Abstract
Providing care to a family member with dementia is conceptualized as a chronic stressor with adverse psychological and physical effects. The purpose of this pilot study was to evaluate mood and immune outcomes of caregivers exposed to a community-based psychoeducational nursing intervention based on the Progressively Lowered Stress Threshold (PLST) model. The PLST intervention is designed to strengthen the psychological resources of dementia caregivers by teaching methods of preventing and/or managing behavioral problems exhibited by the person with dementia. Mood and immune outcomes were compared between caregivers randomly assigned to receive either the PLST or a comparison intervention. Results of this pilot study suggest that caregivers who received the PLST intervention demonstrated significantly stronger T-cell proliferative responses to both PHA and ConA, indicating an improvement in T-cell immune function immediately after the in-home intervention (T2) and again after six months of telephone support for application of the PLST model (T3). Findings do not support the hypothesis that the PLST intervention had a significant effect on total mood disturbance or NK cell cytotoxicity over the course of the study.
There is increasing awareness of the extent of family dementia caregiving and its importance for maintaining the growing number of older persons with dementia who reside in the community. More than two decades of research on the effects of family dementia caregiving (henceforth referred to as caregiving) documents that it is a stressful role with deleterious consequences. In two reviews by Schulz and associates, convergent data support the claim that caregiving results in adverse psychological outcomes, with almost every study indicating that caregivers report significantly higher levels of depressive symptomatology than control groups or normative populations (Schulz, O’Brien, Bookwala, & Fleissner, 1995; Schulz, Visintainer, & Williamson, 1990). While the negative effect of caregiving on physical health outcomes is more ambiguous, a number of studies suggest that the chronic stress of caregiving can negatively impact cellular immune function (Cacioppo et al., 1998; Kiecolt-Glaser, 1999; Vedhara et al., 1999; Vitaliano, 1997). Down regulation of immune function may be clinically important given that spousal caregivers report significantly more days of infectious illness (primarily upper respiratory tract infections) compared with their non-caregiving counterparts (Kiecolt-Glaser, 1990) and a seminal study by Schulz and Beach demonstrates that dementia caregiving is a risk factor for mortality (Schulz & Beach, 1999).
A substantial body of literature shows that both major depression (Herbert & Cohen, 1993a; Weisse, 1992) and chronic stress (Esterling, Kiecolt-Glaser, Bodnar, & Glaser, 1994; Herbert & Cohen, 1993b; Irwin, 1994) are associated with reliable alterations in functional immune assays such as mitogen induced lymphocyte proliferation and natural killer (NK) cell cytotoxicity (Esterling et al., 1994; Herbert et al., 1993b). Lymphocyte response to stimulation by mitogens such as phytohemagglutinin (PHA) and concanavalin A (ConA) are thought to provide an in-vitro model of the body’s response to viral or bacterial challenge. NK cells play an important role in the prevention and spread of cancer and in the control of viral infections. Appling this literature to the caregiving population, it is thought that the prolonged distress inherent in caring for a family member with dementia may combine with individual vulnerabilities to jeopardize homeostatic mechanisms in some caregivers (Esterling et al., 1994; Vitaliano et al., 1998), increasing their risk for disease (Kiecolt-Glaser & Glaser, 1999; Schulz et al., 1999; Schulz et al., 1997; Shaw et al., 1997). If this is the case, spouses may be at greatest risk for the negative consequences of dementia caregiving stress since they are often elderly (i.e., immunosenescent) and may be faced with physical, psychological, and/or financial challenges that could diminish their ability to respond to the demands of the caregiving role (Cacioppo et al., 1998).
In the past, burden (distress) was the primary outcome of dementia caregiving research. Current investigative efforts have shifted to the identification of factors mediating distress among caregivers and evaluation of interventions designed to reduce caregiver burden (Drebing, 1999). Given that a number of studies show that the frequency of behavioral disturbance exhibited by persons with dementia is the strongest predictor of caregiver burden and/or depression (Bedard, Molloy, Pedlar, Lever, & Stones, 1997; Chappell & Penning, 1996; Coen, Swanwick, O’Boyle, & Coakley, 1997; Cook, Peason, & Ahrens, 1997; Levesque, Cossette, & Laurin, 1995; Pruchno & Resch, 1980; Song, Biegel, & Milligan, 1997; Streuning et al., 1995; Stuckey, Neundorfer, & Smyth, 1996; Teri, 1997; Williamson & Schulz, 1993), it is imperative that a body of knowledge regarding effective behavioral management techniques for persons with dementia be developed and systematically evaluated.
The purpose of this pilot study was to evaluate mood and immune outcomes of caregivers exposed to a community-based psychoeducational nursing intervention based on the Progressively Lowered Stress Threshold (PLST) model. The PLST intervention is designed to strengthen the psychological resources of dementia caregivers by teaching methods of preventing and/or managing behavioral problems exhibited by the person with dementia. Mood and immune outcomes were compared between caregivers randomly assigned to receive either the PLST intervention or the comparison intervention of psychological support, traditional dementia information, and referral to community-based services. This pilot study supplemented a larger (primary), longitudinal, multi-site study that investigated the effects of the PLST intervention on the frequency of behavioral disturbances among persons with dementia; as well as burden, mood (depression), knowledge, and role satisfaction/mastery among their caregivers (Buckwalter et al., 1999a; 1999b). While this pilot study was primarily designed to evaluate immune outcomes of the PLST intervention, mood outcomes were added to determine if they could be replicated in an independent community sample of family caregivers (independent from the larger study where N = 245).
Hypotheses
It was hypothesized that family caregivers receiving education and psychological support in the application of the PLST model (experimental intervention) would report lower total mood disturbance (TMD) scores than family caregivers receiving traditional support (comparison intervention). Caregivers in the experimental treatment group were also expected to demonstrate: a) higher levels of Natural Killer (NK) cell cytotoxicity, and b) stronger T-cell proliferative responses to phytohemagglutinin (PHA) and concanavalin A (ConA) immediately after the in-home intervention (T2) and 6 months after telephone support (T3), as compared to baseline (T1).
Theory Base
The PLST model (Hall & Buckwalter, 1987) is theoretically grounded in the concept of person-environment fit (Lawton, 1975), and is based on the premise that persons with dementia demonstrate an increasing inability to interpret, appropriately respond to, and/or interact with, the environment because of progressive cerebral pathology and associated cognitive decline (Wolanin & Phillips, 1981). A number of dementia-related behaviors (e.g., wandering, night awakening, repetitive vocalizations) are thought to result from the care recipient’s inability to interpret and/or appropriately respond to internal and external environmental stimuli. If the stimulus continues or increases, behavioral patterns of the care recipient become increasingly dysfunctional (bothersome) and often catastrophic (e.g., agitated or aggressive).
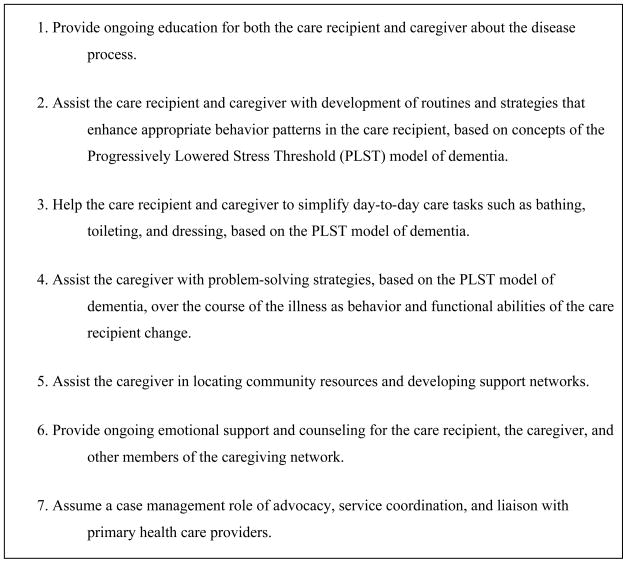
The PLST intervention was based on the model described above and was individualized for each caregiver. The intervention focused on psychological support and instruction in behavioral techniques aimed at diminishing problematic behaviors in the care recipient such as reducing environmental stressors, compensating for executive dysfunction and communication deficits, providing unconditional positive regard, and allowing for a lowered stress threshold (see Figure 1). The PLST intervention was designed to guide family caregivers in the interpretation of, as well as their response to, behaviors demonstrated by the care recipient
Figure 1.
Key Elements of the Progressively Lowered Stress Threshold Intervention
Support for the PLST Intervention
This study builds upon previous empirical work done on the PLST intervention, which was first described in this journal 15 years ago (Hall & Buckwalter, 1987) and subsequently evaluated in acute care and long-term care facilities. Results of these studies suggest that implementation of the PLST intervention significantly reduces the number of problematic behaviors among persons with dementia and improves caregiver burden or distress (Hall, 1999; Maas & Buckwalter, 1991). Concurrent with this pilot study, psychological outcomes of the PLST intervention were longitudinally evaluated among 245 family dementia caregivers in four states (Iowa, Minnesota, Arizona, and Indiana). Both quantitative and qualitative results from the primary study strongly suggest positive effects of the PLST intervention on caregiving affect, depression, burden, sense of mastery and satisfaction with caregiving (Buckwalter et al., 1999a; 1999b). This pilot study tests the PLST intervention by attempting to replicate mood outcomes while determining the effects of the PLST intervention on in-vitro measures of immune function.
Methods
Sample
Over a 16-month recruitment period, a total of 58 family caregivers expressed interest in the pilot study. These individuals were contacted by telephone and given a brief description of the study. During the initial telephone conversation, caregivers were screened for the following inclusion/exclusion criteria: 1) providing a minimum of four hours of care each week to a non-institutionalized family member with a diagnosis of probable dementia (any type), 2) no history of immunosuppressive disease or taking medications/treatments known to alter immune function (e.g., systemic corticosteroids within the past three months, chemotherapy or radiation treatment for cancer within the past five years), 3) consumes less than 10 alcoholic drinks per week, 4) not currently taking anticoagulant medication or history of a blood coagulation disorder (possible hemorrhage from venipuncture), 5) no previous exposure to the PLST intervention, and, 7) live within a 120 mile radius of the University of Iowa (for rapid transportation of blood samples). Nineteen family caregivers were excluded from study participation, based upon the criteria listed above.
The study sample consisted of 39 subjects; the majority of whom (58.9%, n=23) were recruited through church/synagogue bulletins. The remaining subjects were recruited through local media and word of mouth. Of the 39 subjects meeting inclusion/exclusion criteria and providing informed consent, two subjects (5.1% of sample) discontinued participation before completion of the in-home intervention due to institutionalization of the care recipient. Each of these subjects was assigned to a different treatment group and there were no statistically significant differences on baseline demographic or outcome variables between the two subjects dropping participation and the 37 subjects completing the study.
Design
This study used a two-group randomized single-blind (subject blind to treatment group assignment) design with outcome measures obtained at baseline (T1), one week post-intervention (T2), and after 6 months of biweekly telephone contact to support the intervention provided (T3).
Analyses
Independent sample t-tests were conducted on all demographic, health, and outcome variables to determine if groups were equivalent at baseline. Repeated measures, two-way analysis of covariance (ANCOVA) was computed for between group differences, over time, for TMD, NK cell cytotoxicity, and T-cell proliferation to PHA and ConA (controlling for initial differences between groups). One-way ANCOVAs were then computed when main effects for treatment group were detected. Immune data were transformed (log10) and all analysis used a 0.05 level of statistical significance.
Procedures
Experimental Intervention
The PLST intervention consisted of two phases; the first phase was implemented in the caregiver’s home on two separate occasions, each lasting approximately three hours. During the first home visit, the interventionist focused on developing a therapeutic relationship with the caregiver while teaching underlying principles of the PLST model and instructing caregivers in the use behavioral logs. The behavioral logs served as a basis for planning care strategies and focusing discussions on troublesome behaviors during the second phase of the intervention. At the second home visit, the plan of care was reviewed, specific behavioral techniques were taught, and the therapeutic relationship was reinforced. A plan for home safety was also outlined during this phase of the intervention and supporting literature was left with the caregiver. Referrals for support groups, legal counsel, and case management were provided as indicated.
Phase two of the intervention consisted of telephone contacts with subjects (by the same interventionist), approximately every other week, for six months. During follow-up telephone discussions, behavioral logs were reviewed and principles underlying the PLST intervention were reinforced while providing concrete suggestions for managing difficult behaviors exhibited by the care recipient. Throughout both phases of the intervention, caregivers were encouraged to discuss feelings associated with the caregiving experience, as well as general life stressors they encountered, and to be actively involved in the care planning process.
Comparison Intervention
The comparison intervention was identical to the experimental intervention, with the exception of education based on the PLST model. During the first phase of the intervention, a therapeutic relationship was fostered, behavioral logs were discussed, routine information on dementia was provided, a plan for home safety was outlined, and referrals were made for community-based services. Subjects in the comparison group also received follow-up telephone contacts every other week to offer routine information and support. At the study conclusion, subjects in the comparison group were offered the opportunity to receive the experimental intervention
Measures
Subject Demographic and Health Data
Information pertaining to age, sex, race, educational level, employment status, income, financial burden, and perceived social support (Social Provisions Scale) was gathered on each subject for descriptive purposes. Subjects were also asked about their relationship to the care recipient, household composition, hours per week of formal (paid) and informal (friends/family) help with caregiving, frequency of support group attendance, and exposure to other forms of caregiver training.
Immediately before each data collection session, subjects were screened for subjective report of current acute (infectious) illness and quality of sleep the previous night since both variables impact immune parameters. When episodes of acute illness were acknowledged, data collection was postponed until 14 days after symptoms of the illness subsided or ten days after treatment with antibiotics. If the subject did not sleep “as well as usual” the previous night, data collection was postponed until the subject acknowledged a “typical” night of sleep. Additional health data included plasma albumin level, history of chronic illness, over-the-counter and prescription medication usage, daily caffeine intake, weekly alcohol consumption, tobacco use, and approximate hours of sleep per night.
Care Recipient Information
Information pertaining to the care recipient included age, gender, race, type of dementia diagnosed, both acute and chronic health conditions, and medication usage (over-the-counter and prescription). Throughout the intervention phase of the study, caregivers in both treatment groups completed and mailed bi-monthly behavioral logs to indicate current (in the past two weeks) behavioral problems exhibited by the care recipient, as well as strategies used to manage such behaviors. For subjects in the experimental treatment group, information from the behavioral logs was used to formulate individualized care strategies and validate application of the PLST intervention.
Mood
Total mood disturbance (TMD) was evaluated with the 65-item Profile of Mood States (POMS), a factor analytically derived inventory that measures six mood states (Tension-Anxiety, Depression-Dejection, Anger-Hostility, Vigor-Activity, Fatigue-Inertia, and Confusion-Bewilderment), using a 5-point adjective rating scale (McNair, Lorr, & Dropleman, 1971). Subjects were asked to mark the intensity rating that best described how they felt during the past week, including the day of assessment. A TMD (Distress) score was computed by summing the scores across all six mood states, weighting Vigor negatively (range −32 to 200 with lower scores indicating less mood disturbance).
The POMS is a reliable and valid measure of mood disturbance for persons with at least a 7th grade education. This scale is widely used, is a sensitive measure of the effects of experimental manipulations upon normal populations and correlates highly with other scales used to measure affective mood states. Internal consistency for the six subscales ranges from .84–.95. Reliability studies show that respondents’ scores vary over time, supporting the sensitivity of the test to variations in mood. When used with older subjects, psychometric evaluations of the POMS show similar factor structures as with the original standardized samples (Kaye et al., 1988). Construct validity is reported by high correlations between the POMS and other scales measuring emotional states of various types (Peterson & Headen, 1984).
Immune Function
Prior to gathering interview data, a research phlebotomist obtained 40 cubic centimeters (cc) of peripheral venous blood, using heparinized vacutainer tubes (Becton Dickinson, Rutherford, NJ). To control for diurnal variation, all blood samples were obtained within a two-hour window of time and maintained at room temperature as they were promptly transported to our lab at the Iowa City Veterans Administration Medical Center for analysis. Efforts were made to collect data from subjects in each treatment group simultaneously. Blood samples were also collected from a young male control subject each assay day to determine inter-assay variability. Technical difficulties with several assays resulted in the total sample with immune data to vary from one data collection point to another.
Peripheral blood samples were diluted 1:2 in RPMI 1640 medium and a 40 ml diluted sample was layered onto 10 ml of Histopaque 1077 (Sigma). Samples were then centrifuged at 2,500 rpm for 25 minutes in a Sorvall RC3 centrifuge at room temperature. Mononuclear cells were collected from the interface and washed by centrifugation three times to remove all Histopaque. The final cell pellet was resuspended in complete medium consisting of RPMI 1640 supplemented with 1% sodium pyruvate, 1% L-glutamine, 1% Eagles nonessential amino acids, and 10% heat inactivated fetal calf serum (Hyclone). Viable lymphocytes were determined by Erythrosine dye exclusion and resuspended to a concentration of 1 × 106 viable cells/ml in complete medium.
Natural Killer (NK) Cell Cytotoxicity
NK cell cytotoxicity was determined by a 4-hour microtiter 51Chromium (51Cr) release assay (Lubaroff, Reynolds, & Culp, 1979) using the, NK-sensitive, K562 cell line as target cells. Target cells were labeled with 300 μCi of the radioisotope Na251CrO4 (51 Cr) (Amersham) for 60 minutes at 37°C. Target cells were then washed twice and counted (as described above). Target cell concentration was adjusted to 5 × 106 cells/ml in complete media.
Serial 2-fold dilutions of the original lymphocyte suspension were added in triplicate 100 μl aliquots to wells of 96-well, conical bottom tissue culture (microtiter) plates (Costar) containing 100 μl of target cell suspensions. This produced final effector:target ratios ranging from 100:1 to 3.125:1. Additionally, wells containing only target cells suspensions, and wells containing targets plus detergent (1% NP40 or Triton X solution) were prepared to determine spontaneously released radioactivity and maximal lysis. The microtiter plates were then centrifuged for five minutes at 500 rpm before incubation for 4 hours in a 5% CO2 humidified incubator at 37°C.
After incubation, plates were centrifuged at 1100 rpm for ten minutes before 100 μl of supernatant was harvested from each well. Supernatants were counted on a Beckman 300-System gamma counter and percent specific lysis was determined by the formula: 100 X (experimental–cpm spontaneous cpm)/(maximal cpm – spontaneous cpm), where cpm equals gamma counts per minute. This formula determines what percentage of the maximal cell destruction (maximal destruction being the proportion achieved with a detergent) occurs in a given NK/target cell sample, after controlling for effects of spontaneous cell destruction occurring in the absence of NK activity. Lytic units were computed for final analysis of NK data. One lytic unit (LU) was defined as the number of effector cells that were required to lyse 20% of the target cells.
T-Cell Proliferation to ConA and PHA
T-cell proliferative response of peripheral blood mononuclear cells to the mitogens PHA (Sigma) and ConA (Sigma) were measured by tritiated methyl thymidine (3H) incorporation microculture assay (Greiner, Reynolds, & Lubaroff, 1982). For these assays, single lots of both ConA and PHA (mitogens) were purchased, aliquoted, and cryopreserved before the study began. Prior to use in the assays, the mitogens were titrated and multiple dose-response curves were determined. The optimal doses of PHA were 2.5×10−5g/ml and 1.25×10−5 g/ml while the optimal doses for ConA were 1.25×10−4 g/ml and 6.25×10−5g/ml.
To determine the proliferative response of lymphocytes, effectors were resuspended to a concentration of 1× 106/ml. and triplicate cultures of each subject’s effectors were stimulated with the optimal concentrations of ConA and PHA in 96-well round-bottom microtiter plates. Triplicate wells also contained media alone and effectors alone for determination of background proliferation. Following incubation for 42 and 66 hours at 37°C in a 5% CO2 humidified incubator, each well was pulsed with 0.1 μCi of 3H-thymidine and re-incubated for another six hours. Cells were harvested after a total of 48 and 72 hours of incubation, onto glass fiber disks (Whatman GF/A) using a cell harvester.
The amount of radioactive 3H-thymidine utilized by effectors was determined by a Liquid Beta Scintillation counter (Beckman, Fullerton Ca). Each subject’s effector responsiveness at various concentrations of mitogens was expressed as a Stimulation Index (SI). The Stimulation Index formula was computed as follows: SI = (counts per minute or cpm with mitogen) ÷ (cpm without mitogen). In each case, the SI is the average of the triplicate wells treated in the same manner.
Results
Sample
The typical subject was a Caucasian (100%) female (92%) spouse (73%) with a mean age of 65.49 (± 10.75). Subjects had at least one year of higher education (M = 13.81 years, ± 2.26) with a combined annual income from $10,000 to $30,000 (51.4%) and verbalized no financial burden (81.9%). Approximately one-third of the sample (38%) utilized community-based services (e.g., home health or respite care) with an average of 13.76 hours (± 28.55) of paid help per week while friends and family members assisted with caregiving an average of 2.78 (± 5.08) hours a week. Random assignment resulted in a significant difference (t (37) = −2.81 [p = .009]) between subjects in each treatment group based on total hours of care provision per week. Subjects in the comparison group provided an average of 161.57 (± 10.13) hours of care per week while subjects in the experimental group provided an average of 133.35 (± 46.27) hours per week. Most of the sample (97.3%) reported no previous caregiver training or education although approximately one-third the sample (37.8%) attended a caregiver support group on a monthly basis. Perceived social support among the sample reflected normative data for community dwelling older adults (Cutrona & Russell, 1987).
Sample Health and Health-Related Behaviors
The sample was relatively healthy with one subject experiencing an acute episode of pneumonia and the total sample reporting from one to two chronic medical conditions. There was not a statistically significant difference between treatment groups based on the number of subjects taking beta-blockers or hormone replacement therapy with approximately one-fifth of the sample (20.6%) taking beta blockers and nearly one-half of the female caregivers (44.1%) taking hormone replacement therapy. Plasma albumin levels were calculated as a rough indication of nutritional status and all subjects were within normal limits. The typical subject slept approximately six hours a night, drank one-half cup of caffeinated beverage a day, and rarely consumed alcohol or tobacco products. Caregiver health-related variables did not change over the course of the study.
Care Recipient Characteristics
Subjects typically cared for male (67.6%), Caucasian (100%) spouses (73%) who were approximately ten years older (M = 74.29 years, ±11.29) and had one (32.4%) or two (27.0 %) chronic illness (e.g., diabetes, hypertension) in addition to dementia. A majority of care recipients had a diagnosis of dementia of the Alzheimer’s type (43.2%) for an average of five years (M = 61.51 months, ±63.17). Other types of dementia diagnosed among care recipients include vascular dementia (13.5%), mixed dementia (13.5%), other etiologies (e.g., Pick’s and Parkinson’s disease, 13.5%), dementia of unknown etiology (10.8%), and no formal diagnosis of dementia (5.4%). Care recipients repeatedly exhibited an average of 23.57 (± 6.85) problematic behaviors over a two-week time interval.
Mood Outcomes
Preliminary analysis (independent sample t-test) revealed that subjects in the comparison group were significantly more distressed (higher TMD scores) than subjects in the experimental group at baseline (t (37) = −2.09, [p = .044]). Analysis of POMS subscale scores revealed that the comparison group was significantly more depressed (t (37) = −2.22, [p = .033]) and fatigued (t (37) = −2.10, [p = .043]) at baseline, compared to the experimental group.
The experimental intervention did not significantly impact mood outcomes over the course of the study. Repeated measures, two-way ANCOVA (controlling for initial differences between group means on TMD scores) did not reveal a significant group by time interaction effect for TMD scores, nor were there significant main effects for treatment group or time (see Table 1). Effect size for treatment group assignment on TMD scores was R2 = .050, indicating a very weak association between treatment group status and mood outcomes.
Table 1.
Treatment group means (SDs); interaction and main effects of repeated measures ANCOVA (controlling for initial differences on baseline TMD scores)
| T1 Means (SDs) | T2 Means (SDs) | T3 Means (SDs) | Group by Time Interaction Effect F statistic (p value) | Group Main Effect F statistic (p value) | Time Main Effect F statistic (p value) | ||
|---|---|---|---|---|---|---|---|
| TMD | Experimental | 36.67 (35.59) | 36.24 (31.39) | 29.80 (38.58) | 0.824 (.371) | 0.058 (.811) | 0.899 (.350) |
| Comparison | 57.14 (25.07) | 58.14 (30.82) | 39.79 (36.77) | ||||
| NK (LU) | Experimental | 2.25 (.44) | 2.37 (.21) | 2.32 (.29) | 1.040 (.360) | 0.007 (.934) | 0.620 (.541) |
| Comparison | 2.27 (.34) | 2.29 (.29) | 2.38 (.37) | ||||
| PHA (SI) | Experimental | 1.58 (.89) | 2.11 (.43) | 2.31 (.19) | .987 (.387) | 6.757* (.015) | 2.36 (.105) |
| Comparison | 1.09 (.89) | 1.14 (1.00) | 2.07 (.29) | ||||
| ConA (SI) | Experimental | 1.65 (.76) | 1.99 (.37) | 2.12 (.22) | 2.025 (.1410) | 12.315* (.001) | 1.645 (.202) |
| Comparison | 1.34 (.86) | 1.15 (.82) | 1.81 (.38) |
Significant at α = 0.05 (two-tailed)
Note: E = Experimental Group and C = Comparison Group
Note: Higher group means indicate healthier immune and mood outcomes
Note: LU = Lytic Units and SI = Stimulation Index
Immune Outcomes
Similarly, no interaction effect was detected for treatment group assignment over time for any of the immune outcomes (see Table 1), although significant main effects for treatment group were found for both of the T-cell specific immune assays (proliferation to PHA and ConA). Further analysis (One-way ANCOVA) revealed that subjects in the experimental treatment group demonstrated significantly stronger T-cell proliferation to PHA and ConA after the in-home intervention (T2) and after six months of telephone support (T3) than subjects in the comparison group (see Table 2). While the effect size for treatment group assignment on NK cell cytotoxicity was extremely low (R2 = .051), the magnitude of the association between T-cell proliferation and treatment group assignment was estimated to be R2 = .716 for PHA proliferation and R2 = .919 for ConA proliferation.
Table 2.
One-way ANCOVA treatment group effects (controlling for initial differences on baseline TMD scores)
| T1 F statistic (p value) | T2 F statistic (p value) | T3 F statistic (p value) | |
|---|---|---|---|
| PHA (SI) | 1.175 (.288) | 14.474* (.001) | 11.130* (.002) |
| ConA (SI) | 0.832 (.368) | 15.809* (.000) | 9.845* (.004) |
Significant at α = 0.05 (two-tailed)
Note: SI = Stimulation Index
Discussion
It is difficult to compare results from the current study with others evaluating mood and immune outcomes of interventions with dementia caregivers since only one such study has been published to date and it did not employ an experimental design (Wilkins, Castle, Heck, Tanzy, & Fahey, 1999). In the study by Wilkins and associates, T-cell proliferative responses to PHA significantly deteriorated by completion of an eight-week group psychoeducational intervention, but showed a trend for improvement one-month after the intervention (Wilkins et al., 1999). In the current study, subjects in both groups demonstrated improvements in T-cell proliferative responses over the course of the study, although subjects in the experimental group demonstrated significantly stronger (higher) T-cell proliferation responses after the intervention (T2 and T3) than subjects in the comparison group. Differences in intervention formats (group versus individualized) may explain the discrepant findings of these two studies since meta-analytic reviews show that group psychosocial interventions are associated with small positive effects on caregiver distress whereas individualized psychosocial interventions demonstrate moderately strong effects (Kennet, Burgio, & Schulz, 2000; Knight, Lutzy, & Macofsky-Urban, 1993). Findings related to the impact of the PLST intervention on immune outcomes are consistent with the psychoneuroimmunology (PNI) literature (Kiecolt-Glaser & Glaser, 1992; Kiecolt-Glaser et al., 1985), where psychosocial intervention studies among distressed subjects (medical students, psychiatric inpatients, cancer patients) show long-term enhancement of mitogen-stimulated T-cell proliferative responses with equivocal results for NK cell cytotoxicity outcomes.
The NK cell cytotoxicity outcomes of this pilot study are consistent with the PNI literature for older adults (Esterling et al., 1994) and may be explained by data from the laboratory of Grant and associates where caregivers were not significantly different from demographically matched non-caregiving controls for NK cell cytotoxicity, neuroendocrine products, or measures of sympathetic nervous system activation (Grant, Patterson, Hauger, & Irwin, 1992). Grant and colleagues reported that highly stressed caregivers demonstrated higher basal plasma adrenocorticotropic hormone (ACTH) levels than less stressed caregivers (Irwin et al., 1997). This finding is important because high levels of ACTH are known to depress immune function (Holsboer, 2000).
Findings from this study do not support the hypothesis that the PLST intervention enhanced mood outcomes of caregivers. While mood scores improved for both treatment groups over the course of the study, the relatively large standard deviations and small sample size limit the power of this study (R2 = .051 to .553 for individual TMD subscale scores) to detect significant improvements in mood states over time. Further, mood data in this study were not consistent with those of Buckwalter and associates, where treatment group differences in POMS TMD scores approached statistical significance (p=.08) at six-months post intervention (Buckwalter et al., 1999a). When examining the subscales that make up the POMS TMD score, Buckwalter’s group found that caregivers in the PLST intervention group were significantly less depressed (p=.0007), less anxious (p=.006), less angry (p=.02), less fatigued (p=.003), and less confused (p=.0001) than caregivers in the comparison group after six months (T3) of telephone support for the PLST intervention (Buckwalter et al., 1999b). It is plausible that sampling error accounted for the incongruent mood findings between this study and the primary study since caregivers in the pilot study comparison treatment group provided significantly more hours of care per week (F(37) = 13.77, [p = .001]) and were more likely to live alone with the care recipient (versus with other family members) than caregivers in the experimental treatment group (F(37) = 12.96, [p = .001]).
Overall, results of this pilot study suggest that the PLST intervention enhances or preserves T-cell immune function of caregivers. While changes in immune function do not directly translate into changes in health status, these immune data have particular relevance for health outcomes among older persons since significant decrements in immunocompetence are normally associated with aging, and poor cellular immunocompetence is associated with higher mortality in persons over the age of 80 (Roberts-Thomson, Whittingham, Youngchaiyud, & Mackay, 1984). Further work in this area will provide clearer evidence of the extent to which positive immune changes may be translated into improvements in physical and psychological health.
Limitations
The relatively small sample size and large standard deviations negatively affected the power of this study to detect statistically significant differences between treatment groups. A Type II error may have been present because sample size and power calculations computed for each of the hypotheses tested were based on data from a descriptive study of caregiving and non-caregiving older persons (Kiecolt-Glaser et al., 1991). Perhaps a greater difference in mood and/or immune outcomes would have been detected between treatment groups if a wait list control group (e.g., a third group receiving no intervention) had been included in the design, but time and monetary constraints, along with Institutional Review Board considerations, precluded inclusion of a third, non-treatment (control) group.
A combination of random and systematic measurement error may have also contributed to the current findings. While random error was expected with measures of immunity, systematic error was controlled for by using a valid and reliable instrument to detect changes in mood disturbance. Despite the fact that the instrument used in this study demonstrated sound psychometric properties when used with older adults, it is possible that Profile of Mood States is not an appropriate measure of distress among chronically distressed dementia caregivers.
Lastly, the internal validity of this study may have been jeopardized by selection bias because the random assignment of subjects to treatment condition resulted in nonequivalent groups. This is a limitation given that the statistically significant differences in T-cell proliferative responses may also be explained by initial group differences on mood scores and hours of care provision per week, rather than the intervention provided. Along similar lines, stringent inclusion criteria and subject attrition may have jeopardized the study’s external validity. While strict selection criteria are necessary to maintain the internal validity of studies employing immune outcomes (e.g., to make certain that the relationship between the intervention and outcome is not spurious), they also limit the generalizability of the findings to subjects meeting similar criteria. Likewise, even though attrition in this study was low (5.1%) and random (one subject from each treatment group stopped participation before completion of the intervention phase), the findings cannot be generalized to family caregivers seriously considering institutional placement of the care recipient. Further research, using larger and more geographically and ethnically diverse samples that are more representative of the caregiving population at large, is required to validate these preliminary findings, and before results can be applied to caregivers of persons with dementia in general.
Implications for Psychiatric Nursing
The field of psychiatric nursing is undergoing a paradigm shift; directed by advances in biomolecular technology, the identification of new and more effective psychopharmacologic treatments, and an explosion of knowledge related to the neurobiologic basis of mental illness (Flaskerud, 2000). Some of the most important breakthroughs in research into mental illness are occurring through the examination of problems in the neuroendocrine and immune responses to stressors. Studies exploring the complex relationships between the nervous, endocrine, and immune systems (psychoneuroimmunology or PNI) strongly suggest bi-directional communications between these systems, with each modulating the other. There is also consensus that psychological processes can compromise the immune system, and conversely, that components of the immune system can directly influence brain function (reviewed in Ader, Felton, & Cohen, 1991).
Psychiatric nurses are positioned to integrate biologic, behavioral, and environmental concepts into practice, education, and research while remaining centered in the nursing domain and maintaining a focus on caring and sensitivity to the human condition (Flaskerud, 2000). While basic scientists use the PNI framework to generate knowledge about biological and behavioral mechanisms, psychiatric nurse investigators are using similar frameworks to examine the relationships between biological and behavioral phenomena and their influences on health outcomes (Zeller, McCain, McCann, Swanson, & Colletti, 1996). Grounded in a PNI framework, goals of this pilot study were to determine if a nursing intervention designed to reduce caregiver stress would improve the mood states and immune function of family dementia caregivers.
With a tradition of promoting health and maintaining the quality of life of persons with chronic and debilitating diseases, it is extremely important for psychiatric nurses to continue developing, implementing, and evaluating interventions that directly or indirectly affect the daily functioning and health needs of individuals with dementia and their families. Finding from this pilot study suggest that psychiatric nurses endorse the concept of holism when providing care to persons with dementia. Evaluation and treatment of patients with dementia must include a systematic assessment of the caregivers’ health and the caregiving situation. The assessment should include the caregivers’ perceptions of stress, availability of and satisfaction with support systems, the use of coping behaviors, and the presence of depressive symptomatology. Further, since caregivers may be more susceptible to the development of bacterial or viral infections, their physical health status should be monitored frequently and education provided regarding the importance of self-care practices in relation to sleep, nutrition, exercise, stress management, and annual immunizations.
Acknowledgments
The authors wish to express sincere gratitude to Susan Lutgendorf, Ph.D., from the University of Iowa Department of Psychology, for her invaluable guidance in the conduct of this study and Mary Amanda Dew, Ph.D., from the University of Pittsburgh Departments of Psychiatry, Psychology, and Epidemiology, for statistical consultation and guidance in the preparation of this manuscript.
This study was funded through the National Institute of Health (NIH), Office of Research in Women’s Health (ORWH) as an administrative supplement to a four-year, multi-site study evaluating the effects of the PLST intervention on caregiver emotional responses (NINR RO1 NR03234). Additional support was provided through research training grants from NIMH (T32 MH19986), NIA (T32 AG 00214), and NINR (F31 NR07114-01A2 and T32 NR7058).
References
- Ader R, Felton DL, Cohen N, editors. Psychoneuroimmunology. 2. New York: Academic Press; 1991. [Google Scholar]
- Bedard M, Molloy DW, Pedlar D, Lever JA, Stones MJ. 1997 IPA/Bayer Research Awards in Psychogeriatrics. Associations between dysfunctional behaviors, gender, and burden in spousal caregivers of cognitively impaired older adults. International Psychogeriatrics. 1997;9(3):277–90. doi: 10.1017/s1041610297004444. [DOI] [PubMed] [Google Scholar]
- Buckwalter KC, Gerdner LA, Hall GR, Kelly A, Kohout F, Richards B, Sime M. Effects of family caregiver home training based on the progressively lowered stress threshold model. In: Gueldner SH, Poon LW, editors. Gerontological nursing issues for the 21st century: A multidisciplinary dialogue commemorating the International Year of Older Persons. Washington, DC: Sigma Theta Tau International; 1999a. pp. 81–98. [Google Scholar]
- Buckwalter KC, Gerdner L, Kohout F, Hall GR, Kelly A, Richards B, Sime M. A nursing intervention to decrease depression in family caregivers of persons with dementia. Archives of Psychiatric Nursing. 1999b;13(2):80–8. doi: 10.1016/s0883-9417(99)80024-7. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Poehlmann KM, Kiecolt-Glaser JK, Malarkey WB, Burleson MH, Bernston GG, Glaser R. Cellular immune response to acute stress in female caregivers of dementia patients and matched controls. Health Psychology. 1998;17(2):182–189. doi: 10.1037//0278-6133.17.2.182. [DOI] [PubMed] [Google Scholar]
- Chappell NL, Penning M. Behavioral problems and distress among caregivers of people with dementia. Ageing and Society. 1996;16:57–73. [Google Scholar]
- Coen D, Swanwick GRJ, O’Boyle CA, Coakley D. Behaviour disturbances and other predictors of carer burden in Alzheimer’s disease. International Journal of Geriatric Psychiatry. 1997;12:331–336. [PubMed] [Google Scholar]
- Cook JM, Peason JL, Ahrens AH. General and specific events and depressive symptoms in Alzheimer’s disease caregivers. American Journal of Alzheimer’s Disease. 1997;122:32–34. [Google Scholar]
- Cutrona CE, Russell DW. The provisions of social relationships and adaptation to stress. In: Jones WH, Perlman D, editors. Advances in personal relationships. Greenwich, CT: JAI Press; 1987. [Google Scholar]
- Drebing CE. Trends in the content and methodology of Alzheimer’s caregiving research. Alzheimer’s Disease & Associated Disorders. 1999;13(Suppl 1):S93–S100. doi: 10.1097/00002093-199904001-00020. [DOI] [PubMed] [Google Scholar]
- Esterling BA, Kiecolt-Glaser JK, Bodnar JC, Glaser R. Chronic stress, social support, and persistent alterations in natural killer cell response to cytokines in older adults. Health Psychology. 1994;13(4):291–298. doi: 10.1037//0278-6133.13.4.291. [DOI] [PubMed] [Google Scholar]
- Flaskerud JH. Shifting paradigms to neuropsychiatric nursing. Issue in Mental Health Nursing. 2000;21:1–2. doi: 10.1080/016128400248220. [DOI] [PubMed] [Google Scholar]
- Grant I, Patterson T, Hauger R, Irwin M. Biopsychosocial aspects of Alzheimer caregiving: The UCSD study. Archives of Psychiatry. 1992;4(Suppl):77–80. [Google Scholar]
- Greiner DL, Reynolds CW, Lubaroff DM. Maturation of functional T-lymphocyte subpopulations in the rat. Thymus. 1982;4:77–90. [PubMed] [Google Scholar]
- Hall GR. Testing the PLST model with community-based caregivers. Dissertation Abstracts International. 1999;60(02):577. (University Microfilms No. AAT9917556) [Google Scholar]
- Hall GR, Buckwalter KC. Progressively lowered stress threshold: A conceptual model for care of adults with Alzheimer’s disease. Archives of Psychiatric Nursing. 1987;1:399–406. [PubMed] [Google Scholar]
- Herbert TB, Cohen S. Depression and immunity: A meta-analytic review. Psychological Bulletin. 1993a;113:472–486. doi: 10.1037/0033-2909.113.3.472. [DOI] [PubMed] [Google Scholar]
- Herbert T, Cohen S. Stress and Immunity in humans: A meta-analytic review. Psychosomatic Medicine. 1993b;55:364–379. doi: 10.1097/00006842-199307000-00004. [DOI] [PubMed] [Google Scholar]
- Holsboer F. The corticosteroid receptor hypothesis of depression. Neuropsychopharmacology. 2000;23:477–501. doi: 10.1016/S0893-133X(00)00159-7. [DOI] [PubMed] [Google Scholar]
- Irwin M. Stress-induced immune suppression: Role of brain corticotropin releasing hormone and autonomic nervous system mechanisms. Advances in Neuroimmunology. 1994;4:29–47. doi: 10.1016/s0960-5428(06)80188-9. [DOI] [PubMed] [Google Scholar]
- Irwin M, Hauger R, Patterson TL, Semple S, Siegler M, Grant I. Alzheimer’ caregiver stress: Basal natural killer cell activity, pituitary-adrenal cortical function, and sympathetic tone. Annals of Behavioral Medicine. 1997;19(2):83–90. doi: 10.1007/BF02883324. [DOI] [PubMed] [Google Scholar]
- Kaye JM, Lawton MP, Gitlin LN, Kleban MH, Windson LA, Kaye D. Older people’s performance on the Profile of Mood States (POMS) Clinical Gerontologist. 1988;7:35–36. [Google Scholar]
- Kennet J, Burgio L, Schulz R. Interventions for in-home caregivers: A review of research 1990 to present. In: Schulz R, editor. Handbook on dementia caregiving: Evidence-based interventions for family caregivers. New York, NY: Springer Publishing Co, Inc; 2000. pp. 61–125. [Google Scholar]
- Kiecolt-Glaser JK. Stress, personal relationships, and immune function: Health implications. Brain, Behavior, and Immunity. 1999;13:61–72. doi: 10.1006/brbi.1999.0552. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Dura JR, Speicher CE, Trask OJ, Glaser R. Spousal caregivers of dementia victims: Longitudinal changes in immunity and health. Psychosomatic Medicine. 1991;53:345–362. doi: 10.1097/00006842-199107000-00001. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Glaser R. Caregiving, mental health, and immune function. In: Light E, Lebowitz BD, editors. Alzheimer’s disease treatment and family stress. New York: Hemisphere Publishing Corporation; 1990. pp. 245–266. [Google Scholar]
- Kiecolt-Glaser JK, Glaser R. Psychoneuroimmunology: Can psychological interventions modulate immunity? Journal of Consulting and Clinical Psychology. 1992;60(4):569–575. doi: 10.1037//0022-006x.60.4.569. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Glaser R. Chronic stress and mortality among older adults. Journal of the American Medical Association. 1999;282(23):2259–2260. doi: 10.1001/jama.282.23.2259. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Glaser R, Williger D, Stout J, Messick G, Sheppard S, Ricker D, Romisher SC, Briner W, Bonnell G, Donnerberg R. Psychosocial enhancement of immunocompetence in a geriatric population. Health Psychology. 1985;4(1):25–41. doi: 10.1037//0278-6133.4.1.25. [DOI] [PubMed] [Google Scholar]
- Knight BG, Lutzy SM, Macofsky-Urban F. A meta-analytic review of interventions for caregiver distress: Recommendations for future research. The Gerontologist. 1993;33:240–248. doi: 10.1093/geront/33.2.240. [DOI] [PubMed] [Google Scholar]
- Lawton MP. Competence, environmental press and the adaptation of older people. In: Windley PG, Byerts TO, Ernst FG, editors. Theory Development in Environment and Aging. Washington, DC: Gerontological Society; 1975. pp. 85–89. [Google Scholar]
- Levesque L, Cossette S, Laurin L. A multidimensional examination of the psychological and social well-being of caregivers of a demented relative. Research on Aging. 1995;17:332–360. [Google Scholar]
- Lubaroff DM, Reynolds CW, Culp DA. Immunologic studies of prostatic cancer using the R3327 rat model. Transactions of the American Association of GU Surgeons. 1979;70:60–63. [PubMed] [Google Scholar]
- Maas M, Buckwalter KC. Final report, nursing evaluation research: A special Alzheimer’s unit. Bethesda, MD: NIH/NINR; 1991. [Google Scholar]
- McNair DM, Lorr M, Droppleman LF. The profile of mood states manual. San Diego, CA: Educational and Industrial Testing Service; 1971. [Google Scholar]
- Peterson R, Headen S, editors. Profile of mood states. Vol. 1. Kansas City, MO: Westport Publishers; 1984. [Google Scholar]
- Pruchno RA, Resch NL. Aberrant behaviors and Alzheimer’s disease: Mental health effects on spouse caregivers. Journal of Gerontology. 1989;44:S177–S182. doi: 10.1093/geronj/44.5.s177. [DOI] [PubMed] [Google Scholar]
- Roberts-Thomson IC, Whittingham S, Youngchaiyud U, Mackay IR. Aging, immune response, and mortality. The Lancet. 1984;2:368–370. doi: 10.1016/s0140-6736(74)91755-3. [DOI] [PubMed] [Google Scholar]
- Schulz R, Beach SR. Caregiving as a risk factor for mortality. Journal of the American Medical Association. 1999;282(23):2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- Schulz R, Newsom J, Mittelmark M, Burton L, Kirsch C, Jackson S. Health effects of caregiving: The caregiver health effects study: An ancillary study of the cardiovascular health study. Annals of Behavioral Medicine. 1997;19(2):110–116. doi: 10.1007/BF02883327. [DOI] [PubMed] [Google Scholar]
- Schulz R, O’Brien AT, Bookwala J, Fleissner K. Psychiatric and physical morbidity effects of dementia caregiving: Prevalence, correlates, and causes. The Gerontologist. 1995;35(6):771–791. doi: 10.1093/geront/35.6.771. [DOI] [PubMed] [Google Scholar]
- Schulz R, Visintainer P, Williamson GM. Psychiatric and physical morbidity effects of caregiving. Journal of Gerontology: Psychological Sciences. 1990;45:P181–P191. doi: 10.1093/geronj/45.5.p181. [DOI] [PubMed] [Google Scholar]
- Shaw WS, Patterson TL, Semple SJ, Ho S, Irwin MR, Grant I. Longitudinal analysis of multiple indicators of health decline among spousal caregivers. Annals of Behavioral Medicine. 1997;19(2):101–109. doi: 10.1007/BF02883326. [DOI] [PubMed] [Google Scholar]
- Song LY, Biegel DE, Milligan SE. Predictors of depressive symptomatology among lower social class caregivers of persons with chronic mental illness. Community Mental Health Journal. 1997;33:269–286. doi: 10.1023/a:1025090906696. [DOI] [PubMed] [Google Scholar]
- Streuning EOL, Stueve A, Vince P, Kreisman DE, Link BG, Herman DB. Factors associated with grief and depressive symptoms in caregivers of people with serious mental illness. Research in Community Mental Health. 1995;9:91–124. [Google Scholar]
- Stuckey JC, Neundorfer MM, Smyth KA. Burden and well-being: The same coin or related currency? The Gerontologist. 1996;36:686–693. doi: 10.1093/geront/36.5.686. [DOI] [PubMed] [Google Scholar]
- Teri L. Behavior and caregiver burden: Behavioral problems in patients with Alzheimer’s disease and its association with caregiver stress. Alzheimer’s Disease and Associated Disorders. 1997;11(4):s35–s38. [PubMed] [Google Scholar]
- Vedhara K, Cox NKM, Wilcock GK, Perks P, Hunt M, Anderson S, Lightman SL, Shanks NM. Chronic stress in elderly carers of dementia patients and antibody response to influenza vaccination. The Lancet. 1999;353(9153):627–631. doi: 10.1016/S0140-6736(98)06098-X. [DOI] [PubMed] [Google Scholar]
- Vitaliano PP. Physiological and physical concomitants of caregiving: Introduction to special issue. Annals of Behavioral Medicine. 1997;19(2):75–77. doi: 10.1007/BF02883322. [DOI] [PubMed] [Google Scholar]
- Vitaliano PP, Scanlan JM, Ochs HD, Syrjala K, Siegler IC, Snyder EA. Psychological distress, caregiving, and metabolic variables. Journals of Gerontology: Psychological Sciences. 1998;51B(5):290–299. doi: 10.1093/geronb/51b.5.p290. [DOI] [PubMed] [Google Scholar]
- Weisse CS. Depression and immunocompetence: A review of the literature. Psychological Bulletin. 1992;111(3):475–489. doi: 10.1037/0033-2909.111.3.475. [DOI] [PubMed] [Google Scholar]
- Wilkins SS, Castle S, Heck E, Tanzy K, Fahey J. Immune function, mood, and perceived burden among caregivers participating in a psychoeducational intervention. Psychiatric Services. 1999;50(6):747–9. doi: 10.1176/ps.50.6.747. [DOI] [PubMed] [Google Scholar]
- Williamson G, Schulz R. Coping with specific stressors in Alzheimer’s disease caregiving. The Gerontologist. 1993;33:747–755. doi: 10.1093/geront/33.6.747. [DOI] [PubMed] [Google Scholar]
- Wolanin MO, Phillips LR. Confusion: Prevention and care. St. Louis: Mosby; 1981. [Google Scholar]
- Zeller JM, McCain NL, McCann JJ, Swanson B, Colletti MA. Methodologic issues in psychoneuroimmunology research. Nursing Research. 1996;45(5):314–318. doi: 10.1097/00006199-199609000-00012. [DOI] [PubMed] [Google Scholar]