Abstract
Background: Median BP obtained over a single dialysis treatment can diagnose hypertension among hemodialysis patients. Whether median BP is as useful to track change in BP is unknown.
Design, setting, participants, & measurements: Among patients participating in the dry-weight reduction in hypertensive hemodialysis patients (DRIP) trial, interdialytic ambulatory BP was recorded at baseline, 4 weeks, and 8 weeks. The mean interdialytic ambulatory BP was compared to the following recordings: predialysis on one dialysis treatment (Pre1), predialysis averaged over 2 weeks of dialysis treatment (Pre6), postdialysis on one dialysis treatment (Post1), postdialysis averaged over 2 weeks of dialysis treatment (Post6), and median intradialytic BP over one treatment.
Results: Pre1 was unable to detect change in ambulatory BP. Although Pre6 was able to detect change, it overestimated the ambulatory BP. On average, the magnitude of reduction in Post1 in response to probing dry-weight was nearly twice that obtained by ambulatory BP monitoring. Even Post6 overestimated the magnitude of reduction in BP at 8 weeks. Median systolic BP was responsive to probing dry-weight and neither overestimated nor underestimated the interdialytic ambulatory systolic BP at baseline or over time. However, the SD of the differences between median systolic BP and interdialytic ambulatory systolic BP varied from 16 to 20 mmHg.
Conclusions: Median intradialytic BP recordings can detect change in ambulatory BP evoked by reduction in dry-weight at the population level. Because of wide agreement limits between intradialytic and interdialytic BP, the individual prediction of ambulatory BP from median intradialytic BP can be misleading.
Hypertension is a common, modifiable cardiovascular risk factor, but among hemodialysis patients the prognostic significance of this risk factor continues to be debated (1,2). Whereas many have suggested that the treatment of hypertension is of little value in managing cardiovascular risk (3,4), others have argued that BP control is important (2,5,6). In part, these controversies have arisen because of inadequate BP assessment techniques in hemodialysis units. The accurate measurement of arterial pressure is the essential first step in managing this cardiovascular risk factor, yet the best way to diagnose hypertension among hemodialysis patients remains unknown (7,8).
There are several options available for assessment of hypertension among hemodialysis patients (7). These options include techniques to obtain BP both in and out of dialysis units (9). Out-of-dialysis unit BP measurements can provide a better assessment of overall BP because measurements are spaced out over a variety of volume and azotemic states, circumventing the problem of extremes of BP excursion that are typically obtained before and after dialysis (10). Two methods are commonly used to record BP outside the dialysis unit: interdialytic ambulatory BP and home BP measurements (11). Because it is time consuming and requires substantial resources, interdialytic ambulatory BP monitoring remains a research technique (12). This technique is unlikely to be implemented for the day-to-day management of hemodialysis patients. Even home BP monitoring requires additional equipment, education, and data management. Although the American Heart Association calls for universal home BP monitoring among all patients with hypertension, these actions have yet to be implemented (13).
In the dialysis unit, BP recordings are obtained every 30 minutes during dialysis, primarily to ensure the hemodynamic stability of patients during treatment. But the BPs so recorded are usually ignored when making a diagnosis of hypertension. We have previously shown that among long-term hemodialysis patients, median intradialytic BP can diagnose hypertension (14). The diagnostic test performance was excellent, but the study was cross-sectional in nature. Accordingly, it was unable to answer whether median BP could detect change in BP. In this study, which was a prospectively designed, randomized, controlled trial to explore dry-weight reduction versus conventional treatment among hypertensive hemodialysis patients, we asked the question whether median BP could detect the change in ambulatory BP measurement.
Our earlier study had shown the median BP obtained was sufficient to diagnose hypertension even when made on one dialysis occasion (14). However, most investigators have taken 2-week averaged predialysis or postdialysis BP measurements when they have compared these to ambulatory recordings (15,16). What remains unknown is the diagnostic performance of BP recording obtained just before or just after dialysis on a single occasion. Accordingly, in this study we asked the following questions: (1) Can measurement just before and after dialysis on a single occasion detect the change in BP evoked by dry-weight reduction? (2) Can measurement just before and after dialysis averaged over 2 weeks detect the change in BP evoked by dry-weight reduction? (3) Can median BP during a single dialysis treatment better detect the change in BP evoked by dry-weight reduction; and if so, what is the agreement between median BP during a single dialysis treatment and ambulatory BP?
Materials and Methods
Study Cohort
The analyses reported are post hoc results from a previously published dry-weight reduction in hypertensive hemodialysis patients (DRIP) trial (17). Briefly, we recruited patients ages 18 years or older on long-term hemodialysis for at least 3 months who had hypertension defined as mean interdialytic ambulatory BP of 135/85 mmHg or more. After a six-hemodialysis run-in phase, during which baseline data were collected, patients were randomized in 1:2 proportion into control group versus ultrafiltration trial group for 8 weeks. During this 24-dialysis treatment phase, patients were seen at each dialysis visit and had dry-weight probed as assessed by symptoms and signs related to hypovolemia (18,19). Ambulatory BP recordings were made at baseline, 4 weeks, and 8 weeks, and dialysis unit BP was recorded at each treatment. The Institutional Review Board of Indiana University and the Research and Development Committee of the Veterans' Affairs Medical Center approved this study, and all patients gave their written informed consent.
Intradialytic BP
Over a 2-week period at baseline and throughout the 24-dialysis trial (3 treatments per week × 8 weeks of intervention), BPs obtained during dialysis were recorded by dialysis technicians or nurses using the oscillometric BP monitor equipped with dialysis machines. Dialysis machines used were Fresenius H 2008, Fresenius K 2008, Cobe Centry III, and Cobe Plus and were maintained per the protocol of the respective dialysis units. To reflect clinical practice, no technique was specified for measurement of these BP measurements. Typically, measurements were made every 30 min. These measurements were entered into a relational database. Accuracy of data entry into the database was verified by at least two people.
Single predialysis or postdialysis readings were from the midweek dialysis treatment of the week of ambulatory BP monitoring. Averages over six treatments were generated for predialysis BP recordings at baseline, from 2 to 4 weeks and from 6 to 8 weeks. Similarly, averages for postdialysis BP recordings were generated. Median intradialytic BP was generated from the midweek dialysis treatment of the week of ambulatory BP monitoring. Thus, for the purposes of this study, median BP was defined using all BP recordings in the dialysis unit during a single midweek hemodialysis treatment.
Ambulatory BP Monitoring
Ambulatory BP monitoring was performed after the midweek hemodialysis session for 44 hours. Ambulatory BPs were recorded every 20 minutes during the day (6 a.m. to 10 p.m.) and every 30 minutes during the night (10 p.m. to 6 a.m.) using a Spacelab 90207 ABP monitor (SpaceLabs Medical Inc., Redmond, WA) in the nonaccess arm, as done previously (20). Recordings began immediately after hemodialysis and terminated immediately before the subsequent dialysis. Accuracy of ambulatory BP recordings was confirmed against auscultated BP at baseline. Data were analyzed using ABP Report Management System software, version 1.03.05 (SpaceLabs Medical Inc.). The mean interdialytic ambulatory BP served as the reference standard.
Statistical Analysis
We compared the change from baseline to 4 weeks in overall ambulatory BP, predialysis BP, postdialysis BP, and median BP in the control and ultrafiltration groups. In instances of predialysis and postdialysis BP, recordings over a single dialysis run or averaged over 2 weeks were analyzed separately. Next, we compared the change from baseline to 8 weeks. The mean change between methods was compared using a mixed-effects model to account for repeated observations (21). Bland Altman plots were created to show the limits of agreement (22).
The nominal level of significance was set at two-sided P of <0.05, and all statistical analyses were performed with Stata version 11 (StataCorp LP, College Station, TX).
Results
Among the 150 patients who participated, the average age was 54 years, 69% were men, 87% were black, 39% had diabetes, and the average vintage was 4.1 years. The average number of antihypertensive medications was 2.7, and 84% of the participants were using antihypertensive drugs. All patients were hemodialyzed three times weekly for an average of 235 minutes at a blood flow rate of 400 ml/min and dialysate flow rate of 765 ml/min. The baseline characteristics were well matched between groups.
As reported earlier, postdialysis weight was reduced by 0.9 kg at 4 weeks and resulted in −6.9 mmHg (95% confidence interval (CI): −12.4 to −1.3 mmHg; P = 0.016) change in systolic interdialytic ambulatory BP and −3.1 mmHg (95% CI: −6.2 to −0.02 mmHg; P = 0.048) change in diastolic ambulatory BP (Table 1). At 8 weeks, dry-weight was reduced 1 kg. From baseline, systolic ambulatory BP changed −6.6 mmHg (95% CI: −12.2 to −1.0 mmHg; P = 0.021), and diastolic ambulatory BP changed −3.3 mmHg (95% CI: −6.4 to −0.2 mmHg; P = 0.037).
Table 1.
Ambulatory BP levels in the DRIP Trial
| BP Component | Baseline | Change at 4 wk from Baseline | Change at 8 wk from Baseline |
|---|---|---|---|
| Systolic BP | |||
| control | 146.4 | −3.8 | −6.9a |
| control, 95% CI | 142.2 to 150.5 | −8.4 to 0.7 | −11.5 to −2.3 |
| ultrafiltration | 145.8 | −10.7b | −13.5b |
| ultrafiltration, 95% CI | 142.9 to 148.8 | −13.9 to −7.4 | −16.7 to −10.3 |
| difference between groups (ultrafiltration versus control) | −0.5 | −6.9c | −6.6c |
| difference between groups, 95% CI | −5.6 to 4.5 | −12.4 to −1.3 | −12.2 to −1.0 |
| P value of difference between groups | 0.8 | 0.02 | 0.02 |
| Diastolic BP | |||
| control | 83.4 | −3.0c | −3.9a |
| control, 95% CI | 80.2 to 86.6 | −5.5 to −0.5 | −6.5 to −1.4 |
| ultrafiltration | 82.9 | −6.1b | −7.2b |
| ultrafiltration, 95% CI | 80.6 to 85.2 | −7.9 to −4.3 | −9.0 to −5.4 |
| difference between groups (ultrafiltration versus control) | −0.5 | −3.1c | −3.3c |
| difference between groups, 95% CI | −4.4 to 3.4 | −6.2 to −0.0 | −6.4 to −0.2 |
| P value of difference between groups | 0.8 | 0.05 | 0.04 |
0.001 < P < 0.01.
P < 0.001.
0.01 < P < 0.05.
Predialysis Systolic BP
In the DRIP trial, BP measured predialysis on single occasions at baseline, 4 weeks, and 8 weeks was unable to detect change (model P = 0.06) (Table 2). When predialysis BP was averaged over 2 weeks during run-in at baseline, from 2 to 4 weeks, and from 6 to 8 weeks, change was detectable (model P < 0.0001). On average, the magnitude of reduction in systolic BP in response to probing dry-weight was similar to that obtained by ambulatory BP monitoring. However, averaged predialysis systolic BP overestimated interdialytic ambulatory systolic BP by 13 to 19 mmHg consistently (Table 2). The overestimation was not dependent on group assignment, visits, or their interactions.
Table 2.
Single and multiple predialysis BPs and their differences from ambulatory BP
| Characteristic | Systolic BP |
Difference from Ambulatory |
||||
|---|---|---|---|---|---|---|
| Baseline | Change at 4 wk from Baseline | Change at 8 wk from Baseline | Baseline | Change at 4 wk from Baseline | Change at 8 wk from Baseline | |
| Predialysis single | ||||||
| control | 156.6 | −2.7 | −5.8 | 11.2a | 0.6 | 1.7 |
| control, 95% CI | 150.0 to 163.3 | −10.4 to 5.0 | −14.2 to 2.5 | 5.1 to 17.3 | −6.4 to 7.5 | −5.8 to 9.3 |
| ultrafiltration | 158.6 | −7.0b | −8.2c | 13.3a | 3.4 | 4.9 |
| ultrafiltration, 95% CI | 153.6 to 163.5 | −12.7 to −1.3 | −14.2 to −2.1 | 8.8 to 17.8 | −1.7 to 8.5 | −0.6 to 10.4 |
| difference between groups (ultrafiltration versus control) | 1.9 | −4.2 | −2.3 | 2.2 | 2.8 | 3.2 |
| difference between groups 95% CI | −6.4 to 10.2 | −13.8 to 5.3 | −12.7 to 8.0 | −5.4 to 9.7 | −5.8 to 11.5 | −6.1 to 12.5 |
| P value of difference between groups | 0.7 | 0.4 | 0.7 | 0.6 | 0.5 | 0.5 |
| Predialysis multiple | ||||||
| control | 158.9 | −1.6 | −3.8 | 12.9a | 1.9 | 2.6 |
| control, 95% CI | 154.3 to 163.6 | −5.9 to 2.7 | −8.2 to 0.6 | 8.5 to 17.4 | −2.9 to 6.6 | −2.2 to 7.4 |
| ultrafiltration | 160.7 | −9.0a | −10.3a | 15.2a | 1.4 | 3.4 |
| ultrafiltration, 95% CI | 157.4 to 164.0 | −12.1 to −5.8 | −13.5 to −7.1 | 12.0 to 18.4 | −2.0 to 4.9 | −0.1 to 6.8 |
| difference between groups (ultrafiltration versus control) | 1.8 | −7.4c | −6.5b | 2.2 | −0.4 | 0.7 |
| difference between groups, 95% CI | −3.9 to 7.5 | −12.7 to −2.0 | −11.9 to −1.0 | −3.3 to 7.7 | −6.3 to 5.4 | −5.2 to 6.7 |
| P value of difference between groups | 0.5 | 0.007 | 0.02 | 0.4 | 0.9 | 0.8 |
P < 0.001.
0.01 < P < 0.05.
0.001 < P < 0.01.
Postdialysis Systolic BP
In contrast to predialysis systolic BP, postdialysis systolic BP measured on single occasions at baseline, 4 weeks, and 8 weeks was able to detect change (model P < 0.0001) (Table 3). On average, the magnitude of reduction in systolic BP in response to probing dry-weight was nearly twice that obtained by ambulatory BP monitoring. Furthermore, postdialysis systolic BP overestimated or underestimated interdialytic ambulatory systolic BP by variable amounts ranging from underestimating by 4.4 mmHg to overestimating by 6.1 mmHg. The estimation error was most for the control group at week 8 (P = 0.014).
Table 3.
Single and multiple postdialysis BPs and their differences from ambulatory BP
| Characteristic | Systolic BP |
Difference from Ambulatory |
||||
|---|---|---|---|---|---|---|
| Baseline | Change at 4 wk from Baseline | Change at 8 wk from Baseline | Baseline | Change at 4 wk from Baseline | Change at 8 wk from Baseline | |
| Postdialysis single | ||||||
| control | 141 | 0.6 | 2.6 | −4.4 | 3.8 | 10.5a |
| control, 95% CI | 134.3 to 147.7 | −7.0 to 8.2 | −5.8 to 11.0 | −11.0 to 2.1 | −3.8 to 11.3 | 2.1 to 18.9 |
| ultrafiltration | 144.6 | −12.7b | −10.6b | −0.6 | −2.3 | 2.5 |
| ultrafiltration, 95% CI | 139.7 to 149.6 | −18.4 to −7.0 | −16.7 to −4.5 | −5.5 to 4.2 | −8.0 to 3.3 | −3.5 to 8.5 |
| difference between groups (ultrafiltration versus control) | 3.6 | −13.3c | −13.2a | 3.8 | −6.1 | −8 |
| difference between groups 95% CI | −4.7 to 11.9 | −22.7 to −3.8 | −23.6 to −2.9 | −4.4 to 11.9 | −15.5 to 3.3 | −18.3 to 2.3 |
| P value of difference between groups | 0.4 | 0.006 | 0.01 | 0.4 | 0.2 | 0.1 |
| Postdialysis multiple | ||||||
| control | 141.7 | 0.4 | 3.3 | −4.3 | 3.8 | 9.6b |
| control, 95% CI | 136.6 to 146.7 | −4.5 to 5.2 | −1.6 to 8.2 | −9.3 to 0.7 | −1.2 to 8.8 | 4.5 to 14.7 |
| ultrafiltration | 143.1 | −7.0b | −10.7b | −2.4 | 3.3 | 2.9 |
| ultrafiltration, 95% CI | 139.6 to 146.7 | −10.5 to −3.5 | −14.2 to −7.2 | −5.9 to 1.1 | −0.3 to 7.0 | −0.8 to 6.5 |
| difference between groups (ultrafiltration versus control) | 1.5 | −7.4a | −14.0b | 1.9 | −0.4 | −6.7a |
| difference between groups, 95% CI | −4.7 to 7.7 | −13.3 to −1.4 | −20.0 to −7.9 | −4.2 to 8.0 | −6.6 to 5.7 | −12.9 to −0.4 |
| P value of difference between groups | 0.6 | 0.02 | <0.001 | 0.5 | 0.9 | 0.04 |
0.01 < P < 0.05.
P < 0.001.
0.001 < P < 0.01.
When postdialysis BP was averaged over 2 weeks during run-in at baseline and periodically over the trial, change was also detectable (model P < 0.0001). On average, the magnitude of reduction in systolic BP in response to probing dry-weight was similar to ambulatory BP at 4 weeks but nearly twice the reduction obtained by ambulatory BP monitoring at 8 weeks. Furthermore, averaged postdialysis systolic BP overestimated or underestimated interdialytic ambulatory systolic BP by variable amounts ranging from underestimating by 4.3 mmHg to overestimating by 5.3 mmHg (Table 3). Compared with ambulatory BP, averaged postdialysis BP was 9.6 mmHg higher in the control group at week 8 (P < 0.001) and 6.7 mmHg lower in the ultrafiltration group at week 8 (P = 0.036).
Median Systolic BP
Median systolic BP measured on single occasions at baseline, 4 weeks, and 8 weeks was able to detect change (model P < 0.0001) (Table 4). On average, the magnitude of reduction in systolic BP in response to probing dry-weight was similar to that obtained by ambulatory BP monitoring. Median systolic BP neither overestimated nor underestimated the interdialytic ambulatory systolic BP at baseline or over the course of the trial.
Table 4.
Single Median dialysis BP and its difference from ambulatory BP
| Characteristic | Systolic BP |
Difference from Ambulatory |
||||
|---|---|---|---|---|---|---|
| Baseline | Change at 4 wk from Baseline | Change at 8 wk from Baseline | Baseline | Change at 4 wk from Baseline | Change at 8 wk from Baseline | |
| Control | 144.5 | −0.1 | −2.5 | −0.9 | 3 | 4.9 |
| Control, 95% CI | 139.0 to 150.0 | −6.2 to 6.0 | −9.1 to 4.2 | −6.0 to 4.1 | −2.6 to 8.7 | −1.2 to 11.1 |
| Ultrafiltration | 145.9 | −10.6a | −10.8a | 0.6 | −0.1 | 2.3 |
| Ultrafiltration, 95% CI | 141.9 to 150.0 | −15.1 to −6.1 | −15.7 to −6.0 | −3.1 to 4.3 | −4.3 to 4.0 | −2.2 to 6.8 |
| Difference between groups (ultrafiltration versus control) | 1.4 | −10.5b | −8.3c | 1.5 | −3.2 | −2.6 |
| Difference between groups, 95% CI | −5.4 to 8.2 | −18.0 to −2.9 | −16.6 to −0.1 | −4.7 to 7.8 | −10.2 to 3.8 | −10.3 to 5.0 |
| P value of difference between groups | 0.7 | 0.007 | 0.05 | 0.6 | 0.4 | 0.5 |
P < 0.001.
0.001<P < 0.01.
0.01 < P < 0.05.
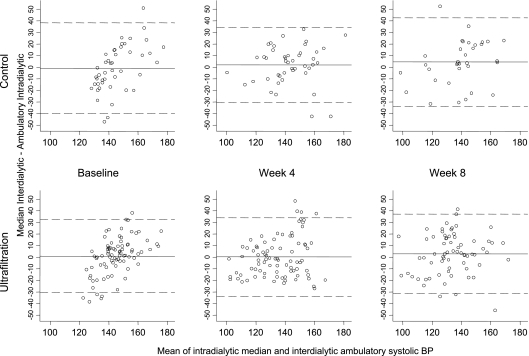
Bland-Altman plots to demonstrate bias and precision over the course of the trial are shown in Figure 1. Although none of the differences between median and interdialytic ambulatory BP measurements were significantly different from zero, the agreement limits were wide. The SD of the differences varied from 16 to 20 mmHg. Using the mixed model, the SD of the differences within patients between median systolic BP and interdialytic ambulatory systolic BP was 11.1 mmHg. The SD of the differences between median and ambulatory BP between patients was 13.4 mmHg.
Figure 1.
Bland-Altman plots showing mean differences between intradialytic median systolic BP and 44-hour interdialytic ambulatory systolic BP plotted against the means of the two BP recordings at baseline, week 4, and week 8 in the control and ultrafiltration groups. In the control group, paired measurements were available in 45, 45, and 34 patients at baseline, week 4, and week 8, respectively. In the ultrafiltration group, the corresponding pairs were available in 82, 85, and 68 patients. The mean differences were not different from zero at any time point. However, the limits of agreement were wide. The SD of the differences between BP measurements varied between 16 and 20 mmHg.
The changes in diastolic BP were similar and have not been shown.
Discussion
The results of this study extend our earlier report that demonstrated excellent diagnostic test performance of single median BP recording in diagnosing hypertension (14). Given that our previous report conducted in a separate cohort was limited to cross-sectional analysis, it was unable to answer the question of whether median BP can also detect change in ambulatory BP over time. This report firmly answers this question in 150 dialysis patients participating in a randomized, controlled trial that altered their BP in response to probing dry-weight.
The major findings of this study are the following: (1) A single measurement of predialysis or postdialysis measurement is either unable to detect clinically significant change in BP or can overestimate this change by a large amount. (2) Even with multiple measurements, predialysis BP can significantly overestimate ambulatory BP. (3) Even with multiple measurements, postdialysis BP can significantly overestimate the change in interdialytic BP. (4) A single determination of median intradialytic BP measurement can detect clinically significant change in BP without overestimation or underestimation of the magnitude of this change. (5) However, median BP cannot predict the individual change in ambulatory BP with a high degree of accuracy.
Several studies have compared the relationship of predialysis and postdialysis BP recordings with ambulatory BP and pointed out the problems associated with measurement (16). One such study measured BP in hemodialysis patients at arrival to the dialysis unit after 10 minutes of rest in a quiet room and compared them to interdialytic ambulatory BP (23). The authors reported that the BP on arrival to the hemodialysis unit was >20/10 mmHg higher than that in the previous 6 hours recorded by ambulatory BP in 15 (41%) of 36 patients. Even after resting for 10 minutes, BP was elevated in 19% of the patients. Whether this elevation is due to a white coat effect or evoked by a true increase in BP as a result of volume expansion or uremic toxin accumulation is unclear. Another study reported poor reproducibility of predialysis and postdialysis BP recordings compared with ambulatory BP (24). Thus, BP recordings measured just before or after dialysis appear to be inadequate surrogates for interdialytic ambulatory BP.
We used ambulatory BP as a reference standard because ambulatory BP recording is an accurate estimate of the arterial pressure and shares a stronger relationship with all-cause mortality compared with BPs obtained in the dialysis unit (25). Not only can ambulatory BP provide a better mean estimate of arterial pressure over the interdialytic period, recent studies using ambulatory BP monitoring have disclosed that systolic BP increases by approximately 1 mmHg every 4 hours, and diastolic BP increases by 1 mmHg every 8 hours (26). The BP fall during dialysis offsets the interdialytic rise in BP. The median interdialytic BP agrees closely with mean intradialytic recordings. Because many more measurements are available during the dialysis procedure compared with predialysis and postdialysis measurement and they span over a range of volume states, it is no surprise that compared with predialysis or postdialysis measurements, a better relationship is shared between median intradialytic BP with interdialytic ambulatory BP recordings.
This study found that even multiple measurements of predialysis or postdialysis BP were not superior to median BP obtained over just one dialysis treatment. This is consistent with our previous cross-sectional report, which revealed that the median BP of a single dialysis treatment had better diagnostic ability than the average of six predialysis or six postdialysis BPs alone. Thus, our study confirms the prior cross-sectional relationship of median intradialytic BP to interdialytic ambulatory BP and extends the utility of this simple measurement to track interdialytic BP longitudinally. Although median intradialytic BP recordings could detect change in BP without bias, the agreement limits with simultaneously measured interdialytic ambulatory BP measurements were wide. The SD of the difference between median systolic BP and interdialytic systolic BP was 16 to 20 mmHg. Thus, the limits of agreement between median intradialytic and mean interdialytic BP would span between 64 and 80 mmHg. These limits would be too wide to predict with any degree of certainty the change in true mean interdialytic ambulatory BP. Nonetheless, median intradialytic BP outperformed predialysis and postdialysis measurements alone in assessing clinically significant BP change in hemodialysis patients.
A shortcoming of our study is that the majority of the participants were black. Although race should not influence the measurement of BP, whether these data are applicable to nonblack individuals requires further studies. Given that this study was used to clarify the value of median intradialytic BP as a diagnostic test, we did not evaluate the prognostic significance of this risk factor. A merit of our study is the large number of intradialytic BP measurements that were prospectively collected in the setting of a randomized, controlled clinical trial.
There are several implications of our study. (1) Future guidelines should take into consideration the poor test performance of single and even multiple predialysis and postdialysis measurements to diagnose hypertension or to detect changes in BP (27). In fact, achievement of prescribed BP goals is associated with more hypotensive episodes when made on the basis of predialysis and postdialysis BP (28). Perhaps median intradialytic BP can be a better method to track BP longitudinally. (2) Because this BP is readily available, epidemiologists may want to reassess the prognostic significance of high or low BP and its change over time on cardiovascular events and mortality; this may better clarify the prognostic significance of median intradialytic BP. (3) For clinicians, our study shows that if home BP monitoring is not available or possible, then the consideration of intradialytic BP recordings may improve the diagnosis and management of hypertension among hemodialysis patients (29).
Disclosures
None.
Acknowledgments
This work was supported by grant number 2R01-DK062030-06 from the National Institutes of Health. We acknowledge the assistance of the dialysis staff at Dialysis Clinics Inc., Clarian Health, and the Roudebush Veterans' Affairs Medical Center and thank the faculty of the Division of Nephrology, who generously allowed us to study their patients.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This trial has been registered at www.clinicaltrials.gov (identifier NCT00067665).
References
- 1.Lacson E, Jr., Lazarus JM: The association between blood pressure and mortality in ESRD–not different from the general population? Semin Dial 20: 510– 517, 2007 [DOI] [PubMed] [Google Scholar]
- 2.Foley RN, Agarwal R: Hypertension is harmful to dialysis patients and should be controlled. Semin Dial 20: 518– 522, 2007 [DOI] [PubMed] [Google Scholar]
- 3.Kalantar-Zadeh K, Kilpatrick RD, McAllister CJ, Greenland S, Kopple JD: Reverse epidemiology of hypertension and cardiovascular death in the hemodialysis population: The 58th annual fall conference and scientific sessions. Hypertension 45: 811– 817, 2005 [DOI] [PubMed] [Google Scholar]
- 4.Li Z, Lacson E, Jr., Lowrie EG, Ofsthun NJ, Kuhlmann MK, Lazarus JM, Levin NW: The epidemiology of systolic blood pressure and death risk in hemodialysis patients. Am J Kidney Dis 48: 606– 615, 2006 [DOI] [PubMed] [Google Scholar]
- 5.Agarwal R: Hypertension and survival in chronic hemodialysis patients–past lessons and future opportunities. Kidney Int 67: 1– 13, 2005 [DOI] [PubMed] [Google Scholar]
- 6.Agarwal R: Exploring the paradoxical relationship of hypertension with mortality in chronic hemodialysis. Hemodialysis Int 8: 207– 213, 2004 [DOI] [PubMed] [Google Scholar]
- 7.Agarwal R: Assessment of blood pressure in hemodialysis patients. Semin Dial 15: 299– 304, 2002 [DOI] [PubMed] [Google Scholar]
- 8.Lazar AE, Smith MC, Rahman M: Blood pressure measurement in hemodialysis patients. Semin Dial 17: 250– 254, 2004 [DOI] [PubMed] [Google Scholar]
- 9.Agarwal R, Peixoto AJ, Santos SF, Zoccali C: Out-of-office blood pressure monitoring in chronic kidney disease. Blood Press Monit 14: 2– 11, 2009 [DOI] [PubMed] [Google Scholar]
- 10.Agarwal R, Light RP: Chronobiology of arterial hypertension in hemodialysis patients: Implications for home blood pressure monitoring. Am J Kidney Dis 54: 693– 701, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Agarwal R, Andersen MJ, Bishu K, Saha C: Home blood pressure monitoring improves the diagnosis of hypertension in hemodialysis patients. Kidney Int 69: 900– 906, 2006 [DOI] [PubMed] [Google Scholar]
- 12.Thompson AM, Pickering TG: The role of ambulatory blood pressure monitoring in chronic and end-stage renal disease. Kidney Int 70: 1000– 1007, 2006 [DOI] [PubMed] [Google Scholar]
- 13.Pickering TG, Miller NH, Ogedegbe G, Krakoff LR, Artinian NT, Goff D: Call to action on use and reimbursement for home blood pressure monitoring: A joint scientific statement from the American Heart Association, American Society Of Hypertension, and Preventive Cardiovascular Nurses Association. Hypertension 52: 10– 29, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agarwal R, Metiku T, Tegegne GG, Light RP, Bunaye Z, Bekele DM, Kelley K: Diagnosing hypertension by intradialytic blood pressure recordings. Clin J Am Soc Nephrol 3: 1364– 1372, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Agarwal R, Lewis RR: Prediction of hypertension in chronic hemodialysis patients. Kidney Int 60: 1982– 1989, 2001 [DOI] [PubMed] [Google Scholar]
- 16.Agarwal R, Peixoto AJ, Santos SF, Zoccali C: Pre and post dialysis blood pressures are imprecise estimates of interdialytic ambulatory blood pressure. Clin J Am Soc Nephrol 1: 389– 398, 2006 [DOI] [PubMed] [Google Scholar]
- 17.Agarwal R, Alborzi P, Satyan S, Light RP: Dry-weight reduction in hypertensive hemodialysis patients (DRIP): A randomized, controlled trial. Hypertension 53: 500– 507, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Charra B, Laurent G, Chazot C, Calemard E, Terrat JC, Vanel T, Jean G, Ruffet M: Clinical assessment of dry weight. Nephrol Dial Transplant 11[ Suppl 2]: 16– 19, 1996 [DOI] [PubMed] [Google Scholar]
- 19.Jaeger JQ, Mehta RL: Assessment of dry weight in hemodialysis: An overview. J Am Soc Nephrol 10: 392– 403, 1999 [DOI] [PubMed] [Google Scholar]
- 20.Agarwal R: Supervised atenolol therapy in the management of hemodialysis hypertension. Kidney Int 55: 1528– 1535, 1999 [DOI] [PubMed] [Google Scholar]
- 21.Holden JE, Kelley K, Agarwal R: Analyzing change: A primer on multilevel models with applications to nephrology. Am J Nephrol 28: 792– 801, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bland JM, Altman DG: Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1: 307– 310, 1986 [PubMed] [Google Scholar]
- 23.Mitra S, Chandna SM, Farrington K: What is hypertension in chronic haemodialysis? The role of interdialytic blood pressure monitoring. Nephrol Dial Transplant 14: 2915– 2921, 1999 [DOI] [PubMed] [Google Scholar]
- 24.Peixoto AJ, Santos SF, Mendes RB, Crowley ST, Maldonado R, Orias M, Mansoor GA, White WB: Reproducibility of ambulatory blood pressure monitoring in hemodialysis patients. Am J Kidney Dis 36: 983– 990, 2000 [DOI] [PubMed] [Google Scholar]
- 25.Alborzi P, Patel N, Agarwal R: Home blood pressures are of greater prognostic value than hemodialysis unit recordings. Clin J Am Soc Nephrol 2: 1228– 1234, 2007 [DOI] [PubMed] [Google Scholar]
- 26.Kelley K, Light RP, Agarwal R: Trended cosinor change model for analyzing hemodynamic rhythm patterns in hemodialysis patients. Hypertension 50: 143– 150, 2007 [DOI] [PubMed] [Google Scholar]
- 27.K/DOQI Workgroup: K/DOQI clinical practice guidelines for cardiovascular disease in dialysis patients. Am J Kidney Dis 45: S1– S153, 2005 [PubMed] [Google Scholar]
- 28.Davenport A, Cox C, Thuraisingham R: Achieving blood pressure targets during dialysis improves control but increases intradialytic hypotension. Kidney Int 73: 759– 764, 2007 [DOI] [PubMed] [Google Scholar]
- 29.Agarwal R, Satyan S, Alborzi P, Light RP, Tegegne GG, Mazengia HS, Yigazu PM: Home blood pressure measurements for managing hypertension in hemodialysis patients. Am J Nephrol 30: 126– 134, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]