Abstract
Human influenza is a seasonal disease associated with significant morbidity and mortality. Influenza vaccination is the most effective means for disease prevention. We have previously shown that mutations in the PB1 and PB2 genes of the live-attenuated influenza vaccine (LAIV) from the cold-adapted (ca) influenza virus A/Ann Arbor/6/60 (H2N2) could be transferred to avian influenza viruses and produce partially attenuated viruses. We also demonstrated that avian influenza viruses carrying the PB1 and PB2 mutations could be further attenuated by stably introducing a hemagglutinin (HA) epitope tag in the PB1 gene. In this work, we wanted to determine whether these modifications would also result in attenuation of a so-called triple reassortant (TR) swine influenza virus (SIV). Thus, the TR influenza A/swine/Wisconsin/14094/99 (H3N2) virus was generated by reverse genetics and subsequently mutated in the PB1 and PB2 genes. Here we show that a combination of mutations in this TR backbone results in an attenuated virus in vitro and in vivo. Furthermore, we show the potential of our TR backbone as a vaccine that provides protection against the 2009 swine-origin pandemic influenza H1N1 virus (S-OIV) when carrying the surface of a classical swine strain. We propose that the availability of alternative backbones to the conventional ca A/Ann Arbor/6/60 LAIV strain could also be useful in epidemic and pandemic influenza and should be considered for influenza vaccine development. In addition, our data provide evidence that the use of these alternative backbones could potentially circumvent the effects of original antigenic sin (OAS) in certain circumstances.
During the 20th century, humans confronted 3 influenza pandemics: the “Spanish flu” in 1918 (H1N1), the “Asian flu” in 1957 (H2N2), and the “Hong Kong flu” in 1968 (H3N2) (5). The current dogma, supported by phylogenetic analysis, indicates that the 1918 pandemic virus was of avian origin (31), whereas the other two pandemic viruses were generated by reassortment with previously circulating human strains. These pandemic strains were the result of the introduction of a new hemagglutinin (HA) subtype not previously seen by humans. In each instance, the pandemic virus also resulted in the eradication of the previous seasonal strain, and thus, epidemics in humans were characterized by the presence of a single type A influenza virus. However, in 1977, the H1N1 virus that was circulating until 1957 was reintroduced into the human population (23). The reemerged H1N1, dubbed the “Russian flu,” has since been cocirculating with H3N2 viruses.
In 2009, a new pandemic strain emerged (24) and has become prevalent in the human population. Interestingly, the 2009 pandemic virus does not contain a new HA subtype but contains an antigenically divergent H1 variant. The new pandemic virus is an H1N1 of swine origin (swine-origin pandemic influenza H1N1 virus [S-OIV]) (27). Pigs have always been considered potential mixing vessels where influenza viruses of avian, swine, and human origins can reassort and generate new viruses (21). In North America, H1N1 viruses, known as classical swine H1N1 influenza viruses (cH1N1), have circulated in pigs (since perhaps 1918) until 1998, with minimal antigenic drift (33). However, this scenario changed completely in 1998 with the emergence of triple reassortant (TR) viruses carrying genes from human, avian, and swine influenza strains. More importantly, TR viruses have been rather promiscuous, generating in less than a decade at least 6 different antigenically distinct influenza strains that cocirculate in pigs in North America (33). Most of the successful swine influenza viruses (SIV) that have become endemic in the U.S. pig population contain the triple reassortant internal gene (TRIG) cassette consisting of the PA and PB2 genes from the North American avian influenza lineage, the NS, NP, and M genes from the classical swine influenza lineage, and the PB1 from a human influenza virus. Vincent et al. have suggested that the TRIG backbone could accept multiple HA and NA subtypes and would provide a selective advantage to swine viruses possessing such gene constellations (33). In fact, the new pandemic S-OIV H1N1 virus is a TR virus itself, although the M and NA genes are derived from an influenza virus of Eurasian origin (27). The HA gene of the S-OIV, one of the most important determinants of antigenicity and transmission, is a derivative of the classical HA gene (cH1N1) that has been circulating in pigs since at least 1930 (27).
Swine influenza is a disease similar to human influenza. Swine influenza virus (SIV) causes an acute respiratory disease in pigs, whose severity depends on many factors, including age, virus strain, and secondary infections (6). Swine are usually vaccinated against influenza to avoid morbidity. More importantly, in light of recent facts, flu swine vaccination could also be beneficial to prevent possible zoonosis, with pandemic consequences. The only available vaccines in the market for swine influenza are whole-killed virus vaccines. Prior to 1998, swine in the United States were vaccinated against cH1N1. With the introduction of the TR viruses, companies need to reformulate killed vaccines to include antigenically distinct strains. However, the constant evolving nature of these viruses and the emergence of novel reassortants with unique antigenic characteristics require constant reformulation, a situation similar to that with influenza vaccines in humans (18). Thus, the use of autogenous influenza vaccine formulations is a common practice in the swine industry in the United States.
Although live-attenuated influenza vaccines (LAIV) have been approved for humans, a similar approach is lacking for swine influenza. Therefore, we have developed a new generation of LAIV for SIV. For this purpose, we chose an H3N2 virus, belonging to cluster III, which along with cluster IV, has been one of the most prevalent influenza viruses in American swine herds (19, 20). By means of reverse genetics, this SIV was modified in the PB2 and PB1 genes, making it temperature sensitive. We examined the potential of these swine vaccine viruses in vitro and in vivo, using mice as animal models. In addition, we also used an avian influenza attenuated backbone previously developed in our lab (29) to compare both backbones as candidates for LAIV for SIV. Our studies suggest that alternative influenza backbones for the preparation of LAIV could be useful for influenza pandemic preparedness and seasonal influenza.
MATERIALS AND METHODS
Cells and viruses.
293T human embryonic kidney and Madin-Darby canine kidney (MDCK) cells were maintained as previously described (29). A/swine/Iowa/15/30 (H1N1) (Sw30) was obtained from the ATCC. A/swine/Wisconsin/14094/99 (H3N2) (Sw99) was kindly provided by Sagar Goyal, University of Minnesota, and A/guinea fowl/Hong Kong/WF10/99 (H9N2) (WF10) was a gift from Robert Webster, St. Jude Children's Research Hospital, Memphis, TN. A/California/04/09 (H1N1) (Ca04) was kindly obtained from the repository at the Centers for Disease Control and Prevention, Atlanta, GA. Viruses were grown in MDCK cells or 10-day-old embryonated eggs. The titers of stock viruses were measured by plaque assay on MDCK cells at 37°C or by the 50% egg infectious dose (EID50) as previously described (26). Experiments using the prototypic pandemic strain Ca04 were performed in an enhanced biosafety level 3 (BSL-3+) facility approved by the U.S. Department of Agriculture.
Cloning and generation of vaccine viruses by reverse genetics.
The eight genes of Sw99 virus were cloned using a set of universal primers as described previously (14). HA and NA from Sw30 were cloned in plasmid pDZ (11), a generous gift from D. Zamarin and P. Palese, Mount Sinai School of Medicine, New York, NY. These genes were engineered to contain an internal restriction site as a genetic tag (silent mutation), an ApaLI site at position 902 in HA, and an AseI site at position 829 in NA. The WF10 virus was cloned in a separate study (25). The thermosensitive (ts) mutations in the PB1 and PB2 genes from Sw99 were introduced by site-directed mutagenesis using a commercially available kit, the QuikChange II site-directed mutagenesis kit (Stratagene, La Jolla, CA). Primer sequences are available upon request. The PB1 gene of the Sw99 virus was further modified by subcloning the HA tag from the PB1 attenuated (att) gene of WF10 (29). Plasmids were sequenced using the 3100 Genetic Analyzer from Applied Biosystems (Foster City, CA). Viruses were recovered as described previously, with minor modifications (13). WF10 ts or att backbones were also used for the generation of vaccine viruses and were described previously (29). Rescued viruses were confirmed by sequencing analysis. Viral titers were determined by plaque assay on MDCK cells at 37°C or 35°C or by EID50.
Transient transfection and minigenome assay.
To test the transcription efficiency of the modified influenza virus polymerases at different temperatures, a minigenome assay was performed in 293T cells. Briefly, ambisense plasmids encoding wild-type (wt) or mutant versions of PB2 and PB1 along with wt versions of PA and NP were cotransfected together with the influenza virus replicon reporter plasmid pPOLI-GFP. The reporter plasmid pPOLI-GFP was constructed by inserting the green fluorescent protein (GFP) open reading frame (ORF) flanked by the noncoding regions of the NS gene of influenza A virus into the SapI site of the pPOLI vector (22) (a generous present from Adolfo García-Sastre). Briefly, 1 μg of each plasmid (∼5 μg) was mixed with 10 μl of TransIT-LT1 (Mirus, Madison, WI). After 45 min of incubation at room temperature (RT), the mixture was added over 80% confluent 293T cells seeded the day before in six-well plates. The transfections were set up at the following different temperatures: 33°C, 35°C, 37°C, and 39°C. At 36 h posttransfection, the cells expressing GFP were visualized by fluorescence microscopy, and photographs were obtained. Subsequently, the cells were treated with trypsin, centrifuged, and resuspended in 500 μl phosphate-buffered saline (PBS). A total of 100 μl of cell suspensions was plated on a 96-well plate to measure GFP intensity in a Victor3 multilabel counter model 1420 (PerkinElmer, Waltham, MA). Values were expressed as relative percentages to the maximum and minimum values of fluorescence units obtained in the samples.
Virus growth curves.
To analyze viral replication, confluent MDCK cells were infected at a multiplicity of infection (MOI) of 0.001 and incubated for different time periods at either 33°C, 35°C, 37°C, or 39°C in the presence of 1 μg/ml of l-(tosylamido-2-phenyl) ethyl chloromethyl ketone (TPCK)-trypsin (Sigma-Aldrich, Saint Louis, MO). Titers were expressed as the number of PFU per ml.
Western blot analysis.
Dishes (diameter, 22 mm) of confluent MDCK cells were mock infected or infected with Sw99, Sw99-rg-wt, Sw99-ts, or Sw99-att at an MOI of 2. The infections were done in parallel at 35°C and 39°C. At every 2 h postinfection (p.i.), cells were lysed in radioimmunoprecipitation assay (RIPA) buffer. Whole-cell lysates were subjected to Western blot analysis using anti-1-73NS1TX/98 (28).
Immunoprecipitation.
Confluent MDCK cells seeded in 22-mm dishes were infected with Sw99-att, Sw99-ts, or Sw99-rg-wt virus at an MOI of 2 at room temperature for 1 h. At 5 h p.i., cells were lysed in RIPA buffer (25 mM Tris-HCl at pH 7.6, 150 mM NaCl, 1% NP-40, 1% sodium deoxycholate, 0.1% sodium dodecyl sulfate [SDS]). Cell lysates were incubated at 4°C with anti-PR8 polyclonal antibody (which recognizes primarily the NP viral protein; a kind gift from Peter Palese) for 4 h. Protein G-Sepharose beads (GE Healthcare, Pittsburgh, PA) were added for 1 h, and immunoprecipitates were washed four times with RIPA buffer. The pellets containing the immunoprecipitates were boiled in Laemmli sample buffer (Bio-Rad, Hercules, CA) and subjected to SDS-PAGE (sodium dodecyl sulfate-polyacrylamide gel electrophoresis). The proteins were visualized by Coomassie blue staining as described previously (9).
Immunoprecipitation of metabolic labeled cells.
Confluent MDCK cells seeded in 22-mm dishes were infected with Sw99-att, Sw99-ts, or Sw99-rg-wt viruses at an MOI of 2 at room temperature for 1 h. Cells were incubated in the presence of 35S-Met-Cys in minimal essential medium (MEM) lacking Met-Cys for 5 h at 35°C or 39°C. Cells were lysed in RIPA buffer. Cell lysates were incubated at 4°C with anti-PR8 antibody for 4 h. Protein G-Sepharose beads were added for 1 h, and immunoprecipitates were washed four times with RIPA buffer. The immunoprecipitated pellets were boiled in Laemmli buffer and subjected to SDS-PAGE. Proteins were visualized by autoradiography.
MLD50.
Four-week-old female BALB/c or DBA/2 mice (NCI, Frederick, MD) were anesthetized with isoflurane before intranasal (i.n.) inoculation with 50 μl virus suspension. The 50% mouse lethal dose (MLD50) for Sw30 and Ca04 was calculated using groups of mice (n = 4) inoculated with various doses ranging from 101 to 106 PFU (Sw30) or 101 to 106 TCID50 (DBA/2) per mouse (see Table 2). Clinical signs, body weight, and mortality were monitored and recorded for 14 days. Animal studies using the pandemic Ca04 virus were conducted under animal biosafety level 3 (ABSL-3) conditions, with USDA approval. Studies performed with Sw30 were done in an ABSL-2 mouse facility. Animal studies were conducted according to protocols approved by the Institutional Animal Care and Use Committee of the University of Maryland, College Park, MD.
TABLE 2.
Titers of virus stocks and MLD50 of wild-type viruses in BALB/c and DBA/2 mice
| Virus | Stock titer | MLD50 of: |
|
|---|---|---|---|
| BALB/c mice | DBA/2 mice | ||
| Sw30 | 8 × 108 PFU/ml | 5 × 102 PFU | 102 PFU |
| Ca04 | 1.08 × 107 TCID50/ml | ≥5.4 × 106 TCID50 | 1.2 × 102 TCID50 |
Vaccination-challenge studies.
To evaluate the safety of the vaccine viruses (Table 1), groups of 12 or 13 mice were vaccinated i.n. with 106 PFU or 106 EID50 per 50 μl. Mock-vaccinated animals were inoculated with 50 μl PBS. All animals were anesthetized with isoflurane. Clinical signs, body weight, and mortality were monitored and recorded for 21 days. At 3 and 6 days postvaccination (dpv), two mice per group were sacrificed, and their lungs were collected and homogenized to measure viral titers. Lungs homogenates were prepared in 1 ml of PBS, and viral titers were determined by plaque assay on MDCK cells at 35°C or by EID50. At 20 or 21 days postvaccination, sera were collected for antibody titration. At 21 days postvaccination, mice were challenged with 100 MLD50 of Sw30 (homologous) or 20 MLD50 of Ca04 (heterologous). Clinical signs, body weight, and mortality were monitored and recorded for 14 days. At 3 and 6 days postchallenge (dpc), two mice per group were sacrificed, and their lungs were collected and homogenized to measure viral titers. Lung homogenates were prepared in 1 ml of PBS, and viral titers were determined by plaque assay with MDCK cells at 37°C.
TABLE 1.
Viruses used in the present study
| Virush | Acronym |
|---|---|
| A/Sw/WI/14094/99 | Sw99 |
| A/Sw/WI/14094/99-atta | Sw99-att |
| A/Sw/WI/14094/99-tsb | Sw99-ts |
| A/Sw/WI/14094/99-rg-wtc | Sw99-rg-wt |
| 6 Sw99-att: 2 H1N1 (Sw30)d | Sw-att |
| 6 Sw99-ts: 2 H1N1 (Sw30)e | Sw-ts |
| 6 WF10-att: 2 H1N1 (Sw30)f | WF-att |
| 6 WF10-ts: 2 H1N1 (Sw30)g | WF-ts |
| A/Sw/IA/15/30 | Sw30 |
| A/CA/04/09 | Ca04 |
Virus carries PB1 and PB2 mutations and HA tag in PB1.
Virus carries PB1 and PB2 mutations.
Wild-type A/Sw/WI/14094/99 generated by reverse genetics.
Recombinant virus carrying 6 internal genes from Sw99-att and the HA and NA surface genes from A/Sw/IA/15/30 (H1N1).
Recombinant virus carrying 6 internal genes from Sw99-ts and the HA and NA surface genes from A/Sw/IA/15/30 (H1N1).
Recombinant virus carrying 6 internal genes from A/guinea fowl/Hong Kong/WF10/99 (H9N2)-att (12) and the HA and NA surface genes from A/Sw/IA/15/30 (H1N1).
Recombinant virus carrying 6 internal genes from A/guinea fowl/Hong Kong/WF10/99 (H9N2)-ts (12) and the HA and NA surface genes from A/sw/IA/15/30 (H1N1).
Sw, swine; WI, Wisconsin; IA, Iowa; CA, California.
Serum passive transfer studies.
DBA/2 mice (n = 16) were vaccinated i.n. with 106 PFU of Sw-att. At 20 days postvaccination, mice were bled, and serum samples were pooled. A total of 150 μl of sera obtained from vaccinated mice was administered intraperitoneally (i.p.) to 12 naïve DBA/2 mice. Four random mice were bled the next day to determine the level of hemagglutination inhibition (HI) antibodies in blood samples. Six mice from the passive vaccinated serum transfer were challenged with 100 MLD50 of Sw30 (homologous). The remaining six mice were challenged under ABSL-3 conditions with 20 MLD50 of Ca04 (heterologous). Challenges were done 24 h after passive transfer of sera. At 3 days postchallenge, two mice per group were sacrificed, and their lungs were collected and homogenized to measure viral titers. Lung homogenates were prepared in 1 ml PBS, and viral titers were determined by plaque assay with MDCK cells at 37°C.
HI assay.
Serum samples were collected 20 or 21 days postvaccination (dpv) and 14 days postchallenge (dpc). The anti-viral antibody titers were evaluated using the hemagglutination inhibition (HI) assay described in the WHO Manual on Animal Influenza Diagnosis and Surveillance (WHO/CDS/CSR/NCS/2002.5 Rev.1 [http://www.who.int/vaccine_research/diseases/influenza/WHO_manual_on_animal-diagnosis_and_surveillance_2002_5.pdf]). HI assays were performed using homologous and heterologous viruses with chicken (Sw30) or turkey (Ca04) red blood cells before and after challenge.
RESULTS
Genetic modifications in the PB2 and PB1 genes of a TRIG SIV strain result in impaired polymerase activity at restrictive temperatures.
The mutations responsible for the ts phenotype in the LAIV A/Ann Arbor/6/60 influenza virus strain have been mapped to the following 5 amino acids in the viral polymerases: N265S in PB2, K391E, E581G, and A661T in PB1, and D34G in NP (15). We have shown that these mutations can be transferred to avian influenza virus strains and generate a similar ts phenotype (29). However, these mutations were not sufficient to confer an attenuated phenotype in vivo; thus, the avian influenza virus backbone was further modified by introducing an HA epitope tag in the C-terminal end of PB1 (29). Viruses carrying the combination of ts and HA tag mutations are highly stable in vitro and in vivo and are referred to throughout the text as att viruses.
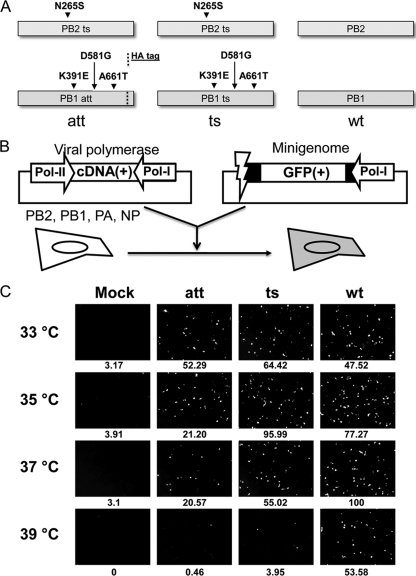
Building upon our prior experience, we wanted to determine whether our strategy could be used to generate an att TRIG SIV vaccine. We chose an SIV H3N2 that belongs to cluster III. The A/swine/Wisconsin/14094/99 (H3N2) (Sw99) virus was cloned and sequenced, and the polymerase genes were mutated by site-directed mutagenesis to engineer the ts and att mutations (Fig. 1A).
FIG. 1.
Combination of mutations in PB1 and PB2 provides attenuation to the polymerase complex of a swine influenza virus strain. (A) Schematic representation of the polymerases att, ts, and the wt. (B) Scheme of the minigenome GFP reporter assay. (C) Pictures from the minigenome assay with the att, ts, and wt polymerases at different temperatures. Numbers below the pictures indicate the number of cells expressing GFP as percentages relative to the maximum and minimum number of fluorescence units. (Numbers reflect data from the experiment shown here. Two other experiments have been performed, with similar results.)
To evaluate if the modifications introduced in the PB2 and PB1 genes produced a ts phenotype in the TRIG virus background, we performed a flu minigenome reporter assay (Fig. 1B). The flu minigenome plasmid containing the GFP reporter gene was cotransfected into 293T cells together with the four plasmids necessary for viral polymerase activity (PB2, PB1, PA, and NP). Transfections were performed at different temperatures: 33°C, 35°C, 37°C, and 39°C. GFP expression was visualized as early as 12 h posttransfection in cells cotransfected with the wild-type polymerase plasmids (data not shown). The GFP fluorescence expression was quantified as described in Materials and Methods. Pictures obtained at 36 h posttransfection, under the fluorescence microscope, showed that the wt polymerase transcriptional activity was highest at 37°C (100%) (Fig. 1C). In contrast, the ts and att polymerase activities were greatly impaired at 37°C (55 and 20%, respectively). This effect was partially recovered for the ts and att polymerases at 35°C and 33°C, respectively (Fig. 1C). More importantly, at 39°C, the ts and att polymerase activities were drastically reduced, with activities close to 0% compared with those of 53% for the wt, confirming the restrictive temperature phenotype of the polymerase mutations in the TRIG virus.
Viruses carrying the att polymerase complex are attenuated in vitro at restrictive temperatures.
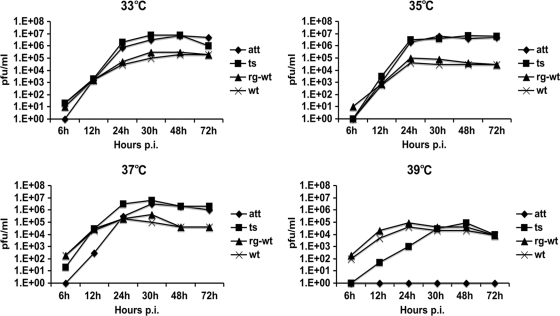
Viruses carrying different versions of the polymerase genes were rescued by reverse genetics (Table 1). Thus, Sw99-rg-wt (the wt virus rescued by reverse genetics [rg]), Sw99-ts, and Sw99-att were produced. A growth curve assay at 33°C, 35°C, 37°C, and 39°C (Fig. 2) was performed to compare the growth characteristics of the different viruses. As expected, the Sw99-att virus was not able to grow at 39°C (the restrictive temperature) and was delayed in its growth at 37°C at early time points. The Sw99-ts virus had an intermediate phenotype compared to those of the Sw99-rg-wt and Sw99-att viruses. More importantly, the Sw99-att and Sw99-ts viruses yielded ∼2 log10 more viruses than Sw99-rg-wt and Sw99 at the permissive temperatures (Fig. 2), which is consistent with the notion that ts mutations provide also a cold-adapted (ca) phenotype. Such a phenotype is maintained despite the presence of the HA tag in the att backbone.
FIG. 2.
att and ts mutations affect the in vitro growth properties of a swine influenza virus. Growth curves of the different viruses att, ts, rg-wt, and the wt on MDCK cells. Cells were infected at an MOI of 0.001, and samples were taken at different time points. (The numbers of viral titers reflect a single experiment, but this experiment has been done one more time, with similar results.)
Viral protein synthesis is affected in the att virus.
We next examined viral protein expression in cells infected with the different viruses at the permissive (35°C) and restrictive (39°C) temperatures. MDCK cells were infected with an MOI of 2, and then viral NS1 protein accumulation was monitored at 2 h intervals (Fig. 3A). Due to lower metabolic rates, protein accumulation was slower in infected cells incubated at 35°C compared to those incubated at 39°C. Nevertheless, NS1 protein expression followed the same pattern of accumulation at either temperature. The att-infected cells showed delayed NS1 accumulation, followed by the ts-infected cells. NP and M1 protein accumulation revealed the same trend, whereas β-actin (control) remained constant (data not shown). Immunoprecipitation of NP in normal or 35S-Met-Cys-labeled cells (Fig. 3B) also revealed reduced expression in att-infected cells compared to that of the ts- and rg-wt-infected cells at either the permissive or restrictive temperatures. These observations are consistent with our previous studies (29).
FIG. 3.
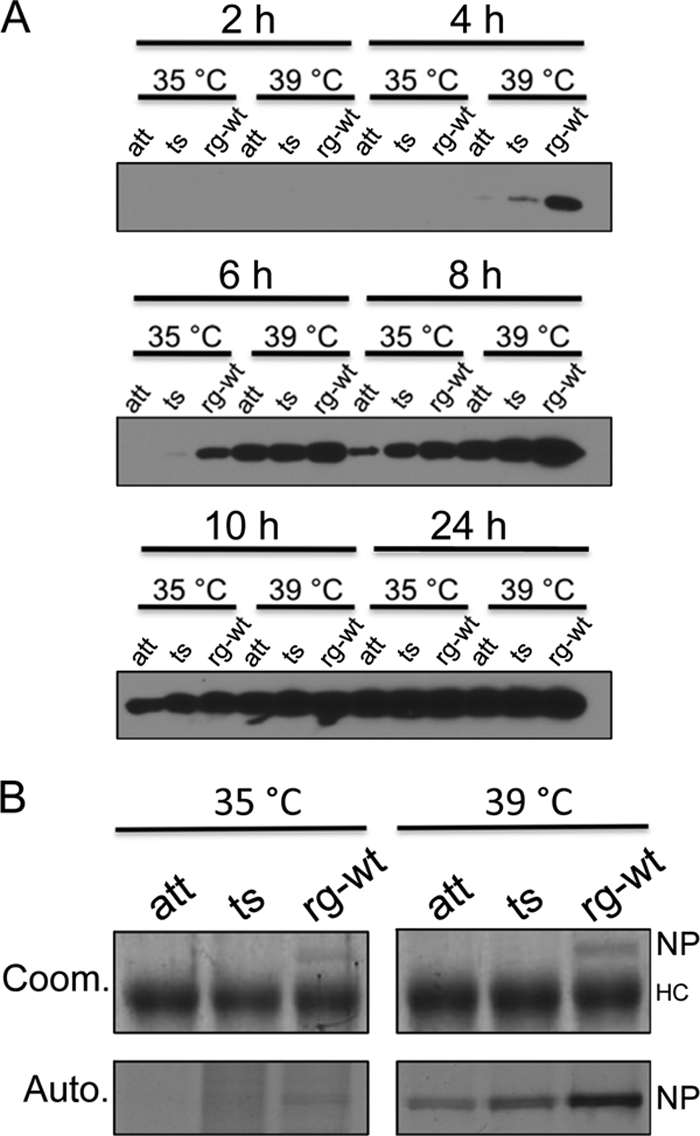
att and ts mutations affect viral protein expression of Sw99-att and Sw99-ts at different temperatures. (A) Western blot against NS1 protein. MDCK cells were infected with the different viruses at an MOI of 2. Cells were harvested at different points p.i. Whole-cell lysates were subjected to Western blot analysis using anti-1-73NS1TX/98 (28). (B) Coom., levels of NP protein determined by immunoprecipitation and Coomassie blue staining. MDCK cells were infected with the different viruses at an MOI of 2. Cells were harvested at 5 h p.i. NP protein from whole-cell lysates was immunoprecipitated using anti-PR8 antibody. NP was visualized by Coomassie blue staining. Auto., levels of NP determined by immunoprecipitation in metabolic-labeled cells. MDCK cells were labeled for 5 h in the presence of 35S-Met-Cys. NP protein from whole-cell lysates was immunoprecipitated using anti-PR8 antibody. NP was visualized by autoradiography. HC, heavy chain.
Viruses that carry the att polymerase complex are attenuated in vivo.
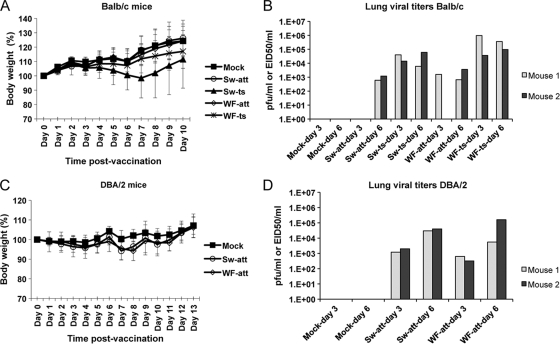
In order to determine if the att mutations would provide an att phenotype in vivo, we tested the Sw99-att and Sw99-ts backbones in a mouse model of influenza infection. Because the Sw99 virus is nonpathogenic in mice (data not shown), we replaced the surface genes of the Sw99 virus with those of A/swine/Iowa/15/30 (H1N1) (Sw30), which have been previously shown to confer a virulent phenotype in mice (35). Thus, 6:2 recombinant viruses were generated by reverse genetics carrying the H1 HA and N1 NA surface genes of Sw30 and the internal backbone of either Sw99-ts or Sw99-att virus (Table 1). In addition, we generated 6:2 reassortants carrying the surface genes of Sw30 and the internal backbone of either WF10-ts or WF10-att virus described previously (29) (Table 1). We monitored the safety of the LAIV by inoculating mice with a high virus dose, as follows: 106 PFU (Sw-att and Sw-ts) or 106 EID50 (WF-att and WF-ts). A mock group was inoculated with PBS. Weight was monitored daily for 10 days postinfection (dpi) (Fig. 4A).
FIG. 4.
Vaccination of BALB/c and DBA/2 mice with att and ts viruses. (A) Body weight in vaccinated BALB/c mice. Mice were vaccinated with Sw-att, Sw-ts, WF-att, WF-ts, or mock vaccinated. Body weight was monitored daily. (B) Lung viral titers in vaccinated BALB/c mice. After vaccination, two mice in each group were sacrificed at days 3 and 6 postvaccination. Lungs were homogenized in 1 ml of PBS, and viral titers were determined by plaque assay (mock, Sw-att, and Sw-ts) and EID50 (WF-att and WF-ts). (C) Body weight in vaccinated DBA/2 mice. Mice were vaccinated with the Sw-att, WF-att, or mock vaccinated. Body weight was monitored daily. (D) Lung viral titers in vaccinated DBA/2 mice. After vaccination, two mice in each group were sacrificed at days 3 and 6 postvaccination. Lungs were homogenized in 1 ml of PBS, and viral titers were determined by plaque assay (mock and Sw-att) and EID50 (WF-att).
Mice inoculated with the Sw-ts virus dropped more than 20% weight compared with that of mock-infected animals. Substantial body weight loss was also observed in the WF-ts-inoculated group. Thus, the mutations in PB1 and PB2 responsible for the attenuated phenotype in the A/Ann Arbor/6/60 strains are not sufficient to attenuate the swine and avian influenza virus strains, as it had been previously shown (16). However, BALB/c mice infected with Sw-att or WF-att virus showed minimal body weight changes and showed no signs of morbidity, suggesting that the incorporation of the HA tag within the att background results in attenuation in mice with the Sw99-att and WF10-att viruses carrying the Sw30 surface proteins. These observations are consistent also with the amount of virus present in the mouse lungs (Fig. 4B). The ts viruses were present in lung homogenates at 3 and 6 dpi, with titers in the order of 104 to 106 PFU. The att virus-infected mice showed much lower viral titers in lung homogenates, with titers of up to 100-fold less than the ts virus-infected mice, confirming its attenuated phenotype.
Recent studies have shown that the mouse strain DBA/2 is more susceptible to influenza virus infection (30). Boon et al. (1) have shown that host genetics influence the outcome of influenza virus infection in these mice. We wanted to determine whether our att viruses would also be attenuated in mice that are more susceptible to influenza (Table 1). Sw30 is five times more virulent in DBA/2 mice than in BALB/c mice, as measured by the MLD50 (Table 2). However, DBA/2 mice inoculated with the Sw-att or WF-att virus presented minor body weight loss and absence of clinical signs of disease (Fig. 4C). The viral lung titers for att viruses at 3 and 6 dpi were comparable to those determined for BALB/c mice (Fig. 4D). Thus, the att backbone provides sufficient attenuation for influenza virus even in a more susceptible mouse strain.
In order to determine the immunogenicity of the att viruses, mice were bled at 21 dpv, and seroconversion was measured by HI against the Sw30 virus. Substantial antibody titers were observed for BALB/c mice in the ts- and att-inoculated groups (Table 3). More importantly, DBA/2-vaccinated animals also developed a strong immune response similar to that of BALB/c mice (Table 3). We conclude that the att viruses are immunogenic and that the increased susceptibility to influenza in DBA/2 mice is not due to the failure to mount an adequate humoral response.
TABLE 3.
HI titers against Sw30 pre- and postchallenge
| Virus | HI titers (pv/pc) against Sw30-homologous challenge with Sw30a |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| BALB/c mice |
DBA/2 mice |
||||||||
| Mouse 1 | Mouse 2 | Mouse 3 | Mouse 4 | Mouse 5 | Mouse 1 | Mouse 2 | Mouse 3 | Mouse 4 | |
| Mock | <10/† | <10/† | <10/† | <10/† | <10/† | <10/† | <10/† | <10/† | <10/† |
| Sw-att | 320/640 | 80/640 | 80/320 | 80/320 | 160/640 | 160/640 | 320/640 | 320/640 | 160/1,280 |
| Sw-ts | 320/2,560 | 640/640 | 640/1,280 | 640/1,280 | 640/2,560 | ND | ND | ND | ND |
| WF-att | 160/320 | 320/640 | 160/80 | 320/640 | 320/1,280 | 320/ND | 160/ND | 320/ND | 160/ND |
| WF-ts | 320/1,280 | 320/320 | 320/320 | 320/320 | 320/320 | ND | ND | ND | ND |
pv/pc, postvaccination/postchallenge; ND, not done; †, dead mouse.
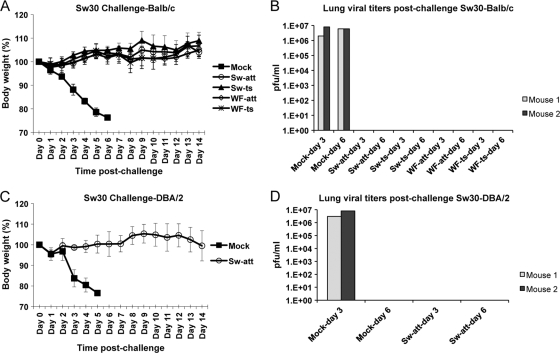
att viruses provide sterile immunity against challenge.
At 21 dpv, BALB/c mice inoculated with the att and ts viruses were challenged with the Sw30 virus (100 MLD50). As shown in Fig. 5A, mock-vaccinated mice succumbed to challenge within 6 dpc, with lung virus titers in the order of 106 PFU (Fig. 5B). In contrast, ts- and att-vaccinated mice survived the challenge, showing neither signs of disease nor body weight loss. The ts- and att-vaccinated mice were also very effective at clearing the challenge virus, as shown by the absence of measurable lung virus titers at 3 and 6 dpc. Full protection was also observed in Sw-att-vaccinated DBA/2 mice (Fig. 5C and D). This study indicates that vaccination with the att viruses provides sterile immunity in homologous challenge. As expected, increased HI titers were observed in vaccinated mice at 14 dpc (Table 3).
FIG. 5.
att viruses provide homologous protection against influenza A/swine/Iowa/15/30 (H1N1) virus in BALB/c- and DBA/2-vaccinated mice. (A) Body weight in vaccinated/challenged BALB/c mice. Mice were vaccinated with Sw-att, Sw-ts, WF-att, WF-ts, or mock vaccinated and challenged with 100 MLD50 of Sw30. Body weight was monitored daily. (B) Lung viral titers in vaccinated/challenged BALB/c mice. After challenge with Sw30, two mice in each group were sacrificed at days 3 and 6 postchallenge. Lungs were homogenized in 1 ml of PBS, and viral titers were determined by plaque assay. (C) Body weight in vaccinated/challenged DBA/2 mice. Mice were vaccinated with Sw-att or mock vaccinated and challenged with 100 MLD50 of Sw30. Body weight was monitored daily. (D) Lung viral titers in vaccinated/challenged DBA/2 mice. After challenge with Sw30, two mice in each group were sacrificed at days 3 and 6 postchallenge. Lungs were homogenized in 1 ml of PBS, and viral titers were determined by plaque assay.
Sw30 att viruses show full protection against the pandemic 2009 H1N1 virus.
The S-OIV 2009 H1N1 is characterized by defective growth in 10-day-old embryonated eggs and poor HA activities. Thus, selection of strains with mutations that improve yield in eggs and get better HA activity has been an obligatory step for the preparation of vaccines against the 2009 pandemic virus (4). We would like to speculate that drift variants of this virus will continue showing limited growth in eggs and low HA activities. Sw30 is a distant relative of the 2009 S-OIV; however, sera obtained from mice vaccinated against Sw30 do not cross-react against Ca04 in HI assays (Table 4). Nevertheless, some monoclonal antibodies prepared in our laboratory against the S-OIV 2009 H1N1 show neutralizing activity against Sw30, indicating at least partial conservation of common epitopes (J. Ye and D. R. Pérez, unpublished results). Furthermore, Sw30 and many strains of the classical SIV lineage are better prepared to grow in eggs and show no deficiencies in HA activity. We decided to test whether the att viruses carrying the Sw30 surface proteins would provide efficient cross-protection against the S-OIV 2009 H1N1. DBA/2 mice were used in these studies due to their high susceptibility to the Ca04 pandemic virus (Table 2).
TABLE 4.
HI titers against Sw30 and Ca04 pre- and postchallenge with Ca04
| Virus | HI titers (pv/pc) in DBA/2-heterologous challenge with Ca04 againsta: |
|||||||
|---|---|---|---|---|---|---|---|---|
| Sw30 |
Ca04 |
|||||||
| Mouse 1 | Mouse 2 | Mouse 3 | Mouse 4 | Mouse 1 | Mouse 2 | Mouse 3 | Mouse 4 | |
| Mock | <10/† | <10/† | <10/† | <10/† | <10/† | <10/† | <10/† | <10/† |
| Sw-att | 160/1,280 | 320/2,560 | 320/1,280 | 160/1,280 | <10/160 | <10/<10 | <10/80 | <10/<10 |
| WF-att | 320/640 | 160/2,560 | 320/640 | 160/640 | <10/<10 | <10/160 | <10/80 | <10/<10 |
pv/pc, postvaccination/postchallenge; †, dead mouse.
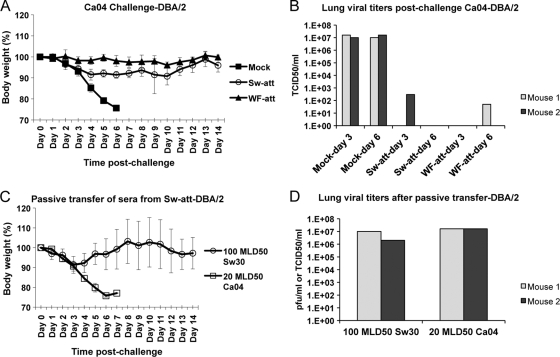
DBA/2 mice vaccinated against Sw30 (Sw-att or WF-att) were challenged with Ca04 (Table 1). Heterologous protection was readily observed in DBA/2 mice. att-vaccinated DBA/2 mice challenged with 20 MLD50 Ca04 survived, in contrast to mock-vaccinated mice (Fig. 6A). Minimal body weight losses were observed in att-vaccinated DBA/2 mice challenged with Ca04, and low virus titers were detected in the lungs (Fig. 6B). These studies showed efficient heterologous protection against the S-OIV 2009 H1N1 provided by att viruses that carry the Sw30 surface proteins.
FIG. 6.
att viruses provide heterologous protection against influenza A/California/04/09 (H1N1) virus in DBA/2-vaccinated mice. (A) Body weight in DBA/2-vaccinated mice. Mice were vaccinated with Sw-att, WF-att, or mock vaccinated and challenged with 20 MLD50 of Ca04. Body weight was monitored daily. (B) Lung viral titers in vaccinated/challenged DBA/2 mice. After challenge with Ca04, two mice in each group were sacrificed at days 3 and 6 postchallenge. Lungs were homogenized in 1 ml of PBS, and viral titers were determined by TCID50. (C) Body weight in mice challenged with 100 MLD50 of Sw30 or 20 MLD50 of Ca04 after passive transfer of antibodies from Sw-att-vaccinated animals into naïve animals. Body weight was monitored daily. (D) Lung viral titers in Sw30- and Ca04-challenged DBA/2 mice after passive transfer of Sw-att antibodies. After challenge with Ca04, two mice in each group were sacrificed at day 3 postchallenge. Lungs were homogenized in 1 ml of PBS, and viral titers were determined by plaque assay (Sw30) or TCID50 (Ca04).
In order to demonstrate whether protection against the Ca04 challenge was due to significantly cross-neutralizing antibody activity, we performed a passive transfer study using sera obtained from Sw-att-vaccinated DBA/2 mice. Pooled mouse sera with a HA titer of 1:160 was used to inoculate i.p. a group of naïve DBA/2 mice (n = 12). At 24 h post-passive transfer, HI titers in recipient mice were 1:20. Subsequently, mice were challenged with either 100 MLD50 Sw30 or 20 MLD50 Ca04 (Table 2). Significant morbidity was observed within the first 3 dpc with Sw30, although mice eventually recovered, and none of them died (Fig. 6C). This result suggests that passive transfer antibodies were effective in controlling Sw30 infection. In contrast, none of the Ca04-challenged mice survived, indicating that the amount and/or level of cross-neutralization activity of antibodies was suboptimal. Viral lung titers in Ca04-challenged animals were very high at 3 dpc (Fig. 6D), which is in agreement with the morbidity observed (Fig. 6C). These results suggest that cellular-mediated immunity, in addition to humoral immunity, must account for the efficient protection observed in the att-vaccinated animals challenged with the Ca04 virus.
Original antigenic sin (OAS) observed after vaccination and heterologous challenge.
OAS was defined half a century ago by Thomas Francis, Jr. (10), corroborated by Robert Webster et al. (7, 8, 34), and revisited recently by Kim et al. (17). OAS is defined as the preference of the immune system to utilize immunological memory based on a previous infection when a second antigenically drifted variant is encountered. Thus, subsequent infections result in preferential stimulation of B-cell memory, resulting from primary infection instead of the new virus. This effect is also seen in the vaccination studies using the att viruses. att-vaccinated DBA/2 mice developed a poor antibody response against Ca04 virus (Table 4), although they were fully protected against challenge (Fig. 6A). In contrast, these same mice showed a substantial increase in the response against the homologous virus Sw30 (Table 4). These observations are consistent with OAS. The Sw-att and WF-att viruses have identical surface proteins but different viral backbones. While the Sw-att TRIG backbone is similar to the TRIG backbone in Ca04 (except for the M gene), the WF-att one is entirely of avian origin. We noted that Sw-att-vaccinated mice challenged with Ca04 had slightly higher HI titers against Sw30 than the WF-att-vaccinated mice (Table 4). However, the WF-att-vaccinated mice showed less variation in body weight changes than those vaccinated with the Sw-att virus (Fig. 6A). Whether such responses are related to the ability of one vaccine virus to induce a more accentuated OAS response versus that of another after challenge requires further investigation, since it may have implications for the development of LAIV.
DISCUSSION
Vaccination is the best method to prevent influenza virus infection. In this report, we showed attenuation of a TRIG SIV after introducing mutations previously shown to attenuate avian influenza viruses. The data in vitro showed the ts phenotype of the att backbones and their ability to produce better virus yields at the permissive temperature than the wild-type Sw99 virus. LAIV are temperature-sensitive viruses, although the exact mechanism for restriction at nonpermissive temperatures is not completely understood. Recent studies showed that the cold-adapted A/AnnArbor/6/60 strain, the master donor for the LAIV in FluMist, has multiple defects at the restrictive temperatures (3). These studies showed that synthesis of viral proteins at the permissive and restrictive temperatures is not significantly affected during a single cycle replication. We performed similar studies with a different outcome: substantial differences were seen in the levels of expression among the att, ts, and rg-wt viruses at early time points, at both the permissive and restrictive temperatures. This discrepancy could be due to multiple factors, including differences in the strains and MOI used (MOI of 2 in our studies versus MOI of 5 in reference 3). Our observations are in agreement with the minigenome assay in which lower reporter activities were observed with the att polymerase than with the ts or wt polymerase complexes. It is important to note that the att virus protein synthesis was also lower than that of the wild-type virus at the permissive temperature; however, the att virus yielded higher virus titers than the wild type after multiple cycles of replication. It is tempting to speculate that the att viruses need to reach a minimum threshold where virus replication and assembly occur at levels equal to or better than the wild type at the permissive temperatures. This feature could make the att backbone an ideal vaccine, since the initial slow replication would allow the host immune system to react accordingly. However, the virus could replicate to significant levels to mount a strong immune response without causing signs of disease. This appears to be the case in our mice studies. We showed that our att approach resulted in virus attenuation both in BALB/c and in DBA/2 mice, a mouse strain previously shown to be highly susceptible to influenza viruses. Boon et al. (1) identified the hemolytic complement gene as one of the genes responsible for increased susceptibility to influenza, whereas Brownstein linked the susceptibility of DBA/2 mice to Sendai virus infection to an effect in tracheal mucociliary transport (2). It is not known whether these genetic alterations could have an effect on the outcome of disease after vaccination. As expected, att viruses replicated more efficiently in DBA/2 mice than in BALB/c mice (Fig. 4D and B). However, DBA/2 mice showed no signs of morbidity and no changes in body weight (Fig. 4C) after vaccination with the att viruses, suggesting that our att strategy is effective for attenuation. Furthermore, DBA/2 mice mounted a strong neutralizing response after vaccination, indicating that genetic alterations that increase their susceptibility to influenza were not an impediment for an adequate humoral response. This is important when considering the testing of vaccines against influenza in mice since, unlike the DBA/2 strain, other mouse strains are usually not susceptible to non-mouse-adapted influenza viruses. Our att backbone showed limited replication in the lungs of DBA/2 mice and greatly reduced replication in the lungs of BALB/c mice. The limited replication of the att viruses should make them safe vaccines for veterinary and human use.
The mechanisms that control influenza cross-protection are not completely understood. Cellular-mediated immunity plays a major role in cross-protection, although recent studies suggest that some level of humoral cross-protective immunity could also be present (36). The role of humoral cross-protective immunity is easier to envision in antigenically drifted HA variants within the same subtype, as it would be expected that there is still some level of cross-recognition. This was the case between Sw30 and Ca04, in which at least one monoclonal antibody showed neutralizing activity for both of the viruses (not shown). Because of partial antigenic relatedness between the Sw30 and Ca04 viruses and because the Sw30 virus is easier to grow in eggs than the Ca04 virus, we wanted to test whether att vaccines prepared against the former virus would be protective against the latter virus. Effective cross-protection was observed in DBA/2 mice, although passive transfer studies suggested that humoral cross-protective immunity might have had very limited effects. Although the use of Sw30-like att viruses are likely not a viable alternative against the S-OIV 2009 H1N1, our studies clearly show the potential of our approach to provide attenuation to influenza viruses of multiple animal origins. Interestingly, the effect of OAS was clearly discernible in the DBA/2 mice vaccinated against Sw30 and then challenged with the Ca04 virus. This observation suggests that the att viruses are most likely to have provided protection against the Ca04 virus mainly through cell-mediated mechanisms. Future studies addressing depletion of CD8+ T cells and enzyme-linked immunospot (ELISPOT) assays are needed to confirm the role of cell-mediated immunity in protection. However, such studies are beyond the scope of the present report.
To our knowledge, this is the first time that OAS has been observed using LAIV. Despite this effect, our att vaccines fully protected against challenge. This is in contrast to the results of the study of Vincent et al., which used killed influenza vaccines against divergent strains and in which vaccinated pigs developed enhanced pneumonia (32). Since LAIV are known to elicit cell-mediated responses, it is highly plausible that protection in our studies was mediated in great part by cell-mediated mechanisms. Our results also suggest that in addition to the surface proteins, the internal genes could play a role in enhancing or decreasing OAS. We would have predicted that the Sw-att backbone would protect better against Ca04 challenge due to their closer relationship. Interestingly, the WF-att backbone provided better protection, which is consistent with our previous studies that suggest that the WF-att backbone could be an ideal universal backbone for live influenza vaccines (12). While surveillance systems are established to determine the antigenic makeup of prevalent influenza virus strains, it is not uncommon to see significant mismatches between the circulating and vaccine strains. Under these circumstances, OAS could occur. Based on our observations, the use of alternative LAIV backbones could overcome more easily the OAS effect, offering better protection. Having different alternative LAIV backbones available should aid in our strategy for the development of better cross-protective vaccines against influenza.
Acknowledgments
This work was supported in part by USDA/CSREES grant 2008-00909 (to A.S. and D.R.P.) and grants 2005-35605 and 2007-04981 (to D.R.P.) and by NIAID-NIH contract HHSN266200700010C (to D.R.P.).
We are indebted to Alex Alfaro and Sharon Azogue for their technical assistance and to Ivan Gómez-Osorio and Yonas Araya for their assistance with the mouse studies.
Footnotes
Published ahead of print on 24 February 2010.
REFERENCES
- 1.Boon, A. C., J. deBeauchamp, A. Hollmann, J. Luke, M. Kotb, S. Rowe, D. Finkelstein, G. Neale, L. Lu, R. W. Williams, and R. J. Webby. 2009. Host genetic variation affects resistance to infection with a highly pathogenic H5N1 influenza A virus in mice. J. Virol. 83:10417-10426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brownstein, D. G. 1987. Resistance/susceptibility to lethal Sendai virus infection genetically linked to a mucociliary transport polymorphism. J. Virol. 61:1670-1671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chan, W., H. Zhou, G. Kemble, and H. Jin. 2008. The cold adapted and temperature sensitive influenza A/Ann Arbor/6/60 virus, the master donor virus for live attenuated influenza vaccines, has multiple defects in replication at the restrictive temperature. Virology 380:304-311. [DOI] [PubMed] [Google Scholar]
- 4.Chen, Z., W. Wang, H. Zhou, A. L. Suguitan, Jr., C. Shambaugh, L. Kim, J. Zhao, G. Kemble, and H. Jin. 2010. Generation of live attenuated novel influenza virus A/California/7/09 (H1N1) vaccines with high yield in embryonated chicken eggs. J. Virol. 84:44-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cox, N. J., and K. Subbarao. 2000. Global epidemiology of influenza: past and present. Annu. Rev. Med. 51:407-421. [DOI] [PubMed] [Google Scholar]
- 6.Easterday, B. C. 1980. The epidemiology and ecology of swine influenza as a zoonotic disease. Comp. Immunol. Microbiol. Infect. Dis. 3:105-109. [DOI] [PubMed] [Google Scholar]
- 7.Fazekas de St. Groth, S., and R. G. Webster. 1966. Disquisitions of original antigenic sin. I. Evidence in man. J. Exp. Med. 124:331-345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fazekas de St. Groth, S., and R. G. Webster. 1966. Disquisitions on original antigenic sin. II. Proof in lower creatures. J. Exp. Med. 124:347-361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fazekas de St. Groth, S., R. G. Webster, and A. Datyner. 1963. Two new staining procedures for quantitative estimation of proteins on electrophoretic strips. Biochim. Biophys. Acta 71:377-391. [DOI] [PubMed] [Google Scholar]
- 10.Francis, T. 1960. On the doctrine of original antigenic sin. Proc. Am. Philos. Soc. 104:572-578. [Google Scholar]
- 11.Grimm, D., P. Staeheli, M. Hufbauer, I. Koerner, L. Martinez-Sobrido, A. Solorzano, A. Garcia-Sastre, O. Haller, and G. Kochs. 2007. Replication fitness determines high virulence of influenza A virus in mice carrying functional Mx1 resistance gene. Proc. Natl. Acad. Sci. U. S. A. 104:6806-6811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hickman, D., M. J. Hossain, H. Song, Y. Araya, A. Solorzano, and D. R. Perez. 2008. An avian live attenuated master backbone for potential use in epidemic and pandemic influenza vaccines. J. Gen. Virol. 89:2682-2690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hoffmann, E., G. Neumann, Y. Kawaoka, G. Hobom, and R. G. Webster. 2000. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc. Natl. Acad. Sci. U. S. A. 97:6108-6113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoffmann, E., J. Stech, Y. Guan, R. G. Webster, and D. R. Perez. 2001. Universal primer set for the full-length amplification of all influenza A viruses. Arch. Virol. 146:2275-2289. [DOI] [PubMed] [Google Scholar]
- 15.Jin, H., B. Lu, H. Zhou, C. Ma, J. Zhao, C. F. Yang, G. Kemble, and H. Greenberg. 2003. Multiple amino acid residues confer temperature sensitivity to human influenza virus vaccine strains (FluMist) derived from cold-adapted A/Ann Arbor/6/60. Virology 306:18-24. [DOI] [PubMed] [Google Scholar]
- 16.Jin, H., H. Zhou, B. Lu, and G. Kemble. 2004. Imparting temperature sensitivity and attenuation in ferrets to A/Puerto Rico/8/34 influenza virus by transferring the genetic signature for temperature sensitivity from cold-adapted A/Ann Arbor/6/60. J. Virol. 78:995-998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim, J. H., I. Skountzou, R. Compans, and J. Jacob. 2009. Original antigenic sin responses to influenza viruses. J. Immunol. 183:3294-3301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee, J. H., M. R. Gramer, and H. S. Joo. 2007. Efficacy of swine influenza A virus vaccines against an H3N2 virus variant. Can. J. Vet. Res. 71:207-212. [PMC free article] [PubMed] [Google Scholar]
- 19.Lekcharoensuk, P., K. M. Lager, R. Vemulapalli, M. Woodruff, A. L. Vincent, and J. A. Richt. 2006. Novel swine influenza virus subtype H3N1, United States. Emerg. Infect. Dis. 12:787-794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ma, W., M. Gramer, K. Rossow, and K. J. Yoon. 2006. Isolation and genetic characterization of new reassortant H3N1 swine influenza virus from pigs in the midwestern United States. J. Virol. 80:5092-5096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ma, W., K. M. Lager, A. L. Vincent, B. H. Janke, M. R. Gramer, and J. A. Richt. 2009. The role of swine in the generation of novel influenza viruses. Zoonoses Public Health 56:326-337. [DOI] [PubMed] [Google Scholar]
- 22.Mayer, D., K. Molawi, L. Martinez-Sobrido, A. Ghanem, S. Thomas, S. Baginsky, J. Grossmann, A. Garcia-Sastre, and M. Schwemmle. 2007. Identification of cellular interaction partners of the influenza virus ribonucleoprotein complex and polymerase complex using proteomic-based approaches. J. Proteome Res. 6:672-682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nakajima, K., U. Desselberger, and P. Palese. 1978. Recent human influenza A (H1N1) viruses are closely related genetically to strains isolated in 1950. Nature 274:334-339. [DOI] [PubMed] [Google Scholar]
- 24.Neumann, G., T. Noda, and Y. Kawaoka. 2009. Emergence and pandemic potential of swine-origin H1N1 influenza virus. Nature 459:931-939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Perez, D. R., R. J. Webby, E. Hoffmann, and R. G. Webster. 2003. Land-based birds as potential disseminators of avian mammalian reassortant influenza A viruses. Avian Dis. 47:1114-1117. [DOI] [PubMed] [Google Scholar]
- 26.Reed, L. J., and H. Muench. 1938. A simple method for estimating 50 percent endpoints. Am. J. Hyg. (Lond.) 27:493-497. [Google Scholar]
- 27.Smith, G. J., D. Vijaykrishna, J. Bahl, S. J. Lycett, M. Worobey, O. G. Pybus, S. K. Ma, C. L. Cheung, J. Raghwani, S. Bhatt, J. S. Peiris, Y. Guan, and A. Rambaut. 2009. Origins and evolutionary genomics of the 2009 swine-origin H1N1 influenza A epidemic. Nature 459:1122-1125. [DOI] [PubMed] [Google Scholar]
- 28.Solorzano, A., R. J. Webby, K. M. Lager, B. H. Janke, A. Garcia-Sastre, and J. A. Richt. 2005. Mutations in the NS1 protein of swine influenza virus impair anti-interferon activity and confer attenuation in pigs. J. Virol. 79:7535-7543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Song, H., G. R. Nieto, and D. R. Perez. 2007. A new generation of modified live-attenuated avian influenza viruses using a two-strategy combination as potential vaccine candidates. J. Virol. 81:9238-9248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Srivastava, B., P. Blazejewska, M. Hessmann, D. Bruder, R. Geffers, S. Mauel, A. D. Gruber, and K. Schughart. 2009. Host genetic background strongly influences the response to influenza a virus infections. PLoS One 4:e4857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Taubenberger, J. K. 2006. The origin and virulence of the 1918 “Spanish” influenza virus. Proc. Am. Philos Soc. 150:86-112. [PMC free article] [PubMed] [Google Scholar]
- 32.Vincent, A. L., K. M. Lager, B. H. Janke, M. R. Gramer, and J. A. Richt. 2008. Failure of protection and enhanced pneumonia with a US H1N2 swine influenza virus in pigs vaccinated with an inactivated classical swine H1N1 vaccine. Vet. Microbiol. 126:310-323. [DOI] [PubMed] [Google Scholar]
- 33.Vincent, A. L., W. Ma, K. M. Lager, B. H. Janke, and J. A. Richt. 2008. Swine influenza viruses a North American perspective. Adv. Virus Res. 72:127-154. [DOI] [PubMed] [Google Scholar]
- 34.Webster, R. G. 1966. Original antigenic sin in ferrets: the response to sequential infections with influenza viruses. J. Immunol. 97:177-183. [PubMed] [Google Scholar]
- 35.Weingartl, H. M., R. A. Albrecht, K. M. Lager, S. Babiuk, P. Marszal, J. Neufeld, C. Embury-Hyatt, P. Lekcharoensuk, T. M. Tumpey, A. Garcia-Sastre, and J. A. Richt. 2009. Experimental infection of pigs with the human 1918 pandemic influenza virus. J. Virol. 83:4287-4296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xie, H., T. M. Liu, X. Lu, Z. Wu, J. A. Belser, J. M. Katz, T. M. Tumpey, and Z. Ye. 2009. A live attenuated H1N1 M1 mutant provides broad cross-protection against influenza A viruses, including highly pathogenic A/Vietnam/1203/2004, in mice. J. Infect. Dis. 200:1874-1883. [DOI] [PubMed] [Google Scholar]