Abstract
The purpose of this study was 2-fold. First, we evaluated standard chemotherapy in the guinea pig model of tuberculosis to determine if this animal species could productively be used for this purpose. Second, given the similarities of the pathology of disease in guinea pigs and humans, we wished to evaluate additional parameters, including magnetic resonance imaging, microscopy, and cytokine expression and lymphocyte phenotypes, in response to an infection treated with drug therapy. This study shows that conventional rifampin-isoniazid-pyrazinamide chemotherapy significantly decreased the numbers of the highly virulent Erdman K01 strain of Mycobacterium tuberculosis, with most of the bacilli being eliminated in a month. Despite this result, bacteria could still be detected in the lungs and other tissues for at least another 3 to 4 months. Resolution of the nonnecrotic granulomas in the lungs and lymph nodes could be clearly visualized by magnetic resonance imaging at the macroscopic level. Microscopically, the majority of the pulmonary and extrapulmonary inflammation resolved spontaneously, leaving residual lesions composed of dystrophic calcification and fibrosis marking the site of necrosis of the primary lesion. Residual calcified lesions, which were also associated with pulmonary lymphangitis, contained acid-fast bacilli even following aggressive chemotherapy. The presence of intact extracellular bacilli within these lesions suggests that these could serve as the primary sites of disease reactivation. The chemotherapy reduced the level of T-cell influx into infected tissues and was accompanied by a large and sustained increase in TH1 cytokine expression. Chemotherapy also prevented the emergence in lung tissues of high levels of interleukin-10 and Foxp3-positive cells, known markers of regulatory T cells.
The global epidemic caused by the bacterial pathogen Mycobacterium tuberculosis continues unabated, with the most recent figures indicating that there are approximately 8 million new cases and about 2.7 million deaths each year (13-15, 22). Of the 45 million individuals infected with HIV, it is now estimated that about one-third are coinfected with M. tuberculosis (16, 19); this situation is particularly serious in Saharan Africa (2, 7, 17). Even more troubling is the fact that the incidence of M. tuberculosis isolates that have become resistant to multiple drugs has now reached 0.5 million cases per year (8, 11). The latter situation is compounded by the fact that a new drug for tuberculosis has not been introduced for a quarter of a century, but there is cause for optimism here, given the establishment of a pipeline of promising new compounds, some of which are now being introduced into controlled clinical trials (18, 42, 43).
Because it is highly cost-effective, the mouse is the animal model of choice for the initial screening of new drugs and drug combinations (30); however, there is growing interest in the further evaluation of secondary animal models. This is driven by the fact that the M. tuberculosis infection in conventional inbred mice differs from that in other small-animal models, notably, the guinea pig and rabbit, in terms of the pathology of pulmonary and extrapulmonary lesions (3). While mice develop poorly organized foci of pulmonary inflammation mostly composed of macrophages interspersed with aggregates of lymphocytes, guinea pigs form well-organized granulomas with central necrosis, a hallmark of the disease in humans. In addition, like humans, guinea pigs develop severe pyogranulomatous and necrotizing lymphadenitis of the draining lymph nodes as part of the primary lesion complex (4). Within necrotic lesions, whether they are pulmonary or extrapulmonary, individual and small clusters of extracellular acid-fast bacilli can be found attached or enmeshed in a complex matrix that is composed of remnants of necrotic host cells and that ultimately heals by dystrophic calcification and fibrosis (3, 31). Given these important similarities, the purpose of the study described here was to comprehensively evaluate the potential usefulness of the guinea pig model for testing the effects of drug therapy.
MATERIALS AND METHODS
Guinea pigs.
Female outbred Hartley guinea pigs (weight, ∼500 g) were purchased from the Charles River Laboratories (North Wilmington, MA) and were held under barrier conditions in a biosafety level 3 animal laboratory. The specific-pathogen-free nature of the guinea pig colonies was demonstrated by testing sentinel animals. All experimental protocols were approved by the Animal Care and Usage Committee of Colorado State University.
Experimental infections in guinea pigs.
Guinea pigs were infected (n = 5) by using a Madison chamber aerosol generation device, which delivered approximately 20 Mycobacterium tuberculosis strain Erdman K01 bacilli into the lungs. The animals were then harvested and analyzed for bacterial load determinations (n = 5), histopathology (n = 5), and flow cytometric analysis (n = 4) on days 25, 50, 75, 100, 125, and 150 days of the infection. As described previously (31), the bacterial loads in the organs of the guinea pigs at each time point of the study were determined by plating serial dilutions of homogenates of lungs (right cranial lobe), spleen, and mediastinal lymph node tissues on nutrient Middlebrook 7H11 agar and counting the numbers of CFU after 6 weeks of incubation at 37°C. The bacterial load for each organ was calculated and converted to logarithmic units. The data were expressed as the mean log10 number of CFU ± the standard error of the mean for each group.
Experimental chemotherapy in guinea pigs.
On day 20 of the infection, four guinea pigs were euthanized to determine the bacterial load prior to the start of drug treatment on day 25. The remaining animals were randomly assigned to two groups: 25 guinea pigs in the control group and 60 guinea pigs in the drug treatment group. Chemotherapy was then administered 5 days a week for the duration of the 19-week treatment regimen. The animals in the control group were treated with a formulation consisting of a mixture of 40% (wt/vol) sucrose and 20% (wt/vol) pumpkin (100% pure pumpkin; Libby) supplemented with vitamin C (50 mg/kg of mean body weight) and commercial Lactobacillus (BD Lactinex) (all purchased from Walmart, Fort Collins CO), while the animals in the experimental group were treated with rifampin (RIF; 50 mg/kg of mean body weight), isoniazid (INH; 30 mg/kg of mean body weight), and pyrazinamide (PZA; 100 mg/kg of mean body weight), which were incorporated into the sucrose vehicle. The doses were chosen on the basis of previous pharmacokinetic and pharmacodynamic studies performed with this species (26, 31). A split feeding protocol was used, with INH and PZA being given in the morning and RIF being given in the afternoon to minimize drug toxicity interactions. The animals were carefully monitored on a daily basis using the Karnovsky scale (40); usually, about a week or so after the drug treatment was started, the animals began to go off feed, necessitating oral feeding with a syringe of the nutrient-rich puree, vitamin C, and Lactobacillus (Lactobacillus was given to help stabilize the cecal flora and prevent gastrointestinal dysbacteriosis or antibiotic-associated enteritis). This was performed by gently cradling the animal in the crook of the arm and allowing the animal to consume the mixture from a 1-ml syringe. Two days prior to necropsy, randomly selected guinea pigs were taken off the drug therapy. These animals were then euthanized; and their lungs, spleens, and mediastinal lymph nodes (MLNs) were removed. The number of viable organisms was determined by plating serial dilutions of 10-ml organ tissue homogenates on nutrient Middlebrook 7H11 agar plates (Gibco BRL, Gaithersburg, MD). The bacterial colonies were then counted after 3 to 4 weeks of incubation at 37°C.
Histological analysis.
The left caudal lung lobe, spleen, and lymph nodes from each guinea pig (n = 5) were collected at necropsy and fixed in 4% paraformaldehyde in phosphate-buffered saline (PBS). Randomly selected tissue sections were embedded in paraffin and cut to 5 μm on a microtome. The tissue sections were mounted on glass slides, deparaffinized and stained with hematoxylin-eosin and carbolfuchsin by the Ziehl-Neelsen method, as reported previously (5). The lung and lymph node lesion areas relative to the normal tissue area were quantified by a stereology-based method, referred to as the area fraction fractionator, with the investigator blind to all treatment groups. The stereology workstation consisted of a Nikon 80i research microscope equipped for bright-field and fluorescence microscopy with chromatic aberration-free infinity (CFI) objectives (×2/0.01 Plan Apo, ×4/0.2 Plan Apo, ×10/0.30 Plan Fluor, ×20/0.75 Plan Apo, ×40/0.75 Plan Fluor, ×100/1.40 Plan Apo), a three-axis computer-controlled stepping stage with linear grid encoders, a z-axis motorized specimen stage for automated sampling, a personal computer with a frame grabber board, a color digital camera, a 24-in. monitor, and stereology and virtual slice zoomify software (StereoInvestigator, version 8.2; MBF Bioscience, Williston, VT) with the following: three-dimensional (3D) serial section reconstruction, solid modeling, virtual slice, and confocal and magnetic resonance imaging (MRI) modules.
The lung and lesion areas on representative hematoxylin-eosin-stained sections were determined. In addition, acid-fast-stained sections were evaluated. The area of inflammation relative to the area of normal tissue parenchyma was estimated from representative lung, lymph node, and spleen tissue sections evaluated at ×20 magnification. A total of 8 to 12 fields were randomly selected by the computer, and a counting frame (2,000 μm2) containing probe points with a grid spacing of 200 μm was used to define the areas of interest (lesions and lungs). The data are expressed as the mean ratio of the lesion area to the lung area for all the animals within a treatment group. A lesion shown in a photomicrograph represents the section that is closest to the mean value for each group.
MRI.
Four lungs were harvested from the animals before the start of treatment, and thereafter, the lungs of two guinea pigs in each group were harvested at the indicated time points. At the time of euthanasia, the lungs were inflated with 20 ml of room air per kg of body weight by tracheal intubation. The pulmonary vasculature was flushed free of blood with 60 ml of phosphate-buffered saline and perfusion fixed with 60 ml of 4% paraformaldehyde via the right ventricle. Once the lungs were perfusion fixed, they were removed en bloc and immersion fixed for 1 week in 4% paraformaldehyde. After immersion fixation, the heart and esophagus of each animal were dissected from the lungs. The lungs and attached mediastinal lymph nodes were embedded in 4% low-melting-point agarose in phosphate-buffered saline. The embedded lungs were then scanned by MRI. The lungs were harvested from the control guinea pigs on days 29, 50, 73, and 100 following exposure to M. tuberculosis and from the drug-treated guinea pigs on days 29, 50, 78, 105, and 134 following exposure to M. tuberculosis. MRI scans were performed with a 1.5-T Signa 9.1 LX magnetic resonance instrument (General Electric Medical Systems, Milwaukee, WI), with the specimens being placed in a phased-array extremity coil (28). A T1-weighted 3D volume scan was acquired (repetition time, 20 ms; echo time, 6.4 ms; slice thickness, 1.2 mm; field of view, 6 cm) for an in-plane spatial resolution of 234 μm. Images of the entire lung specimen obtained by MRI were evaluated by segmentation thresholding analysis with the Amira 2.3 program (Visage Imaging, Andover, MA). A line probe technique was used to select the boundaries between the signal intensities for healthy and diseased lungs. From that signal intensity boundary, a threshold value was used for automated selection of all tissues exhibiting that signal intensity and higher. Tissues such as heart and lymph nodes were segmented manually, and whole-lung tracings were also made to quantify the total sample size.
Flow cytometry.
To prepare single-cell suspensions, the lungs and lymph nodes were perfused with 20.0 ml of a solution containing PBS and heparin (50 U/ml; Sigma-Aldrich, St. Louis, MO) through the pulmonary artery; and the caudal lobe and portions of the lymph nodes were aseptically removed from the pulmonary cavity, weighed, placed in medium, and dissected. In addition, leukocytes were separated from 10 ml of guinea pig blood as described before (40). The dissected lung tissue was incubated with complete Dulbecco modified Eagle medium (cDMEM) containing collagenase XI (0.7 mg/ml; Sigma-Aldrich) and type IV bovine pancreatic DNase (30 μg/ml; Sigma-Aldrich) for 30 min at 37°C. The digested lungs were further disrupted by gently pushing the tissue twice through a cell strainer (BD Biosciences, Lincoln Park, NJ). Red blood cells were lysed with ammonium chloride-potassium (ACK) lysis buffer, washed, and resuspended in cDMEM. Total cell numbers were determined by flow cytometry with liquid counting beads, as described by the manufacturer (BD PharMingen, San Jose, CA).
Flow cytometric analysis of cell surface markers.
Suspensions of single cells from the lungs and portions of the whole spleens and lymph nodes were prepared as described recently (40). Thereafter, suspensions of cells from each guinea pig were first incubated with CD4 (45), CD8 (45), pan-T-cell (44, 45), CD45 (23), MIL4 (24), B-cell (25), macrophage (27), and class II (27, 45) antibodies at 4°C for 30 min in the dark and after the cells were washed with PBS containing 0.1% sodium azide (Sigma-Aldrich). In addition, membrane permeabilization with Leucoperm permeabilizer (Serotec Inc, Raleigh, NC) was completed, according to the instructions of the manufacturer, before staining with macrophages (27) and major histocompatibility complex (MHC) class II (46) antibodies. Data acquisition and analysis were done with a FACscalibur fluorescence-activated cell sorter (FACS; BD Biosciences, Mountain View, CA) and CellQuest software (BD Biosciences, San Jose, CA). Compensation for the spectral overlap for each fluorochrome was done by using CD4, MIL4, or CD3 antigens from cells gated in the low forward scatter versus low side scatter, moderate to high forward scatter versus moderate to high side scatter, low side scatter versus MIL4-positive regions, high side scatter versus MIL4-negative regions, and high side scatter versus MIL4-positive regions. Analyses were performed with an acquisition of at least T cells 100,000 total events.
RT-PCR analysis.
The levels of expression of mRNAs encoding the cytokines gamma interferon (IFN-γ), interleukin-12p40 (IL-12p40), tumor necrosis factor alpha (TNF-α), IL-8, transforming growth factor β (TGF-β), and IL-10, as well as the regulatory T-cell-associated intracellular marker Foxp3, were quantified by real-time reverse transcription-PCR (RT-PCR). One lobe from each guinea pig (n = 5) lung was added to 1 ml of TRIzol RNA reagent (Invitrogen), and the mixture was homogenized and immediately frozen. Total RNA was extracted according to the manufacturer's protocol. RNA samples from each group and each time point were reverse transcribed with reverse transcriptase (Moloney murine leukemia virus reverse transcriptase; Invitrogen). cDNA samples of 4.0 μl were then amplified with iQ SYBR green supermix (Bio-Rad), according to the manufacturer's protocol, on an iQ5 iCycler amplification detection system (Bio-Rad). A negative control prepared by the use of ultrapure molecular biology-grade water as the template and a nontemplate control were run to confirm that the signals were derived from RNA and were not due to the presence of contaminating genomic DNA. In order to ensure that only the correct gene was amplified and that the amplicon was not due to the presence of a primer-dimer or nonspecific secondary products, melting curve analysis was performed for each run. The fold induction of mRNA was determined by analyzing the cycle threshold (CT) values normalized for expression of the CT for hypoxanthine phosphoribosyltransferase (HPRT). The primer sequences for guinea pig IFN-γ, TNF-α, IL-8, TGF-β1, IL-12p40, and 18S rRNA were published previously (1, 10). The primer sequences for guinea pig Foxp3 and IL-10 were determined with assistance from Anand Damodaran (Genotypic Technology, Bangalore, India). The sequences of the primers used for Foxp3 were as follows: forward primer, 5′-AGAAAGCACCCTTTCAAGCA-3′; reverse primer, 5′-GAGGAAGTCCTCTGGCTCCT-3′. The sequences of the primers used for IL-10 were as follows: forward primer, 5′-TTCTTCCAAACACAGGATCAGC-3′; reverse primer, 5′-TCATTTCCGATAGGGCTTGG-3′.
Statistical analysis.
The data presented here are representative of those from two experiments and are presented with the mean values for individual guinea pigs within each group (n = 5) ± the standard errors of the means (SEMs). Analysis was performed by the use of analysis of variance.
RESULTS
Effect of chemotherapy on bacterial load.
The course of infection was compared between control guinea pigs receiving a sucrose-nutrient vehicle and those receiving chemotherapy with INH, RIF, and PZA. Guinea pigs were exposed to approximately 20 bacilli of the highly virulent strain M. tuberculosis Erdman K01; and the bacterial loads in the lungs, spleens, and lymph nodes were determined at the time points indicated in Fig. 1. In the control animals, the infection progressed rapidly for about 50 days, before the tissue bacterial load peaked. Although some decline in the bacterial numbers in all three target organs was seen, by day 100 virtually all of these animals had died or were humanely euthanized because they reached the predetermined value on the Karnovsky scale.
FIG. 1.
The bacterial counts in the lungs (A), lymph nodes (B), and spleens (C) from guinea pigs infected with a low dose of M. tuberculosis Erdman K01 and treated with 40% sucrose (solid squares) and receiving chemotherapy (INH, PZA, and RIF; open squares) were compared on days 25, 50, 75, 100, 125, and 150. The results are expressed as the average (n = 5) bacterial load in each group, expressed as the log10 number of CFU (± SEM). It should be noted that the values at later time points are at or below the usual detection limits for these assays, and hence, their accuracy cannot be guaranteed.
The administration of chemotherapy had a profound effect on the bacterial load over the first 30 days of treatment, rapidly reducing the number of surviving bacilli to about 100 CFU. Similar effects were seen in the draining lymph nodes and the spleen. After 30 days of infection, the rate of reduction of the tissue bacterial counts continued to decline, but very slowly, with some residual bacterial colonies being found on day 100 of infection. Thus, as in the mouse model, the bacterial clearance patterns followed a biphasic curve, with initially rapid reductions being followed by a very slow second phase.
MRI scans and analysis.
MRI scans of ex vivo specimens were performed in order to quantify the lesion burden of the lungs and the draining lymph nodes from the two study groups. A representative scan is shown in Fig. 2A, which shows numerous lung lesions and affected lymph nodes on a typical image obtained by MRI from a paraformaldehyde-fixed lung specimen (collected on day 50 of infection). Serial images through the entire lung were used to quantify the relative lesion-to-lung and lesion-to-lymph node volumes, as shown in Fig. 2B and C. No differences between the control and the treated animals could be seen early on, but after that initial lag, this radiographic approach showed smaller and smaller lesions in the lungs and lymph nodes relative to sizes of the lesions in the control animals. The treated animals also had substantially less lymph node involvement than the untreated controls at 100 days postinfection (Fig. 2C). Comparison of representative MRI slices obtained over the course of the infection clearly illustrate the beneficial effects of the chemotherapy and the gradual resolution of the disease (Fig. 3).
FIG. 2.
MRI scans of guinea pigs receiving chemotherapy. (A) Numerous granulomas (white nodules) and enlarged lymph nodes (*) on a typical two-dimensional MRI slice from the 3D lung volume of a fixed lung specimen from a control guinea pig (collected at 50 days postinfection); (B) granuloma disease burden (cm3) in treated (solid squares) versus control (solid triangles) animals at the baseline (n = 4) and various other time points (n = 2) determined by MRI analyses of ex vivo lung specimens; (C) lymph node enlargement in treated (solid squares) versus control (solid triangles) animals at various time points determined by MRI analyses of ex vivo lung specimens. PI, postinfection.
FIG. 3.
Comparative MRI scans of fixed lung specimens from control guinea pigs and guinea pigs receiving chemotherapy performed on days 29, 50, 78, 105, and 134 of infection. The images obtained by MRI show severe lung consolidation through 100 days postinfection in the control animals compared to the consolidation in the lungs of the animals receiving chemotherapy, which show minimal disease burden.
Progression of organ pathology.
Low-dose aerosol infection of guinea pigs produces multifocal to coalescing foci of granulomatous inflammation in the lungs, followed by extrapulmonary dissemination that can involve any organ of the body (3). As shown in this study, primary lesions with necrosis developed in the lungs and draining mediastinal lymph nodes within the first 30 days of infection (Fig. 4 and 5). In the control animals, the lesions progressed to involve all or most of the normal parenchyma, resulting in the death of the animal by day 125 of the infection. Initiation of treatment of the animals with INH, RIF, and PZA slowed the progression of disease in the lungs, as well as in the spleen (data not shown). Data summarizing the lesion areas relative to the area of more healthy tissue, including necrosis and the degree of calcification, are shown in Fig. 6.
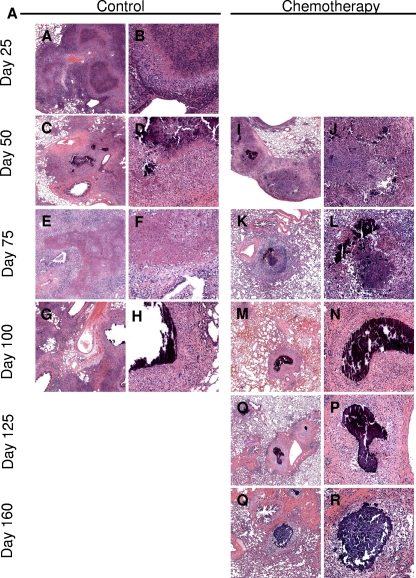
FIG. 4.
Combination drug therapy slows lesion progression in the lungs of M. tuberculosis-infected guinea pigs. Multifocal to coalescing foci of mixed inflammation efface the normal pulmonary architecture by 25 days of infection in control animals receiving sucrose alone (A and B). By day 50 (C, D, I, and J), lesions with central necrosis show evidence of healing by fibrosis and dystrophic calcification, which persists in the primary lesions throughout the course of infection in the control and the drug-treated animals. In the control animals, post-primary lesions efface the remainder of the parenchyma and develop a second phase of lytic necrosis (E and F) that also calcifies in drug-treated animals (K and L). In the drug-treated animals, the post-primary lesions resolve or are prevented from developing, leaving only well-organized calcified lesions that are often perivascular and peribronchial and that correspond to pulmonary lymphatics (M to R), while in the control animals (G and H), the lesions continue to progress to form larger areas of multifocal coalescing inflammation and mineralization that efface large areas of pulmonary parenchyma, resulting in reduced survival. Hematoxylin and eosin staining. Magnifications, ×10 (A to G and I to Q) and ×20 (B to H and J to R).
FIG. 5.
Combination drug therapy slows lesion progression in the mediastinal lymph nodes of M. tuberculosis-infected guinea pigs. Extensive foci of mixed inflammation with expansive foci of lytic necrosis efface the normal architecture of the mediastinal lymph nodes in carrier control animals treated with sucrose alone (A to H). By day 50 (A and B), there is partial resolution of the acute inflammation with extensive fibrosis and early evidence of dystrophic calcification of the necrotic lesions. In the late stages of infection (day 75 [E and F] and day 100 [G and H]), residual necrotic foci have incomplete calcification with active inflammation and a second phase of acute inflammation and necrosis. In contrast, lesion necrosis is limited and the lesions fail to progress in drug-treated animals but do progress in the control animals (I to R). Noncalcified lesion necrosis is evident at day 50 (I and J) of infection, but the necrosis heals by fibrosis and incomplete calcification by day 100 (M and N). In contrast to the findings for the control animals, a normal lymph node architecture is partially retained to day 160 (Q and R), by which time all control animals had died due to progressive disease. By day 160 (∼20 days after drug treatment was discontinued), lymph node lesions can again be found to have extensive necrosis that is delineated from the more normal lymph node parenchyma by a thick fibrous capsule. Hematoxylin and eosin staining. Magnifications: ×10 (A to G and I to Q) and ×20 (B to H and J to R).
FIG. 6.
Lesion scores from lungs, lymph nodes, and spleens from representative infected guinea pigs receiving chemotherapy at each time point. (A) Lesion scores of lungs, lymph nodes, and spleens for the control animals (C) and the drug-treated animals (D) on days 25, 50, 75, 100, 125 and 150 of infection. The pathology scores are the percentages of the areas of the lungs, lymph nodes, and spleens; and the results are expressed as the ratios of the pathology scores for each parameter. (B) A lung tissue specimen from an M. tuberculosis-infected guinea pig receiving chemotherapy for 125 days. A residual primary lung lesion is evidenced by central necrosis (C) (upper photograph) with dystrophic calcification. The lower photograph depicts the magnified region denoted by the square in the upper photograph showing persisting extracellular acid-fast-staining bacilli (arrows) within the central necrotic core of the primary lesion after treatment.
Collectively, the data shown in Fig. 4 to 6 show that therapy had little or no effect on primary lesions with necrosis in the lungs and lymph nodes (although treatment was more effective at preventing progressive inflammation and necrosis in the spleen; data not shown). In both the lungs and the lymph nodes, lesions with necrosis had incomplete dystrophic calcification, leaving residual necrosis with extensive fibrosis, despite drug therapy. Dystrophic mineralization or calcification is a pathological process associated with the intra- and extracellular deposition of mixed calcium salts at sites of tissue necrosis. Calcification is a progressive process, and if it is complete, it is considered, along with fibrosis, to be a favorable healing response. Even after day 160 of the infection, while the lungs were again mostly clear, some mineralized primary lesions still remained (Fig. 4Q and R). The significance of necrotic lesions with or without calcification is that these lesions harbor a population of persistent extracellular bacilli that can be visualized by acid-fast staining, as shown in Fig. 6B (30). Drug therapy was effective at preventing the development of nonnecrotic post-primary lesions in the lung but had little effect on the progression of lymph node lesions that were less extensive but that had residual necrosis with incomplete calcification (Fig. 5). In lesions that developed necrosis prior to the initiation of treatment, lesion progression was accompanied by healing by incomplete dystrophic calcification and fibrosis.
Flow cytometric analysis.
Using a recently described technique (39, 40), we evaluated the influx of T lymphocytes into the lungs and draining lymph nodes, as well as in the peripheral blood circulation, in the control and drug-treated guinea pigs. Figure 7 shows the total numbers of CD4 and CD8 cells in these target organs over the course of the study. The control animals showed static numbers of CD4 cells and increases in the numbers of CD8 cells in the lungs (Fig. 7A and D), decreases in the numbers in the lymph nodes (Fig. 7B and E), and increases in the numbers in blood (Fig. 7C and F). During drug treatment, the numbers of cells in the lung and lymph nodes dropped as the lesions were resolved, and upon the cessation of drug treatment (day 133), increases in the numbers of CD4 and CD8 T cells in the lungs and blood were noted. Interestingly, during the early course of chemotherapy (about day 50), increases in the numbers of CD4 and CD8 T cells in the lymph nodes were noted, after which they steadily declined.
FIG. 7.
CD4 and CD8 T-cell numbers in the lungs, lymph nodes, and blood of guinea pigs during chemotherapy. The numbers of CD4 and CD8 T cells in the lungs, lymph nodes, and blood collected on days 25, 50, 75, 100, 125, and 150 from guinea pigs infected with a low dose of M. tuberculosis Erdman K01 and receiving 40% sucrose treatment (solid squares) or chemotherapy (INH, PZA, and RIF; open squares) were compared. The results are expressed as the mean total number of cells in each tissue expressing CD4 or CD8 (n = 4) per 1.0 g of lung tissue in each group (± SEM).
The upregulation of CD45 (leukocyte common antigen) molecules on CD4 T cells indicates the transduction of antigen receptor signaling during the immune response, and hence, we used it in the present study as an indication of T-cell activation (39, 40). Whereas the control guinea pigs showed progressive increases in CD4 CD45hi T-cell numbers in both organs (Fig. 8A and B), as well as their blood (Fig. 8C), drug treatment rapidly prevented this in the lungs and the levels remained at the background level throughout (Fig. 8A). In contrast, despite therapy, the numbers of cells of the activated CD4 CD45hi T-cell subset increased in the draining lymph node through day 75, before they then fell. Interestingly, the levels of these cells slowly increased in the blood throughout the experiment.
FIG. 8.
Expression of activation markers and homing receptors on CD4 and CD8 T cells in the lungs, lymph nodes, and blood of guinea pigs during chemotherapy. The numbers of CD4 T cells expressing CD45 (A to C), the numbers of CD4 T cells expressing CT4 (D to F), and the numbers of CD8 T cells expressing CT4 cells (G to I) in the lungs, lymph nodes, and blood collected on days 25, 50, 75, 100, 125, and 150 from guinea pigs infected with a low dose of M. tuberculosis Erdman K01 and receiving 40% sucrose treatment (solid squares) or chemotherapy (INH, PZA, and RIF; open squares) were compared. The results are expressed as the average total number of cells expressing CD4 CD45, CD4 CT4, or CD8 CT4 (n = 4) per 1.0 g of each tissue in each group (± SEM).
In addition, we also assessed the levels of the selectin-like homing receptor CT4 on both CD4 and CD8 T cells accumulating in the lungs (Fig. 8D), lymph nodes (Fig. 8E), and blood (Fig. 8F). Figure 8D and E and G to I shows increased numbers of CT4+ cells on both CD4 and CD8 T cells in untreated control guinea pigs over the course of the infection. This was not seen on T cells harvested from the lungs of the drug-treated animals, but the CT4+ levels on cells harvested from the lymph nodes rose and then fell again. Similarly, the blood levels of such cells remained static.
Influx of other leukocyte populations.
In addition to the T-cell response, we also tracked the influx of MHC class II-positive macrophages into the lungs, lymph nodes, and blood. The levels of these macrophages increased progressively in untreated animals but remained at low levels in guinea pigs receiving drug therapy (Fig. 9A to C). Similar increases in B-lymphocyte levels were also seen in control animals (Fig. 9D to F), consistent with our earlier observations (40). MIL4+ granulocytes were also detected (Fig. 9 G to I); the levels of these cells began to rise sharply after 40 to 50 days as the lesions became necrotic, but their influx was prevented by the effects of the chemotherapy.
FIG. 9.
MHC class II expression on MR-1 macrophages, B cells, and granulocytes in the lungs, lymph nodes, and blood of guinea pigs during chemotherapy. The numbers of MR-1 macrophages expressing MHC class II (A to C), the numbers of B cells (D to F), and the numbers of MIL4+ granulocytes (G to I) in the lungs, lymph nodes, and blood collected on days 25, 50, 75, 100, 125, and 150 from guinea pigs infected with a low dose of M. tuberculosis Erdman K01 and receiving 40% sucrose treatment (solid squares) or chemotherapy (INH, PZA, and RIF; open squares) were compared. The results are expressed as the average numbers of cells in the lung, lymph node, and blood expressing MHV class II on MR-1 macrophages, B cells, and MIL4+ granulocytes (n = 4) per 1.0 g of tissue in each group (± SEM).
Differential expression of cytokine and regulatory T-cell responses.
We used RT-PCR to track the expression of several cytokines in each target organ over the course of the experiment. The TH1 cytokines IFN-γ, IL-12, and TNF-α were each relatively poorly expressed in the control guinea pigs, although the TNF-α levels spiked shortly before their death (Fig. 10A to C). In the treated groups, the levels of IFN-γ rose sharply up to day 125, indicating that the drug treatment allowed the expression of a sustained TH1 response, and upon the cessation of chemotherapy, the levels of the TH1 cytokines dropped. Similar kinetics were also observed for IL-12 and TNF-α. We then compared the profiles of these cytokines to those of three other cytokines more associated with downregulation and/or the control of inflammation. We observed that the TGF-β responses remained lower, although some TGF-β expression was seen and peaked on day 125, and IL-10 responses were also kept at a minimum by the chemotherapy (Fig. 10D and E). The expression of Foxp3, a marker for regulatory T cells, increased sharply in the lungs of the Erdman K01-infected control guinea pigs (Fig. 10F) but was not detected in the drug-treated animals.
FIG. 10.
Cytokine mRNA expression in guinea pig lung cells during chemotherapy. The levels of expression of mRNA for IFN-γ (A), IL-12p40 (B), TNF-α (C), TGF-β (D), IL-10 (E), and Foxp3 (F) in the lung tissues collected on days 25, 50, 100, 125, and 150 from guinea pigs receiving 40% sucrose treatment (solid squares) or chemotherapy (INH, PZA, and RIF; open squares) were compared. Cytokine mRNA expression was quantified by real-time reverse transcription-PCR. The fold induction of mRNA was calculated from the CT values normalized to the CT values for HPRT and then to the values for uninfected guinea pig lung cells. The results are expressed as the average (n = 4) of the fold induction in each group (± SEM).
DISCUSSION
Most studies that test the activities of conventional or new antituberculosis drugs in animals evaluate the responses to treatment primarily on the basis of the differences in tissue bacterial loads but rarely on the basis of other parameters. In this study, we achieved three important goals. First, we performed a comprehensive evaluation of the host response to drug therapy in the guinea pig model, in which the guinea pigs develop primary lesions with necrosis similar to those that develop in naturally occurring infections in humans. Unlike conventional mouse models of tuberculosis, immunologically naïve guinea pigs develop a variety of lesion types, including primary lesions with necrosis, that are relatively unaffected by combination drug therapy. In addition, we quantified the response to drug therapy using advanced imaging methods, and the findings obtained by those methods were validated by gross necropsy and histologic evaluation at the time of necropsy. Finally, in this study, we correlated the resolution of pulmonary and extrapulmonary inflammation in response to combination drug therapy with the temporal changes in tissue and circulating inflammatory cell phenotypes and cytokine levels as a measure of acquired immunity.
The results of this study show that conventional chemotherapy with INH, RIF, and PZA rapidly reduced the bacterial burden and the resulting pulmonary and extrapulmonary inflammation induced by strain Erdman K01, a highly virulent strain of M. tuberculosis, with most of the bacilli being eliminated within the first month of treatment. Despite the rapid killing, small numbers of drug-tolerant bacteria could still be recovered in lung and other tissue homogenates after 3 to 4 months of treatment. The ability to culture low numbers of bacilli even following drug therapy correlated with the presence of persistent lesions, especially partially healed primary lesions. Resolution of the majority of the granulomatous lesions in the lungs could be clearly visualized by magnetic resonance imaging at the macroscopic level. In terms of the host immune response, drug treatment reduced the influx of activated T lymphocytes into the lungs and blood and yet seemed to rescue the TH1 response in terms of cytokine expression. The level of TH1 cytokine expression was increased well into the course of chemotherapy, and upon its cessation the TH1 cytokine responses declined. This was associated with increases in the numbers of CD4 and CD8 T cells, whose numbers also steadily decreased after day 50 or so. Other reductions in the numbers of activated macrophages, B lymphocytes, and, perhaps most importantly, granulocytes were seen. An additional important observation was that chemotherapy prevented the emergence of high levels of IL-10 and the expression of Foxp3, known markers of regulatory T lymphocytes. Collectively, these observations illustrate the complexity of the host response in the guinea pig that likely contributes to the control of M. tuberculosis infection in the face of combination drug therapy.
In terms of reductions in the bacterial loads, the results presented here reflect the response to drug therapy seen in mice and humans, which is a biphasic response consisting of rapid killing initially and then delayed and incomplete clearance from tissue (30). The first stage is generally thought to represent the rapidly sterilizing activity of INH, RIF, and PZA treatment against replicating bacilli (9, 35), but a thorough explanation for the second phase remains elusive. One possible explanation is that the residual bacteria are drug tolerant and are cleared less effectively because a minor population has switched to a nonreplicating state or bacilli have spontaneous mutations that render them drug resistant (20).
The central practical issue here, however, is whether a particular regimen is sterilizing, defined as complete eradication of the infection and, thus, there is no potential for disease relapse (21). In conventional methods for determining the colony counts in tissues with confidence, particularly tissues containing low numbers of bacilli, the entire organ must be available for plating of undiluted tissue homogenates. Interpretation of the results for such homogenates on solid agar may be subject to error, since incomplete homogenization may not adequately disperse aggregates of bacilli. This factor, combined with the poor recovery of difficult-to-culture bacilli, can lead to an underestimate of the numbers of CFU, particularly when bacilli are present in low numbers. Because of this limitation, one can argue that estimates of the numbers of CFU when bacilli are present at low numbers may be statistically underpowered (29). This may be further complicated by new evidence that M. tuberculosis can enter a biofilm-like state (37); thus, it may not grow planktonically and therefore not form measurable colonies on agar.
There is an increasing interest in the application of advanced imaging techniques to evaluate the effects of chemotherapy (12). We have previously obtained ex vivo magnetic resonance images to monitor changes in lesion numbers and size in M. bovis BCG-vaccinated and nonvaccinated guinea pigs infected with M. tuberculosis (28). Because MRI under biosafety level 3 containment is not yet available, we are limited to test the proof of principle with specimens that have been fixed by perfusion and in which the bacilli have been inactivated. Nonetheless, these data accurately reflect the whole-lung lesion burden, as validated histologically, and in addition provide a three-dimensional appreciation of the lesion distribution. Thus, the data obtained by imaging techniques can provide a useful adjunct to the data obtained by more traditional methods. In vivo MRI is expected to provide a sensitive means of monitoring the progression and resolution of lung granulomas and lymphadenomegaly due to its excellent inherent ability to provide contrast for soft tissue and the recent technological advances that now enable ultrafast thoracic imaging as a means of noninvasive longitudinal monitoring of vaccine and treatment efficacy.
A major advantage of the use of the guinea pig as a model of human tuberculosis is the consistent development of primary lesions with central caseous necrosis, similar to one of the morphological features of the naturally occurring disease in humans (3, 32, 33, 36). In this regard, it can be argued that the efficacy of a given chemotherapeutic regimen is a reflection of its capacity to resolve this important lesion type. Our results presented here demonstrate that while treatment with INH, RIF, and PZA effectively clears lymphocytic nonnecrotizing secondary lung lesions, even aggressive combination chemotherapy did not completely resolve primary lesions with necrosis. We hypothesize that the association of extracellular bacilli with the necrotic host debris in primary lesions represents a barrier to the cellular immune response and drug therapy. We further suggest that the biological significance of these persisting populations resides in evidence that after sterilizing drug therapy, secondary lesions which never form necrosis are cured and devoid of acid-fast-staining bacilli, while primary lesions which contain necrosis are a potential source of reactivation disease in the guinea pig model. We propose that specific quantification of residual lesions by the methods described here could provide a specific measure of the efficacies of new drug regimens in this relevant small-animal model.
One of the most intriguing findings of the current studies was that the residual primary lesions that existed following combination drug therapy were those associated with pulmonary lymphatic vessels. We subsequently demonstrated that this is a consistent finding (4) in guinea pigs infected by use of a low-dose aerosol, a model that closely mimics the natural route of infection in humans. We previously noted that granulomatous inflammation of the lymphatics results in segmental blockage and is a previously unappreciated but major element of the disease in the context of persistence (3). Given the structural nature of these vessels, which are embedded in the perivascular and peribronchial connective tissue matrix, persisting bacilli not only could be trapped inside these lesions but also could be trapped there for decades in humans because of the poor vascularity and relative isolation from the functional pulmonary parenchyma. The significance of this lesion in the naturally occurring disease in humans is still not fully appreciated but is suggested by recent three-dimensional reconstructions of lesions from patients that show a distinct tubular morphology consistent with lymphangitis (C. Barry, personal communication).
To date, the effects of the removal of the infection by chemotherapy on the immunological status of the animal has not been addressed, not even in the widely used mouse model, yet this seems to be very important, because the status of the T-cell response not only should be expected to influence the rate of clearance of the infection but also should have obvious consequences if residual bacilli begin to reactivate and produce antigen. In the current study, we monitored the status of the immune response in the lungs during the course of the infection using a newly developed flow cytometry protocol (40) and RT-PCR. Our results show that by reversing the progression of disease in the lung and blood with chemotherapy, the chemotactic stimulus for activated T cells and macrophages was reduced during the early and chronic stages of disease, consistent with the histopathology evidence. Interestingly, during the early stage of drug treatment, increased numbers of activated T cells migrated into the lymph nodes and then declined thereafter. We have previously shown (3, 6) that during subacute infection in control animals the lymph node tissue is destroyed and that it is likely that antigen presentation is therefore hindered. During the beginning of chemotherapy, bacterial death and antigen release occur, and so the early increase in the numbers of T cells in the lymph nodes may represent resumed antigen presentation permitted by organ tissue healing. In addition, and importantly, the influx of MIL4+ granulocytes, which is strongly associated with the appearance of necrosis (40), was completely prevented. Despite the apparent dampening of acquired immunity, we observed significant increases in the levels of the TH1-associated cytokines IFN-γ, IL-12, and TNF-α using RT-PCR. A recent report demonstrated that PZA treatment of murine cutaneous leishmaniasis results in a 100-fold reduction in the parasite burden and increased macrophage activation and TH1 cytokine levels (34). It is apparent from the findings of our studies that the cessation of chemotherapy, including PZA therapy, resulted in a decline in TH1 immunity, supporting the findings of that recent study. Overall, this seems to suggest that destruction of the bacilli provides a substantial source of antigens that allows expansion of TH1 immunity, something that we previously demonstrated (40) was lost in the lungs of untreated animals after about day 30 of the infection. This establishment of this T-cell response should conceivably involve an element of memory immunity and thus affect the ability of the host to respond to reactivation or secondary exogenous reexposure.
Many M. tuberculosis strains of high virulence, including the Erdman K01 strain, are potent inducers of CD4+ CD25hi Foxp3+ regulatory T cells (38). We demonstrate here that chemotherapy negated the expression of Foxp3+ regulatory T cells and IL-10 in the lungs of treated guinea pigs. The role of regulatory T cells in tuberculosis may be associated with a reduction in the level of pulmonary inflammation, as previously demonstrated in the mouse model (38). Therefore, the removal of pulmonary inflammation by chemotherapy may significantly reduce the involvement of regulatory T cells, which may be an obvious benefit.
Finally, this study presented us with some serious challenges in animal husbandry, none of which were trivial. In addition to their intrinsic susceptibility to tuberculosis, guinea pigs are easily stressed. Because of this, we believed that it was important to avoid as far as possible any degree of restraint or forced drug feeding. Guinea pigs are easily conditioned, however, and we were able to acclimate the animals to gentle handling and voluntary feeding via a pipette. Two major additional problems, however, were (i) that at about 2 weeks after infection, the animals started to develop fevers, and (ii) once the drugs were introduced into the 40% sucrose delivery vehicle, one could soon notice both behavioral and physical issues probably related to the toxic effects of the drugs on the normal gastrointestinal flora. The primary consequence of this was that the guinea pigs became lethargic and had reduced feed intake. We were able to very successfully alleviate these problems by gently feeding the animals a mixture of drugs given in sucrose to mask the taste, a highly nutritious vegetable puree, a Lactobacillus preparation, and a vitamin C supplement. The animals readily ingested this formulation without any need for forced feeding or restraint.
In summary, in the present study, the guinea pig was shown to be a potentially useful model for evaluation of the effects of chemotherapy on the important necrotic lesion types that are seen in humans with naturally occurring disease. We have developed a number of ways to monitor both the efficacy and the effects of chemotherapy which could give important new information not only about the efficacy of the drug itself but also about how the host response adapts at both the pathological and the immunological levels. Moreover, given the extreme pathology caused by newly emerging strains of M. tuberculosis, including W-Beijing and multidrug-resistant isolates, recently demonstrated (41) in this model, we propose that guinea pigs be used to evaluate new regimens addressing these serious developments in the clinical field.
Acknowledgments
This study was supported by a generous grant from the Bill and Melinda Gates Foundation.
We thank Charles Peloquin for his help with performing the pharmacokinetic and pharmacodynamic determinations to identify the correct drug doses in vivo.
Footnotes
Published ahead of print on 16 February 2010.
REFERENCES
- 1.Allen, S. S., and D. N. McMurray. 2003. Coordinate cytokine gene expression in vivo following induction of tuberculous pleurisy in guinea pigs. Infect. Immun. 71:4271-4277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aziz, M. A., A. Wright, A. Laszlo, A. De Muynck, F. Portaels, A. Van Deun, C. Wells, P. Nunn, L. Blanc, and M. Raviglione. 2006. Epidemiology of antituberculosis drug resistance (the Global Project on Anti-Tuberculosis Drug Resistance Surveillance): an updated analysis. Lancet 368:2142-2154. [DOI] [PubMed] [Google Scholar]
- 3.Basaraba, R. J. 2008. Experimental tuberculosis: the role of comparative pathology in the discovery of improved tuberculosis treatment strategies. Tuberculosis (Edinb.) 88(Suppl. 1):S35-S47. [DOI] [PubMed] [Google Scholar]
- 4.Basaraba, R. J., D. D. Dailey, C. T. McFarland, C. A. Shanley, E. E. Smith, D. N. McMurray, and I. M. Orme. 2006. Lymphadenitis as a major element of disease in the guinea pig model of tuberculosis. Tuberculosis (Edinb.) 86:386-394. [DOI] [PubMed] [Google Scholar]
- 5.Basaraba, R. J., A. A. Izzo, L. Brandt, and I. M. Orme. 2006. Decreased survival of guinea pigs infected with Mycobacterium tuberculosis after multiple BCG vaccinations. Vaccine 24:280-286. [DOI] [PubMed] [Google Scholar]
- 6.Basaraba, R. J., E. E. Smith, C. A. Shanley, and I. M. Orme. 2006. Pulmonary lymphatics are primary sites of Mycobacterium tuberculosis infection in guinea pigs infected by aerosol. Infect. Immun. 74:5397-5401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Basu, S., and A. P. Galvani. 2007. Extensively drug-resistant tuberculosis in South Africa. Lancet 369:272-273. [DOI] [PubMed] [Google Scholar]
- 8.Bifani, P., B. Mathema, N. Kurepina, E. Shashkina, J. Bertout, A. S. Blanchis, S. Moghazeh, J. Driscoll, B. Gicquel, R. Frothingham, and B. N. Kreiswirth. 2008. The evolution of drug resistance in Mycobacterium tuberculosis: from a mono-rifampin-resistant cluster into increasingly multidrug-resistant variants in an HIV-seropositive population. J. Infect. Dis. 198:90-94. [DOI] [PubMed] [Google Scholar]
- 9.Botha, F. J., F. A. Sirgel, D. P. Parkin, B. W. van de Wal, P. R. Donald, and D. A. Mitchison. 1996. Early bactericidal activity of ethambutol, pyrazinamide and the fixed combination of isoniazid, rifampicin and pyrazinamide (Rifater) in patients with pulmonary tuberculosis. S. Afr. Med. J. 86:155-158. [PubMed] [Google Scholar]
- 10.Cho, H., T. M. Lasco, S. S. Allen, T. Yoshimura, and D. N. McMurray. 2005. Recombinant guinea pig tumor necrosis factor alpha stimulates the expression of interleukin-12 and the inhibition of Mycobacterium tuberculosis growth in macrophages. Infect. Immun. 73:1367-1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cohen, T., C. Colijn, A. Wright, M. Zignol, A. Pym, and M. Murray. 2008. Challenges in estimating the total burden of drug-resistant tuberculosis. Am. J. Respir. Crit. Care Med. 177:1302-1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davis, S. L., E. L. Nuermberger, P. Um, C. Vidal, B. Jedynak, M. G. Pomper, W. R. Bishai, and S. K. Jain. 2009. Noninvasive pulmonary [18F]-2-fluoro-deoxy-d-glucose positron emission tomography correlates with bactericidal activity of tuberculosis drug treatment. Antimicrob. Agents Chemother. 53:4879-4884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dye, C. 2006. Global epidemiology of tuberculosis. Lancet 367:938-940. [DOI] [PubMed] [Google Scholar]
- 14.Dye, C., D. Maher, D. Weil, M. Espinal, and M. Raviglione. 2006. Targets for global tuberculosis control. Int. J. Tuber. Lung Dis. 10:460-462. [PubMed] [Google Scholar]
- 15.Dye, C., C. J. Watt, D. M. Bleed, S. M. Hosseini, and M. C. Raviglione. 2005. Evolution of tuberculosis control and prospects for reducing tuberculosis incidence, prevalence, and deaths globally. JAMA 293:2767-2775. [DOI] [PubMed] [Google Scholar]
- 16.Espinal, M. A., and C. Dye. 2005. Can DOTS control multidrug-resistant tuberculosis? Lancet 365:1206-1209. [DOI] [PubMed] [Google Scholar]
- 17.Gandhi, N. R., A. Moll, A. W. Sturm, R. Pawinski, T. Govender, U. Lalloo, K. Zeller, J. Andrews, and G. Friedland. 2006. Extensively drug-resistant tuberculosis as a cause of death in patients co-infected with tuberculosis and HIV in a rural area of South Africa. Lancet 368:1575-1580. [DOI] [PubMed] [Google Scholar]
- 18.Ginsberg, A. M., and M. Spigelman. 2007. Challenges in tuberculosis drug research and development. Nat. Med. 13:290-294. [DOI] [PubMed] [Google Scholar]
- 19.Githui, W. A. 2006. Multi drug resistant tuberculosis. East Afr. Med. J. 83:585-587. [PubMed] [Google Scholar]
- 20.Gomez, J. E., and J. D. McKinney. 2004. M. tuberculosis persistence, latency, and drug tolerance. Tuberculosis (Edinb.) 84:29-44. [DOI] [PubMed] [Google Scholar]
- 21.Grosset, J. 1978. The sterilizing value of rifampicin and pyrazinamide in experimental short-course chemotherapy. Bull. Int. Union Tuberc. 53:5-12. [PubMed] [Google Scholar]
- 22.Harries, A. D., and C. Dye. 2006. Tuberculosis. Ann. Trop. Med. Parasitol. 100:415-431. [DOI] [PubMed] [Google Scholar]
- 23.Hart, I. J., H. Schafer, R. J. Scheper, and G. T. Stevenson. 1992. Subpopulations of guinea-pig T lymphocytes defined by isoforms of the leucocyte common antigen. Immunology 77:377-384. [PMC free article] [PubMed] [Google Scholar]
- 24.Haverson, K., M. Bailey, V. R. Higgins, P. W. Bland, and C. R. Stokes. 1994. Characterization of monoclonal antibodies specific for monocytes, macrophages and granulocytes from porcine peripheral blood and mucosal tissues. J. Immunol. Methods 170:233-245. [DOI] [PubMed] [Google Scholar]
- 25.Hiromatsu, K., C. C. Dascher, M. Sugita, C. Gingrich-Baker, S. M. Behar, K. P. LeClair, M. B. Brenner, and S. A. Porcelli. 2002. Characterization of guinea-pig group 1 CD1 proteins. Immunology 106:159-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoff, D. R., M. L. Caraway, E. J. Brooks, E. R. Driver, G. J. Ryan, C. A. Peloquin, I. M. Orme, R. J. Basaraba, and A. J. Lenaerts. 2008. Metronidazole lacks antibacterial activity in guinea pigs infected with Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 52:4137-4140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kraal, G., R. Shiamatey-Koolma, M. Hoffer, D. Baker, and R. Scheper. 1988. Histochemical identification of guinea-pig macrophages by monoclonal antibody MR-1. Immunology 65:523-528. [PMC free article] [PubMed] [Google Scholar]
- 28.Kraft, S. L., D. Dailey, M. Kovach, K. L. Stasiak, J. Bennett, C. T. McFarland, D. N. McMurray, A. A. Izzo, I. M. Orme, and R. J. Basaraba. 2004. Magnetic resonance imaging of pulmonary lesions in guinea pigs infected with Mycobacterium tuberculosis. Infect. Immun. 72:5963-5971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lenaerts, A. J., P. L. Chapman, and I. M. Orme. 2004. Statistical limitations to the Cornell model of latent tuberculosis infection for the study of relapse rates. Tuberculosis (Edinb.) 84:361-364. [DOI] [PubMed] [Google Scholar]
- 30.Lenaerts, A. J., M. A. Degroote, and I. M. Orme. 2008. Preclinical testing of new drugs for tuberculosis: current challenges. Trends Microbiol. 16:48-54. [DOI] [PubMed] [Google Scholar]
- 31.Lenaerts, A. J., D. Hoff, S. Aly, S. Ehlers, K. Andries, L. Cantarero, I. M. Orme, and R. J. Basaraba. 2007. Location of persisting mycobacteria in a guinea pig model of tuberculosis revealed by r207910. Antimicrob. Agents Chemother. 51:3338-3345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McMurray, D. N. 2001. Disease model: pulmonary tuberculosis. Trends Mol. Med. 7:135-137. [DOI] [PubMed] [Google Scholar]
- 33.McMurray, D. N., S. S. Allen, A. Jeevan, T. Lasco, H. Cho, T. Skwor, T. Yamamoto, C. McFarland, and T. Yoshimura. 2005. Vaccine-induced cytokine responses in a guinea pig model of pulmonary tuberculosis. Tuberculosis (Edinb.) 85:295-301. [DOI] [PubMed] [Google Scholar]
- 34.Mendez, S., R. Traslavina, M. Hinchman, L. Huang, P. Green, M. H. Cynamon, and J. T. Welch. 2009. The antituberculosis drug pyrazinamide affects the course of cutaneous leishmaniasis in vivo and increases activation of macrophages and dendritic cells. Antimicrob. Agents Chemother. 53:5114-5121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mitchison, D. A. 1996. Pyrazinamide—on the antituberculosis drug frontline. Nat. Med. 2:635-636. [DOI] [PubMed] [Google Scholar]
- 36.Mitsuyama, M., and D. N. McMurray. 2007. Tuberculosis: vaccine and drug development. Tuberculosis (Edinb.) 87(Suppl. 1):S10-S13. [DOI] [PubMed] [Google Scholar]
- 37.Ojha, A. K., A. D. Baughn, D. Sambandan, T. Hsu, X. Trivelli, Y. Guerardel, A. Alahari, L. Kremer, W. R. Jacobs, Jr., and G. F. Hatfull. 2008. Growth of Mycobacterium tuberculosis biofilms containing free mycolic acids and harbouring drug-tolerant bacteria. Mol. Microbiol. 69:164-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ordway, D., M. Henao-Tamayo, M. Harton, G. Palanisamy, J. Troudt, C. Shanley, R. J. Basaraba, and I. M. Orme. 2007. The hypervirulent Mycobacterium tuberculosis strain HN878 induces a potent TH1 response followed by rapid down-regulation. J. Immunol. 179:522-531. [DOI] [PubMed] [Google Scholar]
- 39.Ordway, D., M. Henao-Tamayo, C. Shanley, E. E. Smith, G. Palanisamy, B. Wang, R. J. Basaraba, and I. M. Orme. 2008. Influence of Mycobacterium bovis BCG vaccination on cellular immune response of guinea pigs challenged with Mycobacterium tuberculosis. Clin. Vaccine Immunol. 15:1248-1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ordway, D., G. Palanisamy, M. Henao-Tamayo, E. E. Smith, C. Shanley, I. M. Orme, and R. J. Basaraba. 2007. The cellular immune response to Mycobacterium tuberculosis infection in the guinea pig. J. Immunol. 179:2532-2541. [DOI] [PubMed] [Google Scholar]
- 41.Palanisamy, G. S., N. DuTeau, K. D. Eisenach, D. M. Cave, S. A. Theus, B. N. Kreiswirth, R. J. Basaraba, and I. M. Orme. 2009. Clinical strains of Mycobacterium tuberculosis display a wide range of virulence in guinea pigs. Tuberculosis (Edinb.) 89:203-209. [DOI] [PubMed] [Google Scholar]
- 42.Spigelman, M., and S. Gillespie. 2006. Tuberculosis drug development pipeline: progress and hope. Lancet 367:945-947. [DOI] [PubMed] [Google Scholar]
- 43.Spigelman, M. K. 2007. New tuberculosis therapeutics: a growing pipeline. J. Infect. Dis. 196(Suppl. 1):S28-S34. [DOI] [PubMed] [Google Scholar]
- 44.Takizawa, M., J. Chiba, S. Haga, T. Asano, T. Yamazaki, N. Yamamoto, and M. Honda. 2006. Novel two-parameter flow cytometry (MIL4/SSC followed by MIL4/CT7) allows for identification of five fractions of guinea pig leukocytes in peripheral blood and lymphoid organs. J. Immunol. Methods 311:47-56. [DOI] [PubMed] [Google Scholar]
- 45.Tan, B. T., F. Ekelaar, J. Luirink, G. Rimmelzwaan, A. J. De Jonge, and R. J. Scheper. 1985. Production of monoclonal antibodies defining guinea pig T-cell surface markers and a strain 13 Ia-like antigen: the value of immunohistological screening. Hybridoma 4:115-124. [DOI] [PubMed] [Google Scholar]
- 46.Wilcox, C. E., D. Baker, C. Butter, D. A. Willoughby, and J. L. Turk. 1989. Differential expression of guinea pig class II major histocompatibility complex antigens on vascular endothelial cells in vitro and in experimental allergic encephalomyelitis. Cell. Immunol. 120:82-91. [DOI] [PubMed] [Google Scholar]