Abstract
Safe and effective immunization of newborns and infants can significantly reduce childhood mortality, yet conventional vaccines have been largely unsuccessful in stimulating the neonatal immune system. We explored the capacity of a novel mucosal antigen delivery system consisting of non-living, non-genetically modified Lactococcus lactis particles, designated Gram-positive Enhancer Matrix (GEM), to induce immune responses in the neonatal setting. Yersinia pestis LcrV, used as model protective antigen, was displayed on the GEM particles. Newborn mice immunized intranasally with GEM-LcrV developed LcrV-specific antibodies, Th1-type cell-mediated immunity, and were protected against lethal Y. pestis (plague) infection. The GEM particles activated and enhanced the maturation of neonatal dendritic cells both in vivo and in vitro. These dendritic cells showed increased capacities for secretion of pro-inflammatory and Th1-cell polarizing cytokines, antigen presentation and stimulation of CD4+ and CD8+ T cells. These data show that mucosal immunization with L. lactis GEM particles carrying vaccine antigens represents a promising approach to prevent infectious diseases early in life.
INTRODUCTION
One of the major challenges in vaccinology is the development of safe and effective vaccines that can protect newborns and infants against infectious diseases. Conventional vaccines are notoriously poorly immunogenic during the first months of life, inducing immune responses that are short-lived and heavily Th2 biased. Th1-type cell-mediated immunity is modest or absent, and the combination of these factors heightens the risk of intracellular bacterial infections1–3. Even though routine immunization of human infants starts at 6 to 12 weeks of age, several booster doses are needed to achieve protective immunity. Mounting evidence indicates that these poor responses are not due to intrinsic deficiencies of the neonatal immune system, which has a fully constituted T cell repertoire and is capable of responding to antigens, but mainly to the presence of immature or “inexperienced” immune cells, particularly dendritic cells (DC), which have a limited capacity for antigen presentation and stimulation of naïve T cells1,3–5. The field of neonatal vaccinology has experienced unprecedented progress in recent years, and the literature supports the assertion that newborns are indeed capable of mounting potent adaptive immunity, including adult-like Th1-type immune responses to vaccine antigens, provided that these antigens are administered with the appropriate stimulatory signals1–3,5–7.
In this study, we examined the possibility of priming the neonatal immune system through mucosal immunization using a novel antigen delivery system consisting of non-living, non-genetically modified cell wall particles derived from Lactococcus lactis. These particles, referred to as Gram-positive Enhancer Matrix (GEM) particles, are produced by the heat-acid treatment of freshly grown L. lactis, a process that removes the DNA and most of the bacterial proteins, but leaves the peptidoglycan (PGN) envelope intact8,9. Multiple antigens can be displayed on the particle surface using recombinant protein and affinity technology: recombinant fusion proteins containing a vaccine antigen and a PGN protein anchor domain that binds with high affinity to the bacterial PGN, are produced in a suitable host-cell, purified, and then combined with naked GEM particles. The recombinant proteins bind tightly to the GEMs, creating antigen-displaying particles. A major advantage of the GEM particles for neonatal immunization is their safety profile. L. lactis is a non-pathogenic Gram-positive, lactic acid bacterium, generally recognized as safe (GRAS) and widely used in dairy products. Probiotics have been safely given to newborns10, young children in day-care11 and even critically ill children12. Unlike recombinant live organisms, including attenuated pathogens, the L. lactis GEM particles do not contain DNA, i.e. there is no risk of potential reversion to a virulent form. The composition of the GEMs also contributes to their immune-stimulating properties. As spherical particles, the GEMs can be efficiently taken up by M cells in the epithelium above the mucosal lymphoid follicles, and the transported antigens can be delivered directly to underlying DC in mucosal inductive sites. Furthermore, the PGN envelope is a potent stimulator of innate immunity13.
We used Yersinia pestis LcrV as a model vaccine antigen to demonstrate the feasibility of successful early life immunization using the GEM platform technology. The immunogenicity and protective efficacy of L. lactis GEM particles displaying Y. pestis LcrV was investigated in a neonatal mouse model. We showed, for the first time, that intranasal immunization of newborn mice with GEM-LcrV elicits a potent mucosal and systemic immunity that protects against lethal systemic plague infection. We also demonstrated that the L. lactis GEM particles enhance the maturation of neonatal CD11c+ DC, and that these cells have increased capacity for secretion of pro-inflammatory and Th1-type promoting cytokines and can stimulate antigen-specific IFN-γ-secreting CD4+ T cells. Furthermore, we showed that the GEM particles were taken up by DC from human newborns and that these cells also acquired a mature phenotype such that they were able to stimulate human T cells. Together, these results indicate that mucosally delivered antigen-displaying L. lactis GEM particles represent a highly promising vaccine approach for immunization early in life.
RESULTS
L. lactis GEM particles induced maturation of neonatal and adult mouse DC
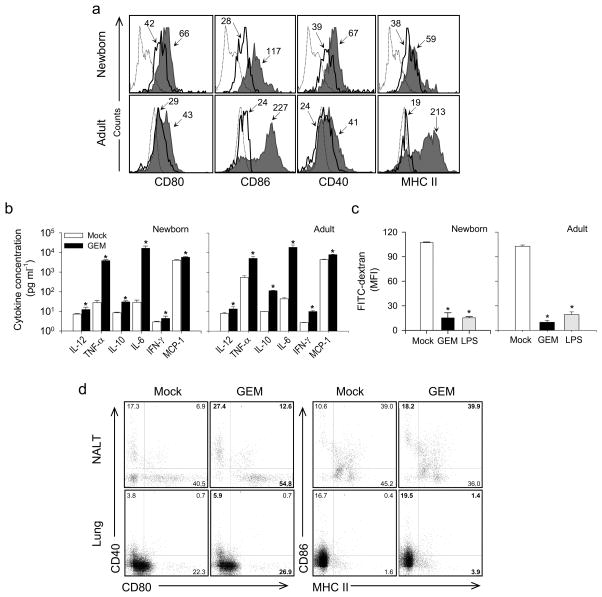
To ascertain whether the L. lactis GEM particles could provide strong immunological signals to stimulate the neonatal immune system, we first examined the ability of the GEM particles to activate and enhance the functional capacity of neonatal DC. The expression of activation and maturation cell surface markers CD80, CD86, CD40 and MHC-class II (I-Ad) was measured on bone marrow (BM)-derived CD11c+ cells from newborn (7-day-old) mice stimulated with L. lactis GEM particles or mock-stimulated (Figure 1a). To determine the strength of the activation of GEM-stimulated neonatal DC in comparison with that of adult DC, BM-derived CD11c+ cells from 6–8 week-old mice were included in all experiments. All markers were upregulated in neonatal and adult DC after GEM stimulation, compared with the mock-treated DC (Figure 1a). Neonatal GEM-exposed DC exhibited a noticeable increase in the expression of CD86, while both CD86 and MHC-II were the markers most abundantly expressed on adult GEM-stimulated DC. A summary of the increases in the expression of cell surface markers in both neonatal and adult DC exposed to the L. lactis GEMs or to E. coli LPS (used as positive control) is shown in Table 1. It is noted that the upregulation of MHC-II and costimulatory molecules in both neonatal and adult GEM-stimulated DC was remarkably similar to that induced by LPS under the same experimental conditions.
Figure 1.
L. lactis GEM particles enhanced maturation and cytokine production of neonatal and adult mouse DC. (a) Expression of activation and maturation cell surface markers CD80, CD86, CD40 and MHC class II on neonatal and adult mouse BM-derived CD11c+ DC treated with GEM particles (shaded area) or mock-treated (solid line); the dashed line indicates isotype control staining. The mean fluorescence intensity (MFI) on CD11c+ gated cells is indicated. (b) Cytokines produced by neonatal and adult mouse BM-derived CD11c+ DC stimulated with GEM particles or mock-stimulated, measured in culture supernatants. Data is representative of three independent experiments. (c) FITC-dextran uptake by neonatal and adult CD11c+ DC exposed to GEM or E. coli LPS (positive control), or mock-treated DC, measured by flow cytometry; data represents MFI±s.d. from three independent experiments. Significant differences (P<0.001) compared with mock-stimulated cells are denoted by an asterisk (*). (d) Activation and maturation of neonatal DC exposed to GEM particles in vivo. Mice were immunized with GEMs or PBS (mock) on day 7 after birth and NALT and lungs were harvested on day 15. The number in each quadrant indicates the percentage of CD11c+ DC expressing activation and maturation cell surface markers CD40, CD80, CD86 and MHC class II. GEM, L. lactis Gram-positive Enhancer Matrix; BM, bone marrow; DC, dendritic cell; LPS, E. coli lipopolysaccharide; NALT, nasal associated lymphoid tissue.
Table 1.
Summary of fold-increases in the expression of surface markers and in cytokine production by human and mouse CD11c+ DC stimulated with L. lactis GEM, E. coli LPS (mDC) or TNF-α (hDC) as compared with mock-treated DC.
| Mouse CD11c+DC |
Human CD11c+DC |
|||||||
|---|---|---|---|---|---|---|---|---|
| GEM |
LPS |
GEM |
TNF-α |
|||||
| Neonatal | Adult | Neonatal | Adult | Neonatal | Adult | Neonatal | Adult | |
| Surface markers | ||||||||
| CD40a or CD83b | 1.0 | 1.3 | 1.0 | 1.3 | 2.2 | 3.6 | 2.9 | 3.0 |
| CD80 | 1.2 | 1.1 | 1.4 | 1.8 | 2.2 | 2.5 | 2.7 | 1.8 |
| CD86 | 4.0 | 7.2 | 4.2 | 6.1 | 5.1. | 6.9 | 4.8 | 5.1 |
| I-Ada or HLA-DRb | 1.1 | 8.9 | 0.9 | 7.2 | 1.4 | 3.1 | 1.4 | 3.2 |
| Cytokines | ||||||||
| IL-12p70 | 1.7 | 1.7 | 2.1 | 1.6 | 2.3 | 1.6 | 1.5 | 2.0 |
| TNF-α | 140.1 | 9.4 | 93.4 | 10.8 | 163.0 | 541.8 | 24.4 | 1,119.7 |
| IL-10 | 3.6 | 11.4 | 3.6 | 20.3 | 4.1 | 47.6 | 16.3 | 2.1 |
| IL-6 | 565.5 | 421.3 | 707.9 | 428.6 | 164.7 | 329.1 | 1,108.3 | 1.6 |
| IFN-γa or IL-1βb | 1.5 | 3.7 | 1.9 | 7.3 | 1.7 | 3.1 | 2.3 | 2.0 |
| MCP-1a or IL-8b | 1.4 | 1.7 | 2.9 | 1.7 | 58.9 | 13.4 | 125.5 | 2.6 |
one fold increase represents a response that is twice as high as the response of mock-treated cells.
Mouse only
Human only
DC stimulated with L. lactis GEMs secreted pro-inflammatory cytokines
To assess the functional capacity of the GEM-activated DC, we examined their ability to secrete pro-inflammatory, Th1-promoting and regulatory cytokines, as these are all critical signals required for the development of an effective adaptive immune response. The levels of IL-12p70, TNF-α, IL-10, IL-6, IFN-γ and MCP-1 were measured in culture supernatants from neonatal and adult BM-derived CD11c+ cells treated with L. lactis GEMs or LPS, or from mock-treated cells. For all of the cytokines tested, both neonatal and adult GEM-stimulated DC had an increased capacity for cytokine production as compared with mock-treated cells (Figure 1b). The levels of cytokines produced by both adult and neonatal mouse DC stimulated with the L. lactis GEM particles were comparable, suggesting that neonatal GEM-activated DC can reach a degree of functional activity similar to that of adult mature DC. Interestingly, the fold-increases for TNF-α and IL-6 were much higher in DC from the newborns regardless of whether they were stimulated with the GEMs or LPS (Table 1).
GEM-exposed mature DC had reduced capacity for antigen uptake
During the process of maturation, DC relent their endocytic and phagocytic activity as they become more efficient antigen-presenting cells14. Accordingly, we examined the capacity of GEM-stimulated DC to incorporate FITC-dextran as a measure of antigen uptake. Both neonatal and adult CD11c+ DC exposed to the GEM particles had a markedly lower capacity to incorporate FITC-dextran (Figure 1c). Compared with mock-stimulated DC, the adult and neonatal DC showed 85% and 90% reduction in FITC-dextran incorporation, respectively, further attesting to their mature phenotype.
In vivo activation of mucosal neonatal mouse DC by the GEM particles
To confirm that the in vitro process of neonatal DC maturation mediated by the GEM particles also occurs in vivo, we examined the phenotype of CD11c+ DC in the nasal-associated lymphoid tissue (NALT) and the lungs of 15-day-old mice that had been immunized with the L. lactis GEM particles at 7 days of age. Figure 1d shows the expression of CD40, CD80, CD86 and MHC-class II on CD11c+ cells. As observed in vitro, DC from newborn mice exposed in vivo to the GEM particles also exhibited a more activated and mature phenotype as compared with the naïve (mock-exposed) controls. A remarkable increase in the number of CD11c+ cells expressing both CD40 and CD80 was seen in the NALT. A more pronounced level of activation was observed in this tissue as compared with the lungs, consistent with the proximity of the nasal tissue to the site of inoculation.
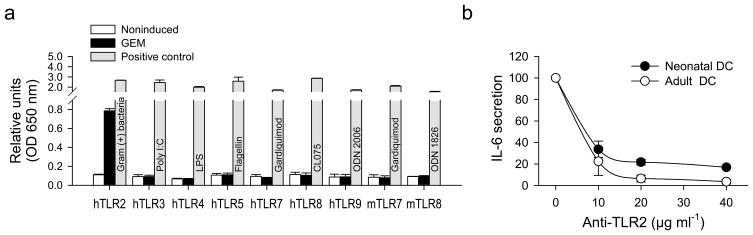
GEM particles activated neonatal and adult DC through TLR2
We hypothesized that the recognition of GEM particles by DC and their subsequent activation was mediated through toll-like receptor (TLR) signaling. Thus, we investigated the capacity of the GEMs to bind a panel of human and mouse TLRs expressed in HEK293 cells. NF-κB activity was measured and used as a readout for activation. The GEM particles interacted with human TLR2 but not with any of the other TLRs tested, (human TLR3, TLR4, TLR5, TLR7, TLR8 and TLR9, and mouse TLR7 and TLR8; Figure 2a). The capacity of the GEM particles to signal through TLR2 expressed on neonatal and adult mouse DC was confirmed by antibody inhibition. In this assay, the production IL-6, detected in culture supernatants, were used as a measure of TLR2 activation. CD11c+ DC pre-incubated with increasing amounts of TLR2-specific antibodies and subsequently stimulated with the GEM particles produced significantly lower levels of IL-6 than untreated DC (or DC incubated with isotype control). The level of IL-6 produced decreased in a dose-dependent manner, further confirming the specificity of the antibody blockage and the TLR2 involvement (Figure 2b).
Figure 2.
L. lactis GEM particles activate neonatal and adult mouse DC and evoke IL-6 production through TLR2 activation. (a) GEM interaction with human (h) and mouse (m) TLRs individually expressed on HEK93 cells, as measured by NF-κB activation using a phosphatase alkaline reporter gene. Data represents relative units for OD 650 nm±s.d. from duplicate screening experiments. (b) Inhibition of IL-6 production by GEM-stimulated neonatal and adult mouse CD11c+ DC in the presence of TLR2-blocking monoclonal antibody. TLR2 inhibition curve shows relative cytokine levels (expressed as a percentage of the max. IL-6 production by GEM-stimulated DC in the absence of TLR blocking) measured by ELISA in culture supernatants; data are representative of two independent experiments. GEM, Gram-positive Enhancer Matrix; TLR, toll like receptor; ELISA, enzyme-linked immunosorbent assay; DC, dendritic cell.
Enhancement of neonatal antigen presentation and stimulation of antigen-specific T cells
We used the Y. pestis LcrV as a model antigen to test the ability of the L. lactis GEMs to prime an immune response in the neonatal setting. LcrV-based vaccines have been shown to induce complete protection against Y. pestis challenge in animal models [Reviewed in15]. However, none of these vaccines has been tested for tolerability and efficacy in young hosts. We therefore undertook the study of the GEM-LcrV system as a plague vaccine candidate for neonatal and infant immunization. LcrV-PGN binding domain fusions were produced in a recombinant L. lactis and attached externally to the GEM particles, as described in Figure 3.
Figure 3.
Schematic representation illustrating the preparation of L. lactis GEM particles displaying Y. pestis LcrV. (a) GEM particles are obtained by heat-acid treatment of L. lactis followed by extensive washing. The resulting bacterial “shell” (GEM) particles have an appearance and dimensions similar to those of the living organism. L. lactis contains an extracellular cell-wall degrading enzyme (hydrolase AcmA), which in its natural form allows separation of daughter cells by cleaving the PGN wall during bacterial division. This enzyme is naturally exported and attaches (from the outside) to the bacterial cell wall though a C-terminal binding domain that has high affinity for the L. lactis PGN. The use of this PGN binding domain allows for a strong non-covalent binding of the fusion proteins to GEM particles. (b) The AcmA locus, containing the enzyme active site next to the PGN binding domain and preceded by a signal peptide (SP), was cloned into an expression plasmid (pPA3). LcrV was inserted in lieu of the AcmA active site on pPA3 so that the LcrV sequence is in tandem with the PGN binding domain. The resulting plasmid, pPA281, was introduced into live L. lactis, which then produced the LcrV-PGN binding domain fusion as a recombinant protein and released it into the culture medium. The producer cells were removed by centrifugation, and the antigen was concentrated and used for particle coating (no additional purification is needed). (c) GEM particles and LcrV-PGN binding domain fusion protein were mixed, resulting in immediate non-covalent binding of LcrV to the PGN layer. (d) Fluorescence microscopy showing GEM particles displaying LcrV using an LcrV-specific monoclonal antibody; no staining was observed with GEM alone (shown on a light microscopy image). GEM, Gram-positive Enhancer Matrix; PGN, peptidoglycan; PA, PGN protein anchor domain.
We first examined in vitro the capacity of neonatal DC exposed to LcrV-carrying GEM particles to process the vaccine antigen and present it to T cells. To this end, neonatal CD11c+ DC pre-treated with GEM-LcrV or LcrV, or mock-treated DC, were incubated with LcrV- specific CD4+ and CD8+ T cells. Lymphocyte proliferation and the frequency of IFN-γ secreting CD4+ T cells were measured as readouts of T cell activation (Figure 4a and b). Both CD4+ and CD8+ T lymphocytes showed remarkable proliferative responses when stimulated with neonatal DC previously exposed to GEM-LcrV. These responses largely surpassed those of T cells stimulated with LcrV- or mock-treated DC. The frequency of LcrV-specific IFN-γ-secreting CD4+ T cells also rose sharply and in a dose-dependent manner when T cells were stimulated with DC treated with GEM-LcrV, as opposed to stimulation with LcrV- or mock-treated DC, both of which failed to induce a significant IFN-γ response (Figure 4b).
Figure 4.
L. lactis GEM-LcrV enhanced antigen presentation by neonatal mouse DC and stimulation of LcrV-specific T cells. (a) Stimulation of LcrV-specific CD4+ and CD8+ T cells by CD11c+ neonatal DC previously exposed to GEM-LcrV or LcrV, or mock-treated DC (DC:T cell ratio 1:2). Cell proliferation was measured by [3H] thymidine incorporation; data represent mean stimulation index±s.e.m. from replicate cultures. (b) Frequency of IFN-γ secreting CD4+ T cells stimulated with GEM-LcrV-, LcrV- or mock-treated CD11c+ neonatal DC (at increasing DC:T cell ratios) measured by ELISPOT. Data show mean IFN-γ spot forming cells (SFC)±s.e.m. from replicate cultures. Significant differences compared with the mock-treated (*P<0.002) and LcrV-treated-DC (**P<0.01) are indicated. GEM, Gram-positive Enhancer Matrix; ELISPOT, enzyme linked immunospot assay; IFN, interferon; DC, dendritic cell.
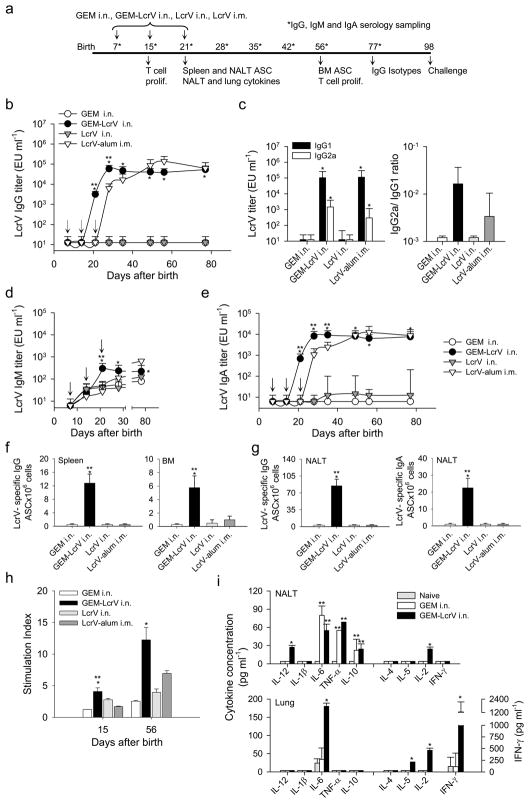
Immunization with GEM-LcrV elicited potent mucosal and systemic immunity early in life
We next evaluated the immunogenicity and protective efficacy of the GEM-LcrV particles in vivo. Newborn mice were immunized intranasally (i.n.) on days 7, 15 and 21 after birth, with GEM-LcrV, recombinant LcrV or GEM alone (Figure 5a). A group immunized intramuscularly (i.m.) with recombinant LcrV adsorbed to alum was included as control. The GEM-LcrV particles elicited high levels of LcrV-specific serum IgG antibodies that were first detected on day 21 after birth; 80% of the animals seroconverted at this time. The IgG levels increased on day 28 after birth, one week after the last immunization, and remained increased up to day 77, the last time point tested (Figure 5b). In contrast, no responses were detected in mice immunized i.n. with GEMs or LcrV alone. The control group immunized i.m. with LcrV-alum developed IgG responses, but they peaked on day 56 after birth (5 weeks after the last immunization) and started to decrease soon after (IgG mean titers on day 56 and 77 were 137,708.1 and 62,262.9 EU ml−1, respectively). Both IgG1 and IgG2a were produced in mice that received GEM-LcrV or LcrV-alum (Figure 5c). However, the proportion of IgG2a was larger in the GEM-LcrV group, resulting in a higher IgG2a/IgG1 ratio, as compared with group that received LcrV-alum (Figure 5c).
Figure 5.
Intranasal immunization of newborn mice with L. lactis GEM-LcrV elicited potent systemic and mucosal immune responses. (a) Timeline for immunization and analysis of immune responses. Newborn mice (1-week-old, n=21 pups per group) were immunized i.n. with GEM-LcrV (carrying ~12 μg of LcrV), GEMs alone or recombinant LcrV (20 μg) on days 7, 15 and 21 after birth (arrows). A positive control group received 2 μg of LcrV-alum i.m. (b) Kinetics of LcrV-specific serum IgG levels. (c) IgG subclass distribution (IgG1 and IgG2a titers) and IgG2a/IgG1 ratio. (d) Kinetics of LcrV-specific IgM and (e) IgA production. (b–e) Data represent median titers and ratios±one quartile. (f) LcrV-specific IgG ASC in the spleen and BM measured on days 21 and 56 after birth, respectively. (g) IgG and IgA ASC measured in the NALT 21 days after birth. Results shown are the mean ASC frequency per 1×106 cells±s.e.m. of replicate wells. (h) Proliferation of LcrV-specific T cells measured by [3H] thymidine incorporation. Results are expressed as stimulation index±s.e.m. from replicate wells. (b–h) Significant differences compared with newborn mice that received GEM alone (*P <0.002) or LcrV-alum i.m. (**P<0.01) are indicated. (i) Cytokine profile in the NALT and lungs measured on day 21 after birth. Cells were restimulated in vitro with LcrV. Data represent mean cytokine levels±s.d. from triplicate cultures. Significant differences compared with GEMs alone (*P<0.001) and naïve mice (**P<0.005) are indicated. GEM, Gram-positive Enhancer Matrix; ASC, antibody secreting cell; BM, bone marrow; NALT, nasal associated lymphoid tissue.
Increased levels of LcrV-specific IgM were observed in mice immunized with GEM-LcrV on day 21 after birth, which exceeded those of all the other groups (Figure 5d). Immunization with GEM-LcrV also produced high LcrV-specific serum IgA responses that were first seen on day 21; these IgA levels peaked on day 28 and remained steady thereafter (Figure 5e). The similarity between the kinetics of IgG and IgA production is noteworthy, with both curves showing faster responses following immunization with GEM-LcrV over LcrV-alum (Figure 5b and e).
We also examined the presence of LcrV-specific antibody secreting cells (ASC) in the spleen and BM, which are believed to represent reservoirs of vaccine-induced plasma cells that support the production and maintenance of circulating antibodies. Significant IgG LcrV ASC responses were found in mice immunized with GEM-LcrV but not in mice immunized with LcrV or GEMs alone. The positive control group immunized with LcrV-alum also lacked IgG LcrV ASC responses (Figure 5f).
The induction of mucosal immunity was assessed by measuring the frequency of IgA and IgG ASC in the NALT (Figure 5g). Mice immunized i.n. with GEM-LcrV exhibited high numbers of IgA and IgG ASC on day 21 after birth, coinciding with the appearance of serum antibodies. IgG ASC were also found in the lungs 21 days after birth, albeit at a much lower frequency (data not shown). No mucosal ASC responses were ever detected in any of the other groups.
We also investigated the induction of cell-mediated immunity by measuring the proliferative responses of LcrV-specific T cells in the spleen at different time points. Newborn mice immunized with GEM-LcrV exhibited a significant T cell response on day 15 after birth, and this response further increased on day 56; in contrast, responses were negligible in mice immunized i.n. with GEMs or LcrV alone (Figure 5h). Mice that received LcrV-alum had a positive response on day 56, albeit at a significantly lower level compared to those of mice that received GEM-LcrV.
Finally, we examined the cytokine profile induced in response to GEM-LcrV immunization, in the NALT and lungs as critical mucosal lymphoid tissues. These measurements were performed 21 days after birth, ~ one week after the second immunization. Th1, Th2, pro-inflammatory and T regulatory cytokines were measured in the culture supernatants of cells stimulated in vitro with LcrV or mock-stimulated cells. We included in this experiment only the most relevant groups: newborn mice immunized i.n. with GEM-LcrV or GEMs alone, and mock-immunized (naïve controls). Increased levels of IL-2 and IL-12 (p40 and p70) were observed in the NALT of newborns immunized with GEM-LcrV but not in those that received GEMs alone (Figure 5i). IL-6, TNF-αand IL-10 were also increased, but this increase occurred in both groups (GEMs and GEM-LcrV), suggesting a broad and non-specific stimulation of neonatal immune cells induced by the GEMs alone. This non-specific stimulation was not seen in naïve mice. Lung cells from newborn mice immunized with GEM-LcrV produced remarkably high levels of IFN-γ and exhibited increased production of IL-2 and IL-6 upon in vitro antigen stimulation, none of which was seen in mice immunized with GEMs alone or in naïve controls. Marginal levels of IL-5 were found in the lungs of GEM-LcrV immunized mice, whereas IL-4 was negligible in both tissues; IL-5 and IL-4 were undetectable in mice that received GEMs alone or in naïve controls.
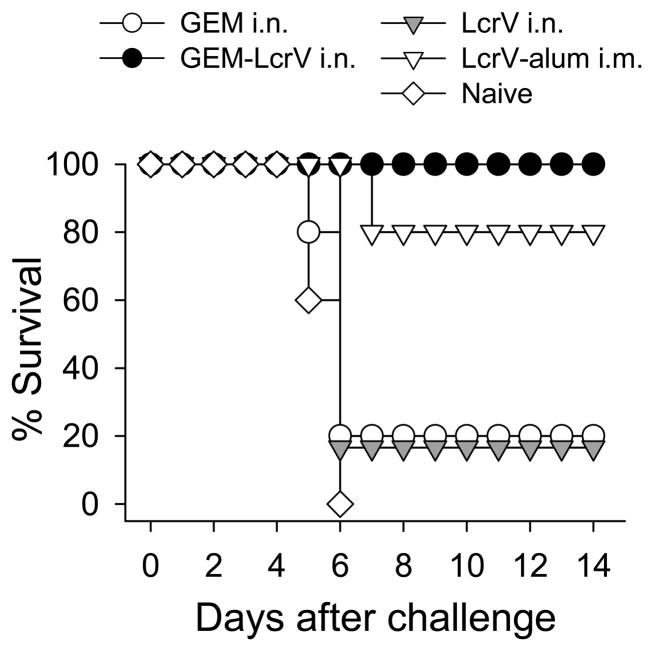
GEM-LcrV protected newborn mice against systemic lethal plague
Mice immunized as newborns with GEM-LcrV, LcrV and GEMs alone, along with naïve controls, were challenged intravenously with ~30 lethal doses of Y. pestis EV76, 8 weeks after the last immunization (Figure 6). The attack rate in naïve mice was 100%. These animals showed significant weight loss and severe disease, and all died by day 6 after challenge. In contrast, all mice immunized with GEM-LcrV were protected. Some of these animals exhibited minimal weight variations and mild signs of disease during the first week after challenge, but completely recovered thereafter. Only 20% of the animals immunized i.n. with LcrV or GEMs alone survived after challenge; mice in these groups showed significant weight loss and signs of disease. Among those immunized i.m. with LcrV-alum, 80% were protected. These animals showed moderate signs of disease during the first week but recovered thereafter.
Figure 6.
Protection against systemic lethal plague infection. Newborn mice (n=5–6 pups per group) were immunized as described above. Eight weeks after the last immunization they were challenged i.v. with Y. pestis EV76 (~30 MLD50) in the presence of FeCl2. Data show percent survival during the monitoring period. GEM, Gram-positive Enhancer Matrix.
Human DC stimulated with GEM particles exhibited an activated and mature phenotype
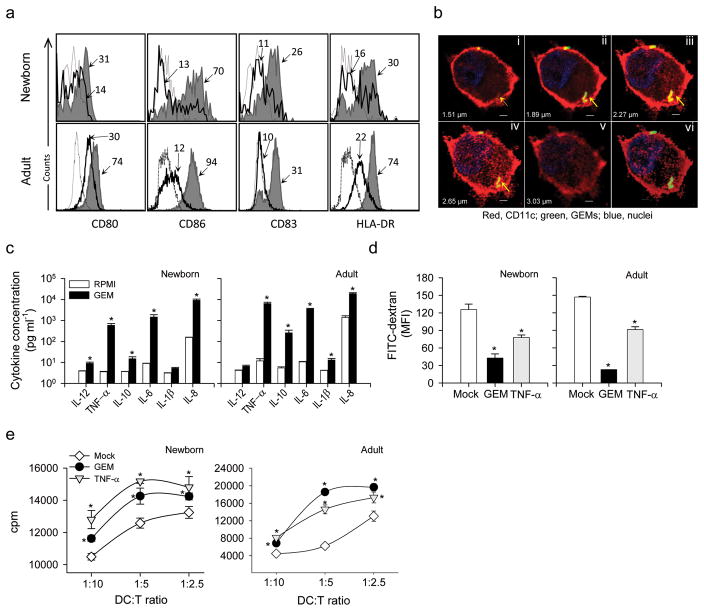
To further evaluate the potential of the L. lactis GEM particles as a vaccine platform for human newborns, we investigated whether the immune stimulatory properties observed in mice also extended to human neonatal DC. Human newborn DC derived from CD34+ precursors from umbilical cord blood were stimulated with GEM particles or were mock-treated. DC derived from peripheral mononuclear cells from adult human subjects were tested in parallel to compare the degree of activation of neonatal vs. adult DC. In both cases, stimulation with TNF-α was included as a positive control. The expression of activation and maturation markers on CD11c+ DC was measured by flow cytometry. GEM-stimulated neonatal and adult human DC upregulated expression of MHC-II (HLA-DR) and costimulatory molecules CD80, CD86 and CD83 (Figure 7a). Consistent with the results obtained in mice, CD86 exhibited the highest increase in neonatal DC, whereas both CD86 and HLA-DR were the most increased in adult cells (Table 1). The ability of human newborn CD11c+ DC to phagocytose the GEM particles was demonstrated by confocal laser microscopy (Figure 7b). A cluster of FITC-stained GEM particles can be seen in the DC cytoplasm, and the abundant red surface staining indicates CD11c expression.
Figure 7.
GEM particles enhanced the maturation of neonatal and adult human DC and the stimulation of T cells in a MLR. (a) Expression of cell surface markers CD80, CD86, CD83 and HLA-DR on human CD11c+ neonatal and adult DC stimulated with GEM particles (shaded area) or mock- treated (solid line); the dashed line indicates the isotype control. The MFI on CD11c+ gated cells is indicated. (b) Individual (i–v) and Z-stack projection (vi) confocal laser microscopy images showing CD11c+ DC from human newborns harboring FITC-labeled GEM particles (arrows). CD11c+ cell-surface expression is shown in red, and nuclei are shown by blue fluorescent staining. Scale bars, 2 μm. (c) Cytokines produced by human neonatal CD34+- and adult derived DC stimulated with GEM particles or mock-stimulated and measured in culture supernatants. Data represent mean cytokine concentration±s.e.m. from two independent experiments. (d) FITC-dextran uptake by neonatal CD11c+ and adult human DC exposed to GEM or TNF-α (positive control), or mock-treated DC, measured by flow cytometry; data represents MFI±s.e.m. from three independent experiments. (e) Allogeneic stimulation of adult CD3+ T cells in the presence of neonatal and adult human DC stimulated with GEM particles or TNF-α, or mock-stimulated DC. Data show mean cpm±s.e.m. from one of two independent experiments. (c–e) Significant differences (*P<0.05) compared with mock-stimulated cells. GEM, Gram-positive Enhancer Matrix; MLR, mixed lymphocyte reaction, DC, dendritic cell; TNF, tumor necrosis factor; MFI, mean fluorescence intensity; HLA, human histocompatibility leukocyte antigen.
Human DC matured by GEM particles had decreased phagocytic activity and enhanced capacity for cytokine secretion and T cell activation
The functional capacity of GEM-stimulated neonatal and adult human CD11c+ DC was assessed by measuring the levels of Th1-promoting, pro-inflammatory and T regulatory cytokines in culture supernatant of cells treated with GEMs or TNF-α (positive control), or mock-treated cells. Increased levels of TNF-α, IL-10, IL-6 and IL-8 were produced by both neonatal and adult human DC. Production of IL-12p70 was also elevated in neonatal DC, and production of IL-1β was elevated in adult DC (Figure 7c). Consistent with their activated and mature phenotype, human neonatal and adult DC stimulated with GEM particles exhibited reduced phagocytic activity, as evidenced by lower levels of FITC-dextran uptake compared with mock-treated DC (Figure 7d).
Finally, we examined the capacity of the GEM-activated human neonatal and adult DC to stimulate CD3+ T cells in a mixed lymphocyte reaction (Figure 7e). TNF-α- and mock treated-DC were included as controls. Mature DC expressing high levels of MHC-II molecules, as opposed to immature DC, are expected to activate allogeneic T cells. Indeed, proliferative responses were higher when T cells were stimulated with GEM-activated DC compared with mock-treated DC. T cell activation followed a dose-response pattern, with proliferation levels increasing in the presence of higher DC:T cell ratios.
DISCUSSION
In this study, we demonstrated the usefulness of non-living and non-genetically modified L. lactis antigen-displaying particles for early life immunization. We show, for the first time, that intranasal immunization of newborn mice with L. lactis GEMs displaying Y. pestis LcrV is well tolerated and elicits a potent mucosal and systemic immunity that protects against lethal plague infection.
The GEM particles accomplished one of the most desired tasks for a neonatal vaccine: they effectively targeted a vaccine antigen into neonatal DC, and activated and enhanced the maturation of these cells in such a manner that they became proficient antigen presenting cells capable of stimulating antigen-specific Th1-type effector cells. Both neonatal mouse and human DC were powerfully activated and acquired a mature phenotype when exposed to the GEMs. Neonatal DC from mucosal lymphoid tissues also acquired a mature phenotype when stimulated by the GEM particles in vivo.
Newborn mice immunized intranasally with GEMs displaying Y. pestis LcrV induced high levels of LcrV-specific serum antibodies, systemic and mucosal IgG and IgA ASC and robust T cell responses. LcrV was remarkably immunogenic when carried by the GEM particles but not when given alone, which is probably the result of higher efficiency of key processes, including activation of innate immunity through interaction with TLR2, DC uptake and direct stimulation of B cells. A pro-inflammatory cytokine milieu with elevated levels of IL-6 and TNF-α, indicative of a general immune stimulation, was found in the NALT of newborns immunized with the GEMs. IL-10 was also produced, most likely to counter-balance such broad immune activation. The excellent tolerability of the vaccine also indicates that a finely tuned mechanism of immune balance indeed takes place.
Neonatal mucosal immunization with GEM-LcrV also surpassed parenteral immunization with LcrV-alum in 1) the swiftness to reach peak antibody level, 2) the steadiness of the antibody response, 3) the capacity to induce mucosal and systemic ASC and 4) the ability to prime systemic effector T cells early in life. The induction of potent immune responses in the respiratory mucosa is particularly important, as this is the portal of entry for many of the pathogens that cause severe disease in early childhood. Such a response can block infection locally, preventing systemic dissemination of the pathogen. Earlier studies have shown mucosal and systemic responses in adult mice immunized i.n. with GEM particles displaying pneumococcal antigens16 and significant protection against lethal respiratory pneumococcal challenge17. The capacity of the GEM-LcrV particles to induce high levels of antigen-specific IFN-γ and IL-2 in the lungs is a remarkable finding considering the importance of Th1-type responses in the protection of young hosts against intracellular pathogens and the difficulty of inducing such effector responses early in life, especially in a mucosal tissue. Most importantly for its use as a prophylactic vaccine, intranasal immunization with GEM-LcrV conferred the highest level of protection against lethal Y. pestis infection in neonatally immunized mice. The capacity of the GEMs to activate non-specific immune defenses, can explain the 20% survival in mice that received particles alone, as opposed to complete lethality in the naïve group. This effect is most likely due the PGN (exposed on the particle surface), which has been shown to stimulate not only innate immune cells but also T cells, including those of neonatal origin, through interaction with TRL218–20. Despite this broad immune activation, the protection conferred by the GEM-LcrV was clearly antigen-specific.
Y. pestis causes a severe and often fatal disease in humans for which no licensed vaccine is available15. The pulmonary form (pneumonic plague) is particularly virulent as it quickly spreads from person to person via aerosol droplets21. Y. pestis has drawn considerable attention lately as a potential biological weapon, and biowarfare concerns have revived efforts toward the development of new vaccines candidates. These endeavors, however, have been focused almost exclusively on vaccines for adults, and these vaccines are unlikely to meet the needs of other (more vulnerable) segments of the population, such as children. A L. lactis GEM-based plague vaccine for pediatric use would represent a unique tool in the biodefense armamentarium. If needed, the GEM-LcrV platform could be further improved by displaying additional Y. pestis antigens such as F1 or Yersinia outer proteins (Yops). A GEM-based plague vaccine would be ideal for early life, surpassing the leading alum-adjuvanted F1-V vaccine in the quality and strength of the responses and surpassing live attenuated vaccine strains with regards to safety.
Recombinant lactic acid bacteria, including L. lactis strains, expressing heterologous antigens have been sought as mucosal vaccines and could potentially be used in children22–25. Major concerns associated with the use of these organisms include the possibility of causing disease by establishing niches within the commensal flora and the introduction of exogenous DNA, especially plasmids that confer antibiotic resistance. The GEM particles alleviate these concerns because they are non-living and non-genetically modified. They also have many other advantages over live recombinant vectors that increase their appeal for infant immunization: 1) the amount of antigen displayed and delivered in vivo is known and remains constant, unlike antigen expression in living recombinant organisms, which can be affected by plasmid loss, metabolic burden and promoter activation; 2) the antigen is always exposed on the particle surface at a high density and in a multimeric form, facilitating the activation of B cells; 3) multiple antigens can be displayed simultaneously, a feature that has not yet been achieved using live probiotics, and 4) the GEMs are highly stable and can be stored at room temperature, avoiding the need of cold chain.
The GEMs have additional properties that make them suitable for large-scale vaccination in field settings: their production is simple and inexpensive, and they are easy to preserve and to administer. A recent structural analysis of GEM-LcrV particles showed that the attachment of the LcrV-PGN binding domain fusion proteins to the particle surface is indeed strong, stable, specific (proteins without the PGN anchor domain do not bind to the particles), and abundant (multiple antigen clusters are loaded onto the surface)26. It is also pH specific: LcrV binds to the particles under physiological conditions (pH 7.2) but detaches when exposed to an acidic environment (pH 4.4), facilitating its release within the phagolysosomes for processing and presentation26.
The L. lactis GEMs were administered i.n. to newborn mice with the rationale that being inert particles, L. lactis GEMs could also conceivably be given to human infants by the nasal route, thus departing from the traditional orogastric delivery of live probiotics. There are also many advantages associated with intranasal immunization. Vaccine antigens administered by this route are less likely to be blocked by maternal antibodies27,28. Intranasal vaccination is not affected by physiological intestinal barriers, including the resident flora, which may prevent access of vaccine antigens to immunological inductive sites. Nor does intranasal vaccination disturb the gastrointestinal microbial environment, which plays an important role in the process of neonatal immune development29. Furthermore, a nasally delivered vaccine would encounter a higher frequency of “immunogenic” as opposed to “tolerogenic” DC, which more prevalent in the gut.
A handful of studies have examined the ability of L. lactis to activate mouse and human DC in vitro17,23,30–33. These studies described the phenotype of the activated cells but, for the most part, did not examine their capacity for immunological priming. We demonstrated the ability of “mature” GEM-stimulated neonatal DC to present a vaccine antigen and to stimulate Th1-type effectors cells in a neonatal setting. Our results agree with those of Niers et al., who showed in vitro that naïve neonatal human T cells can be skewed towards a Th1-type response upon exposure to L. lactis-primed DC32.
This is the first report seeking the use of probiotic antigen-displaying particles to “jump-start” the neonatal immune system for the purpose of early life immunization. Also unique to our studies is the comparison of vaccine-activated neonatal and adult DC from both mice and humans, demonstrating in both cases that the GEM particles can induce neonatal DC activation levels comparable to those achieved by adult DC.
In summary, we demonstrated that L. lactis GEM particles have the inherent capacity to activate the neonatal immune system and that they provide a well tolerated, effective and practical vaccine platform for early life immunization, overcoming the limitations of conventional vaccines. These results show the exceptional potential of GEM-based vaccines and warrant future studies of such vaccines in humans.
METHODS
Generation of neonatal and adult DC
Dendritic cells were isolated from the BM of newborn (7-day-old) and adult (6 to 8-week-old) BALB/c mice as previously described34. One-week-old newborn mice were used in all experiments as their state of immune maturation is considered equivalent to that of human neonates1. Cells were cultured in RPMI 1640 containing 2 mM L-glutamine, 10 mM HEPES (Gibco-Invitrogen, Grand Island NY), 0.1 mM 2-mercaptoethanol (Sigma-Aldrich, St. Louis MO), 50 μg ml−1 gentamicin and 10% FBS (HyClone, Logan, UT) (cRPMI) for 7 days in the presence of GM-CSF and IL-4 (10 ng ml−1) (PeproTech, Rocky Hill, NJ) at 37°C, 5% CO2. CD11c+ DC were further purified by negative magnetic cell sorting (BD Pharmingen, San Jose, CA); purity ranged between 80 and 95%. Human cord blood was obtained from the placentas of normal, full-term deliveries at the University of Maryland Medical Center. DC were generated from magnetically sorted CD34+ progenitors (Miltenyi Biotec, Auburn, CA). Adult peripheral blood samples were obtained from healthy volunteers, and mononuclear cells were isolated by density gradient centrifugation with Lymphocyte Separation Medium (LSM®, MP Biomedicals, Ontario, Canada). Cells were allowed to adhere during 3 h at 37°C, 5% CO2. Adult adherent and magnetically sorted cord-blood CD34+ cells were cultured for 7 days in cRPMI with 50 ng ml−1 of human GM-CSF and 10 ng ml−1 of IL-4 (Peprotech). Blood collection was approved by the University of Maryland Institutional Review Board.
DC stimulation and flow cytometry
CD11c+ DC from adult and newborn mice were cultured for 24 h in the presence of GEM particles (1:150 DC:GEM), E. coli LPS (5 ng ml−1, Sigma-Aldrich, St. Louis, MO) as positive control or cRPMI (mock-treated). Following incubation, the cells were washed and stained with FITC-, PE- or allophycocyanin-labeled monoclonal antibodies (mAbs) specific for CD40, CD80, MHC II, CD86 and CD11c in PBA (PBS containing 0.1% BSA and 0.01% NaN3)34. Fc-Block (anti-mouse CD16/32) was used to reduce background staining. In studies of in vivo DC activation, mononuclear cells from nasal and lung tissues were collected from 15 days-old mice that had been immunized with GEM particles (or mock immunized) and stained as described above. Human DC were cultured for 24 h with GEMs (1:150), human TNF-α (5 ng ml−1, PeproTech) or cRPMI (mock-treated). Cells were stained with FITC-, PE-, allophycocyanin or PerCP Cy5.5-labeled mAbs specific for CD1a, CD80, CD83, CD86, CD11c and HLA-DR (BD Pharmingen). FcγR-binding inhibitor (eBioscience, San Diego, CA) was used to reduce background straining. Stained cells were fixed with 4% paraformaldehyde and run on a DakoCytomation MoFlo flow cytometer (Carpinteria, CA). Data were collected from 10,000 to 30,000 cells and were analyzed using WinList 6.0 3D software (Verity Software House, Topsham, ME).
DC cytokine production
Cytokines were measured in 24 h culture supernatants from GEM-and control-treated DC using Cytometric Bead Array (CBA) mouse and human pro-inflammatory cytokine kits (BD Pharmingen). Samples were run on a Beckman Coulter Epics Elite flow cytometer. Cytokine concentrations were determined using standard reference curves using CBA software (BD Pharmingen).
FITC dextran uptake
Mouse and human CD11c+ cells treated with GEMs or mock-treated were incubated with 1 mg ml−1 FITC-dextran (Sigma-Aldrich, St. Louis, MO) for 1 h at 37°C or 4°C. Cells were washed with cold PBA buffer and analyzed by flow cytometry. Dextran uptake was measured as the increase in the number of FITC-positive cells incubated at 37°C vs. 4°C.
TLR signaling
TLR stimulation was assessed in HEK293 cells expressing human TLR2, 3, 4, 5, 7, 8 or 9 or expressing mouse TLR7 or TLR9 (one TLR at a time). The activity of alkaline phosphatase, which was under the control of an NF-κB inducible promoter, was measured as a readout for TLR activation. The assays were performed at InvivoGen (San Diego, CA). Briefly, cells were incubated for 16–20 h with 20 μl of GEMs (~5×108 particles) or positive control ligands as follows: hTLR2, heat-killed Listeria monocytogenes (108 cells ml−1); hTLR3, Poly(I:C) (1 μg ml−1); hTLR4, E. coli K12 LPS (100 ng ml−1); hTLR5, Salmonella typhimurium flagellin (100 ng ml−1); hTLR7, gardiquimod (1 μg ml−1); hTLR8, CL075 (1 μg ml−1); hTLR9, CpG ODN 2006 (100 ng ml−1); mTLR7, gardiquimod (1 μg ml−1); and mTLR9, CpG ODN 1826 (1 μg ml−1). Cells incubated with TNF-α (100 ng ml−1) were included as a positive control for NF-κB activation. Absorbance at 650 nm was measured in an ELISA reader.
TLR2 neutralization
Newborn or adult mouse BM-derived magnetically sorted CD11c+ DC were pre-incubated with 20 μg ml−1 of anti-human and mouse TLR2 mAb (eBioscience) or isotype control (1 h at room temperature) and were then cultured for 24 h with GEM particles (1:150) or cRPMI (mock-treated). IL-6 released to the culture supernatants was measured by ELISA (eBioscience).
Vaccines
Lactococcal GEM-LcrV particles were prepared as follows: the lcrV gene from Y. pseudotuberculosis (identical to the LcrV gene of Y. pestis strain KIM5, nt 481–1461 of Genbank entry #M26405) was subcloned by PCR from plasmid pSEC91-LcrV, and the amplified lcrV gene fragment was cloned into plasmid pPA335. The correct insertion of the gene was verified by DNA sequencing. The resulting plasmid, pPA281, was electroporated into L. lactis PA1001 for expression and secretion of the recombinant LcrV-PGN anchor domain fusion protein, as previously described9. The lactococcal PGN binding domain enables strong non-covalent binding of the vaccine antigen to GEM particles8. GEM particles prepared by heat-acid treatment of L. lactis were mixed with LcrV-PGN binding domain fusions for 30 min at room temperature8,9. One vaccine dose for GEM and GEM-LcrV contained 2.5×109 particles. The amount of LcrV bound to the GEM particles was determined by densitometry analysis; 2.5×109 particles contained 20 μg of LcrV-PGN fusion protein. The LcrV fragment represents about 60% of the fusion protein, meaning that 12 μg LcrV was present in each vaccine dose. The particles were centrifuged and resuspended in enough sterile PBS to obtain the desired GEM-LcrV concentration prior to immunization. Recombinant full length Y. pestis LcrV (without the PGN binding domain) purified from E. coli was used as subunit vaccine for nasal and parenteral immunization. Residual LPS was removed using Detoxi-Gel columns (Thermo Scientific, Rockford, IL) and endotoxin levels (<0.19 EU mg−1) monitored by chromogenic LAL test (Lonza, Allendale, NJ ).
Fluorescence microscopy
GEM-LcrV and GEM particles were stained with mouse anti-LcrV mAb (AbCam, Cambridge, MA) or an isotype control in PBA for 1 h at room temperature, followed by staining with FITC-labeled anti-mouse IgG (Invitrogen, Carlsbad, CA) for 30 min. The particles were washed, mounted in Prolong Gold (Invitrogen) and visualized using a Nikon Eclipse 2000-E UV fluorescence microscope (Melville, NY). Images were acquired using MetaVue software, version 6.1 (Universal ImagingCorp, Downingtown, PA).
In vitro antigen presentation
Negatively sorted CD11c+ DC from newborn mice were cultured for 24 h with GEMs alone, GEM-LcrV (1:100), LcrV (1.8 μg ml−1) or cRPMI (mock-stimulated). Cells were washed, irradiated and co-cultured with CD4+ and CD8+ T cells (90–95% purity) obtained from the spleen of naïve and LcrV-immune adult mice by magnetic sorting (Dynal Biotech, Oslo Norway). This last group had been immunized twice with 2 μg of LcrV-alum via i.m., 14 days apart, and spleens were harvested 3 weeks after the last immunization. Increasing numbers of purified CD11c+ DC were co-cultured with 1×105 naïve or LcrV-specific CD4+ and CD8+ T cells. As readouts of T cell stimulation, we measured lymphocyte proliferation by [3H]thymidine incorporation and the frequency of IFN-γ-secreting cells by ELISPOT, as previously described34. CD4+ and CD8+ T cells alone, CD11c+ DC alone and CD11c+ DC cultured with naïve CD4+ and CD8+ T cells were included as negative controls and their responses were subtracted from experimental wells. ConA (2 μg ml−1, Sigma) or LcrV (5 μg ml−1) served as positive controls.
Mice and immunization
BALB/c mice (8–10 weeks old, Charles River Laboratories, Wilmington, MA) were bred and housed under specific pathogen-free conditions as previously described36. Experimental groups contained 3–5 litters (~6 pups per litter). Newborn mice were immunized i.n. on day 7, 15 and 21 after birth with 1 dose (2.5×109 particles) of GEM-LcrV (12 μg LcrV), with GEMs alone or with 20 μg of recombinant LcrV (~5 μl, 2.5 μl per nare). A group immunized i.m. on days 7, 15 and 21 after birth with 2 μg of LcrV adsorbed to 0.5% alhydrogel (Brenntag Biosector, Frederikssund, Denmark) was included as a positive control. Blood samples were obtained at different time points, as previously described34. Studies were approved by the University of Maryland Institutional Animal Care and Use Committee.
LcrV-specific antibodies
LcrV-specific serum IgG, IgM and IgA levels were measured by ELISA. Immulon II plates were coated with endotoxin-free LcrV at 1 μg ml−1 in carbonate buffer (pH 9.6) for 3 h at 37°C and blocked overnight with 10% dry milk (Nestle USA, Solon, OH) in PBS. Sera were tested in serial dilutions in PBS containing Tween 20 and 10% dry milk. Antibodies were detected with HRP-labeled antibodies specific for mouse IgG, IgG1, IgG2a (Roche, Indianapolis, IN), IgM (Kirkegaard & Perry Laboratories, KPL, Gaithersburg, MD) and IgA (Zymed Laboratories, San Francisco, CA) followed by the TMB substrate (KPL). After 15 min of incubation, the reaction was stopped with 1 M H3PO4. Endpoint titers were calculated through a linear regression as the reciprocal of the serum dilution that produced an Absorbance 450 nm value of 0.2 above the blank and reported in ELISA units (EU) ml−1.
IgG and IgA ASC
Single cell suspensions from the spleen, BM and NALT collected on days 15, 21 and 56 after birth, as previously described34, were incubated overnight at 37°C, 5% CO2 in plates previously coated with LcrV (5 μg ml−1) and blocked with cRPMI. HRP-labeled goat anti-mouse IgG or IgA (Zymed) diluted in PBS with 1% BSA were used as conjugates in agarose overlay. True Blue was used as the substrate (KPL). Spots were counted in a stereomicroscope, and the results were expressed as the mean number of IgG ASC per 106 cells from quadruplicate wells. Spots from control wells were subtracted from experimental wells. A positive response was defined as ≥4 spots per 106 cells.
Cytokines in mucosal tissues
NALT and lung mononuclear cells were obtained on day 21 after birth from naïve, GEM- and GEM-LcrV-immunized newborn mice, as previously described36. Cells were stimulated in vitro for 48 h with LcrV (2.5 μg ml−1) or cRPMI (mock-stimulated), and cytokine levels in the culture supernatants were measured using multiplex Meso ScaleDiscovery (MSD, Gaithersburg, MD) kits, as recommended by the manufacturer. Plates were read using the MSD Sector Imager 2400.
T cell proliferation
Single cell suspensions from spleens were incubated with 2.5 μg ml−1 of LcrV, cRPMI or ConA (5 μg ml−1, positive control) for 3–7 days at 37°C, 5% CO2. Cell proliferation was measured by incorporation of [3H]thymidine, as previously described34,36.
Y. pestis challenge
Mice were challenged i.v. with ~ 30 MLD50 (3.36×103 CFU) of Y. pestis EV76 in 0.2 ml of sterile PBS. FeCl2 (40 μg per mouse) was administered intraperitoneally immediately before challenge to enhance bacterial virulence. Health status, weight loss and survival were monitored daily for 14 days34. All survivors were humanely euthanized at the end of the monitoring period.
Laser confocal microscopy
GEM particles (25×109 particles) were incubated with 0.01g FITC (Sigma) in 0.1 M boric acid, pH 9.0, for 60 min at room temperature in a shaker. Cord blood-derived CD11c+DC were cultured with FITC-GEMs (1:100), washed, blocked with human FcγR- binding inhibitor and stained with a monoclonal anti-human CD11c antibody (BD Pharmingen) in PBA for 1 h at room temperature, followed by staining with Alexa Fluor 546-labeled anti-mouse IgG (Invitrogen). To visualize the nuclei, cells were incubated with 4′,6′-diamidino-2-phenylindole dihydrochloride (DAPI, Invitrogen) in PBA buffer and were mounted in Prolong Gold (Invitrogen). Stained DC were visualized using a Zeiss LSM510 META laser scanning confocal microscope (Gottingen, Germany). Images show the individual and Z-stack projections collected at 0.41 μm intervals, analyzed with Zeiss LSM Examiner version 4.2 software.
Mixed lymphocyte reaction
Magnetically sorted adult human CD3+ T cells obtained from peripheral blood were cultured for 5 days with irradiated cord blood- or adult-derived CD11c+ DC pre-treated with GEMs, human TNF-α, or cRPMI (mock-treated). Negative controls included T cells and DC alone. T cell proliferation was measured by [3H]thymidine incorporation.
Statistical analysis
Immune responses were compared using the Student’s t-test or the Mann-Whitney U test. Differences with P<0.05 were considered significant. Statistical analysis was performed using SigmaStat 3.1 (SigmaStat software, Erkrath, Germany).
Acknowledgments
The authors thank personnel from the CVD Applied Immunology Section for exceptional technical support, Dr. Scott Lloyd (CVD) for providing plasmid pSEC91-LcrV, Dr. Wilbur Chen and Dr. Alan Cross (CVD) for TLR2/4 preliminary studies and Dr. Govert Schouten (Mucosis BV) for helpful discussions. This work was supported, in part, by National Institute of Health grant R01-AI065760 (to M.F. P) and Mucosis BV.
Footnotes
DISCLOSURE
The authors declare no conflict of interest.
References
- 1.Siegrist CA. Neonatal and early life vaccinology. Vaccine. 2001;19:3331–3346. doi: 10.1016/s0264-410x(01)00028-7. [DOI] [PubMed] [Google Scholar]
- 2.Siegrist CA. The challenges of vaccine responses in early life: selected examples. J Comp Pathol. 2007;137(Suppl 1):S4–S9. doi: 10.1016/j.jcpa.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 3.Wilson CB, Kollmann TR. Induction of antigen-specific immunity in human neonates and infants. Nestle Nutr Workshop Ser Pediatr Program. 2008;61:183–195. doi: 10.1159/000113493. [DOI] [PubMed] [Google Scholar]
- 4.Cortese VS. Neonatal immunology. Vet Clin North Am Food Anim Pract. 2009;25:221–227. doi: 10.1016/j.cvfa.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Willems F, Vollstedt S, Suter M. Phenotype and function of neonatal DC. Eur J Immunol. 2009;39:26–35. doi: 10.1002/eji.200838391. [DOI] [PubMed] [Google Scholar]
- 6.Adkins B, Leclerc C, Marshall-Clarke S. Neonatal adaptive immunity comes of age. Nat Rev Immunol. 2004;4:553–564. doi: 10.1038/nri1394. [DOI] [PubMed] [Google Scholar]
- 7.Demirjian A, Levy O. Safety and efficacy of neonatal vaccination. Eur J Immunol. 2008;39:36–46. doi: 10.1002/eji.200838620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bosma T, et al. Novel surface display system for proteins on non-genetically modified Gram-positive bacteria. Appl Environ Microbiol. 2006;72:880–889. doi: 10.1128/AEM.72.1.880-889.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Roosmalen ML, et al. Mucosal vaccine delivery of antigens tightly bound to an adjuvant particle made from food-grade bacteria. Methods. 2006;38:144–149. doi: 10.1016/j.ymeth.2005.09.015. [DOI] [PubMed] [Google Scholar]
- 10.Mshvildadze M, Neu J, Mai V. Intestinal microbiota development in the premature neonate: establishment of a lasting commensal relationship. Nutr Rev. 2008;66:658–663. doi: 10.1111/j.1753-4887.2008.00119.x. [DOI] [PubMed] [Google Scholar]
- 11.Guandalini S. Probiotics for children with diarrhea: an update. J Clin Gastroenterol. 2008;42(Suppl 2):S53–S57. doi: 10.1097/MCG.0b013e3181674087. [DOI] [PubMed] [Google Scholar]
- 12.Srinivasan R, Meyer R, Padmanabhan R, Britto J. Clinical safety of Lactobacillus casei shirota as a probiotic in critically ill children. J Pediatr Gastroenterol Nutr. 2006;42:171–173. doi: 10.1097/01.mpg.0000189335.62397.cf. [DOI] [PubMed] [Google Scholar]
- 13.Myhre AE, Aasen AO, Thiemermann C, Wang JE. Peptidoglycan--an endotoxin in its own right. Shock. 2006;25:227–235. doi: 10.1097/01.shk.0000191378.55274.37. [DOI] [PubMed] [Google Scholar]
- 14.Ueno H, et al. Dendritic cell subsets in health and disease. Immunol Rev. 2007;219:118–142. doi: 10.1111/j.1600-065X.2007.00551.x. [DOI] [PubMed] [Google Scholar]
- 15.Smiley ST. Current challenges in the development of vaccines for pneumonic plague. Expert Rev Vaccines; 2008;7:209–221. doi: 10.1586/14760584.7.2.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Audouy SA, et al. Lactococcus lactis GEM particles displaying pneumococcal antigens induce local and systemic immune responses following intranasal immunization. Vaccine. 2006;24:5434–5441. doi: 10.1016/j.vaccine.2006.03.054. [DOI] [PubMed] [Google Scholar]
- 17.Audouy SA, et al. Development of lactococcal GEM-based pneumococcal vaccines. Vaccine. 2007;25:2497–2506. doi: 10.1016/j.vaccine.2006.09.026. [DOI] [PubMed] [Google Scholar]
- 18.Yamamoto S, Tin-Tin WS, Yoshida Y, Kunugita N, Arashidani K, Fujimaki H. Children’s immunology, what can we learn from animal studies (2): Modulation of systemic Th1/Th2 immune response in infant mice after prenatal exposure to low-level toluene and toll-like receptor (TLR) 2 ligand. J Toxicol Sci. 2009;34(Suppl 2):SP341–SP348. doi: 10.2131/jts.34.sp341. [DOI] [PubMed] [Google Scholar]
- 19.McCarron M, Reen DJ. Activated human neonatal CD8+ T cells are subject to immunomodulation by direct TLR2 or TLR5 stimulation. J Immunol. 2009;182:55–62. doi: 10.4049/jimmunol.182.1.55. [DOI] [PubMed] [Google Scholar]
- 20.Parant M, Parant F, Chedid L. Enhancement of the neonate’s nonspecific immunity to Klebsiella infection by muramyl dipeptide, a synthetic immunoadjuvant. Proc Natl Acad Sci U S A. 1978;75:3395–3399. doi: 10.1073/pnas.75.7.3395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kool JL. Risk of person-to-person transmission of pneumonic plague. Clin Infect Dis. 2005;40:1166–1172. doi: 10.1086/428617. [DOI] [PubMed] [Google Scholar]
- 22.Mohamadzadeh M, Duong T, Sandwick SJ, Hoover T, Klaenhammer TR. Dendritic cell targeting of Bacillus anthracis protective antigen expressed by Lactobacillus acidophilus protects mice from lethal challenge. Proc Natl Acad Sci U S A. 2009;106:4331–6. doi: 10.1073/pnas.0900029106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xin KQ, et al. Immunogenicity and protective efficacy of orally administered recombinant Lactococcus lactis expressing surface-bound HIV Env. Blood. 2003;102:223–228. doi: 10.1182/blood-2003-01-0110. [DOI] [PubMed] [Google Scholar]
- 24.Daniel C, et al. Protection against Yersinia pseudotuberculosis infection conferred by a Lactococcus lactis mucosal delivery vector secreting LcrV. Vaccine. 2009;27:1141–1144. doi: 10.1016/j.vaccine.2008.12.022. [DOI] [PubMed] [Google Scholar]
- 25.Robinson K, Chamberlain LM, Schofield KM, Wells JM, Le Page RW. Oral vaccination of mice against tetanus with recombinant Lactococcus lactis. Nat Biotechnol 1997. 2009;15:653–657. doi: 10.1038/nbt0797-653. [DOI] [PubMed] [Google Scholar]
- 26.Zeng G, et al. NSOM- and AFM-based nanotechnology elucidates nano-structural and atomic-force features of a Y. pestis V immunogen-containing particle vaccine capable of eliciting robust response. Proteomics. 2009;9:1538–1547. doi: 10.1002/pmic.200800528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Siegrist CA. Mechanisms by which maternal antibodies influence infant vaccine responses: review of hypotheses and definition of main determinants. Vaccine. 2003;21:3406–3412. doi: 10.1016/s0264-410x(03)00342-6. [DOI] [PubMed] [Google Scholar]
- 28.Griebel PJ. Mucosal vaccination of the newborn: an unrealized opportunity. Expert Rev Vaccines. 2009;8:1–3. doi: 10.1586/14760584.8.1.1. [DOI] [PubMed] [Google Scholar]
- 29.Conroy ME, Shi HN, Walker WA. The long-term health effects of neonatal microbial flora. Curr Opin Allergy Clin Immunol. 2009;9:197–201. doi: 10.1097/ACI.0b013e32832b3f1d. [DOI] [PubMed] [Google Scholar]
- 30.Latvala S, et al. Potentially probiotic bacteria induce efficient maturation but differential cytokine production in human monocyte-derived dendritic cells. World J Gastroenterol 2008. 2009;14:5570–5583. doi: 10.3748/wjg.14.5570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yam KK, Pouliot P, N’diaye MM, Fournier S, Olivier M, Cousineau B. Innate inflammatory responses to the Gram-positive bacterium Lactococcus lactis. Vaccine. 2008;26:2689–2699. doi: 10.1016/j.vaccine.2008.03.024. [DOI] [PubMed] [Google Scholar]
- 32.Niers LE, et al. Selection of probiotic bacteria for prevention of allergic diseases: immunomodulation of neonatal dendritic cells. Clin Exp Immunol. 2007;149:344–352. doi: 10.1111/j.1365-2249.2007.03421.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Debarry J, et al. Acinetobacter lwoffii and Lactococcus lactis strains isolated from farm cowsheds possess strong allergy-protective properties. J Allergy Clin Immunol. 2007;119:1514–1521. doi: 10.1016/j.jaci.2007.03.023. [DOI] [PubMed] [Google Scholar]
- 34.Ramirez K, Capozzo AV, Lloyd SA, Sztein MB, Nataro JP, Pasetti MF. Mucosally delivered Salmonella typhi expressing the Yersinia pestis F1 antigen elicits mucosal and systemic immunity early in life and primes the neonatal immune system for a vigorous anamnestic response to parenteral F1 boost. J Immunol. 2009;182:1211–1222. doi: 10.4049/jimmunol.182.2.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Steen A, et al. Cell wall attachment of a widely distributed peptidoglycan binding domain is hindered by cell wall constituents. J Biol Chem. 2003;278:23874–23881. doi: 10.1074/jbc.M211055200. [DOI] [PubMed] [Google Scholar]
- 36.Capozzo AV, Cuberos L, Levine MM, Pasetti MF. Mucosally delivered Salmonella live vector vaccines elicit potent immune responses against a foreign antigen in neonatal mice born to naive and immune mothers. Infect Immun. 2004;72:4637–4646. doi: 10.1128/IAI.72.8.4637-4646.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]