Abstract
Latino immigrants in the United States are disproportionally impacted by the HIV epidemic but face barriers to clinic-based testing. We assessed a community-based strategy for rapid HIV testing by conducting “door-to-door” outreaches in apartments with predominately Latino immigrants in Durham, North Carolina, that has experienced an exponential growth in its Latino population. Eligible persons were 18 years or older, not pregnant, and reported no HIV test in the previous month. Participants were asked to complete a survey and offered rapid HIV testing. Of the 228 Latino participants, 75.4% consented to HIV testing. There was a high prevalence of sexual risk behaviors among participants, with 42.5% acknowledging ever having sex with a commercial sex worker (CSW). Most (66.5%) had no history of prior HIV testing. In bivariate analysis, perceived HIV risk, no history of HIV testing, sex with a CSW, sex in exchange for drugs or money, living with a partner, and alcohol use were significantly associated with test acceptance. In the multivariate analysis, participants who had never been tested for HIV were more likely to consent to rapid HIV testing than those who had tested in the past (adjusted odds ratio 2.5; 95% confidence interval [CI], 1.1, 5.6). Most participants supported rapid HIV testing in the community (97%). Door-to-door rapid HIV testing is a feasible and acceptable strategy for screening high-risk Latino immigrants in the community. Factors associated with HIV risk among Latino migrants and immigrants in the United States should be considered along with novel testing strategies in HIV prevention programs.
Introduction
The disproportionate effect of HIV/AIDS on the Latino population compared to whites has been an evident and persistent trend in the United States.1,2 Despite representing only 14% of the population, Latinos comprise 19% of AIDS cases in the United States.1 Latinos are more likely than whites to be concurrently diagnosed with HIV/AIDS and receive medical care later in their course of illness.1 A key to controlling the spread of HIV is early diagnosis of infection through expanded HIV testing.3 A study of HIV-infected persons revealed that although 73% had visited health care facilities prior to their diagnoses, there were missed opportunities during those visits to provide HIV testing.4 The Centers for Disease Control and Prevention (CDC) has since recommended opt-out HIV testing for all patients in health care settings.5 However, this strategy is likely to have a limited impact on Latinos in the United States, who may face multiple barriers when accessing health care for HIV-related services due to lack of acculturation and English language proficiency, illegal status, lack of formal education, and inadequate health insurance.6 The stigma associated with HIV, fear of disclosure, and lack of information about where to get tested are also barriers to HIV-testing in the Latino population.6–8
Community-based rapid HIV testing is a strategy that can provide HIV screening to Latino immigrants by overcoming some of the limitations of opt-out clinic-based testing. Rapid HIV testing in community-based testing locations such as free clinics has been found acceptable by both patients and test counselors, who preferred the reduced testing time and number of return visits for results when accompanied by high quality counseling.9 Rapid HIV testing can reach out to populations at high risk for HIV infection who are unaware of their status, and have been offered in nontraditional settings (e.g., worksites, health fairs, etc.) among high-risk individuals, including prison inmates, homeless and marginally housed populations, and men who have sex with men (MSM).10–13 Community-based organizations in seven U.S. cities recently demonstrated the feasibility of offering rapid HIV testing in outreach and community settings for members of minority groups and people at high risk for HIV infections.14
A novel community-based HIV testing strategy for Latino populations in the United States is the door-to-door approach, which involves bringing HIV information and education to individuals directly in their homes through the use of promotores, who are trained Latino lay community health workers. In this study, we explored (1) the feasibility of door-to-door rapid HIV testing in reaching at-risk Latinos who are unaware of their HIV status in a small metropolitan area in North Carolina, (2) the acceptability of this approach among Latinos in the community, and (3) the HIV risk factors of Latinos and their association with the likelihood of testing through this community-based strategy.
Methods
The study was reviewed and approved by the University of North Carolina at Chapel Hill Institutional Review Board (IRB). In addition, a Certificate of Confidentiality was obtained from the National Institute of Allergy and Infectious Diseases before study implementation to provide further protection for the privacy of study participants enrolled in sensitive research.
The study was conducted in Durham, North Carolina, a small metropolitan area with an estimated county population of 262,715 residents in 2008, of whom 11.9% are of Latino origin.15 North Carolina is considered one of the “rapid growth states” of the southern United States that has seen more than a doubling of Latinos since the 1990s,16 and Durham has experienced an estimated 68% increase in its Latino population in the last decade. Although the HIV rates decreased from 41.3 per 100,000 in 2006 to 38.1 per 100,000 in 2007, Durham County continues to have one of the highest rates of HIV/AIDS statewide.17
We identified apartment complexes with a large number of Latino residents in Durham County based on data from a prior study involving Latinos and HIV risk that did not include an HIV testing component.18 These predominantly Latino apartment complexes were lower income housing units located in urban areas throughout the county. From October 2006 to October 2007, we conducted outreach events on Saturday afternoons among a convenience sample of these apartment complexes.
Prior to the testing outreaches, promotores were identified from a local Latino community center and trained in research ethics and study methods using bilingual research staff and a research training module approved by the IRB. The promotores consisted of 3 male and 1 female Latino health educators who had prior experience in providing HIV education and conducting community outreach through the community center. During the outreaches, promotores knocked on apartment doors within the complexes to solicit participants. When a potential participant opened the door, promotores provided information to the person(s) in the household aged 18 and over regarding the study and recruited people to take part in the survey and rapid HIV testing. People congregating in parking lots and other outdoor areas in the apartment complexes were also solicited for participation. Eligible participants were at least 18 years of age, not pregnant, and reported no HIV test in the previous month. Individuals who had a history of known HIV infection and prior study enrollment were excluded from further participation.
After obtaining verbal informed consent from participants, promotores or other trained bilingual research staff administered the structured survey in a location that was convenient for the participant and where confidentiality could be ensured (i.e., inside their apartment, outdoors in the vicinity of the testing area away from others). The surveys were available in Spanish or English, and were administered by trained bilingual interviewers in the language of the participants' choice. For confidentiality, all surveys were assigned study codes in order to link the surveys to the test results. The survey consisted of 70 questions with closed-ended response categories and took approximately 15 min to complete. The questions covered demographics, risk factors including number of sexual partners in the past 6 months, prior sex with a commercial sex worker (CSW), sex in exchange for drugs or money, sex with the same gender, condom use, HIV testing history, and access to health care. Self-perceived risk for HIV was determined by asking “Do you think you are at risk for HIV?” Additional survey questions assessed acceptability of rapid HIV testing in the community (versus a clinic) and preferences about HIV testing method and location.
Upon survey completion, participants interested in undergoing confidential rapid HIV testing were asked by bilingual HIV counselors for additional written consent as required in the state at the time of study implementation. Pretest HIV counseling in Spanish or English was also provided by the trained counselors in accordance with current state HIV testing requirements. Participants who chose to do the survey only received brochures with general information about HIV infection, and note pads and pens for their participation. Participants who underwent testing received brochures with more detailed information on HIV testing, $5 gift cards, and condoms.
HIV-1/2 antigen testing was performed using oral swabs according to the manufacturer's instructions (Orasure Advanced®, Orasure, Inc., Bethlehem, PA). Storage for control and testing kits were maintained in the field according to CDC guidelines, and control kits were tested during each outreach event due to changes in testing area temperatures. After collection of oral fluid, specimens were immediately taken to a stable outdoor testing area at the apartment complex (i.e., a table set up in an area of the apartment grounds protected from heat and wind conditions, or a temperature-controlled van during cooler months). The rapid HIV tests were conducted following the CDC's guidelines for quality assurance of testing procedures.19 After 20 min, the results were determined by 1–2 trained research staff, and posttest counseling was provided to participants in a private location either in the participant's home or elsewhere in the apartment complex where confidentiality could be maintained. The HIV counselors were trained to provide post-test counseling to any participant with a positive rapid HIV test and to provide immediate referral to the local health department for confirmatory testing. Individuals found to be HIV positive after confirmatory testing were to be reported to the state health department as per North Carolina communicable disease requirements and referred for HIV care.
Survey responses were numerically coded and entered into SAS 9.1 (SAS Corporation, Cary, NC) for data analysis. Means, medians, and percents were calculated to describe sample demographics. The prevalence of HIV risk factors among this population was determined from the self-reported histories. The demographic factors and risk factors of participants who tested were compared to those who did not. Bivariate analyses were conducted to determine associations between factors and rapid HIV testing by estimating odds ratios (OR) with 95% confidence intervals (CI). Factors with p ≤ 0.05 in the bivariate analysis were entered into a multiple logistic regression model to determine each factor's independent association with testing.
To assess the feasibility of the door-to-door approach in providing rapid HIV testing to persons unaware of their HIV status, we determined the proportion of those tested who had no prior HIV testing. We also assessed the acceptability of our community-based rapid HIV testing strategy by calculating the proportion of participants who underwent testing among both eligible persons contacted by the promotores and all participants in the study. In addition, the proportion of those who preferred rapid testing was compared to those who preferred standard HIV testing, which was described as serum testing sent to the state laboratory with a turn-around time of two weeks for results. Among participants preferring rapid testing, the proportions of preferred testing locations were also analyzed.
Results
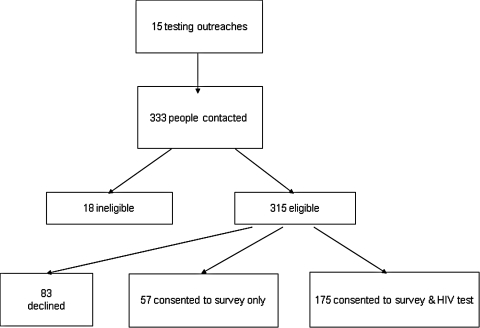
Fifteen outreach events were held among 9 apartment complexes in Durham during the study period. Of the 333 people contacted about the study by the promotores, 315 were eligible for study participation (Fig. 1). Of the residents who were eligible, 232 (73.7%) agreed to participate in the study and 83 (26.3%) declined participation. Among study participants, 57 (24.6%) consented to the survey only and 175 (55.2% of eligible or 75.4% of participants) consented to both the survey and rapid HIV test. Among study participants, 228 (98.3%) were Hispanic/Latino, 2 were African-American, 1 was Asian, and 1 was Native American. To make the results more applicable to Latinos, the 4 non-Latinos were removed from the rest of the analysis.
FIG. 1.
Participant recruitment and enrollment for HIV surveys and rapid community-based testing in Durham County, North Carolina.
The majority of participants were men (81.1%, Table 1), which is higher than the proportion of the state's Latino population who are male (55%).20 The median age of the sample was 30 years old (range, 18–65), and the median number of years attended school was 6. Among participants, 74.1% were from Mexico and the mean duration of years living in the United States was 5. Nearly half of participants (47.2%) reported living with family members, and the mean number of persons that they reported living in their household was five (range, 1–9). Although 42.5% of the participants were married, less than half (46%) of the married men were living with their spouse or sexual partner.
Table 1.
Sociodemographic Characteristics of Participants and Predictors of Rapid HIV Testing
| All participants N = 228 n (%)a | Survey and HIVtest N = 171 n (%)a | Survey only N = 57 n (%)a | OR (95% CI) | aOR (95% CI)b | |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 185 (81.1%) | 142 (83.0%) | 43 (75.4%) | 1.6 (0.8, 3.3) | — |
| Female | 43 (18.9%) | 29 (17.0%) | 14 (24.6%) | 1 | — |
| Age (years) | |||||
| 18–25 | 74 (32.5%) | 56 (32.7%) | 18 (31.6%) | 0.4 (0.1, 1.9) | — |
| 26–35 | 86 (37.7%) | 65 (38.0%) | 21 (36.8%) | 0.4 (0.1, 1.8) | — |
| 36–45 | 50 (21.9%) | 34 (19.9%) | 16 (28.1%) | 0.3 (0.1, 1.3) | — |
| >45 | 18 (7.9%) | 16 (9.4%) | 2 (3.5%) | 1 | — |
| Years attended school | |||||
| 0–5 | 59 (26.5%) | 49 (29.2%) | 10 (18.2%) | 0.1 (0.1, 9.3) | — |
| 6–8 | 87 (39.0%) | 63 (37.5%) | 24 (43.6%) | 0.5 (0.1, 4.7) | — |
| 9–12 | 71 (31.8%) | 51 (30.4%) | 20 (36.4%) | 0.5 (0.1, 4.6) | — |
| >12 | 6 (2.7%) | 5 (3.0%) | 1 (1.8%) | 1 | — |
| Country of origin | |||||
| Mexico | 169 (74.1%) | 127 (74.3%) | 42 (73.7%) | 1.1 (0.3, 4.5) | — |
| Honduras | 40 (17.5%) | 29 (16.9%) | 11 (19.3%) | 1.0 (0.2, 4.4) | — |
| El Salvador | 11 (4.8%) | 8 (4.7%) | 3 (5.3%) | 1 | — |
| Guatemala | 6 (2.6%) | 6 (3.5%) | 0 (0.0%) | — | — |
| United States | 2 (0.9%) | 1 (0.6%) | 1 (1.8%) | — | — |
| Years living in United States | |||||
| <1 | 14 (7.0%) | 12 (7.9%) | 2 (4.2%) | 3.3 (0.5, 20.3) | — |
| 1–5 | 110 (55.0%) | 86 (56.6%) | 24 (50.0%) | 2.5 (0.8, 7.8) | — |
| 6–10 | 57 (28.5%) | 43 (28.3%) | 14 (29.2%) | 2.2 (0.7, 7.1) | — |
| >10 | 19 (9.5%) | 11 (7.2%) | 8 (16.7%) | 1 | — |
| Marital status | |||||
| Married | 97 (42.5%) | 77 (45.8%) | 20 (36.4%) | 1 | — |
| Single | 88 (38.6%) | 67 (39.9%) | 21 (38.2%) | 0.8 (0.4, 1.7) | — |
| Consensual relationship | 28 (12.3%) | 20 (11.9%) | 8 (14.5%) | 0.7 (0.3, 1.7) | — |
| Separated, divorced, or widowed | 15 (6.6%) | 4 (2.4%) | 6 (10.9%) | — | — |
| Lives with family | |||||
| Yes | 103 (47.2%) | 72 (44.4%) | 31 (55.4%) | 1 | — |
| No | 115 (52.8%) | 90 (55.6%) | 25 (44.6%) | 1.6 (0.8, 2.9) | — |
| Lives with sex partner | |||||
| Yes | 79 (36.1%) | 52 (31.7%) | 27 (49.1%) | 0.5 (0.3, 0.9) | 1.3 (0.6, 2.9) |
| No | 140 (63.9%) | 112 (68.3%) | 28 (50.9%) | 1 | — |
| Primary language | |||||
| Spanish | 219 (99.0%) | 164 (99.4%) | 55 (98.2%) | 3.0 (0.2, 48.5) | — |
| English | 2 (1.0%) | 1 (0.6%) | 1 (1.8%) | 1 | — |
| Reads/writes in English | |||||
| Yes | 41 (18.6%) | 28 (16.8%) | 13 (24.1%) | 1 | — |
| No | 180 (81.4%) | 139 (83.2%) | 41 (75.9%) | 1.6 (0.8, 3.3) | — |
% represents the proportion of individuals with the characteristics divided by the number of respondents to the survey question.
Significant factors with p ≤ 0.05 in the bivariate analysis were entered into the model for the logistic regression analysis.
N, total number; n, number of individuals with the characteristics; OR, prevalence odds ratio; aOR, adjusted odds ratio; CI, confidence intervals.
Risk factors
A high prevalence of sexual risk behaviors was evident in our study population (Table 2). Participants reported an average of three sexual partners in the previous 6 months (range, 0–102). Although all male participants were asked if they had ever had sex with another man, only one male participant acknowledged this behavior. Forty-five participants (20.2%) reported ever having sex in exchange for drugs or money; however, a greater proportion (42.5%) acknowledged ever having sex with a CSW. Condom use was reported by 75.6% of participants who disclosed ever having sex in exchange for drugs or money, and 80.6% of persons who reported sex with a CSW during those sexual encounters. Only one female participant reported ever having sex in exchange for drugs or money. Among men who reported the number of sexual encounters with a CSW in the previous 6 months, the mean number was four.
Table 2.
HIV Risk Factors of Participants and Predictors of Rapid HIV Testing
| All participants N = 228 n (%)a | Survey and HIV test N = 171 n (%)a | Survey only N = 57 n (%)a | OR (95% CI) | aOR (95% CI)b | |
|---|---|---|---|---|---|
| Sex partners in past 6 mo. | |||||
| 0–1 | 139 (64.1%) | 100 (61.3%) | 39 (72.2%) | 0.6 (0.1, 5.9) | — |
| 2–5 | 57 (26.3%) | 45 (27.6%) | 12 (22.2%) | 0.9 (0.1, 9.2) | — |
| 6–10 | 16 (7.4%) | 14 (8.6%) | 2 (3.7%) | 1.8 (0.1, 24.7) | — |
| >10 | 5 (2.3%) | 4 (2.5%) | 1 (1.9%) | 1 | — |
| Ever diagnosed with an STI | |||||
| Yes | 18 (8.1%) | 14 (8.3%) | 4 (7.4%) | 1.1 (0.3, 4.3) | — |
| No | 205 (91.9%) | 155 (91.7%) | 50 (92.6%) | 1 | — |
| Ever exchanged sex for drugs or money | |||||
| Yes | 45 (20.2%) | 41 (24.4%) | 4 (7.3%) | 4.1 (1.4, 12.1) | 2.3 (0.5, 10.1) |
| No | 178 (79.8%) | 127 (75.6%) | 51 (92.7%) | 1 | — |
| Ever had sex with a CSW | |||||
| Yes | 93 (42.5%) | 77 (47.0%) | 16 (29.1%) | 2.2 (1.1, 4.2) | 1.8 (0.7, 4.7) |
| No | 126 (57.5%) | 87 (53.0%) | 39 (70.9%) | 1 | — |
| # sexual encounters with a CSW in past 6 mo. | |||||
| 0 | 14 (17.5%) | 11 (15.9%) | 3 (27.3%) | 0.1 (0, 1.5) | — |
| 1–3 | 38 (47.5%) | 31 (44.9%) | 7 (63.6%) | 0.2 (0, 1.4) | — |
| >3 | 28 (35.0%) | 27 (39.1%) | 1 (9.1%) | 1 | — |
| Uses drugs | |||||
| Yes | 21 (9.3%) | 17 (10%) | 4 (7.3%) | 1.4 (0.5, 4.4) | — |
| No | 204 (90.7%) | 153 (90%) | 51 (92.7%) | 1 | — |
| Ever injected drugs or vitamins | |||||
| Yes | 24 (10.7%) | 19 (11.3%) | 5 (8.8%) | 1.3 (0.5, 3.7) | — |
| No | 201 (89.3%) | 149 (88.7%) | 52 (91.2%) | 1 | — |
| Uses drugs or drinks beer/alcohol before sex | |||||
| Yes | 32 (14.4%) | 25 (15.0%) | 7 (12.7%) | 1.2 (0.5, 3.0) | — |
| No | 190 (85.6%) | 142 (85.0%) | 48 (87.3%) | 1 | — |
| Drinks beer | |||||
| Yes | 150 (66.1%) | 113 (66.5%) | 37 (64.9%) | 1.1 (0.6, 2.0) | — |
| No | 77 (33.9%) | 57 (33.5%) | 20 (35.1%) | 1 | — |
| Drinks alcohol | |||||
| Yes | 43 (19.1%) | 39 (23.1%) | 4 (7.0%) | 4.0 (1.4, 11.7) | 1.3 (0.4, 3.8) |
| No | 183 (80.9%) | 130 (76.9%) | 53 (93.0%) | 1 | — |
| Has limited access to care | |||||
| Yes | 111 (48.6%) | 88 (51.5%) | 23 (40.1%) | 1.6 (0.9 2.8) | — |
| No | 117 (51.4%) | 83 (48.5%) | 34 (59.6%) | 1 | — |
| Perceives self-risk for HIV | |||||
| Yes | 96 (48.7%) | 81 (54.7%) | 15 (30.6%) | 2.7 (1.4, 5.5) | 2.1 (0.9, 4.5) |
| No | 101 (51.3%) | 67 (45.3%) | 34 (69.4%) | 1 | — |
| Ever tested for HIV | |||||
| Yes | 76 (33.5%) | 49 (28.8%) | 27 (47.4%) | 1 | — |
| No | 151 (66.5%) | 121 (71.2%) | 30 (52.6%) | 2.2 (1.2, 4.1) | 2.5 (1.1, 5.6) |
% represents the proportion of individuals with the risk factors divided by the number of respondents to the survey question.
Significant factors with p ≤ 0.05 in the bivariate analysis were entered into the model for the logistic regression analysis.
N, total number; n, number of individuals with the characteristics; OR, prevalence odds ratio; aOR, adjusted odds ratio; CI, confidence intervals.
Participants also reported engaging in drug and alcohol-related risk behaviors. Drug use in the past month was reported by 9.3% of participants (3% used marijuana, 4% used crack/cocaine, and 2% reported use of both marijuana and crack); only 2 male participants acknowledged prior injection drug use (IDU) with cocaine. A majority of participants (66.1%) reported drinking beer, and 19.1% reported alcohol use (defined as drinking hard liquor and in a distinct category from drinking beer). Among participants, 14.4% reported using drugs or drinking beer or alcohol before sex.
Almost half (48.7%) of all participants reported self-perceived risk for HIV infection. Among 96 participants, all but six reported engaging in at least one risky behavior, including ever having sex with a CSW (60.4%), using drugs (13.8%), and injecting drugs/vitamins (11.7%). However, risky behaviors were also present among those who did not perceive themselves at risk; 27.3% of those not perceiving self-risk for HIV reported previous sex with a CSW.
Nearly half (48.6%) of study participants reported having limited access to health care. Among those participants, 42.0% did not know where to go for medical care, and 59.2% were unaware of where to receive a free/low-cost HIV test. Participants identified other barriers to accessing medical care, with 37.6% not having transportation to a health clinic and 10.5% having no one to call in an emergency.
HIV testing
The majority of study participants (66.5%) that we reached through this community-based strategy reported no prior HIV testing. Reasons for not having HIV testing in the past included no self-perceived risk for HIV (41.4%), worrying about the results (17.1%), work hours (14.6%), and not knowing where to get tested (13.0%).
The majority of study participants (n = 171) consented to rapid HIV testing, and 57 (25.0%) declined testing. The characteristics of participants who completed the survey only and those who consented to the survey and HIV testing are described in Table 1. Among those who did not test and stated reasons for not doing so, fear of the test results, history of recent HIV testing, and no perceived risk were the most commonly cited reasons for declining rapid HIV testing on the day of the outreach.
All participants who underwent rapid testing had negative rapid HIV test results. One male participant was found to have an indeterminate rapid test but had a negative confirmatory serum test. Results and posttest counseling were provided to 99% of people who tested in the apartment complexes. Two participants did not receive their results because they did not return to the HIV counselor during the outreach event or left their home before the results of the rapid HIV tests were available.
Predictors of testing
Bivariate analysis was conducted on 23 variables (Tables 1 and 2), and the following factors were found to be significantly associated with acceptance of rapid HIV testing (p < 0.05): perceiving oneself to be at risk for HIV; no history of prior HIV testing; history of ever having sex with a CSW; ever having sex in exchange for drugs or money; living with a partner; and reported alcohol consumption (other than beer consumption). Ever having sex in exchange for drugs or money (OR 4.1, 95% CI, 1.4,12.1) was strongly associated with HIV testing, while living with a sex partner was associated with a decreased likelihood of testing (OR 0.5; 95% CI, 0.3, 0.9).
Of the six variables that had an association with rapid HIV test acceptance in the bivariate analyses, HIV testing history was the only variable that remained significant in the multivariate analysis. Participants who had never been tested for HIV were two and a half times more likely to consent to rapid HIV testing than those who had tested in the past (adjusted odds ratio [aOR] 2.5; 95% CI, 1.1, 5.6).
Acceptability of rapid HIV testing in the community
Overall, nearly all participants who were surveyed supported community-based rapid HIV testing (Table 3). The majority of participants (91.5%) preferred the rapid HIV test over the standard HIV testing method. Of those who preferred the rapid HIV testing method, 73.4% identified at home or in the community as their preferred location for receiving the test. Participants who preferred a different location for rapid HIV testing favored a Latino community center (14.0%), a clinic (10.0%), the workplace (2.3%), or a health fair (1.4%) as testing venues.
Table 3.
Acceptability of Community-Based Rapid HIV Testing and Preferences for HIV Testing Method and Location
| % (n/N)a | 95% CI | |
|---|---|---|
| Preferred rapid testing over standard testing | 91.5 (195/213) | (88–95) |
| Preferred receiving test results immediately | 89.9 (186/207) | (86–94) |
| Preferred rapid testing in the home or community | 73.4 (141/192) | (67–80) |
| Supported rapid testing in community | 97.7 (217/222) | (96–100) |
| Had no concerns about rapid HIV testing in community | 91.8 (202/220) | (88–95) |
n, number of participants who responded “yes” to the question; N, total number of respondents to the survey question.
CI, confidence interval.
While only 5 participants (2 who tested and 3 who did not test) stated that they did not support this activity in the community, 13 additional participants also provided reasons against community-based rapid HIV testing. The most frequently identified reasons were worrying that others would find out the test results (6/18), worrying about the results (5/18), and preferring clinic-based testing (4/18).
Discussion
We demonstrated that door-to-door rapid HIV testing is a feasible and acceptable strategy to reach Latinos who were unaware of their HIV status in the community. Prior HIV testing was reported by 33% of our participants, compared to other studies of Latino men which found prior HIV testing rates ranging from 21%–66%.21–24 Among residents who were eligible to participate in our study, 55.2% accepted a rapid HIV test. A similar acceptance rate of 60% was reported among persons from various racial/ethnic groups who were offered rapid HIV testing in community settings.14 The rapid HIV test was preferred by the vast majority of participants over the standard test, similar to other reports on test preferences.25,26
With respect to testing location, inside the home or in the community was preferred over other locations among study participants, including those who opted not to test. In contrast, a study of HIV testing preference among a predominantly Black female population at a housing authority in Chicago found that most preferred to go to primary care clinics and multispecialty sites for HIV testing instead of community centers.27 Differences in the preference of HIV testing sites may exist between different racial/ethnic groups and communities, possibly due to their level of knowledge, familiarity, and trust in the health care system. Focus groups conducted among Latino men in North Carolina revealed that participants had a misunderstanding of the U.S. health care system and its eligibility, and a desire for creative HIV prevention strategies using non-traditional venues.28
Strategies to reach the Latino population in their communities have been explored by other investigators. Rapid HIV testing initiatives conducted as part of a national demonstration project in nontraditional venues (e.g., parks, health fairs, community clinics) or in mobile vans have been successful in reaching Latinos immigrants and other at-risk racial/ethnic groups.10,14 Soccer matches have also been identified as a potentially effective venue for HIV prevention programs among Latino men and should be further investigated.29 A strategy of “bundling” HIV testing with other services, or combining with other tests, was assessed in one study involving rapid HIV testing of Latinos in bars.30 However, no significant difference was found in the proportion of participants who took the HIV test when bundled with other tests (10.2% compared to 8.9% who agreed to HIV testing only).30
Our study is one of a few in the literature that utilizes a door-to-door outreach strategy, which have been described during outbreak investigations for tuberculosis and syphilis in the United States.30,31 North Carolina has recently adopted the door-to-door strategy as a key component of their universal opt-out HIV testing campaign.17 In Malawi, door-to-door HIV testing has been offered in some communities, where the investigators noted a high level of acceptance due to the convenience of testing among persons who would not otherwise pursue an HIV test at a health facility.33 We did encounter some logistical issues since the outreach events and rapid testing outdoors were subject to variations in temperature and weather, and clearly dependent on the number of residents who were not working and were present in their homes. However, we successfully provided HIV education and testing to a large sample of Latino immigrants of which nearly half had self-perceived risk for HIV but also reported limited access to health care. Although this suggests that this sample had some knowledge of their HIV risk factors which has been supported by previous assessments of the same population,18 there were some individuals who did not perceive themselves as at-risk despite engaging in risky behaviors. Improving HIV education prior to outreach events may increase testing participation by enhancing individual awareness of risk behaviors and dispel possible concerns about testing (i.e., fears related to immigration status and interacting with the U.S. health system, concerns about confidentiality), and should be further explored in qualitative research.
Overall, the majority of our participants engaged in at least one sexual risk behavior, including multiple sexual partners in the past 6 months (36%) and ever having sex with a CSW (40%). In comparison, a population-based study conducted in California found that 22% of Latino immigrant men reported multiple sexual partners in the past 6 months and 36% had ever paid for sex.34 Among Latino male migrant workers who came to New Orleans post-Hurricane Katrina, investigators reported that 49% had more than one sexual partner in the past month, 52% had paid for sex, and 11% acknowledged having sex with a man.35 Other studies of Latino male populations conducted in North Carolina and from other parts of the country have identified a range of participants who had reported sex with a CSW from 18%–70%.18,32,36–38 Interestingly, our participants who acknowledged sex with a CSW reported 81% condom use during those encounters, which is much higher than the 23%–31% reported by investigators from California.37,38 Parrado et al.,18 also reported a high rate of condom use (92%) among Latino immigrants having sex with CSWs in Durham; however, condom use decreased as familiarity with the CSW increased.
Several investigators have recognized the potential impact of migration on HIV risk behaviors among the Latino population.39–41 A California-Mexico binational collaboration project found that migrants who had been to the United States in the past 12 months reported more sexual partners and noninjecting drug use than non-migrant Mexicans living in the same communities in Mexico.42 However, migrants reported higher condom use during vaginal sex and were more likely to have had HIV testing. Migration is associated with constant mobility, family separation, social isolation, and dramatic changes in cultural environment that may lead to the adoption of new sexual practices to compensate for the alienating aspects of the migration experience.41 Family separation and social isolation were not as evident among our Latino immigrants, with almost half reporting that they lived with family members and/or multiple persons in their household. We did not ask about participants' mobility or assess their level of acculturation; however, our population in Durham had a mean duration of 5 years in the United States. A higher degree of acculturation may have contributed to the greater use of condoms among our participants having sex with CSWs. Interestingly, greater acculturation into the U.S. culture can have effects on Latino immigrant health behaviors that are both positive (e.g., communicating with partners about practicing safer sex) and negative (e.g., engaging in behaviors that increase the risk for HIV infection).43
Although other investigators have described predictors of HIV testing among Latinos,22,24 we provide information on risk factors that affect predominantly male Latino immigrants who had rapid HIV testing rather than merely intent to test or prior history of testing, thereby giving a more accurate measurement of the factors affecting test acceptance. We found five factors in the bivariate analysis that had a positive association with rapid HIV test acceptance among our participants: perceiving oneself at-risk for HIV, having ever had sex with a CSW, having ever had sex in exchange for drugs or money, drinking alcohol, and having no prior HIV testing. Similarly, a study which measured intent to test for HIV reported that Latino immigrant men with more sexual partners in the past year and those who perceived themselves to be at risk were more likely to test.24 In a study of Latino immigrant men from South Florida, other investigators found that being MSM and having been previously tested predicted future HIV testing intentions among their participants.22 In contrast, no prior HIV testing was a significant predictor of accepting rapid HIV testing among Latino participants during our outreach events.
Only one factor, living with a sex partner, was negatively associated with rapid HIV testing in the bivariate analysis. A study conducted among Latino immigrants in North Carolina by Parrado et al.18 found that single men and unaccompanied married men were more likely to have used CSWs, suggesting that the presence of a partner in the home may decrease risky behaviors as well as perception of risk that reduces the likelihood of testing. However, despite the lower proportion of married men living with their spouses who reported sex with CSWs, these investigators observed a higher frequency of visits with CSWs among accompanied married men than unaccompanied ones. The contribution of Latino cultural and social norms to this observation remains unclear, such as the traditional male role of machismo, which encourages men to demonstrate their masculinity through sex including having multiple sexual partners.28,44
Despite the high prevalence of risk factors among those who tested, none of the 171 individuals tested positive for HIV infection. Our finding of a high prevalence of HIV risk factors and low incidence of HIV is congruent with data collected from previous studies reported among Latino migrants in California.37,38,45 The most recent investigation involved rapid HIV testing of 1041 Mexican migrants along the U.S.–Mexico border in southern California, which identified no positive results despite the presence of HIV risk factors in their study population.45 The authors hypothesized that HIV infection might not yet be endemic among the sexual partners of Mexican migrants due to unclear epidemiologic or cultural factors. In our study, the high degree of condom use reported by our participants likely reduced their risk of HIV acquisition.
In North Carolina, 65% of HIV cases among Latino men in 2007 were associated with MSM behaviors,17 which indicates that heterosexual sex is not (yet) the dominant mode of HIV transmission in this community. National data have shown that sexual contact with other men is the primary mode of HIV transmission among Latino men born in Central or South America and Mexico, and that Puerto Ricans have a much higher prevalence of HIV/AIDS than Mexican Americans.46 Sanchez et al.47 reviewed several studies conducted among different groups of Latinos in California, and demonstrated higher HIV prevalence among Latino MSM (5%–35%) and Mexicans who practiced IDU (12%) than Mexican migrant farm workers (0%). We did not test any self-identified Latino MSM or Puerto Rican immigrants in our study, and only 1% of our participants reported IDU, which may partly account for the absence of any HIV infections detected by our community-based testing efforts.
Our study has demonstrated a novel community-based strategy that should be considered in similar communities with a growing Latino population that may not access clinic-based HIV prevention services. However, there are some limitations based on our sampling and study procedures that should be noted. First, our convenience sampling of the apartment complexes could have introduced bias affecting our acceptability estimates if the sample was not representative of all predominantly Latino immigrant neighborhoods in the community. In addition, most of our participants were men, but may reflect a different risk profile and testing acceptability than Latino immigrant women. Although the study had a high acceptability rate among participants, the consent and study procedures may have discouraged participation among Latino residents possibly due to concerns related to immigration status, which would have underestimated the proportion who may agree to test using the door-to-door approach. We described risk factors for HIV infection but could not compare differences in risk factors by HIV status because we did not diagnose any HIV-positive persons during the study. Lastly, since this was a study exploring rapid HIV testing feasibility and acceptability, we did not estimate the staffing and financial resources necessary to implement this program which should be compared with other community based testing strategies (i.e., health fairs or soccer matches) by public health programs in the United States.
There is a ongoing need for updated information on the social-behavioral and situational HIV risk factors that affect Latino immigrants in rapid growth states in the U.S., especially to help overcome barriers to testing.16 The social and circumstantial factors that affect the risk behaviors of the predominantly male Latino population in this country who are migrant workers should also be distinguished from the factors that affect immigrant Latino men who have had longer durations of residence in the United States. Our study found that over 40% of predominantly male Latino participants in our community reported ever having sex with a CSW; yet, the majority had never had HIV testing. Although we did not detect any HIV infections during our outreach events, community-based rapid HIV testing and education for Latino immigrants is well justified given the risk factors for HIV that we identified in this study. HIV testing and prevention services should be accessible and culturally appropriate to Latinos in the United States, and local HIV prevention efforts should identify barriers to clinic-based testing and community-based preferences regarding testing method and locations in their area. Latino immigrant men represent a group that has reported HIV risk behaviors and is already disproportionately affected by HIV/AIDS in our country; therefore opportunities to intervene using innovative strategies to reach individuals in their communities should be taken now to hinder the epidemic in this population.
Acknowledgments
We thank Dr. Chris McQuiston, Dr. Peter Leone, and Hsiao Tien at the University of North Carolina at Chapel Hill for assisting with the study design and implementation; Alba Onofrio, Colleen Blue, Julio Olmos, and Jessica Burroughs with El Centro Hispano for assisting in the training and coordination of the promotores; Dr. Heidi Swygard and Megan Randall for volunteering as HIV counselors; and Maximillian Hernandez, Gladys Gutarra, Isidro Torres, and Tomas Montillo for their work in recruiting and enrolling participants. This research was supported by the University of North Carolina at Chapel Hill Center for AIDS Research (CFAR), a National Institutes of Health-funded program #P30 AI50410.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Centers for Disease Control and Prevention. HIV/AIDS among Hispanics—United States, 2001–2005. MMWR Morb Mortal Wkly Rep. 2007;56:1052–1057. [PubMed] [Google Scholar]
- 2.Karon J. HIV in the United States at the turn of the century: An epidemic in transition. Am J Public Health. 2001;91:1060–1068. doi: 10.2105/ajph.91.7.1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gallant JE. HIV counseling, testing, and referral. Am Fam Physician. 2004;70:295–302. [PubMed] [Google Scholar]
- 4.Duffus WA. Weis K. Kettinger L. Stephens T. Albrecht H. Gibson JJ. Risk-based HIV testing in South Carolina health care settings failed to identify the majority of infected individuals. AIDS Patient Care STDs. 2009;23:339–345. doi: 10.1089/apc.2008.0193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Branson BM. Handsfield HH. Lampe MA, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Morb Mortal Wkly Rep. 2006;55:1–17. [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. HIV/AIDS: Hispanics/Latino: Prevention Challenges. www.cdc.gov/hiv/hispanics/challenges.htm. [Aug 20;2009 ]. www.cdc.gov/hiv/hispanics/challenges.htm
- 7.Betancourt JR. Carrillo JE. Green AR. Maina A. Barriers to health promotion and disease prevention in the Latino population. Clin Cornerstone. 2004;6:16–26. doi: 10.1016/s1098-3597(04)80061-9. [DOI] [PubMed] [Google Scholar]
- 8.Zúñiga ML. Brennan J. Scolari R. Strathdee SA. Barriers to HIV care in the context of cross-border health care utilization among HIV-positive persons living in the California/Baja California US-Mexico border region. J Immig Minor Health. 2008;10:219–227. doi: 10.1007/s10903-007-9073-7. [DOI] [PubMed] [Google Scholar]
- 9.Guenter D. Greer J. Barbara A. Robinson G. Roberts J. Browne G. Rapid point-of-care HIV testing in community-based anonymous HIV testing program: A valuable alternative to conventional testing. AIDS Patient Care STDs. 2008;22:195–204. doi: 10.1089/apc.2007.0137. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Rapid HIV testing in outreach and other community settings—United States, 2004–2006. MMWR Morb Mortal Wkly Rep. 2007;56:1233–1237. [PubMed] [Google Scholar]
- 11.Beckwith CG. Atunah-Jay S. Cohen J, et al. Feasibility and acceptability of rapid HIV testing in jail. AIDS Patient Care STDs. 2007;21:41–47. doi: 10.1089/apc.2006.006. [DOI] [PubMed] [Google Scholar]
- 12.Bucher JB. Thomas KM. Guzman D. Riley E. Dela Cruz N. Bangsberg DR. Community-based rapid HIV testing in homeless and marginally housed adults in San Francisco. HIV Med. 2007;8:28–31. doi: 10.1111/j.1468-1293.2007.00423.x. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. Rapid HIV testing among racial/ethnic minority men at gay pride events—Nine U.S. cities, 2004–2006. MMWR Morb Mortal Wkly Rep. 2007;56:602–604. [PubMed] [Google Scholar]
- 14.Bowles KE. Clark HA. Tai E, et al. Implementing rapid HIV testing in outreach and community settings: results from an advancing HIV prevention demonstration project conducted in seven U.S. cities. Public Health Rep. 2008;23:78–85. doi: 10.1177/00333549081230S310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.US Census Bureau. State and County Quickfacts. http://quickfacts.census.gov/qfd/states/37/37063.html. [Jun 1;2009 ]. http://quickfacts.census.gov/qfd/states/37/37063.html
- 16.Painter TM. Connecting the dots: When the risks of HIV/STD infection appear high but the burden of infection is not known—The case of male Latino migrants in the southern United States. AIDS Behav. 2008;12:213–226. doi: 10.1007/s10461-007-9220-0. [DOI] [PubMed] [Google Scholar]
- 17.North Carolina Department of Health and Human Services. Epidemiologic Profile HIV/STD Prevention & Care Planning, October 2008
- 18.Parrado EA. Flippen CA. McQuiston C. Use of commercial sex workers among Hispanic migrants in North Carolina: Implications for the spread of HIV. Perspect Sex Reprod. 2004;36:150–156. doi: 10.1363/psrh.36.150.04. [DOI] [PubMed] [Google Scholar]
- 19.U.S. Department of Health and Human Services. Quality assurance guidelines for testing using rapid HIV antibody tests waived under the clinical laboratory improvement amendments of 1988, 2007
- 20.Kasarda JD. Johnson JH. The econonic impact of the Hispanic population on the state of North Carolina. Chapel Hill, NC: Frank Hawkins Kenan Institute of Private Enterprise; 2006. [Google Scholar]
- 21.Centers for Disease Control and Prevention. Persons tested for HIV—United States, 2006. MMWR Morb Mortal Wkly Rep. 2008;57:845–849. [PubMed] [Google Scholar]
- 22.Fernandez MI. Perrino T. Royal S. Ghany D. Bowen GS. To test or not to test: Are Hispanic men at highest risk for HIV getting tested? AIDS Care. 2002;14:375–384. doi: 10.1080/09540120220123757. [DOI] [PubMed] [Google Scholar]
- 23.Fernandez MI. Collazo JB. Bowen GS. Varga LM. Hernandez N. Perrino T. Predictors of HIV testing and intention to test among Hispanic farmworkers in South Florida. J Rural Health. 2005;21:56–64. doi: 10.1111/j.1748-0361.2005.tb00062.x. [DOI] [PubMed] [Google Scholar]
- 24.Ehrlich SF. Organista KC. Oman D. Migrant Latino day laborers and intentions to test for HIV. AIDS Behav. 2007;11:743–752. doi: 10.1007/s10461-006-9182-7. [DOI] [PubMed] [Google Scholar]
- 25.Liang TS. Erbelding E. Jacob CA, et al. Rapid HIV testing of clients of a mobile STD/HIV clinic. AIDS Patient Care STDs. 2005;19:253–257. doi: 10.1089/apc.2005.19.253. [DOI] [PubMed] [Google Scholar]
- 26.Wurcel A. Zaman T. Zhen S. Stone D. Acceptance of HIV antibody testing among inpatients and outpatients at a public health hospital: A study of rapid versus standard testing. AIDS Patient Care STDs. 2005;19:499–505. doi: 10.1089/apc.2005.19.499. [DOI] [PubMed] [Google Scholar]
- 27.Djokic D. Englund J. Daum R, et al. HIV knowledge and attitudes toward HIV testing of south side Chicago housing authority residents. AIDS Patient Care STDs. 2009;23:23–28. doi: 10.1089/apc.2008.0110. [DOI] [PubMed] [Google Scholar]
- 28.Rhodes SD. Eng E. Hergenrather KC, et al. Exploring Latino men's HIV risk using community-based participatory research. Am J Health Behav. 2007;31:146–158. doi: 10.5555/ajhb.2007.31.2.146. [DOI] [PubMed] [Google Scholar]
- 29.Rhodes SD. Hergenrather KC. Montano J, et al. Using community-based participatory research to develop an intervention to reduce HIV and STD infections among Latino men. AIDS Educ Prev. 2006;18:375–389. doi: 10.1521/aeap.2006.18.5.375. [DOI] [PubMed] [Google Scholar]
- 30.Galvan FH. Bluthenthal RN. Ani C. Bing EG. Increasing HIV testing among Latinos by bundling HIV testing with other tests. J Urban Health. 2006;83:849–859. doi: 10.1007/s11524-006-9072-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Clark PA. Cegielski JP. Hassell W. TB or not TB ? Increasing door-to-door response to screening. Pub Health Nurs. 1997;14:268–271. doi: 10.1111/j.1525-1446.1997.tb00374.x. [DOI] [PubMed] [Google Scholar]
- 32.Paz-Bailey G. Teran S. Levine W. Markowitz LE. Syphilis outbreak among Hispanic immigrants in Decatur, Alabama: Association with commercial sex. Sex Trans Dis. 2004;31:20–25. doi: 10.1097/01.OLQ.0000104813.21860.E1. [DOI] [PubMed] [Google Scholar]
- 33.Angotti N. Bula A. Gaydosh L. Zimchi EZ. Thornton RL. Yeatman SE. Increasing the acceptability of HIV counseling and testing with three C's: Convenience, confidentiality and credibility. Soc Sci Med. 2009;68:2263–2270. doi: 10.1016/j.socscimed.2009.02.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Levy V. Page-Shafer K. Evans J, et al. HIV-related risk behavior among Hispanic/Latino immigrant men in a population-based household survey in low-income neighborhoods of northern California. Sex Transm Dis. 2005;32:487–490. doi: 10.1097/01.olq.0000161185.06387.94. [DOI] [PubMed] [Google Scholar]
- 35.Kissinger P. Liddon N. Schmidt N. Curtin E. Salinas O. Narvaez A. HIV/STI risk behaviors among Latino migrant workers in New Orleans post-hurricane Katrina disaster. Sex Transm Dis. 2008;35:924–929. doi: 10.1097/OLQ.0b013e31817fa2cc. [DOI] [PubMed] [Google Scholar]
- 36.Viadro CL. Earp JAL. The sexual behavior of married Mexican immigrant men in North Carolina. Soc Sci Med. 2000;50:723–735. doi: 10.1016/s0277-9536(99)00305-6. [DOI] [PubMed] [Google Scholar]
- 37.Ruiz JD. Da Valle L. Jungkeit M, et al. Seroprevalence of HIV and syphilis, and assessment of risk behaviors among migrant and seasonal farmworkers in five Northern California counties. Sacramento, CA: California Department of Health Services, Office of AIDS; Jun, 1997. [Google Scholar]
- 38.Mishra SI. Sanudo F. Connor RF. Collaborative research toward HIV prevention among migrant farm workers. In: Bowser BP, editor; Mishra SI, editor; Reback CJ, editor; Lemp GF, editor. Preventing AIDS: Community-Science Collaborations. New York: The Haworth Press; 2004. [Google Scholar]
- 39.Decosas J. Kane F. Anarfi JK. Sodji KD. Wagner HU. Migration and AIDS. Lancet. 1995;346:826–828. doi: 10.1016/s0140-6736(95)91631-8. [DOI] [PubMed] [Google Scholar]
- 40.Organista KC. Organista PB. Migrant laborers and AIDS in the United States: A review of the literature. AIDS Educ Prev. 1997;9:83–93. [PubMed] [Google Scholar]
- 41.Magis-Rodriguez C. Gayet C. Negroni M, et al. Migration and AIDS in Mexico: An overview based on recent evidence. J Acquir Immune Defic Syndr. 2004;37(Suppl 4):S215–S226. doi: 10.1097/01.qai.0000141252.16099.af. [DOI] [PubMed] [Google Scholar]
- 42.Magis-Rodriguez C. Lemp G. Hernandez MT. Sanchez MA. Estrada F. Bravo-Garcia E. Going North: Mexican migrants and their vulnerability to HIV. J Acquir Immune Defic Syndr. 2009;51(Suppl 1):S21–S25. doi: 10.1097/QAI.0b013e3181a26433. [DOI] [PubMed] [Google Scholar]
- 43.Rojas-Guyler L. Ellis N. Sanders S. Acculturation, health protective sexual communication, and HIV/AIDS risk behavior among Hispanic/Latino women in a large midwestern city. Health Educ Behav. 2005;32:767–779. doi: 10.1177/1090198105277330. [DOI] [PubMed] [Google Scholar]
- 44.Marin BV. HIV prevention in the Hispanic community: Sex, culture, and empowerment. J Transcul Nurs. 2003;14:186–192. doi: 10.1177/1043659603014003005. [DOI] [PubMed] [Google Scholar]
- 45.Martinez-Donate AP. Rangel MG. Hovell MF. Santibanez J. Sipan CL. Izazola JA. HIV infection in mobile populations: The case of Mexican migrants to the United States. Rev Panam Salud Publica. 2005;17:26–29. doi: 10.1590/s1020-49892005000100004. [DOI] [PubMed] [Google Scholar]
- 46.Centers for Disease Control and Prevention. HIV/AIDS surveillance report, 2006. US Department of Health and Human Services. 2007;18:1–46. [Google Scholar]
- 47.Sanchez MA. Lemp GF. Magis-Rodriguez C. Bravo-Garcia E. Carter S. Ruiz JD. The epidemiology of HIV among Mexican migrants and recent immigrants in California and Mexico. J Acquir Immune Defic Syndr. 2004;37(Suppl 4):S204–S213. doi: 10.1097/01.qai.0000141253.54217.24. [DOI] [PubMed] [Google Scholar]