Observational studies and in vivo experiments have raised concern that the cardioprotective effects of taking aspirin are blocked by ibuprofen, a non-steroidal anti-inflammatory drug that competitively inhibits aspirin's binding site on platelets.1,2 We determined whether prescribing aspirin and ibuprofen to patients being discharged after myocardial infarction was associated with increased risk of death.
Participants, methods, and results
The database compiled by the Cooperative Cardiovascular Project consisted of 234 769 Medicare patients in the United States who were hospitalised with a myocardial infarction between 1994 and 1996.3 We identified patients aged ≥ 65 with myocardial infarction who were prescribed aspirin on discharge and excluded patients who had repeat admissions, had terminal illness, had incomplete drug records, or had been transferred. The outcome measure was time to death within a year of discharge, which we ascertained from the Medicare enrolment database.4 We compared the baseline characteristics of patients prescribed only aspirin, prescribed aspirin and ibuprofen, and prescribed aspirin and other non-steroidal anti-inflammatory drugs with χ2 tests and analysis of variance. We compared Kaplan-Meier survival curves with the log rank test. We developed a Cox proportional hazards mortality model including demographics, medical history, admission presentation, hospital course, and discharge care. We did statistical calculations with SAS.
A total of 70 316 patients were prescribed aspirin at discharge from hospital; 66 739 were prescribed aspirin alone, 844 aspirin and ibuprofen, and 2733 aspirin and other non-steroidal anti-inflammatory drugs. Patients prescribed only aspirin had more comorbidity and had had more complications in hospital (see bmj.com). Totals of 11 546 (17.5%) patients who were prescribed only aspirin, 118 (14.0%) who were prescribed aspirin and ibuprofen, and 432 (15.8%) who were prescribed aspirin and other non-steroidal anti-inflammatory drugs died within a year after discharge (log rank P = 0.003) (figure). Our multivariable model found that patients prescribed aspirin and ibuprofen on discharge had a risk of death that was comparable to that of patients prescribed aspirin alone (hazard ratio 0.84; 95% confidence interval 0.70 to 1.01) or prescribed aspirin and another non-steroidal anti-inflammatory drug (0.96; 0.86 to 1.06).
Figure 1.
Kaplan-Meier survival curves for elderly US survivors of myocardial infarction prescribed aspirin alone, aspirin and ibuprofen, or aspirin and a different non-steroidal anti-inflammatory drug on discharge from hospital
Comment
Aspirin and ibuprofen did not adversely interact in this cohort of elderly patients discharged after myocardial infarction. The pharmacodynamic interaction of aspirin and ibuprofen may not have a significant impact on patient outcomes.
Recently, investigators reported that patients with established cardiovascular disease who were prescribed aspirin and ibuprofen on discharge were at increased risk of death compared with patients discharged on aspirin alone.2 The findings received extensive media attention and prompted recommendations against patients with coronary disease using ibuprofen.5 However, their study included only 187 patients on both aspirin and ibuprofen and did not adjust for severity of cardiovascular disease. Conversely, we found that patients taking aspirin and ibuprofen have similar mortality to patients discharged on aspirin alone. In comparison, our analysis included four times as many patients prescribed both aspirin and ibuprofen and we could adjust for measures of severity of disease, such as shock, ejection fraction, and heart failure.
Because of the non-experimental design, our analysis may have allowed residual confounding. In particular, we had no information about patterns of use of ibuprofen after discharge from hospital. Because ibuprofen and other non-steroidal anti-inflammatory drugs are available over the counter, we have likely underestimated the overall use of ibuprofen, which could bias our results toward the null. Nevertheless, recommendations that patients with coronary artery disease should avoid taking both ibuprofen and aspirin may be unfounded.
Supplementary Material
Editorial by Kimmel and Strom
Contributors: HMK and JPC conceived and designed the study and drafted the report. YW provided statistical expertise. ELP, FAM, and EPH did analysis and wrote the report. HMK is guarantor.
Funding: FAM is supported by NIH/NIA Research Career Award K08-AG01011.
Competing interests: EPH has received funds from Sanofi.
Ethical approval: Not needed.
References
- 1.FitzGerald GA. Parsing an enigma: the pharmacodynamics of aspirin resistance. Lancet 2003;361: 542-4. [DOI] [PubMed] [Google Scholar]
- 2.MacDonald TM, Wei L. Effect of ibuprofen on cardioprotective effect of aspirin. Lancet 2003;361: 573-4. [DOI] [PubMed] [Google Scholar]
- 3.O'Connor GT, Quinton HB, Traven ND, Ramunno LD, Dodds TA, Marciniak TA, et al. Geographic variation in the treatment of acute myocardial infarction: the cooperative cardiovascular project. JAMA 1999;281: 627-33. [DOI] [PubMed] [Google Scholar]
- 4.Fleming C, Fisher ES, Chang CH, Bubolz TA, Malenka DJ. Studying outcomes and hospital utilization in the elderly: the advantages of a merged database for Medicare and Veterans Affairs hospitals. Med Care 1992;30: 377-91. [DOI] [PubMed] [Google Scholar]
- 5.Associated Press. Ibuprofen may not be heart healthy. USA Today 2003. Feb 13: D1.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



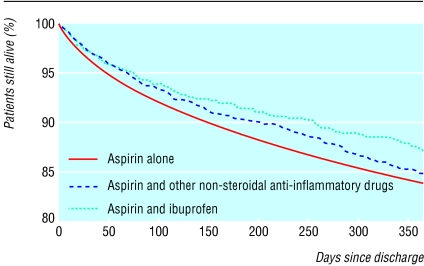
 Table A on
Table A on