Abstract
The glycoproteins (GPs) of filoviruses are responsible for virus entry into cells. It is known that GP interacts with cellular C-type lectins for virus attachment to cells. Since primary target cells of filoviruses express C-type lectins, C-type lectin-mediated entry is thought to be a possible determinant of virus tropism and pathogenesis. We compared the efficiency of C-type lectin-mediated entry between Marburg virus strains Angola and Musoke by using a vesicular stomatitis virus (VSV) pseudotype system. VSV pseudotyped with Angola GP (VSV-Angola) infected K562 cells expressing the C-type lectin, human macrophage galactose-type C-type lectin (hMGL), or dendritic cell-specific ICAM-3-grabbing nonintegrin (DC-SIGN) more efficiently than VSV pseudotyped with Musoke GP (VSV-Musoke). Unexpectedly, the binding affinity of the C-type lectins to the carbohydrates on GPs did not correlate with the different efficiency of C-type lectin-mediated entry. Site-directed mutagenesis identified the amino acid at position 547, which switched the efficiency of C-type lectin-mediated entry. In a three-dimensional model of GP, this amino acid was in close proximity to the putative site of cathepsin processing. Interestingly, the cathepsin inhibitors reduced the infectivity of VSV-Angola less efficiently than that of VSV-Musoke in C-type lectin-expressing K562 cells, whereas only a limited difference was found in control cells. The amino acid at position 547 was critical for the different effects of the inhibitors on the virus infectivities. These results suggest that the efficiency of C-type lectin-mediated entry of filoviruses is controlled not only by binding affinity between C-type lectins and GP but also by mechanisms underlying endosomal entry, such as proteolytic processing by the cathepsins.
Marburg virus (MARV) and Ebola virus (EBOV), which belong to the family Filoviridae, have produced sporadic outbreaks of hemorrhagic fever in Africa. After the initial outbreak of MARV infection in 1967 in Europe, which resulted in 7 deaths among 32 confirmed patients (41), there were three small, isolated outbreaks of MARV infection in Africa between 1975 and 1987. During one of the outbreaks in Kenya in 1980, one of the two patients died (42), and experimental studies showed that this Kenyan MARV Musoke strain (Musoke) killed monkeys within 12 days after infection (6). On the other hand, throughout a recent outbreak of MARV infection in Angola, 84% of the 422 patients died (29). This MARV Angola strain (Angola) produced fatal disease in monkeys within 8 days after inoculation and was thought to be more pathogenic than the Musoke strain (5, 17). Among EBOVs, a difference in pathogenicity was also suggested. Zaire EBOV is thought to be the most pathogenic EBOV, killing approximately up to 90% of patients, whereas Reston EBOV has never caused lethal infection in humans (31) and is less pathogenic in experimentally infected nonhuman primates than Zaire EBOV (16). However, the factors that influence the different pathogenicity among filoviruses remain unclear.
The envelope glycoprotein (GP) of filoviruses is the only spike protein and is responsible for both receptor binding and membrane fusion. GP is comprised of two molecules, GP1 and GP2, which are linked by a disulfide bond. GP1 contains the receptor-binding domain, which is responsible for the viral attachment to cell surface molecules (9, 25). GP2 has the heptad repeat regions required for assembling GP as a trimer and the internal fusion loop, which is thought to interact with the cellular membrane (50). Although the trigger to promote the conformational change leading to membrane fusion is not fully understood, it was recently suggested that endosomal proteolysis of EBOV GP by cysteine proteases such as cathepsins B and L plays an important role in inducing membrane fusion (4).
Both MARV and EBOV GPs are heavily glycosylated and contain both N- and O-linked carbohydrate chains with different terminal sialylation patterns that seem to depend on the virus strains and cell lines used for virus propagation (12, 18, 39, 48). The middle one-third of the GP molecule particularly varies among filoviruses and includes a mucin-like region (MLR) that contains a number of potential N- and O-linked glycosylation sites (32, 52). It is thought that carbohydrate chains on GP are recognized by cellular C-type lectins, such as the liver-specific C-type lectin asialoglycoprotein receptor (ASGP-R) (3), dendritic cell-specific ICAM-3-grabbing nonintegrin (DC-SIGN), liver/lymph node-SIGN (L-SIGN) (1, 2, 20, 30, 33, 40), human macrophage galactose-type C-type lectin (hMGL) (46), and liver and lymph node sinusoidal endothelial cell C-type lectin (LSECtin) (8, 19, 20, 34). While these C-type lectins show different specificities, depending on the structures of target glycans, all have been reported to promote filovirus entry. Hepatocytes, dendritic cells (DCs), monocytes, and macrophages are thought to be the preferred target cells of filoviruses, and infection of these cells is important for hemorrhagic manifestation and immune disorders (7, 13, 15, 36). Thus, increased infection of these cells might be directly involved in the pathogenesis of filoviruses (16).
In the present study, using the vesicular stomatitis virus (VSV) pseudotype system (VSV that contains the green fluorescent protein [GFP] gene rather than the receptor-binding GP gene [VSVΔG*]) described previously (45), we compared the properties of Angola and Musoke GPs and found a significant difference in the ability to utilize hMGL and DC-SIGN for their entry. Importantly, GP binding affinity for the C-type lectins was not the primary factor contributing to the difference. We identified a single amino acid involved in the different efficiency of C-type lectin-mediated entry between Angola and Musoke. Three-dimensional analysis suggested that this amino acid might affect the processing of GP by endosomal cysteine proteases and/or flexibility of the GP internal fusion loop. Here, mechanisms underlying the different efficiencies for C-type lectin-mediated entry of filoviruses are discussed.
MATERIALS AND METHODS
Viruses and cells.
VSVΔG* expressing GFP pseudotyped with MARV GPs was generated as previously described (45). The viruses were treated with neutralizing monoclonal antibody I1 to VSV G protein before use (28). The virus titer was determined by counting the number of cells expressing GFP using fluorescence microscopy or flow cytometry.
Vero E6 and HEK293T cells were grown in Dulbecco's modified Eagle's medium supplemented with 10% fetal bovine serum, l-glutamine, and antibiotics. Human chronic myelogenous leukemia (K562) cells were grown in RPMI 1640 supplemented with 10% fetal bovine serum, l-glutamine, and antibiotics. K562 clones expressing hMGL (K562/hMGL) were generated as previously described (46). cDNA encoding DC-SIGN was isolated from a placenta cDNA library (Invitrogen) and then cloned into a mammalian cell expression vector, pcDNA3.1(+) (Invitrogen). K562 cells were transfected with the plasmid using Attractene transfection reagent (Qiagen). After selection with Geneticin (G418 sulfate; Calbiochem), DC-SIGN-positive cells (K562/DC-SIGN) were enriched with immunomagnetic beads by using monoclonal antibody CD209 (Beckman Coulter). K562 cells transfected with the empty vector pcDNA3.1(+) and selected by Geneticin were used as control cells (K562/mock).
Expression of soluble recombinant hMGL and DC-SIGN.
Soluble hMGL was purified by affinity chromatography on a column of galactose-Sepharose 4B as described previously (44). The expression plasmid pET-15b encoding the extracellular domain (ECD) of DC-SIGN was similarly constructed. The plasmid was subsequently used to transform Escherichia coli BL21/DE3 pLysS. The recombinant DC-SIGN ECD was prepared from inclusion bodies in E. coli. The recombinant DC-SIGN ECD was bound to mannose-Sepharose 4B and eluted with 10 mM EDTA. Subsequently, biotinylation of these soluble proteins was performed using EZ-Link sulfo-NHS-LC-biotin (Pierce).
Lectin-ELISA analysis.
VSVΔG* pseudotyped with GPs was purified by ultracentrifugation through a 25% sucrose cushion and diluted to give a titer of 5 × 105 infectious units (IU)/ml in phosphate-buffered saline (PBS). Enzyme-linked immunosorbent assay (ELISA) plates were coated with the viruses and then blocked with 3% bovine serum albumin in PBS. After each well was washed with Dulbecco's Tris-buffered saline (dTBS), biotinylated hMGL or DC-SIGN in dTBS was added. To detect C-type lectins bound to the viruses, horseradish peroxidase (HRP)-streptavidin (Jackson ImmunoResearch) and 3,3′,5,5′-tetramethylbenzidine (Sigma) were used.
Mutagenesis.
To construct the mutant GPs, MARV GP cDNAs were cloned into the pATX vector, kindly provided by H. Ebihara (Laboratory of Virology, Department of Health and Human Services, Rocky Mountain Laboratories, Division of Intramural Research, NIAID, NIH). By using the primers containing the sequences of the desired regions and the class IIS restriction enzyme, the BsmBI site, the MLR-deletion mutant, and chimeric GP constructs were generated. Mutant GPs with a single substitution (A/H504T, A/G547V, A/A596T, A/R618K, M/T504H, M/V547G, M/T596A, and M/K618R) were generated by using the primers containing the desired mutations and the BsmBI site. All the mutant GP genes were cloned into pCAGGS, the mammalian expression plasmid, and used for expression of the GPs in HEK293T cells.
Virus titration.
The infectivity of VSVΔG* pseudotyped with GPs on K562 clones was determined by counting the number of GFP-positive cells using flow cytometry. To test C-type lectin-mediated entry, 105 cells of the K562 clones in 96-well plates were infected with the respective viruses, whose titers were standardized (i.e., all the viruses were diluted to give 1 × 105 to 5 × 105 IU/ml in Vero E6 cells that uniformly gave approximately 1 × 104 to 5 × 104 IU/ml in K562/mock cells), and the number of GFP-positive cells were counted. To investigate the effects of the cathepsin B and L inhibitors, CA-074Me and FY-dmk, respectively (Calbiochem), cells were treated with one of the inhibitors for 3 h before infection.
Binding assay.
Approximately 106 infectious units (in Vero E6 cells) of purified VSVΔG* pseudotyped with GPs were incubated with 105 cells of K562/hMGL and K562/DC-SIGN for 1 h on ice. After being washed three times with PBS(+), cells were lysed to measure the amount of VSV matrix protein in the virions which bound on the cell surface.
SDS-PAGE and Western blotting.
Cells or purified viruses were lysed with PBS containing 1% Triton X-100 and protease inhibitor cocktail Complete Mini (Roche), and the insoluble fraction was removed by centrifugation. Lysates were mixed with Laemmli sample buffer (Bio-Rad), electrophoresed by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) on 10 to 20% SuperSep (Wako), and blotted on a polyvinylidene difluoride (PVDF) membrane (Millipore). Non-specific binding to the membrane was blocked with 3% skim milk in PBS. A mixture of the sera obtained from mice immunized with Angola virus-like particles and Musoke virus-like particles for detecting MARV GPs or anti-VSV matrix protein monoclonal antibody (195-2) was incubated with the membrane. Peroxidase-conjugated AffiniPure goat anti-mouse IgG(H+L) (Jackson ImmunoResearch) and Immobilon Western (Millipore) were used for visualization. Intensities of specific bands were measured with ATTO CS Analyzer 2.1.
Molecular modeling.
A three-dimensional model of Angola GP was generated by a homology modeling method using the crystal structure of EBOV GP (Protein Data Bank [PDB] code 3CSY) (27) as a template. The sequence alignment between MARV and EBOV GPs was based on that previously reported by Lee et al. (27). One hundred models of the first construction were generated using the automodel class in Modeller 9v6 (35), and the model with the lowest value of the Modeller objective function was selected. Next, to fill the gap of some potential loop conformation that the structural template of Zaire EBOV GP lacks (residues 174 to 197, 208 to 218, and 272 to 291 in the Angola GP numbering that correspond to residues 190 to 213, 224 to 225, and 279 to 298 in Zaire EBOV GP, respectively), two hundred models were generated by the loop model class (14). The best loop model was chosen by a combination of the Modeller objective function value and the discrete optimized protein energy (DOPE) statistical potential score (38). Then, the model, after addition of hydrogen atoms, was refined by energy minimization (EM) with the minimization protocols in the Discovery Studio 2.1 software package (Accelrys, San Diego, CA), using a CHARMM force field. Steepest descent, followed by conjugate gradient minimizations, was carried out until the root mean square (RMS) gradient was less than or equal to 0.01 kcal/mol/Å. The generalized Born implicit solvent model (43, 47) was used to model the effects of solvation. The model of Angola GP was finally evaluated by using PROCHECK (26), WHAT_CHECK (22), and Verify3D (10).
RESULTS
Efficiency of C-type lectin-mediated entry differs between MARV strains.
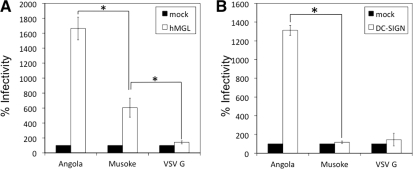
We generated VSVΔG* bearing VSV G (VSV-VSV G), VSVΔG* bearing Angola GP (VSV-Angola), or VSVΔG* bearing Musoke GP (VSV-Musoke), and the infectivities of these viruses in K562/hMGL or K562/DC-SIGN cells were compared (Fig. 1). No significant enhancement of VSV-VSV G infectivity was seen in these C-type lectin-expressing cells. Consistent with a previous study (46), the viruses infected K562/hMGL cells more efficiently than they infected control K562/mock cells. In K562/DC-SIGN cells, the difference was observed only for VSV-Angola infectivity. It was noted that VSV-Angola showed significantly higher infectivity in these C-type lectin-expressing cells than VSV-Musoke, as was seen between Zaire and Reston EBOVs (46).
FIG. 1.
Infectivity of VSVΔG* pseudotyped with MARV GPs in K562 cells expressing the C-type lectins. The infectivities of VSV-Angola and -Musoke were standardized using Vero E6 cells, as described in Materials and Methods, and approximately the same titers of viruses were used to infect K562/mock, K562/hMGL, and K562/DC-SIGN cells. The infected cells were counted using a flow cytometer, and the percentages of infectivity (i.e., relative infectivities) in K562/hMGL (A) and K562/DC-SIGN (B) cells were determined by setting the number of the infected K562/mock cells to 100% (46). All experiments were done in triplicate, and average results and standard deviations are shown. Statistical significance was determined by Student's t test. *, P < 0.05.
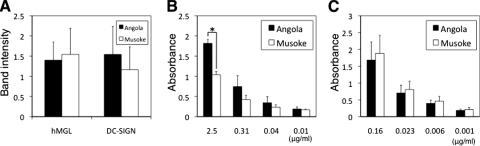
hMGL and DC-SIGN bind to MARV GPs in a different manner.
To test the attachment of VSV-Angola and -Musoke to the surfaces of the cells expressing C-type lectins, a direct binding assay was performed (Fig. 2A). In both K562/hMGL and K562/DC-SIGN cells, only limited differences of the viruses attached on the cell surfaces were observed. For more quantitative analysis of the binding of MARV GPs to the C-type lectins, we next carried out a lectin-ELISA using soluble forms of hMGL and DC-SIGN and purified viruses (Fig. 2B and C). We found that both lectins bound to Angola and Musoke GPs in a dose-dependent manner and that hMGL had slightly higher ability to bind to Angola GPs than to bind to Musoke GPs, whereas DC-SIGN similarly bound to both GPs, confirming the different glycan specificities of these lectins (i.e., hMGL and DC-SIGN preferentially react with O-glycans and high-mannose-type N-glycans, respectively) (11, 21, 44).
FIG. 2.
Binding affinity of the C-type lectins to VSVΔG* pseudotyped with MARV GPs. (A) The amounts of VSV-Angola and -Musoke that attached on K562/hMGL or K562/DC-SIGN cells were shown as band intensities of VSV matrix protein. (B, C) A lectin-ELISA was performed, using purified VSV-Angola and -Musoke as antigens. Biotinylated recombinant soluble hMGL (B) and DC-SIGN ECD (C) were incubated at the indicated concentrations and visualized, as described in Materials and Methods. All experiments were done in triplicate, and average results and standard deviations are shown. Statistical significance was determined by Student's t test. *, P < 0.05.
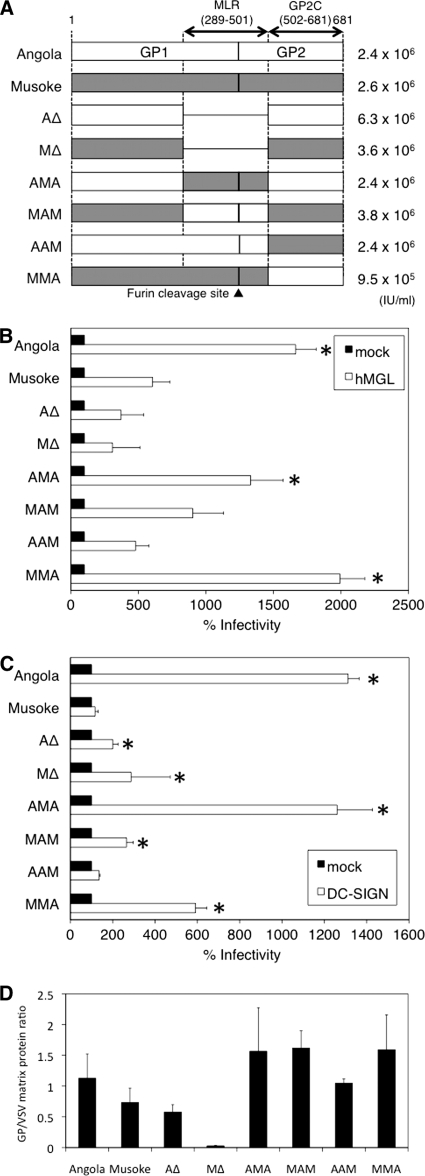
MLRs and GP2 are important for efficient entry mediated by C-type lectins.
MLRs of filoviruses have been shown to play an important role in interaction with the C-type lectins. To ascertain the contribution of the MLR of MARV GP to C-type lectin-mediated entry, we first constructed MLR-deletion mutants (AΔ and MΔ) (Fig. 3A) and examined the infectivities of VSVΔG* pseudotyped with these mutant GPs (VSV-AΔ and -MΔ) in Vero E6, K562/hMGL, and K562/DC-SIGN cells. VSV-AΔ and -MΔ showed no defects in their infectivities in Vero E6 cells, consistent with a previous study (32), indicating that glycosylation in the MLR and GP cleavage by furin are not essential to infect Vero E6 cells. In contrast, these viruses infected K562 cells expressing the C-type lectins much less efficiently than VSVΔG* pseudotyped with full-length wild-type GPs (Fig. 3B and C). These results indicate the major contribution of the MLR to C-type lectin-mediated entry of MARV.
FIG. 3.
Infectivity of VSVΔG* pseudotyped with the deletion or chimeric mutant GPs in C-type lectin-expressing cells. (A) The names of the MARV mutant GPs and the relevant amino acid positions are shown in the schematic. The number of infectious units determined for each virus in Vero E6 cells are shown on the right. (B, C) The relative infectivities of the viruses in K562/hMGL (B) and K562/DC-SIGN (C) cells were determined, as described in the legend of Fig. 1. All experiments were done in triplicate, and average results and standard deviations are shown. Statistical significance was determined (compared to the infectivity of VSV-Musoke in each K562/hMGL or K562/DC-SIGN cell) by Student's t test. *, P < 0.05. (D) The amounts of mutant GPs incorporated within the pseudotyped VSVΔG* were quantitated by using Western blotting of purified virions. Band intensities of MARV GPs and VSV matrix protein were determined, and their ratios are shown.
Next, we constructed chimeric GPs whose MLRs were swapped (AMA and MAM) (Fig. 3A), and the infectivities of VSVΔG* pseudotyped with these chimeric GPs (VSV-AMA and VSV-MAM) were tested (Fig. 3B and C). Unexpectedly, the relative infectivity of VSV-AMA in K562 cells expressing the C-type lectins was significantly higher than that of VSV-Musoke and similar to that of VSV-Angola. Replacement of the MLR of Musoke GP with that of Angola GP (MAM) showed only minimal effects on the enhancement of infectivity in the C-type lectin-expressing cells if compared with VSV-Musoke infectivity.
We finally replaced amino acid positions 502 to 681 of the GP2 regions (GP2C) of each (AAM and MMA) (Fig. 3A) and found that VSVΔG* pseudotyped with the chimeric Angola GP that had Musoke GP2C (VSV-AAM) infected both K562/hMGL and K562/DC-SIGN cells less efficiently than VSV-Angola (Fig. 3B and C), and the relative infectivities of VSV-AAM were similar to that of VSV-Musoke in both C-type lectin-expressing cell types. In contrast, the infectivities of VSV-MMA in both types of cells were significantly higher than that of VSV-Musoke or -AAM. These results indicate that GP2C is critical for the difference in the efficiency of C-type lectin-mediated entry between VSV-Angola and -Musoke. It was confirmed that all the chimeric GPs were similarly incorporated into virions (Fig. 3D). MΔ was not clearly detected by Western blotting. It was most likely due to the lack of the MLR containing many specific epitopes, resulting in the different reactivity of polyclonal serum to MΔ. We further confirmed that fully functional GPs were incorporated into VSV virions, since there is no significant difference in the infectivities in Vero E6 cells among these viruses.
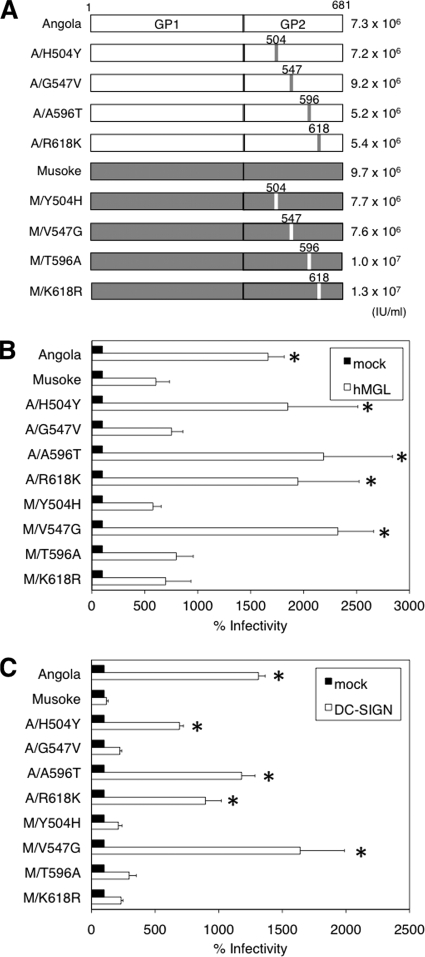
Substitution of an amino acid at position 547 in the GP2 region influences the efficiency of C-type lectin-mediated entry.
There are four different amino acids in GP2C between the Angola and Musoke GPs. To identify which amino acid(s) contributes to the different ability of C-type lectin-mediated entry between the Angola and Musoke strains, the following eight mutant GPs that contain single-amino-acid substitutions were constructed: four Angola-based mutant GPs (A/H504T, A/G547V, A/A596T, and A/R618K) and four Musoke-based mutant GPs (M/T504H, M/V547G, M/T596A, and M/K618R) (Fig. 4A). The infectivity levels of VSVΔG* pseudotyped with these mutant GPs in K562/hMGL or K562/DC-SIGN cells were compared (Fig. 4B and C). While the mutations at position 504, 596, or 618 did not affect the infectivity of the respective viruses in cells expressing the C-type lectins, the infectivities of VSVΔG* pseudotyped with mutant GPs with substitution at position 547 (VSV-A/G547V and -M/V547G) were clearly switched (i.e., the relative infectivities of VSV-Angola and -M/V547A in the C-type lectin-expressing cells were comparable and higher than those of VSV-Musoke and -A/G547V).
FIG. 4.
Infectivity of VSVΔG* pseudotyped with the single-amino-acid mutant GPs in the C-type lectin-expressing cells. (A) The names of the MARV GP mutants and the positions of substituted amino acids are shown in the schematic. The number of infectious units determined for each virus in Vero E6 cells are shown on the right. (B, C) The relative infectivities of the viruses in K562/hMGL (B) and K562/DC-SIGN (C) cells were determined, as described in the legend of Fig. 1. All experiments were done in triplicate, and average results and standard deviations are shown. Statistical significance was determined (compared to the infectivity of VSV-Musoke in each K562/hMGL or K562/DC-SIGN cell) by Student's t test. *, P < 0.05.
Infectivities of VSV-Angola and -Musoke are reduced in different manners by cathepsin inhibitors in the C-type lectin-expressing cells.
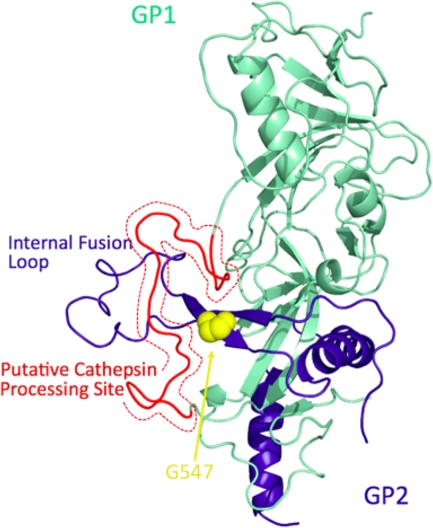
Because the GP binding affinity for C-type lectins (i.e., attachment) did not seem essential for the different ability levels of C-type lectin-mediated entry between the Angola and Musoke strains, we then focused on the following steps of viral entry. In EBOV and human coronavirus entry, it has been reported that proteolysis of GP by cellular endosomal cysteine proteases cathepsins B and/or L is necessary (4, 23, 24, 37). A three-dimensional model of Angola GP revealed that glycine at position 547 of Angola GP is presumed to form a β strand included in the internal fusion loop and is in close proximity to the putative cathepsin processing site (Fig. 5) (9, 27). Thus, we hypothesized that the amino acid change at position 547 affected the efficiency of cathepsin processing, which might lead to membrane fusion.
FIG. 5.
Three-dimensional structure of the Angola GP monomer. The crystal structure of EBOV GP (PDB code 3CSY) was used as a template for homology modeling. GP1 (lime green) and GP2 (dark blue) are shown as ribbon models. Glycine at position 547 (G547, yellow) is shown as a space-filling model. The putative cathepsin cleavage site (amino acid residues 174 to 197 of Angola GP, corresponding to amino acid residues 190 to 213 of Zaire EBOV GP) is colored in red. This figure was prepared using PyMOL (DeLano Scientific LLC).
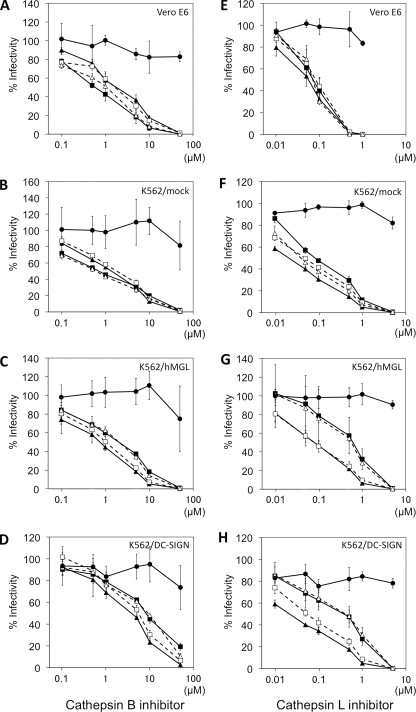
To test our hypothesis, VSVΔG* pseudotyped with wild-type or mutant (A/G547V and M/V547G) GPs was analyzed by comparing the infectivities of these viruses in Vero E6, control K562/mock, K562/hMGL, and K562/DC-SIGN cells pretreated with cathepsin inhibitors (Fig. 6). The infectivities of all the viruses were reduced by both of the inhibitors in a dose-dependent manner in all cells tested, suggesting that the proteolysis of GP by cathepsins B and/or L is also required for MARV entry. Interestingly, the infectivities of VSV-Angola and -M/V547G in K562 cells expressing the C-type lectins were less effectively reduced by these cathepsin inhibitors than those of VSV-Musoke and -A/G547V, whereas in Vero E6 and K562/mock cells, the differences in the infectivity at each concentration of the inhibitors were limited among the viruses. Paired Student's t test revealed significant differences (P < 0.01) in the following pairs: VSV-Angola and -Musoke, VSV-Angola and -A/G547C, and VSV-Musoke and -M/V547G (Fig. 6C, G, and H). And in Fig. 6D, the significant differences among these viruses were observed at a concentration of 10 μM by Student's t test. The infectivities of VSVΔG* pseudotyped with the other mutant GPs (i.e., VSV-A/H504T, -A/A596T, -A/R618K, -M/T504H, -M/T596A, and -M/K618R) were reduced by these cathepsin inhibitors similar to those of VSVΔG* pseudotyped with the respective wild-type GPs (data not shown).
FIG. 6.
Inhibition of virus infectivity by cathepsin inhibitors. Vero E6 (A and E), K562/mock (B and F), K562/hMGL (C and G), and K562/DC-SIGN (D and H) cells were pretreated with cathepsin B inhibitor (A, B, C, and D), cathepsin L inhibitor (E, F, G, and H), or dimethyl sulfoxide (DMSO) for 3 h and then infected with VSV-Angola (closed square), -Musoke (closed triangle), -A/G547V (open square), -M/V547G (open triangle) or -VSV G (closed circle). The number of infected cells, given in DMSO-treated cells, was used to set the 100% infectivity level for each cell type, and the relative infectivity was determined at each concentration of the inhibitors. All experiments were done in triplicate, and average results and standard deviations are shown.
DISCUSSION
It has been shown that cellular C-type lectins are utilized for the attachment of several viruses to host cells. hMGL, which was originally founded as a macrophage-specific C-type lectin recognizing galactose/N-acetylgalactosamine, is expressed in monocyte-derived DCs and macrophages (44), and it was demonstrated that hMGL promoted the infection of EBOV and MARV (46). DC-SIGN, which recognizes high-mannose-type N-glycans and plays an important role in regulating the immune system (53), has also been shown to promote infection by several viruses (e.g., Ebola, Marburg, human immunodeficiency, hepatitis C, measles, dengue, and influenza viruses) (49, 53). A liver-specific C-type lectin, ASGP-R, which recognizes galactose in carbohydrate side chains, has been shown to be exploited for MARV infection of hepatocytes (3) and is thought to be one of the possible determinants of hepatotropism of MARV (17). Taken together, increased infection of these cells expressing C-type lectins and subsequent destruction of the host immune functions and coagulation system may be crucial for the pathogenesis of filoviruses. Our previous study (46) and the present study show that the different abilities used to utilize the C-type lectins among filoviruses to promote cellular entry might be correlated with the pathogenicities of the viruses. In vivo study may be needed to provide a direct link between the pathogenicity of MARV and its ability to use C-type lectins for entry into target cells.
Using deletion mutant GPs, we found that both hMGL and DC-SIGN principally recognized MLRs. Amino acid comparison between Angola and Musoke GPs indicates that the similarity of their MLRs is 86.4% (data not shown). The numbers of potential O-glycosylation sites vary between Angola and Musoke GPs (the number of these sites for Musoke GP is less than the number of these sites for Angola GP), whereas the potential N-glycosylation sites are relatively conserved, supporting our observation that hMGL, but not DC-SIGN, bound more efficiently to Angola GP than to Musoke GP in the lectin-ELISA. However, using chimeric mutant GPs, we showed that the structure of the MLR itself was not essential for the different levels of infectivity between VSV-Angola and -Musoke in K562 cells expressing these C-type lectins, suggesting that the capacity of the GP for binding to C-type lectins through the MLR (i.e., the glycosylation pattern of MLR) is not the only factor contributing to the efficiency of C-type lectin-mediated entry. Indeed, we identified that the amino acid at position 547 in GP2, but not in the MLR, was critical for the different efficiency levels of C-type lectin-mediated entry between VSV-Angola and -Musoke. It is of interest to confirm the importance of this amino acid in MARV infection by using a reverse genetics approach.
In our three-dimensional model, it seemed unlikely that glycine/valine at position 547 directly influenced the binding to the putative specific receptors, since substitution of this amino acid did not affect the infectivity of pseudotyped viruses in Vero E6 or control K562 cells (data not shown), and this amino acid was not located around the putative receptor-binding domain (9, 25). We showed that the effects of cathepsin inhibitors on the infectivity differ between Angola and Musoke only in the C-type lectin-expressing cells, and the single-amino-acid substitution at position 547 altered the effects of cathepsin inhibitors. However, no significant difference in the susceptibility to cathepsins was seen in direct digestion assays in vitro using soluble forms of the C-type lectins and purified virions (data not shown). These results suggest that glycine at position 547 increases sensitivity of GPs to endosomal cathepsins during C-type lectin-mediated entry, but our in vitro digestion assay did not provide actual conditions for interaction between GPs and C-type lectins in endosomes. It may be also possible that when the viruses are internalized to endosomes through the interaction with C-type lectins, (i) the amino acid at position 547 affects the flexibility of the fusion loop and/or the efficiency of conformational change, and (ii) glycine at position 547 weakens GP1-GP2 interaction, resulting in reduced cathepsin dependence in virus entry, as reported with EBOV GP (51). It is interesting to clarify how this amino acid contributes to the intramolecule interaction required for GP functions.
In summary, our data suggest that the efficiency of C-type lectin-mediated entry of filoviruses is determined not only by direct interaction between GP and C-type lectins but also by some mechanisms underlying endosomal entry, such as proteolytic processing, and likely by cathepsins or membrane fusion machinery. Although further investigations are required to prove our hypotheses, this study provides new insights into understanding the molecular basis of the C-type lectin-mediated entry of filoviruses, which may have a possible link to their pathogenicity.
Acknowledgments
We thank Hiroko Miyamoto, Ayaka Yokoyama, Teiji Murakami, and Aiko Ohnuma for technical assistance and Kim Barrymore for editing the manuscript.
This work was supported by Research Fellowships for Young Scientists from the Japan Society for the Promotion of Science, by Takeda Science Foundation, by a Grant-in-Aid for Scientific Research on Priority Areas (grant 19041001), and in part by the Program of Founding Research Centers for Emerging and Reemerging Infectious Diseases (grant 05021011) and the Global COE Program “Establishment of International Collaboration Centers for Zoonosis Control” (F-001) from the Ministry of Education, Culture, Sports, Science and Technology (MEXT), Japan (http://www.mext.go.jp/english/index.htm).
The funders had no role in study design, data collection and analysis, the decision to publish, or preparation of the manuscript.
Footnotes
Published ahead of print on 10 March 2010.
REFERENCES
- 1.Alvarez, C. P., F. Lasala, J. Carrillo, O. Muñiz, A. L. Corbí, and R. Delgado. 2002. C-type lectins DC-SIGN and L-SIGN mediate cellular entry by Ebola virus in cis and in trans. J. Virol. 76:6841-6844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baribaud, F., S. Pöhlmann, G. Leslie, F. Mortari, and R. W. Doms. 2002. Quantitative expression and virus transmission analysis of DC-SIGN on monocyte-derived dendritic cells. J. Virol. 76:9135-9142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Becker, S., M. Spiess, and H. D. Klenk. 1995. The asialoglycoprotein receptor is a potential liver-specific receptor for Marburg virus. J. Gen. Virol. 76(Pt. 2):393-399. [DOI] [PubMed] [Google Scholar]
- 4.Chandran, K., N. J. Sullivan, U. Felbor, S. P. Whelan, and J. M. Cunningham. 2005. Endosomal proteolysis of the Ebola virus glycoprotein is necessary for infection. Science 308:1643-1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Daddario-DiCaprio, K. M., T. W. Geisbert, J. B. Geisbert, U. Ströher, L. E. Hensley, A. Grolla, E. A. Fritz, F. Feldmann, H. Feldmann, and S. M. Jones. 2006. Cross-protection against Marburg virus strains by using a live, attenuated recombinant vaccine. J. Virol. 80:9659-9666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Daddario-DiCaprio, K. M., T. W. Geisbert, U. Ströher, J. B. Geisbert, A. Grolla, E. A. Fritz, L. Fernando, E. Kagan, P. B. Jahrling, L. E. Hensley, S. M. Jones, and H. Feldmann. 2006. Postexposure protection against Marburg haemorrhagic fever with recombinant vesicular stomatitis virus vectors in nonhuman primates: an efficacy assessment. Lancet 367:1399-1404. [DOI] [PubMed] [Google Scholar]
- 7.Davis, K. J., A. O. Anderson, T. W. Geisbert, K. E. Steele, J. B. Geisbert, P. Vogel, B. M. Connolly, J. W. Huggins, P. B. Jahrling, and N. K. Jaax. 1997. Pathology of experimental Ebola virus infection in African green monkeys. Involvement of fibroblastic reticular cells. Arch. Pathol. Lab. Med. 121:805-819. [PubMed] [Google Scholar]
- 8.Dominguez-Soto, A., L. Aragoneses-Fenoll, E. Martin-Gayo, L. Martinez-Prats, M. Colmenares, M. Naranjo-Gomez, F. E. Borras, P. Munoz, M. Zubiaur, M. L. Toribio, R. Delgado, and A. L. Corbi. 2007. The DC-SIGN-related lectin LSECtin mediates antigen capture and pathogen binding by human myeloid cells. Blood 109:5337-5345. [DOI] [PubMed] [Google Scholar]
- 9.Dube, D., M. B. Brecher, S. E. Delos, S. C. Rose, E. W. Park, K. L. Schornberg, J. H. Kuhn, and J. M. White. 2009. The primed ebolavirus glycoprotein (19-kilodalton GP1,2): sequence and residues critical for host cell binding. J. Virol. 83:2883-2891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eisenberg, D., R. Lüthy, and J. U. Bowie. 1997. VERIFY3D: assessment of protein models with three-dimensional profiles. Methods Enzymol. 277:396-404. [DOI] [PubMed] [Google Scholar]
- 11.Feinberg, H., D. A. Mitchell, K. Drickamer, and W. I. Weis. 2001. Structural basis for selective recognition of oligosaccharides by DC-SIGN and DC-SIGNR. Science 294:2163-2166. [DOI] [PubMed] [Google Scholar]
- 12.Feldmann, H., S. T. Nichol, H. D. Klenk, C. J. Peters, and A. Sanchez. 1994. Characterization of filoviruses based on differences in structure and antigenicity of the virion glycoprotein. Virology 199:469-473. [DOI] [PubMed] [Google Scholar]
- 13.Feldmann, H., H. Bugany, F. Mahner, H. D. Klenk, D. Drenckhahn, and H. J. Schnittler. 1996. Filovirus-induced endothelial leakage triggered by infected monocytes/macrophages. J. Virol. 70:2208-2214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fiser, A., R. K. G. Do, and A. Šali. 2000. Modeling of loops in protein structures. Protein Sci. 9:1753-1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Geisbert, T. W., P. B. Jahrling, M. A. Hanes, and P. M. Zack. 1992. Association of Ebola-related Reston virus particles and antigen with tissue lesions of monkeys imported to the United States. J. Comp. Pathol. 106:137-152. [DOI] [PubMed] [Google Scholar]
- 16.Geisbert, T. W., and L. E. Hensley. 2004. Ebola virus: new insights into disease aetiopathology and possible therapeutic interventions. Expert Rev. Mol. Med. 6:1-24. [DOI] [PubMed] [Google Scholar]
- 17.Geisbert, T. W., K. M. Daddario-DiCaprio, J. B. Geisbert, H. A. Young, P. Formenty, E. A. Fritz, T. Larsen, and L. E. Hensley. 2007. Marburg virus Angola infection of rhesus macaques: pathogenesis and treatment with recombinant nematode anticoagulant protein c2. J. Infect. Dis. 196(Suppl. 2):S372-S381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Geyer, H., C. Will, H. Feldmann, H. D. Klenk, and R. Geyer. 1992. Carbohydrate structure of Marburg virus glycoprotein. Glycobiology 2:299-312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gramberg, T., H. Hofmann, P. Möller, P. F. Lalor, A. Marzi, M. Geier, M. Krumbiegel, T. Winkler, F. Kirchhoff, D. H. Adams, S. Becker, J. Münch, and S. Pöhlmann. 2005. LSECtin interacts with filovirus glycoproteins and the spike protein of SARS coronavirus. Virology 340:224-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gramberg, T., E. Soilleux, T. Fisch, P. F. Lalor, H. Hofmann, S. Wheeldon, A. Cotterill, A. Wegele, T. Winkler, D. H. Adams, and S. Pöhlmann. 2008. Interactions of LSECtin and DC-SIGN/DC-SIGNR with viral ligands: differential pH dependence, internalization and virion binding. Virology 373:189-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Higashi, N., K. Fujioka, N. Denda-Nagai, S. Hashimoto, S. Nagai, T. Sato, Y. Fujita, A. Morikawa, M. Tsuiji, M. Miyata-Takeuchi, Y. Sano, N. Suzuki, K. Yamamoto, K. Matsushima, and T. Irimura. 2002. The macrophage C-type lectin specific for galactose/N-acetylgalactosamine is an endocytic receptor expressed on monocyte-derived immature dendritic cells. J. Biol. Chem. 277:20686-20693. [DOI] [PubMed] [Google Scholar]
- 22.Hooft, R. W. W., C. Sander, M. Scharf, and G. Vriend. 1996. The PDBFINDER database: a summary of PDB, DSSP and HSSP information with added value. Comput. Appl. Biosci. 12:525-529. [DOI] [PubMed] [Google Scholar]
- 23.Kaletsky, R. L., G. Simmons, and P. Bates. 2007. Proteolysis of the Ebola virus glycoproteins enhances virus binding and infectivity. J. Virol. 81:13378-13384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kawase, M., K. Shirato, S. Matsuyama, and F. Taguchi. 2009. Protease-mediated entry via the endosome of human coronavirus 229E. J. Virol. 83:712-721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kuhn, J. H., S. R. Radoshitzky, A. C. Guth, K. L. Warfield, W. Li, M. J. Vincent, J. S. Towner, S. T. Nichol, S. Bavari, H. Choe, M. J. Aman, and M. Farzan. 2006. Conserved receptor-binding domains of Lake Victoria marburgvirus and Zaire ebolavirus bind a common receptor. J. Biol. Chem. 281:15951-15958. [DOI] [PubMed] [Google Scholar]
- 26.Laskowski, R. A., M. W. MacArthur, D. S. Moss, and J. M. Thornton. 1993. PROCHECK: a program to check the stereochemical quality of protein structures. J. Appl. Crystallogr. 26:283-291. [Google Scholar]
- 27.Lee, J. E., M. L. Fusco, A. J. Hessell, W. B. Oswald, D. R. Burton, and E. O. Saphire. 2008. Structure of the Ebola virus glycoprotein bound to an antibody from a human survivor. Nature 454:177-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lefrancois, L., and D. S. Lyles. 1982. The interaction of antibody with the major surface glycoprotein of vesicular stomatitis virus. I. Analysis of neutralizing epitopes with monoclonal antibodies. Virology 121:157-167. [PubMed] [Google Scholar]
- 29.Ligon, B. L. 2005. Outbreak of Marburg hemorrhagic fever in Angola: a review of the history of the disease and its biological aspects, p. 219-224. In C. R. Woods (ed.), Seminars in pediatric infectious diseases, vol. 16. Elsevier, New York, NY. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lin, G., G. Simmons, S. Pöhlmann, F. Baribaud, H. Ni, G. J. Leslie, B. S. Haggarty, P. Bates, D. Weissman, J. A. Hoxie, and R. W. Doms. 2003. Differential N-linked glycosylation of human immunodeficiency virus and Ebola virus envelope glycoproteins modulates interactions with DC-SIGN and DC-SIGNR. J. Virol. 77:1337-1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mahanty, S., and M. Bray. 2004. Pathogenesis of filoviral haemorrhagic fevers. Lancet Infect. Dis. 4:487-498. [DOI] [PubMed] [Google Scholar]
- 32.Manicassamy, B., J. Wang, E. Rumschlag, S. Tymen, V. Volchkova, V. Volchkov, and L. Rong. 2007. Characterization of Marburg virus glycoprotein in viral entry. Virology 358:79-88. [DOI] [PubMed] [Google Scholar]
- 33.Marzi, A., T. Gramberg, G. Simmons, P. Möller, A. J. Rennekamp, M. Krumbiegel, M. Geier, J. Eisemann, N. Turza, B. Saunier, A. Steinkasserer, S. Becker, P. Bates, H. Hofmann, and S. Pöhlmann. 2004. DC-SIGN and DC-SIGNR interact with the glycoprotein of Marburg virus and the S protein of severe acute respiratory syndrome coronavirus. J. Virol. 78:12090-12095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Powlesland, A. S., T. Fisch, M. E. Taylor, D. F. Smith, B. Tissot, A. Dell, S. Pöhlmann, and K. Drickamer. 2008. A novel mechanism for LSECtin binding to Ebola virus surface glycoprotein through truncated glycans. J. Biol. Chem. 283:593-602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Šali, A. 1995. Comparative protein modeling by satisfaction of spatial restraints. Mol. Med. Today 234:779-815. [DOI] [PubMed] [Google Scholar]
- 36.Schnittler, H. J., and H. Feldmann. 1999. Molecular pathogenesis of filovirus infections: role of macrophages and endothelial cells. Curr. Top. Microbiol. Immunol. 235:175-204. [DOI] [PubMed] [Google Scholar]
- 37.Schornberg, K., S. Matsuyama, K. Kabsch, S. Delos, A. Bouton, and J. White. 2006. Role of endosomal cathepsins in entry mediated by the Ebola virus glycoprotein. J. Virol. 80:4174-4178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shen, M., and A. Šali. 2006. Statistical potential for assessment and prediction of protein structures. Protein Sci. 15:2507-2524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Simmons, G., R. J. Wool-Lewis, F. Baribaud, R. C. Netter, and P. Bates. 2002. Ebola virus glycoproteins induce global surface protein down-modulation and loss of cell adherence. J. Virol. 76:2518-2528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Simmons, G., J. D. Reeves, C. C. Grogan, L. H. Vandenberghe, F. Baribaud, J. C. Whitbeck, E. Burke, M. J. Buchmeier, E. J. Soilleux, J. L. Riley, R. W. Doms, P. Bates, and S. Pöhlmann. 2003. DC-SIGN and DC-SIGNR bind Ebola glycoproteins and enhance infection of macrophages and endothelial cells. Virology 305:115-123. [DOI] [PubMed] [Google Scholar]
- 41.Slenczka, W. G. 1999. The Marburg virus outbreak of 1967 and subsequent episodes. Curr. Top. Microbiol. Immunol. 235:49-75. [DOI] [PubMed] [Google Scholar]
- 42.Smith, D. H., B. K. Johnson, M. Isaacson, R. Swanapoel, K. M. Johnson, M. Killey, A. Bagshawe, T. Siongok, and W. K. Keruga. 1982. Marburg-virus disease in Kenya. Lancet i:816-820. [DOI] [PubMed] [Google Scholar]
- 43.Still, W. C., A. Tempczyk, R. C. Hawley, and T. Hendrickson. 1990. Semianalytical treatment of solvation for molecular mechanics and dynamics. J. Am. Chem. Soc. 112:6127-6129. [Google Scholar]
- 44.Suzuki, N., K. Yamamoto, S. Toyoshima, T. Osawa, and T. Irimura. 1996. Molecular cloning and expression of cDNA encoding human macrophage C-type lectin. Its unique carbohydrate binding specificity for Tn antigen. J. Immunol. 156:128-135. [PubMed] [Google Scholar]
- 45.Takada, A., C. Robison, H. Goto, A. Sanchez, K. G. Murti, M. A. Whitt, and Y. Kawaoka. 1997. A system for functional analysis of Ebola virus glycoprotein. Proc. Natl. Acad. Sci. U. S. A. 94:14764-14769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Takada, A., K. Fujioka, M. Tsuiji, A. Morikawa, N. Higashi, H. Ebihara, D. Kobasa, H. Feldmann, T. Irimura, and Y. Kawaoka. 2004. Human macrophage C-type lectin specific for galactose and N-acetylgalactosamine promotes filovirus entry. J. Virol. 78:2943-2947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tsui, V., and D. A. Case. 2000. Theory and applications of the generalized Born solvation model in macromolecular simulations. Biopolymers 56:275-291. [DOI] [PubMed] [Google Scholar]
- 48.Volchkov, V. E., A. A. Chepurnov, V. A. Volchkova, V. A. Ternovoj, and H. D. Klenk. 2000. Molecular characterization of guinea pig-adapted variants of Ebola virus. Virology 277:147-155. [DOI] [PubMed] [Google Scholar]
- 49.Wang, S. F., J. C. Huang, Y. M. Lee, S. J. Liu, Y. J. Chan, Y. P. Chau, P. Chong, and Y. M. Chen. 2008. DC-SIGN mediates avian H5N1 influenza virus infection in cis and in trans. Biochem. Biophys. Res. Commun. 373:561-566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Weissenhorn, W., A. Carfí, K. H. Lee, J. J. Skehel, and D. C. Wiley. 1998. Crystal structure of the Ebola virus membrane fusion subunit, GP2, from the envelope glycoprotein ectodomain. Mol. Cell 2:605-616. [DOI] [PubMed] [Google Scholar]
- 51.Wong, A. C., R. G. Sandesara, N. Mulherkar, S. P. Whelan, and K. Chandran. 2010. A forward genetic strategy reveals destabilizing mutations in the ebolavirus glycoprotein that alter its protease dependence during cell entry. J. Virol. 84:163-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yang, Z. Y., H. J. Duckers, N. J. Sullivan, A. Sanchez, E. G. Nabel, and G. J. Nabel. 2000. Identification of the Ebola virus glycoprotein as the main viral determinant of vascular cell cytotoxicity and injury. Nat. Med. 6:886-889. [DOI] [PubMed] [Google Scholar]
- 53.Zhou, T., Y. Chen, L. Hao, and Y. Zhang. 2006. DC-SIGN and immunoregulation. Cell. Mol. Immunol. 3:279-283. [PubMed] [Google Scholar]