Abstract
Three patients with extensive necrotizing pneumonia due to Panton-Valentine leukocidin-positive Staphylococcus aureus strains and with aggravating factors (leukopenia count of less than 3 × 109/liter in all three cases and hemoptysis in two cases) were successfully treated with toxin-suppressing agents introduced rapidly after hospital admission.
CASE REPORT
Patient 1.
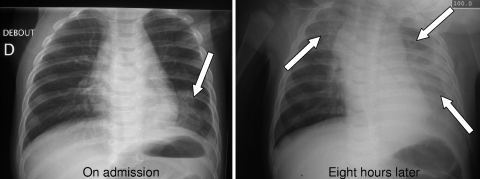
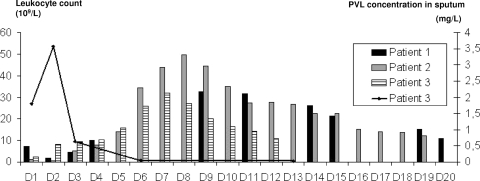
In December 2007, a 6-month-old boy presented to the emergency department with a 5-day history of a viral-like syndrome, including rhinorrhea, fever, and diarrhea. On admission, he had dry cough, moderate dyspnea, altered general status, and sepsis (39.4°C, heart rate of 198 beats per minute [bpm], tachypnea, and marbling). The initial laboratory tests showed a C-reactive protein level of 73.4 mg/liter and a total leukocyte count of 7.3 × 109/liter. Chest radiography revealed a basal left-sided infiltrate without pleural effusion (Fig. 1). Treatment with ceftriaxone and supportive measures was started, but his respiratory status worsened. Severe hypoxemia was present, with partial pressure of oxygen in arterial blood (PaO2) of 3.9 kPa under 3 liters/min of nasal oxygenotherapy. Eight hours after admission, a second chest radiograph revealed extensive bilateral infiltrate and pleural effusion (Fig. 1). He was admitted to the pediatric intensive care unit (PICU) with signs of septic shock (oliguria and altered mental status) which improved with fluid resuscitation. Laboratory tests showed lactic acidosis (pH 7.27 and lactic acid at 5.50 mmol/liter), hypoxemia, and leukopenia (1.83 × 109/liter) (Fig. 2). Pleural puncture yielded purulent fluid (40 ml) that tested negative by Gram staining and pneumococcal antigen detection. Staphylococcal necrotizing pneumonia was suspected in view of the rapid clinical deterioration, leukopenia, and negative tests for pneumococci. Vancomycin and clindamycin were added to ceftriaxone 15 h after admission. Staphylococcus aureus was detected in pleural fluid 24 h after admission, and culture yielded a Panton-Valentine leukocidin (PVL)-positive community-acquired methicillin-resistant S. aureus (MRSA) strain belonging to European clone sequence type 80 (ST80). The strain was susceptible to clindamycin, and the MIC to vancomycin was 1.5 mg/liter. The patient's status gradually improved, despite the need for pleural drainage because of recurrent pleural effusion. He was discharged from the PICU on day 7. Eight days after PICU admission, he remained febrile (39.3°C) and still had respiratory disorders (dyspnea and diminished left vesicular murmur), but the leukocyte count had risen to 32 × 109/liter (Fig. 2). Computed tomography (CT) revealed significant pleural effusion, multiple lung lesions, and pleural abscesses. Pleural decortication was performed. Intraoperative pleural samples were positive for the same strain of PVL-positive MRSA, and antibiotic treatment was switched to rifampin plus clindamycin. The boy was discharged from the hospital on day 28, on a 3-week course of oral antibiotics. Serologic tests and PCR were negative for influenza virus. Follow-up visits showed a healthy child with no clinical or radiographic signs of pulmonary relapse. The father had a history of furuncles but did not appear to carry S. aureus.
FIG. 1.
Rapid deterioration of radiographic pulmonary status in patient 1, with bilateral pneumonia and pleural effusion (arrows).
FIG. 2.
Time course of leukocyte counts and PVL expression during necrotizing pneumonia. Bars represent the leukocyte counts in each patient, and the line represents the evolution of PVL expression in patient 3. L, liter; D, day.
Patient 2.
A previously healthy 38-year-old man was admitted to the intensive care unit in February 2008 with a 48-hour history of an influenza-like syndrome. On admission, he had dyspnea with hypoxemia (partial pressure of oxygen [PO2] of 8.9 kPa and saturation of peripheral oxygen [SpO2] of 86% on room air), tachypnea (40 breaths per min), a heart rate of 130 bpm, and mild fever (37.9°C). The initial laboratory tests showed leukopenia (1.1 × 109/liter) with a polymorphonuclear leukocyte (PMN) count of 0.48 × 109/liter, thrombocytopenia (120 × 109/liter), an elevated C-reactive protein level (314 mg/liter), and a markedly elevated procalcitonin value (10 ng/ml; a normal value is <2 ng/ml). Chest radiography revealed bilateral pneumonia without pleural effusion. Treatment was started with ceftriaxone, amikacin, and levofloxacin. Six hours after admission, he developed septic shock, with acute respiratory distress syndrome, hemodynamic failure, and diffuse intravascular coagulation. He was intubated, and tracheal aspiration yielded hemorrhagic fluid containing grape-like clusters of Gram-positive cocci. Treatment was switched to vancomycin plus gentamicin. Eight hours later, methicillin-sensitive S. aureus (MSSA) (108 CFU/ml) was recovered in pure culture from an endotracheal aspiration sample. Necrotizing pneumonia due to PVL-positive S. aureus was suspected, and antibiotic treatment was again switched, 14 h after admission, to clindamycin (600 mg every 6 h) and linezolid (600 mg every 12 h), plus intravenous Ig (IVIg) (Tegeline at 1 g/kg of body weight/day on two consecutive days). The S. aureus isolate was methicillin and clindamycin susceptible, with a MIC to vancomycin of 2 mg/liter, carried the PVL genes, and belonged to ST8. After 48 h, the patient's respiratory status improved and his leukocyte count rose from 1.1 × 109/liter to 5.1 × 109/liter (Fig. 2); a CT scan showed bilateral lung compressions with fluid-air levels suggestive of necrotic lesions, as well as bilateral pleural effusion. The effusion was drained and found to be sterile. Ten days after admission, the patient developed a biological inflammatory syndrome along with intestinal and pulmonary failure. Clindamycin-associated colitis was suspected, and clindamycin was withdrawn. Colitis was not confirmed, but S. aureus persisted in pulmonary samples. Vancomycin was reintroduced in combination with rifampin, and linezolid was stopped. Twenty days after admission, vancomycin was replaced by oxacillin for 15 days. Serologic tests were positive for influenza virus on day 13. The patient was discharged from hospital on day 39. Follow-up visits showed a healthy man without relapse after 1 year.
Patient 3.
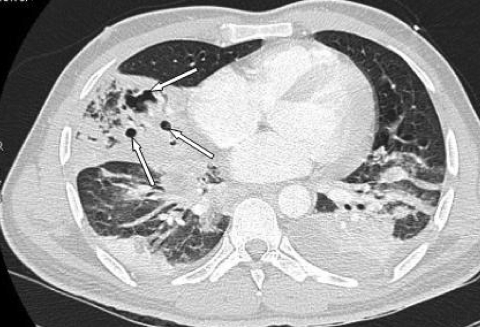
A previously healthy 35-year-old man from India was admitted to the emergency department in January 2009 with a 72-hour history of fever (38.9°C) and chest pain. On admission, he had dyspnea with hypoxemia and tachypnea (PO2 of 5.9 kPa and heart rate of 117 bpm). The initial laboratory tests showed leukopenia (2.2 × 109/liter with 1.9 × 109/liter PMN), a C-reactive protein level of 193 mg/liter, and negative urinary tests for pneumococcal antigen. Treatment was started with amoxicillin-clavulanate (1 g every 8 h) and ofloxacin (200 mg every 12 h). The patient quickly developed acute respiratory distress syndrome requiring noninvasive ventilation, as well as lactic acidosis (2.4 mmol/liter). Chest radiography showed bilateral pneumonia without pleural effusion. A CT scan confirmed bilateral pneumonia associated with disseminated necrotizing lesions (Fig. 3). Bronchoscopy showed hemorrhagic alveolar fluid. Methicillin-and clindamycin-susceptible S. aureus was recovered from bronchoalveolar lavage fluid in pure culture (108 CFU/ml); the MIC to vancomycin was 1.5 mg/liter. On day 2, the isolate was shown to carry the PVL genes. This MSSA strain was ST217 and belonged to clonal complex 22 (CC22). The antibiotic treatment was switched to linezolid (600 mg every 12 h), clindamycin (600 mg every 8 h), and ofloxacin (200 mg every 12 h), plus IVIg (Tegeline at 1 g/kg/day on three consecutive days). The patient's status improved, and respiratory support was withdrawn. His laboratory values improved at the same time, with an increase in the leukocyte count to 10.2 × 109/liter on day 3 and a decline in the C-reactive protein level. He was discharged from the intensive care unit on day 8. Treatment with linezolid and clindamycin was continued for 15 days, and the patient was discharged from the hospital on day 23. Serologic tests and PCR were negative for influenza virus. PVL in serial sputum samples was quantified with an enzyme-linked immunosorbent assay method (1); the concentration peaked at 3.6 mg/liter on day 2 and fell rapidly when antitoxin treatment was started (0.06 mg/liter on day 5) (Fig. 2). Follow-up consultations showed a healthy man with no clinical sign of pulmonary relapse. Two months later, a CT scan confirmed a quasi-complete regression of lung lesions.
FIG. 3.
A CT scan confirmed bilateral pneumonia associated with disseminated necrotizing lesions (arrows) in patient 3.
Panton-Valentine leukocidin (PVL)-positive Staphylococcus aureus strains have been linked to necrotizing pneumonia complicating influenza or other respiratory virus-caused disease (2, 8, 9, 14, 15, 17). Necrotizing pneumonia mainly affects children and young adults (median age, 14 years) and is fatal in one-half to three-quarters of cases (8, 9). Death usually occurs rapidly, after a median time of only 4 days.
The risk of superadded infection by PVL-producing S. aureus strains may be increased by influenza. Indeed, the incidence of documented S. aureus coinfection increased 5-fold in the United States during the 2004-2007 influenza seasons compared to the incidence in interepidemic periods (5). Kallen et al. identified 51 cases of community-acquired S. aureus pneumonia in 19 American states during the 2006-2007 influenza season, of which 79% involved methicillin-resistant strains and 51% were fatal (11). In Hageman et al.'s study (10), PVL genes were detected in 85% of community-acquired S. aureus strains causing pneumonia during the 2003-2004 influenza season.
The onset of leukopenia and hemoptysis in influenza patients with a rapidly extensive pneumonia syndrome is suggestive of necrotizing pneumonia and is independently associated with a poor outcome in multivariate analysis (9). In a previous series of 50 cases of staphylococcal necrotizing pneumonia, the survival rate was less than 10% among patients with leukocyte counts below 3 × 109/liter (9).
Necrotizing pneumonia being both rare and rapidly lethal, new therapeutic approaches are difficult to evaluate, partly for ethical reasons, thus placing the onus on experimental studies. PVL is overexpressed in the presence of β-lactams, but its expression can be blocked by combining a toxin-suppressing agent, such as clindamycin, linezolid, or rifampin, with bactericidal antibiotics acting on the cell wall (3, 4, 16). In addition, intravenous immunoglobulin (IVIg) blocks the lytic effect of PVL on polymorphonuclear cells (PMN) in vitro (6).
We describe three cases of severe and rapidly progressive necrotizing pneumonia due to PVL-positive strains of S. aureus, one of which was methicillin resistant. The three patients had minimal leukocyte counts below 3 × 109/liter, and two had hemoptysis. PVL was measured in sputum samples of one patient and was found to peak on the second hospital day. Clindamycin was added to the ongoing antibiotic regimen 15 h after hospital admission in one case, while clindamycin, linezolid, and IVIg were administered 14 h after admission in the second case and within 24 h in the third case. All three patients survived.
The three cases described here suggest that rapid administration of antitoxinic therapy with clindamycin/linezolid and/or IVIg may improve the outcome of PVL-associated staphylococcal necrotizing pneumonia (13), even when aggravating factors are present. Although based on three observations with the quantification of PVL in respiratory samples for one case only, it also suggests that necrotizing pneumonia may evolve through successive phases (Fig. 2). The initial phase, in which the leukocyte count is likely to be normal, is characterized by an influenza-like syndrome that may be followed by the onset of clinical or radiological pulmonary disorders. The following acute “toxinic” phase corresponds to the onset of pulmonary infiltration, hemoptysis, and leukopenia that, by analogy to in vitro and animal observations, may be a consequence of exacerbated inflammation induced by the massive influx of PMN and the subsequent lysis of these cells by PVL (7, 12). PVL production peaked during this phase in our patient 3, reaching a concentration of 3.6 mg/liter in sputum samples. Abscess fluid PVL concentrations above 1 mg/liter have been linked to larger abscess size (1). In an in vitro system, even very low PVL concentrations are capable of inducing leukopenia (7), and the effect of the direct administration of PVL in the mouse pneumonia model recalls the necrotic aspect of lung tissue at autopsy (8, 12). In our three patients, this toxinic phase may have been abrogated by the rapid administration of clindamycin, linezolid, and/or IVIg. The final phase is a more classical suppurative phase, with abscess formation, leukocyte counts of 20 × 109 to 30 × 109/liter (as in our three patients), and no detectable PVL. Dumitrescu et al. (3) showed that β-lactam agents upregulate PVL release and that the combination of β-lactams with clindamycin, rifampin, or linezolid suppressed PVL induction.
It is noteworthy that all three patients showed a marked clinical improvement despite the persistence of S. aureus in the lungs. This suggests that the main goal of treatment in the early life-threatening stages of the disease should be to counter the effects of the toxin, by inhibiting its production or blocking its biological effects, rather than to obtain bacterial clearance. A renewed increase in the leukocyte count would signal that this objective has been reached. However, bacterial clearance is clearly necessary for full recovery, and bactericidal treatment should therefore be given both concomitantly with antitoxinic treatment and after the crisis phase.
In conclusion, in the case of severe community-acquired pneumonia, empirical treatment active against the main culprit bacterial species (Streptococcus pneumoniae) should be started immediately. If a rapid fall in the leukocyte count is observed in this setting, then PVL-producing S. aureus should be suspected and an antibiotic that blocks toxin expression should be rapidly added to any ongoing antibiotic therapy (chosen according to the local epidemiological situation); the use of IVIg should be considered in the most severe cases. Clindamycin is active against most community MRSA isolates of clonal groups USA300 (in the United States) and ST80 (in Europe). Further clinical studies could allow confirmation of these recommendations.
Acknowledgments
We are very grateful to David Young for editorial assistance.
Footnotes
Published ahead of print on 3 February 2010.
REFERENCES
- 1.Badiou, C., O. Dumitrescu, M. Croze, Y. Gillet, B. Dohin, D. H. Slayman, B. Allaouchiche, J. Etienne, F. Vandenesch, and G. Lina. 2008. Panton-Valentine leukocidin is expressed at toxic levels in human skin abscesses. Clin. Microbiol. Infect. 14:1180-1183. [DOI] [PubMed] [Google Scholar]
- 2.Chetchotisakd, P., S. Anunnatsiri, S. Puapermpoonsiri, C. Prariyachatgul, and J. Chumpol. 2007. A rapidly fatal case of Panton-Valentine leukocidin positive Staphylococcus aureus necrotizing pneumonia in an HIV-infected patient. Southeast Asian J. Trop. Med. Public Health 38:690-694. [PubMed] [Google Scholar]
- 3.Dumitrescu, O., C. Badiou, M. Bes, M. E. Reverdy, F. Vandenesch, J. Etienne, and G. Lina. 2008. Effect of antibiotics, alone and in combination, on Panton-Valentine leukocidin production by a Staphylococcus aureus reference strain. Clin. Microbiol. Infect. 14:384-388. [DOI] [PubMed] [Google Scholar]
- 4.Dumitrescu, O., S. Boisset, M. Bes, Y. Benito, M. E. Reverdy, F. Vandenesch, J. Etienne, and G. Lina. 2007. Effect of antibiotics on Staphylococcus aureus producing Panton-Valentine leukocidin. Antimicrob. Agents Chemother. 51:1515-1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Finelli, L., A. Fiore, R. Dhara, L. Brammer, D. K. Shay, L. Kamimoto, A. Fry, J. Hageman, R. Gorwitz, J. Bresee, and T. Uyeki. 2008. Influenza-associated pediatric mortality in the United States: increase of Staphylococcus aureus coinfection. Pediatrics 122:805-811. [DOI] [PubMed] [Google Scholar]
- 6.Gauduchon, V., G. Cozon, F. Vandenesch, A. L. Genestier, N. Eyssade, S. Peyrol, J. Etienne, and G. Lina. 2004. Neutralization of Staphylococcus aureus Panton Valentine leukocidin by intravenous immunoglobulin in vitro. J. Infect. Dis. 189:346-353. [DOI] [PubMed] [Google Scholar]
- 7.Genestier, A. L., M. C. Michallet, G. Prevost, G. Bellot, L. Chalabreysse, S. Peyrol, F. Thivolet, J. Etienne, G. Lina, F. M. Vallette, F. Vandenesch, and L. Genestier. 2005. Staphylococcus aureus Panton-Valentine leukocidin directly targets mitochondria and induces Bax-independent apoptosis of human neutrophils. J. Clin. Invest. 115:3117-3127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gillet, Y., B. Issartel, P. Vanhems, J. C. Fournet, G. Lina, M. Bes, F. Vandenesch, Y. Piemont, N. Brousse, D. Floret, and J. Etienne. 2002. Association between Staphylococcus aureus strains carrying gene for Panton-Valentine leukocidin and highly lethal necrotising pneumonia in young immunocompetent patients. Lancet 359:753-759. [DOI] [PubMed] [Google Scholar]
- 9.Gillet, Y., P. Vanhems, G. Lina, M. Bes, F. Vandenesch, D. Floret, and J. Etienne. 2007. Factors predicting mortality in necrotizing community-acquired pneumonia caused by Staphylococcus aureus containing Panton-Valentine leukocidin. Clin. Infect. Dis. 45:315-321. [DOI] [PubMed] [Google Scholar]
- 10.Hageman, J. C., T. M. Uyeki, J. S. Francis, D. B. Jernigan, J. G. Wheeler, C. B. Bridges, S. J. Barenkamp, D. M. Sievert, A. Srinivasan, M. C. Doherty, L. K. McDougal, G. E. Killgore, U. A. Lopatin, R. Coffman, J. K. MacDonald, S. K. McAllister, G. E. Fosheim, J. B. Patel, and L. C. McDonald. 2006. Severe community-acquired pneumonia due to Staphylococcus aureus, 2003-04 influenza season. Emerg. Infect. Dis. 12:894-899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kallen, A. J., J. Brunkard, Z. Moore, P. Budge, K. E. Arnold, G. Fosheim, L. Finelli, S. E. Beekmann, P. M. Polgreen, R. Gorwitz, and J. Hageman. 2009. Staphylococcus aureus community-acquired pneumonia during the 2006 to 2007 influenza season. Ann. Emerg. Med. 53:358-365. [DOI] [PubMed] [Google Scholar]
- 12.Labandeira-Rey, M., F. Couzon, S. Boisset, E. L. Brown, M. Bes, Y. Benito, E. M. Barbu, V. Vazquez, M. Hook, J. Etienne, F. Vandenesch, and M. G. Bowden. 2007. Staphylococcus aureus Panton Valentine leukocidin causes necrotizing pneumonia. Science 315:1130-1133. [DOI] [PubMed] [Google Scholar]
- 13.Morgan, M. S. 2007. Diagnosis and treatment of Panton-Valentine leukocidin (PVL)-associated staphylococcal pneumonia. Int. J. Antimicrob. Agents 30:289-296. [DOI] [PubMed] [Google Scholar]
- 14.Roberts, J. C., S. P. Gulino, K. K. Peak, V. A. Luna, and R. Sanderson. 2008. Fatal necrotizing pneumonia due to a Panton-Valentine leukocidin positive community-associated methicillin-sensitive Staphylococcus aureus and influenza co-infection: a case report. Ann. Clin. Microbiol. Antimicrob. 7:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schefold, J. C., F. Esposito, C. Storm, D. Heuck, A. Kruger, A. Jorres, W. Witte, and D. Hasper. 2007. Therapy-refractory Panton Valentine leukocidin-positive community-acquired methicillin-sensitive Staphylococcus aureus sepsis with progressive metastatic soft tissue infection: a case report. J. Med. Case Rep. 1:165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stevens, D. L., Y. Ma, D. B. Salmi, E. McIndoo, R. J. Wallace, and A. E. Bryant. 2007. Impact of antibiotics on expression of virulence-associated exotoxin genes in methicillin-sensitive and methicillin-resistant Staphylococcus aureus. J. Infect. Dis. 195:202-211. [DOI] [PubMed] [Google Scholar]
- 17.Wenzel, J. J., J. Hentschel, W. Silvis, W. Permanetter, J. Mattes, B. Kochanowski, R. Herterich, W. Jilg, and H. J. Linde. 2009. Rapidly fatal necrotizing pneumonia in a 12-year-old boy caused by co-infection with parainfluenza virus type 1 and Panton-Valentine leukocidin (PVL)-positive methicillin-sensitive Staphylococcus aureus. Infection 37:75-77. [DOI] [PubMed] [Google Scholar]