxiety disorders. Feasibility based on this pilot study is briefly discussed herein, as the focus of the White et al. paper (2009a; note that the program in that publication is referred to by its previous name—MCIT) was exploratory in nature and designed to demonstrate initial efficacy and effect size estimation.
Treatment feasibility can be defined as a product of treatment integrity, adherence to the treatment, and consumer satisfaction (Pavuluri et al. 2004). In this pilot study, feasibility was assessed three ways: (1) integrity of the treatment intervention (the degree to which the therapist delivered treatment as intended), (2) adherence to the protocol by the adolescent and his family (attendance at scheduled sessions and completion of between-session homework), and (3) consumer satisfaction with the program (how helpful parents and adolescents viewed the program). A treatment integrity checklist was used to record the degree to which the treatment objectives for each therapy module were delivered as intended. Following each session, the therapist recorded how many of the module’s intended treatment objectives were actually completed. Integrity was assessed as a percentage [# of delivered treatment components/number of planned components for that session * 100] (Pavuluri et al. 2004), with a benchmark of 80% set as a minimally acceptable level. Integrity was computed for every module. When a module was repeated for one or more of the families, that module’s reported integrity represented the average across administrations so that each module received only one overall integrity rating for each subject. Across the 12 modules included in the treatment program, overall integrity ranged from 81.25 to 100%, with a mean of 92.5%. No modules fell below the 80% cutoff for acceptable treatment integrity.
Adherence, defined as the degree to which participants in the program accepted and followed the treatment curriculum, included attendance at scheduled sessions and compliance with prescribed homework assignments. All participants completed the program, and every participant received at least 12 individual therapy sessions. Although it was necessary to reschedule some appointments due to scheduling conflicts, there were no missed appointments. Sessions ranged in length from 48 to 75 min (M = 58 min.). Following each session, the therapist rated how involved the client was (i.e., degree to which s/he participated in session activities and volunteered information). Averaged across participants, involvement ranged from 3.33 to 5, on a 1 (uninvolved) to 5 (actively involved) scale (M = 4.20). The third indicator of adherence, compliance with assigned between-session homework, was rated by the therapist on a 1–4 scale: 1 (client did not complete homework), 2 (client completed homework but did not bring it in, or partially completed it), 3 (client brought in completed homework), 4 (not applicable). As homework was assigned at the end of every treatment session, the only module that received ratings of 4 (N/A) was Orientation, as it was the first session. Clients generally completed assigned homework between sessions, at least partially. Averaged across participants, compliance ranged from 1 to 3, with an average score across modules of 2.10.
Consumer satisfaction with the content and delivery of the program was assessed via a brief Satisfaction Questionnaire, which was completed separately by the adolescent and the parent after every session and at the completion of the program. The questionnaire asked about satisfaction with the treatment, including the relevance of homework, adequacy of delivery, and overall content. To avoid biased responses, it was explained to the families that the therapist would not see their responses until after the program ended, and the parent and adolescent completed and sealed their completed questionnaires in envelopes following each session when the therapist was out of the room. Results indicated that the youth generally found the sessions helpful (range: 4–10, M = 7.21 ± 1.66, on 1–10 scale) and overall program satisfaction was quite high (range: 7–10, M = 7.75 ± 1.50). Individual therapy was rated as most helpful by the adolescents, followed by group therapy. Parents also rated the sessions as helpful (range: 5–10, M = 8.33 ± 1.58) with program satisfaction equally high (8–10, M = 8.75 ± .96). Individual therapy was rated as the most useful component by parents, followed by between-session assignments.
Conclusions/Implications
Anxiety symptoms and anxiety disorders are relatively common among young people with ASD. When present, anxiety may contribute to impairment above and beyond the social disability that is fundamental to these disorders. Furthermore, anxiety is more likely to be problematic among cognitively higher functioning individuals with ASD as they enter adolescence. Surprisingly little research has systematically evaluated treatment that dually targets anxiety and social competence in this adolescent population. This review briefly described the development of a psychosocial treatment program designed specifically for adolescents who have ASD and co-occurring anxiety disorders, and presented initial feasibility data based on a pilot study.
Preliminary feasibility data are promising, indicating that the program was acceptable to consumers and that it could be delivered across four participants. Initial findings also show that the program can be delivered as intended (treatment integrity) and that clients generally adhere to the curriculum (session attendance, engagement). Although between-session homework completion was variable across participants and modules, most assigned treatment homework was at least partially completed. Consumers indicated that the individual therapy component of the program was most useful.
This evaluation of program feasibility has several limitations. Although the purpose was to pilot the intervention and gather initial feasibility data with which to make further refinements to the curriculum, the fact that a single therapist delivered the intervention to only four participants limits the generalizability of conclusions. Second, although its modular format allows for a fair degree of flexibility in delivery, this intervention is neither comprehensive nor completely individualized. It targets only anxiety reduction and development of social competence. Finally, evaluating ‘dosage’ effects is challenging in this type of multi-faceted treatment. Some participants (and parents) were more motivated, and/or able, to master the curriculum and practice skills between sessions. Although not unique to this program, the fact that MASSI delivers treatment across three modalities adds complexity to attempts to understand the differential utility of aspects of the intervention (e.g., group therapy versus parent training). As efficacious treatments for ASD are identified and refined, further inquiry will be needed to dismantle treatments into their component parts, and to use randomized group design outcome studies and meta-analyses evaluating mediators and moderators of treatment response.
Based on these initial findings, a randomized clinical trial to evaluate efficacy is currently underway (Phase II, treatment development; Carroll and Nuro 2002), which will address some of these limitations. Multiple therapists are delivering the program, allowing for evaluation of therapist training procedures and assessment of uniformity in delivery across therapists as well as clients. A larger, more diverse sample will receive the treatment, randomized to either receive treatment immediately or enter a wait-list condition. The treatment curriculum and fidelity assessment measures have also been modified based on feedback from parents and participants and clinical observations from the pilot. In summary, the development of this program represents a natural step in the progression of psychosocial treatments for higher functioning young people with ASD. Future research will evaluate its efficacy and more fully assess the program’s acceptability and feasibility.
Acknowledgments
This project was supported by a grant from the National Institute of Mental Health [1K01MH079945-01; PI: S. W. White]. The authors acknowledge consultation from the grant’s full advisory panel, which includes: Matthew Fritz, PhD, Angela Scarpa, PhD, and Michael Southam-Gerow, PhD in addition to the authors of this paper. We also thank the participants in this study and their parents.
References
- Attwood T. Cognitive behaviour therapy for children and adults with Asperger’s syndrome. Behaviour Change. 2004;21:147–161. [Google Scholar]
- Baron-Cohen S. Mindblindness: An essay on autism and theory. Cambridge, MA: MIT Press; 1995. [Google Scholar]
- Bauminger N, Kasari C. Loneliness and friendship in high-functioning children with autism. Child Development. 2000;71:447–456. doi: 10.1111/1467-8624.00156. [DOI] [PubMed] [Google Scholar]
- Beaumont R, Sofrononoff K. A multi-component social skills intervention for children with Asperger syndrome: The junior detective training program. The Journal of Child Psychology and Psychiatry. 2008;49(7):743–753. doi: 10.1111/j.1469-7610.2008.01920.x. [DOI] [PubMed] [Google Scholar]
- Bellini S. Social skill deficits and anxiety in high-functioning adolescents with autism spectrum disorders. Focus on Autism and Other Developmental Disabilities. 2004;19:78–86. [Google Scholar]
- Bellini S. The development of social anxiety in adolescents with autism spectrum disorders. Focus on Autism and Other Developmental Disabilities. 2006a;21:138–145. [Google Scholar]
- Bellini S. Building social relationships: A systematic approach to teaching social interaction skills to children and adolescents with autism spectrum disorders and other social difficulties. Shawnee Mission, KS: Autism Asperger Publishing Co; 2006b. [Google Scholar]
- Bellini S, Akullian J. A meta-analysis of video modeling and video self-modeling interventions for children and adolescents with autism spectrum disorders. Exceptional Children. 2007;73(3):264–287. [Google Scholar]
- Bellini S, Peters JK, Benner L, Hopf A. A meta-analysis of school-based social skills interventions for children with autism spectrum disorders. Remedial and Special Education. 2007;28(3):153–162. [Google Scholar]
- Bradley EA, Summers JA, Wood HL, Bryson SE. Comparing rates of psychiatric and behavior disorders in adolescents and young adults with severe intellectual disability with and without autism. Journal of Autism and Developmental Disorders. 2004;34:151–161. doi: 10.1023/b:jadd.0000022606.97580.19. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Nuro KF. One size cannot fit all: A stage model for psychotherapy manual development. Clinical Psychology Science and Practice. 2002;9:396–406. [Google Scholar]
- Carter A, Davis N, Klin A, Volkmar F. Social development in autism. In: Volkmar FR, Paul R, Klin A, Cohen D, editors. Handbook of autism and pervasive developmental disorders. 3. Hoboken, NJ: Wiley; 2005. pp. 312–334. [Google Scholar]
- Chalfant A, Rapee R, Carroll L. Treating anxiety disorders in children with high functioning autism spectrum disorders: A controlled trial. Journal of Autism and Developmental Disorders. 2007;37:1842–1857. doi: 10.1007/s10803-006-0318-4. [DOI] [PubMed] [Google Scholar]
- Chorpita BF. Modular cognitive-behavioral therapy for childhood anxiety disorders. In: Persons JB, editor. Guides to individualized evidence-based treatment. New York: Guilford; 2007. [Google Scholar]
- Chu BC, Choudhury MS, Shortt AL, Pincus DB, Creed TA, Kendall PC. Alliance, technology, and outcome in the treatment of anxious youth. Cognitive and Behavioral Practice. 2004;11:44–55. [Google Scholar]
- Colle L, Baron-Cohen S, Hill J. Do children with autism have a theory of mind? A non-verbal test of autism vs. specific language impairment. Journal of Autism and Developmental Disorders. 2007;37(4):716–723. doi: 10.1007/s10803-006-0198-7. [DOI] [PubMed] [Google Scholar]
- DeWit DJ, Ogborne A, Offord DR, MacDonald K. Antecedents of the risk of recovery from DSM-III-R social phobia. Psychological Medicine. 1999;29:569–582. doi: 10.1017/s0033291799008399. [DOI] [PubMed] [Google Scholar]
- Engstrom I, Ekstrom L, Emilsson B. Psychosocial functioning in a group of Swedish adults with Asperger syndrome of high-functioning autism. Autism. 2003;7:99–110. doi: 10.1177/1362361303007001008. [DOI] [PubMed] [Google Scholar]
- Foxx RM. Applied behavior analysis treatment of autism: The state of the art. Child and Adolescent Psychiatric Clinics of North America. 2008;17:821–834. doi: 10.1016/j.chc.2008.06.007. [DOI] [PubMed] [Google Scholar]
- Ghaziuddin M. Asperger syndrome: Associated psychiatric and medical conditions. Focus on Autism and Other Developmental Disabilities. 2002;17:138–144. [Google Scholar]
- Grant BF, Hasin DS, Blanco C, Stinson FS, Chous SP, Goldstein RB, et al. The epidemiology of social anxiety disorder in the United States: Results from the national epidemiologic survey on alcohol and related conditions. Journal of Clinical Psychiatry. 2005;66:1351–1361. doi: 10.4088/jcp.v66n1102. [DOI] [PubMed] [Google Scholar]
- Green G. Early behavioral intervention for autism: What does research tell us? In: Maurice C, Green G, Luce SC, editors. Behavioral intervention for young children with autism: a manual for parents and professionals. Austin, TX: Pro-Ed; 1996. [Google Scholar]
- Howlin P, Goode J, Hutton J, Rutter M. Adult outcome for children with autism. Journal of Child Psychology and Psychiatry. 2004;45:212–229. doi: 10.1111/j.1469-7610.2004.00215.x. [DOI] [PubMed] [Google Scholar]
- Johnson CR, Handen BJ, Butter E, Wagner A, Mulick J, Sukhodolsky DG, et al. Development of a parent training program for children with pervasive developmental disorders. Behavioral Interventions. 2007;22:201–221. [Google Scholar]
- Karver MS, Handelsman J, Fields S, Bickman L. Meta-analysis of therapeutic relationship variables in youth and family therapy: The evidence for different relationship variables in the child and adolescent treatment outcome literature. Clinical Psychology Review. 2006;26(1):50–65. doi: 10.1016/j.cpr.2005.09.001. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Aschenbrand SG, Hudson JL. Child-focused treatment of anxiety. In: Kazdin AE, Weisz JR, editors. Evidence-based psychotherapies for children and adolescents. New York: Guilford Press; 2003. [Google Scholar]
- Klin A, Jones W, Schultz R, Volkmar F. The enactive mind—from actions to cognition: Lessons from autism. In: Cohen DJ, Volkmar FR, editors. Handbook of autism and pervasive developmental disorders. 2. New York: Wiley; 2003. pp. 682–704. [Google Scholar]
- Klin A, Volkmar FR. Treatment and intervention guidelines for individuals with Asperger syndrome. In: Klin A, Volkmar FR, Sparrow SS, editors. Asperger syndrome. New York: Guilford Press; 2000. pp. 340–366. [Google Scholar]
- Kuusikko S, Pollock-Wurman R, Jussila K, Carter AS, Mattila M, Ebieling H, et al. Social anxiety in high-functioning children and adolescents with autism and Asperger syndrome. Journal of Autism and Developmental Disorders. 2008;38:1697–1709. doi: 10.1007/s10803-008-0555-9. [DOI] [PubMed] [Google Scholar]
- Lehmkuhl HD, Storch EA, Bodfish JW, Geffken GR. Brief report: Exposure and response prevention for obsessive compulsive disorder in a 12-year-old with autism. Journal of Autism and Developmental Disorders. 2008;38:977–981. doi: 10.1007/s10803-007-0457-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C, Risi S, Lambrecht L, Cook EH, Jr, Leventhal BL, DiLavore PC, et al. The autism diagnostic observation schedule-generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders. 2000;30:205–223. [PubMed] [Google Scholar]
- Lord C, Rutter M, LeCouteur A. Autism diagnostic interview-revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders. 1994;24:659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- Losh M, Adolphs R, Poe MD, Couture S, Penn D, Baranek GT, et al. Neuropsychological profile of autism and broad autism phenotype. Archives of General Psychiatry. 2009;66(5):518–526. doi: 10.1001/archgenpsychiatry.2009.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loveland KA, Tunali-Kotoski B. The school-age child with an autistic spectrum disorder. In: Volkmar FR, Paul R, Klin A, Cohen D, editors. Handbook of autism and pervasive developmental disorders. 3. New York: Wiley; 2005. pp. 247–287. [Google Scholar]
- Lyneham HJ, Abbott MJ, Wignall A, Rapee RM. The cool kids family program—therapist manual. Sydney, Australia: Macquarie University; 2003. [Google Scholar]
- McAfee J. Navigating the social world: A curriculum for individuals with Asperger’s syndrome, high functioning autism and related disorders. Arlington, TX: Future Horizons; 2001. [Google Scholar]
- Minshew NJ, Goldstein G, Siegel DJ. Neuropsychologic functioning in autism: Profile of a complex information processing disorder. Journal of the International Neuropsychological Society. 1997;3:303–316. [PubMed] [Google Scholar]
- Myles B. Behavioral forms of stress management for individuals with Asperger syndrome. Child and Adolescent Psychiatric Clinics of North America. 2003;12:123–141. doi: 10.1016/s1056-4993(02)00048-2. [DOI] [PubMed] [Google Scholar]
- Myles B, Barnhill G, Hagiwara T, Griswold D, Simpson R. A synthesis of studies on the intellectual, academic, social/emotional and sensory characteristics of children with Asperger syndrome. Education and Training in Mental Retardation and Developmental Disabilities. 2001;36:304–311. [Google Scholar]
- Ollendick TH, King NJ. Empirically supported treatments for children with phobic and anxiety disorders: Current status. Journal of Clinical Child Psychology. 1998;27:156–167. doi: 10.1207/s15374424jccp2702_3. [DOI] [PubMed] [Google Scholar]
- Ollendick TH, King NJ, Chorpita BF. Empirically supported treatments for children and adolescents. In: Kendall PC, editor. Child and adolescents therapy: Cognitive-behavioral procedures. 3. New York, NY: Guilford Press; 2006. pp. 492–520. [Google Scholar]
- Ozonoff S. Causal mechanisms of autism: Unifying perspectives from an information-processing framework. In: Cohen DJ, Volkmar FR, editors. Handbook of autism and pervasive developmental disorders. 2. New York: Wiley; 1997. pp. 868–879. [Google Scholar]
- Ozonoff S, Jensen J. Brief report: Specific executive function profiles in three neurodevelopmental disorders. Journal of Autism and Developmental Disorders. 1999;29:171–177. doi: 10.1023/a:1023052913110. [DOI] [PubMed] [Google Scholar]
- Pavuluri MN, Graczyk PA, Henry DB, Carbray JA, Heidenreich J, Miklowitz DJ. Child- and family-focused cognitive-behavioral therapy for pediatric bipolar disorder: Development and preliminary results. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:528–537. doi: 10.1097/00004583-200405000-00006. [DOI] [PubMed] [Google Scholar]
- Rao PA, Beidel DC, Murray MJ. Social skills interventions for children with Asperger’s syndrome or high-functioning autism: A review and recommendations. Journal of Autism and Developmental Disorders. 2008;38:353–361. doi: 10.1007/s10803-007-0402-4. [DOI] [PubMed] [Google Scholar]
- Reaven J, Blakeley-Smith A, Nichols S, Dasari M, Flanigan E, Hepburn S. Cognitive-behavioral group treatment for anxiety symptoms in children with high-functioning autism spectrum disorders. Focus on Autism and Other Developmental Disabilities. 2009;24(1):27–37. [Google Scholar]
- Reaven J, Hepburn S. Cognitive-behavioral treatment of obsessive-compulsive disorder in a child with Asperger syndrome: A case report. Autism. 2003;7:145–164. doi: 10.1177/1362361303007002003. [DOI] [PubMed] [Google Scholar]
- Research Units on Pediatric Psychopharmacology [RUPP] Autism Network. Parent training for children with pervasive developmental disorders: A multi-site feasibility trial. Behavioral Interventions. 2007;22:179–199. [Google Scholar]
- Schreibman L. Intensive behavioral/psychoeducational treatments for autism: Research needs and future directions. Journal of Autism and Developmental Disorders. 2000;30:373–378. doi: 10.1023/a:1005535120023. [DOI] [PubMed] [Google Scholar]
- Shirk SR, Gudmundsen G, Kaplinski HC, McMakin DL. Alliance and outcome in cognitive-behavioral therapy for adolescent depression. Journal of Clinical Child & Adolescent Psychology. 2008;37(3):631–639. doi: 10.1080/15374410802148061. [DOI] [PubMed] [Google Scholar]
- Shirk SR, Karver M. Prediction of treatment outcome from relationship variables in child and adolescent therapy: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2003;71:452–464. doi: 10.1037/0022-006x.71.3.452. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. The anxiety disorders interview schedule for DSM- IV–Child and parent versions. San Antonio, TX: Graywind; 1996. [Google Scholar]
- Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:921–929. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- Smith T, Scahill L, Dawson G, Guthrie D, Lord C, Odom S, et al. Designing research studies on psychosocial interventions in autism. Journal of Autism and Developmental Disorders. 2007 doi: 10.1007/s10803-006-0173-3. [DOI] [PubMed] [Google Scholar]
- Sofronoff K, Attwood T, Hinton S. A randomized controlled trial of a CBT intervention for anxiety in children with Asperger syndrome. Journal of Child Psychology and Psychiatry. 2005;46:1152–1160. doi: 10.1111/j.1469-7610.2005.00411.x. [DOI] [PubMed] [Google Scholar]
- Sukhodolsky DG, Scahill L, Gadow KD, Arnold LE, Aman MG, McDougle CJ, et al. Parent-rated anxiety symptoms in children with pervasive developmental disorders: Frequency and association with core autism symptoms and cognitive functioning. Journal of Abnormal Child Psychology. 2008;36:117–128. doi: 10.1007/s10802-007-9165-9. [DOI] [PubMed] [Google Scholar]
- Sze KM, Wood JJ. Cognitive behavioral treatment of comorbid anxiety disorders and social difficulties in children with high-functioning autism: A case report. Journal of Contemporary Psychotherapy. 2007;37:133–143. [Google Scholar]
- Tantam D. The challenge of adolescents and adults with Asperger syndrome. Child and Adolescent Psychiatric Clinics of North America. 2003;12:143–163. doi: 10.1016/s1056-4993(02)00053-6. [DOI] [PubMed] [Google Scholar]
- Tsatsanis KD. Heterogeneity in learning style in Asperger syndrome and high- functioning autism. Topics in Language Disorders. 2004;24(4):260–270. [Google Scholar]
- Tse J, Strulovich J, Tagalakis V, Meng L, Fombonne E. Social skills training for adolescents with Asperger syndrome and high-functioning autism. Journal of Autism and Developmental Disorders. 2007;37:1960–1968. doi: 10.1007/s10803-006-0343-3. [DOI] [PubMed] [Google Scholar]
- United States Centers for Disease Control and Prevention. Prevalence of autism spectrum disorders-Autism and developmental disabilities monitoring network, 14 sites, United States, 2002. Surveillance Summaries, MMWR 2007. 2007;56(SS-1) [PubMed] [Google Scholar]
- Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, Sherrill JT, et al. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. The New England Journal of Medicine. 2008;359(26):2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisbrot DM, Gadow KD, DeVincent CJ, Pomeroy J. The presentation of anxiety in children with pervasive developmental disorders. Journal of Child and Adolescent Psychopharmacology. 2005;15:477–496. doi: 10.1089/cap.2005.15.477. [DOI] [PubMed] [Google Scholar]
- White SW, Koenig K, Scahill L. Social skills development in children with autism spectrum disorders: A review of the intervention research. Journal of Autism and Developmental Disorders. 2007;37:1858–1868. doi: 10.1007/s10803-006-0320-x. [DOI] [PubMed] [Google Scholar]
- White SW, Ollendick T, Scahill L, Oswald D, Albano A. Preliminary efficacy of a cognitive-behavioral treatment program for anxious youth with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2009 doi: 10.1007/s10803-009-0801-9. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- White SW, Oswald D, Ollendick T, Scahill L. Anxiety in children and adolescents with autism spectrum disorders. Clinical Psychology Review. 2009b;29(3):216–229. doi: 10.1016/j.cpr.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood JJ, Drahota A, Sze K, Har K, Chiu A, Langer DA. Cognitive behavioral therapy for anxiety in children with autism spectrum disorders: A randomized, controlled trial. Journal of Child Psychology and Psychiatry. 2009;50(3):224–234. doi: 10.1111/j.1469-7610.2008.01948.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood JJ, McLeod BM. Child anxiety disorders: A treatment manual for practitioners. New York: Norton; 2008. [Google Scholar]