Abstract
Objective
To explore bidirectional comorbidity between bipolar disorder (BPD) and obsessive-compulsive disorder (OCD) in youth and to examine the symptom profile and clinical correlates of both the disorders in the context of reciprocal comorbidity and ascertainment status.
Methods
Two samples of consecutively referred youth (ages 6–17 years) ascertained contemporaneously for respective studies of BPD and OCD were compared using clinical and scalar assessment and structured diagnostic interviews.
Results
A total of 21% (17/82) of the BPD subjects and 15% (19/125) of the OCD subjects met DSM-III-R diagnostic criteria for both disorders. In the presence of BPD, youth with OCD more frequently experienced hoarding/saving obsessions and compulsions along with a clinical profile of greater comorbidity, poorer global functioning and higher rate of hospitalization that is characteristic of BPD. Multiple anxiety disorders (≥3), especially generalized anxiety disorder and social phobia, were present at a higher frequency when OCD and BPD were comorbid than otherwise. In subjects with comorbid OCD and BPD, the primary disorder of ascertainment was associated with an earlier onset and more severe impairment.
Conclusions
An unexpectedly high rate of comorbidity between BPD and OCD was observed in youth irrespective of primary ascertainment diagnosis. In youth with comorbid OCD and BPD, the clinical characteristics of each disorder run true and are analogues to their clinical presentation in youth without reciprocal comorbidity, with the exception of increased risk for obsessions and compulsions of hoarding/saving and comorbidity with other anxiety disorders.
Keywords: bipolar disorder, comorbidity, obsessive, compulsive disorder, OCD, youth
Minimal extant literature and no systematic data exist on the challenging clinical dilemma of children and adolescents who present with obsessive-compulsive disorder (OCD) that is comorbid with bipolar disorder (BPD). Individually, each disorder may inflict a significant burden on children and their families with a prevalence of at least 1% (1–3). Although the diagnosis of BPD in children has generated some controversy in the child psychiatry community, recent reports suggest that it is not uncommon in clinical settings, and, when present, is often accompanied by high levels of anxiety, including OCD (4–11). Despite the fact that descriptions of OCD symptoms in patients with BPD date back to the 19th century (12), almost all reports on the comorbidity of BPD and OCD are descriptive rather than systematic and focus exclusively on adults (13–15). In adults, evidence of a higher than expected overlap between OCD and BPD first came from the Epidemiological Catchment Area study, where 23% of those with BPD also met criteria for OCD (16). Subsequent studies have consistently found a greater than expected overlap between OCD and BPD at rates as high as 15–35% (17–19).
The unexpectedly frequent concurrence of these two disorders may have both clinical and scientific implications. OCD and BPD comorbidity in adults may herald an episodic course of OCD with higher rates of certain obsessions (aggressive/impulsive, sexual, religious, and obsessional doubts) and compulsions (compulsions of control, hoarding, ordering/arranging), which require more frequent hospitalizations and complex pharmacological interventions (17, 20–22). Similarly, the presence of OCD comorbidity has been reported to predict a more chronic course of BPD and greater frequency of major depressive episodes, with a trend toward poor response to mood stabilizers (17, 23). Because pharmacological treatments of the two illnesses diverge and medications used to manage OCD can exacerbate BPD symptoms, their co-occurrence is a therapeutic challenge for clinicians.
Despite the frequent juvenile onset of both OCD and BPD, little attention is paid to the presence of comorbid OCD and BPD in youth. Rates of comorbid OCD in the range of 15–44% have been reported in pediatric BPD populations (4, 8) and, similarly, studies of OCD have documented comorbidity rates of mania as high as 27–45% (24, 25).
The only reports addressing the clinical presentation of comorbid OCD and BPD in a pediatric population suggest that when BPD and OCD co-occur in young patients, both clinical syndromes have a substantial and additive impact on clinical presentation and global functioning (24, 26).
If, as the literature suggests, BPD and OCD co-occur in children and adolescents at rates greater than expected with significant bidirectional overlap, the nature of this relationship remains underexamined. Identification of BPD and OCD comorbidity based on DSM nomenclature (27) may represent as an artifact a secondary phenomenon (28), an unusual manifestation of a more severe form of disorder, a product of the selection bias (referral or ascertainment), or instead, a marker for a specific subtype of disorder (29). Alternatively, BPD and OCD could represent valid comorbid ‘nosologically true’ disorders. If nosologically true, then the syndromatic presentation and associated clinical correlates, including other comorbidities and functional indices of each disorder, should be readily recognizable in children who present with both the disorders, and furthermore, neither referral nor ascertainment bias should substantially alter the clinical characteristics of each disorder.
Parsing out the relationship between comorbid disorders has significant therapeutic implications, as the decision to treat either one or both the disorders may be dictated by whether or not one disorder is secondary to the other. Additionally, scientific delineation of comorbid BPD and OCD from OCD and mood disorders may lead to the identification of a more homogeneous clinical subtype of disorder with distinct psychopathology, familiality, and genetic underpinnings.
One avenue for the exploration of the BPD and OCD comorbidity is the examination of the symptom presentation and other clinical correlates of BPD and OCD in the context of reciprocal comorbidity and ascertainment status. If the clinical correlates of the comorbid disorders are indistinguishable from their respective typical presentation and if their comorbid presentation does not alter with different focus for ascertainment, it would suggest that the comorbidity is a valid co-occurrence of disorders and not an artifact. We hypothesized that children and adolescents who fulfill the DSM nosological criteria of both BPD and OCD suffer from both the disorders. To this end, we analyzed data on children and adolescents with BPD and OCD ascertained contemporaneously for a study of pediatric OCD and of pediatric BPD with an aim to compare the clinical characteristics of OCD and BPD in youth (i) with and without reciprocal comorbidity and (ii) with reciprocal comorbidity ascertained through an OCD diagnosis versus those ascertained for a BPD diagnosis.
Methods
Subjects
Subjects were probands participating in a National Institute of Mental Health (NIMH)-funded family genetic study of pediatric OCD (NIMH K08 MH01481, principal investigator: DG; N = 125) and a contemporaneous NIMH-funded family genetic study of pediatric BPD (NIMH K08 MH01503-05; principal investigator: JW; N = 82) using identical methodology details of which are available in Geller et al. (30) and Wozniak et al. (31), respectively. These subjects, aged 6–17 years, were primarily ascertained for BPD or for OCD from the pediatric psychopharmacology program at the Massachusetts General Hospital, Boston, MA, USA. Each study was approved by the Subcommittee on Human Studies of the Massachusetts General Hospital.
All children and adolescents were evaluated by the principal investigator of the respective study by conducting direct clinical interview of the subjects along with their parent(s) and by administering the Schedule for Affective Disorders and Schizophrenia for School-Age Children-Epidemiologic Version (K-SADS-E)(32) to the parent(s), usually the mother, and to the youth aged 12 and older. K-SADS-E interviews were conducted by raters who had been trained and supervised by the senior investigator (JB). For every diagnosis, information was gathered regarding the age at onset and offset of symptoms, number of episodes, and treatment history. All diagnoses were reviewed by a diagnostic sign-off committee chaired by one of the senior program board-certified child psychiatrists (JB, JW, DG), who reviewed both the items endorsed during the interview and detailed notes taken by the interviewer.
All diagnoses of mania and OCD were presented for review and were considered positive only if there was consensus that diagnostic criteria were met to a degree that would be considered clinically meaningful. By ‘clinically meaningful’ we mean that the data collected from the structured interview indicated that the diagnosis should be a clinical concern due to the nature of the symptoms, the associated impairment, and the coherence of the clinical picture. Thus, these diagnoses were of clinical concern and not simply research diagnosis computed by counting symptoms endorsed and applying an algorithm. We computed kappa (κ) coefficients of diagnostic agreement by having three experienced, board-certified, blinded child and adolescent psychiatrists diagnose subjects from audio taped interviews of parent and subject (aged 12 and older) made by the assessment staff. Based on 500 assessments, the median κ was 0.98. We attained a κ of 1.0 for OCD and 0.95 for mania.
To be given the lifetime diagnosis of mania, the child had to meet the full DSM-III-R criteria for a manic episode with associated impairment. To be given the diagnosis of OCD, the child had to meet full DSM-III-R diagnostic criteria for OCD. In addressing the course of mania, we utilized information on subjects’ onset and offset ages, to determine the duration of the disorder, combined with their reported number of lifetime episodes, to yield a categorical description of their manic experience as being either chronic or episodic. A chronic course was defined by more than four reported episodes per year, multiple episodes each lasting (on average) at least 12 months, or a single episode lasting more than 12 months.
Severity and type of obsessive and compulsive symptoms were rated by using the Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS) (33). Psychosocial functioning was assessed using the Global Assessment of Functioning Scale (GAF) (34). Socioeconomic status (SES) was measured using the Hollingshead Four-Factor Index, with lower scores indicating higher SES (35). Treatment history was obtained in a systematic fashion using standardized questions at the end of each diagnostic module regarding hospitalization, counseling, and use of medications. Finally, school dysfunction was examined by documenting repeated grades, placement in special classes, or need for tutoring or extra help.
Data analysis
Subjects were assigned to four groups according to their diagnostic status and referral status. The groups were first compared on demographic variables. While controlling for any demographic confounders, the groups were then compared on clinical features, comorbid diagnoses, and functional outcomes. Data are expressed as frequencies (percents) or means ± standard deviations. Logistic regression was used for binary outcomes (e.g., lifetime diagnoses), linear regression for continuous outcomes (e.g., GAF scores), ordinal logistic regression for ordinal outcomes (e.g., SES), and negative binomial regression for count variables (e.g., number of symptoms). Omnibus analyses reaching significance were followed by pair-wise comparisons. Fisher’s exact test was used in lieu of logistic regression when there were one or more zero frequencies in the two-way table defined by the categorical predictor and the dichotomous outcome. All tests were two-tailed, with statistical significance set at the 5% level (p < 0.05).
Results
Eighty-two youth with BPD from the pediatric bipolar family genetic study and 125 youth with OCD from the pediatric OCD family genetic study were included in the analyses. Subjects were stratified into four groups based on their primary ascertainment source and comorbidity status: (i) BPD without comorbid OCD (BPD; n = 65); (ii) OCD without comorbid BPD (OCD; n = 106); (iii) BPD with comorbid OCD (BPD+OCD; n = 17); and (iv) OCD with comorbid BPD (OCD+BPD; n = 19). Rates of BPD and OCD comorbidity in BPD and OCD cohorts were comparable (20.7% versus 15.2%; p = 0.30).
Table 1 shows demographic and clinical features of the four groups. Groups differed in mean age at evaluation and gender; mean age of subjects ascertained for OCD (OCD+BPD and OCD) was older than that of subjects ascertained for BPD (BPD+OCD and BPD). There were more males with BPD than OCD (p = 0.04). Subsequent analyses were therefore controlled for both age and gender.
Table 1.
Demographics and clinical features
| BPD cohort (N = 82) | OCD cohort (N = 125) | Test statistic | p-value | |||
|---|---|---|---|---|---|---|
| BPD | BPD+OCD | OCD | OCD+BPD | |||
| Demographics | ||||||
| Subjects | 65 (79.3) | 17 (20.7) | 106 (84.8) | 19 (15.2) | χ2(1) = 1.05 | 0.30 |
| Male | 48 (73.9)a* | 15 (88.2)c* | 62 (58.5) | 14 (73.7) | χ2(3) = 8.72 | 0.03 |
| Caucasian race | 60 (96.8) | 16 (100) | 97 (91.5) | 17 (94.4) | χ2(3) = 3.07 | 0.38 |
| Intact family | 21 (72.4) | 2 (66.7) | 58 (54.7) | 12 (66.7) | χ2(3) = 3.46 | 0.33 |
| Socioeconomic status | 1.8 ± 0.9 | 1.6 ± 0.8 | 1.7 ± 0.8 | 1.6 ± 0.6 | χ2(3) = 0.69 | 0.88 |
| Age at participation | 10.0 ± 3.8 | 10.5 ± 2.9 | 11.4 ± 3.2a** | 12.5 ± 3.0b**, d* | F(3,203) = 3.90 | 0.01 |
| Age at onset | ||||||
| OCD | – | 7.6 ± 3.4 | 7.7 ± 3.0 | 6.6 ± 3.3 | F(2,137) = 3.90 | 0.10 |
| BPD | 5.1 ± 3.6 | 6.4 ± 3.3 | – | 9.2 ± 3.9b** | F(3,96) = 5.58 | 0.005 |
| Duration of illness (years) | ||||||
| BPD | 3.6 ± 3.3b** | 2.9 ± 3.0 | – | 2.0 ± 2.5 | F(2,95) = 3.44 | 0.04 |
| OCD | – | 2.4 ± 2.7 | 4.2 ± 3.6 | 6.2 ± 3.6d*** | F(2,137) = 3.34 | 0.04 |
| Number of symptoms | ||||||
| Mania | 6.0 ± 1.1 | 6.2 ± 0.9 | – | 5.8 ± 1.1 | χ2(2) = 0.24 | 0.89 |
| OCD | – | 3.2 ± 1.6 | 4.4 ± 1.2 | 4.8 ± 0.7 | χ2(2) = 5.25 | 0.07 |
| Sequence of onset | ||||||
| OCD preceded BPD | – | 2 (11.8) | – | 14 (73.7) | Z = 3.07 | 0.002 |
| BPD preceded OCD | – | 9 (52.9) | – | 1 (5.3) | Z = −32.01 | < 0.001 |
| Simultaneous onset | – | 6 (35.3) | – | 4 (21.0) | Z = −0.45 | 0.65 |
| Current disorder(s) at ascertainment | ||||||
| Mania only | 50 (78.1) | 13 (76.5) | – | 9 (47.4) | χ2(2) = 4.03 | 0.13 |
| OCD only | – | 13 (76.5) | 98 (92.4) | 18 (94.7) | χ2(2) = 4.16 | 0.13 |
| Mania + OCD | – | 10 (58.8) | – | 8 (42.1) | Z = −0.46 | 0.64 |
| Chronic course (> 1 year) | ||||||
| BPD | 44 (68.8) | 11 (64.7) | – | 8 (42.1) | χ2(2) = 5.38 | 0.07 |
| OCD | – | 10 (58.8) | 78 (73.6) | 18 (94.7) | χ2(2) = 3.94 | 0.14 |
Values displayed as mean ± standard deviation or n (%). Statistical significance level set at p ≤ 0.05;
p ≤ 0.05;
p ≤ 0.01;
p ≤ 0.001.
BPD = bipolar disorder; OCD = obsessive-compulsive disorder; BPD+OCD = bipolar disorder with comorbid obsessive-compulsive disorder; OCD+BPD = obsessive-compulsive disorder with comorbid bipolar disorder.
BPD versus OCD.
BPD versus OCD+BPD.
OCD versus BPD+OCD.
BPD+OCD versus OCD+BPD.
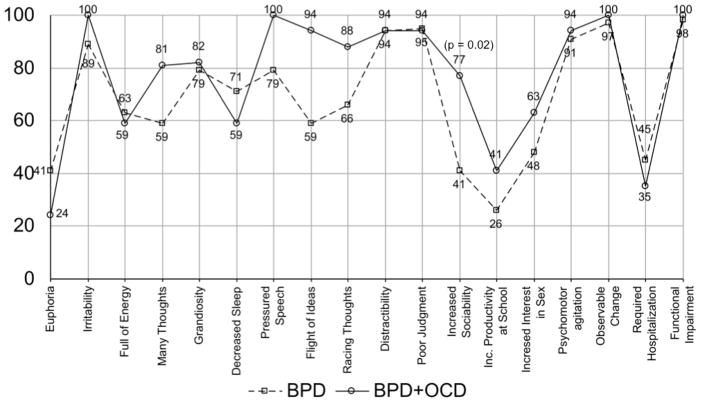
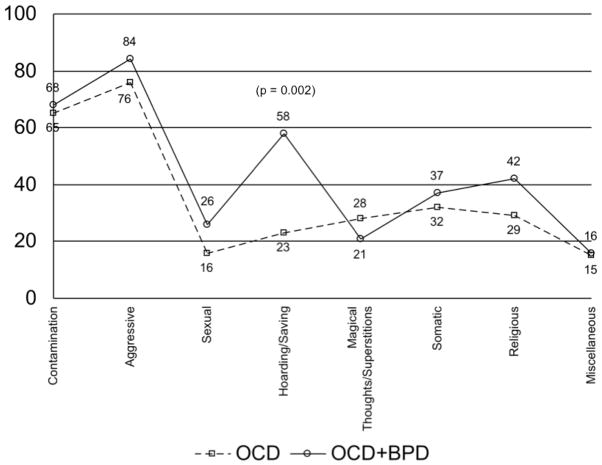
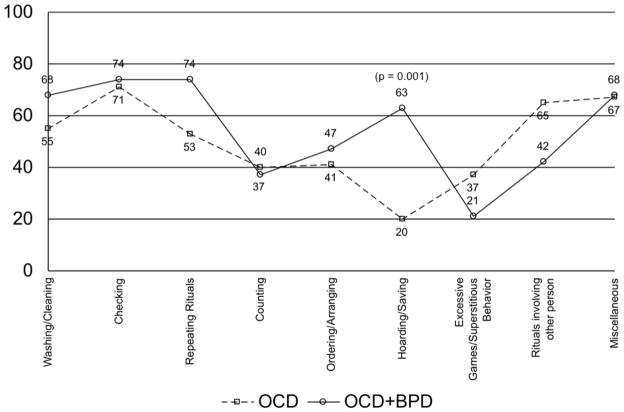
The onset of BPD usually preceded OCD in children ascertained for BPD (53% versus 5%; p < 0.001), while onset of OCD preceded BPD in children ascertained through the OCD study (74% versus 12%; p = 0.002). At ascertainment, 50% (18/36) of youth with comorbid OCD and BPD met full diagnostic criteria for both disorders in the past month, and another 11% (4/36) met full diagnostic criteria for one and subthreshold criteria for the other disorder in the past month. The number and frequency of mania symptoms in children with and without OCD were strikingly similar (Fig. 1; Table 1). The number and frequency of obsessive and compulsive symptoms did not differ between OCD with and without BPD comorbidity (Figs. 2 and 3; Table 1), except for the obsessive and compulsive symptom of ‘hoarding/saving’, observed at a higher frequency in the OCD+BPD group than in the OCD group. No differences were observed in other demographic variables, mood episode sequence, or mood episode polarity (Table 1).
Fig. 1.
Lifetime mania symptoms [Schedule for Affective Disorders and Schizophrenia for School-Age Children-Epidemiologic Version (K-SADS-E)]. BPD= bipolar disorder; BPD+OCD = bipolar disorder with comorbid obsessive-compulsive disorder.
Fig. 2.
Lifetime obsessive symptoms [Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS)]. OCD = obsessive-compulsive disorder; OCD+BPD = obsessive-compulsive disorder with comorbid bipolar disorder.
Fig. 3.
Lifetime compulsive symptoms [Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS)]. OCD = obsessive-compulsive disorder; OCD+BPD = obsessive-compulsive disorder with comorbid bipolar disorder.
As reflected in Table 2, a higher mean number of comorbid disorders, especially oppositional defiant disorder (ODD), major depressive disorder (MDD), and psychosis, were associated with BPD groups (BPD, BPD+OCD, and OCD+BPD) compared to the non-BPD group (OCD). Rates of multiple anxiety disorders (≥3) were significantly higher in both comorbid groups (BPD+OCD = 65%, OCD+BPD = 74%) compared to non-comorbid cohorts (BPD = 35%, OCD = 37%). Among various anxiety disorders, generalized anxiety disorder (GAD) occurred in greater frequency with the BPD+OCD comorbid group than the BPD non-comorbid group (77% versus 37%; p = 0.008) and social phobia (SP) co-occurred at a significantly higher frequency with OCD+BPD subjects than OCD subjects (47% versus 19%; p = 0.01).
Table 2.
Comorbidities
| BPD (n = 65) | BPD+OCD (n = 17) | OCD (n = 106) | OCD+BPD (n = 19) | Test statistic | p-value | |
|---|---|---|---|---|---|---|
| No. of comorbidities | 5.5 ± 2.3a*** | 6.5 ± 1.7d*** | 3.5 ± 2.1 | 5.9 ± 2.0e*** | χ2(3) = 58.05 | < 0.001 |
| ≥ 1 comorbidity (besides BPD/OCD) | 64 (98.5) | 17 (100) | 100 (94.3) | 19 (100) | FET | 0.45 |
| Multiple anxiety disorders (≥ 3) | 23 (35.4) | 11 (65)b*, d* | 39 (36.8) | 14 (74)c**, e** | χ2(3) = 13.01 | 0.005 |
| ADHD | 55 (84.6)a***, c* | 14 (82.4)d** | 43 (40.6) | 11 (57.9) | χ2(3) = 30.38 | < 0.001 |
| ODD | 59 (90.8)a*** | 15 (88.2)c*, d** | 46 (43.8) | 14 (73.7)e* | χ2(3) = 32.83 | < 0.001 |
| CD | 35 (53.9)a***, c*** | 9 (52.9)d***, f** | 7 (06.7) | 3 (15.8) | χ2(3) = 41.45 | < 0.001 |
| Tics/Tourette’s disorder | 16 (24.6) | 6 (35.3) | 35 (33.3) | 10 (52.6) | χ2(3) = 5.04 | 0.17 |
| Panic disorder | 6 (9.2) | 3 (17.7) | 16 (15.1) | 6 (31.6) | χ2(3) = 3.62 | 0.31 |
| Agoraphobia | 17 (26.2) | 3 (17.7) | 38 (35.9) | 8 (42.1) | χ2(3) = 3.72 | 0.29 |
| Specific phobia | 20 (30.8) | 9 (52.9) | 36 (34.0) | 9 (47.4) | χ2(3) = 5.75 | 0.12 |
| Separation anxiety disorder | 36 (55.4) | 10 (58.8) | 47 (44.3) | 11 (57.9) | χ2(3) = 2.70 | 0.44 |
| Avoidant disorder | 8 (12.3) | 5 (29.4) | 13 (12.3) | 5 (26.3) | χ2(3) = 5.22 | 0.16 |
| PTSD | 6 (9.4) | 0 (0) | 3 (2.8) | 1 (5.3) | FET | 0.21 |
| Social phobia | 18 (27.7) | 6 (35.3) | 20 (18.9) | 9 (47.4)e** | χ2(3) = 8.78 | 0.03 |
| GAD | 24 (36.9) | 13 (76.5)b**, d** | 48 (45.3) | 12 (66.7) | χ2(3) = 9.24 | 0.03 |
| MDD | 56 (86.2)a*** | 16 (94.1)d** | 47 (44.3) | 17 (89.5)e** | χ2(3) = 39.27 | < 0.001 |
| Psychosis | 19 (29.2)a*** | 8 (47.1)d*** | 11 (10.4) | 7 (36.8)e** | χ2(3) = 16.30 | 0.001 |
Values displayed as mean ± standard deviation or n (%). Statistical significance level set at p ≤ 0.05;
p ≤ 0.05;
p ≤ 0.01;
p ≤ 0.001.
BPD = bipolar disorder; OCD = obsessive-compulsive disorder; BPD+OCD = bipolar disorder with comorbid obsessive-compulsive disorder; OCD+BPD = obsessive-compulsive disorder with comorbid bipolar disorder; ADHD = attention-deficit hyperactivity disorder; ODD = oppositional defiant disorder; CD = conduct disorder; PTSD = posttraumatic stress disorder; GAD = generalized anxiety disorder; MDD = major depressive disorder; FET = Fisher’s Exact Test.
BPD versus OCD.
BPD versus BPD+OCD.
BPD versus OCD+BPD.
OCD versus BPD+OCD.
OCD versus OCD+BPD.
BPD+OCD versus OCD+BPD.
As shown in Table 3, all BPD groups (BPD, BPD+OCD, and OCD+BPD) were associated with significantly lower lifetime and current level of functioning on the GAF scale compared to the non-BPD group (OCD). Significantly higher rates of severe impairment of OCD were noted in subjects ascertained via an OCD diagnosis compared to those ascertained for BPD (68% versus 6%; p = 0.003). Compared to the non-BPD group (OCD), rates of psychiatric hospitalization were significantly higher in subjects ascertained for BPD (BPD and BPD+OCD groups).
Table 3.
Functioning and treatment history
| BPD (n = 65) | BPD+OCD (n = 17) | OCD (n = 106) | OCD+BPD (n = 19) | Test statistic | p-value | |
|---|---|---|---|---|---|---|
| GAF | ||||||
| Past | 39.8 ± 6.2a*** | 39.5 ± 5.2c*** | 48.7 ± 4.9 | 41.8 ± 7.4d*** | F(3,200) = 41.37 | < 0.001 |
| Present | 44.7 ± 6.3a*** | 44.8 ± 6.5c*** | 53.5 ± 5.0 | 47.3 ± 6.8d*** | F(3,200) = 32.66 | < 0.001 |
| Severe impairment (K-SADS-E) | ||||||
| BPD | 47 (72.3)b** | 10 (58.8) | 7 (36.8) | χ2(3) = 9.02 | 0.01 | |
| OCD | 1 (5.9) | 48 (45.3)c** | 13 (68.4)e** | χ2(3) = 9.30 | 0.01 | |
| Total | 47 (72.3)a*** | 11 (64.7) | 48 (45.3) | 11 (57.9) | χ2(3) = 13.82 | 0.003 |
| School functioning | ||||||
| Repeated grades | 7 (10.8) | 2 (11.8) | 9 (8.5) | 2 (10.5) | χ2(3) = 0.84 | 0.84 |
| Extra help | 35 (53.9) | 11 (64.7) | 61 (57.6) | 13 (68.4) | χ2(3) = 0.43 | 0.93 |
| Special class | 32 (49.2)a***, b** | 5 (29.4) | 14 (13.2) | 3 (15.8) | χ2(3) = 25.79 | < 0.001 |
| Treatment | ||||||
| No treatment | 0 (0) | 0 (0) | 6 (5.7) | 0 (0) | FET | 0.22 |
| Counseling only | 1 (1.5) | 1 (5.9) | 16 (15.1)a** | 1 (5.3) | χ2(3) = 10.32 | 0.02 |
| Medication only | 4 (6.2) | 0 (0) | 9 (8.5) | 0 (0) | FET | 0.51 |
| Counseling + medication | 34 (52.3) | 9 (52.9) | 64 (60.4) | 12 (63.2) | χ2(3) = 0.46 | 0.93 |
| Hospitalization | 26 (40.0)a*** | 7 (41.2)c** | 11 (10.4) | 6 (31.6)d* | χ2(3) = 21.69 | < 0.001 |
Values displayed as mean ± standard deviation or n (%). Statistical significance level set at p ≤ 0.05;
p ≤ 0.05;
p ≤ 0.01;
p ≤ 0.001.
BPD = bipolar disorder; OCD = obsessive-compulsive disorder; BPD+OCD = bipolar disorder with comorbid obsessive-compulsive disorder; OCD+BPD = obsessive-compulsive disorder with comorbid bipolar disorder; GAF = Global Assessment of Functioning Scale; K-SADS-E = Schedule for Affective Disorders and Schizophrenia for School-Age Children-Epidemiologic Version; FET = Fisher’s Exact Test.
BPD versus OCD.
BPD versus OCD+BPD.
OCD versus BPD+OCD.
OCD versus OCD+BPD.
BPD+OCD versus OCD+BPD.
In subjects with BPD and OCD, the disorder that emerged first was associated with worse impairment (p = 0.047; Table 4). When BPD emerged first, it was more impairing than OCD in 80% of cases (versus 19% when BPD did not emerge first). When OCD emerged first, it was more impairing than BPD in 31% of cases (versus 10% when OCD did not emerge first).
Table 4.
Sequence of age at onset versus level of impairment (K-SADS-E)
| BPD preceded OCD (n = 10) | Simultaneous onset (n = 10) | OCD preceded BPD (n = 16) | Test statistic | |
|---|---|---|---|---|
| Absolute impairment (severe) | ||||
| BPD | 7 (70) | 4 (40) | 6 (37.5) | χ2(2) = 3.64 |
| OCD | 1 (10) | 3 (30) | 10 (62.5) | χ2(2) = 4.74 |
| Relative impairment | χ2(4) = 9.66 | |||
| BPD worse than OCD | 8 (80) | 4 (40) | 1 (6.3) | |
| BPD and OCD equally severe | 1 (10) | 5 (50) | 10 (62.5) | |
| OCD worse than BPD | 1 (10) | 1 (10) | 5 (31.3) | |
Values displayed as n (%).
K-SADS-E = Schedule for Affective Disorders and Schizophrenia for School-Age Children-Epidemiologic Version; BPD = bipolar disorder; OCD = obsessive-compulsive disorder.
Discussion
Our systematic evaluation of structured interview-derived data from two large samples of consecutive clinically referred children and adolescents ascertained for BPD and for OCD show substantial and symmetrical overlap between BPD and OCD. Both OCD and BPD presented with clinical correlates typical of clinical populations reported in the literature. Barring few differences, examination of the clinical characteristics of OCD and BPD in youth reveals similar correlates irrespective of the reciprocal comorbidity or primary disorder of ascertainment. In the presence of BPD, youth with OCD experienced greater morbidity (poorer functioning and more frequent hospitalization), increased prevalence of other comorbid disorders, and frequent expression with obsessive and compulsive symptom of hoarding/saving. On the other hand, in the presence of OCD, youth with BPD more often experienced comorbidity with GAD. Comorbidity with multiple anxiety disorders was higher in youth with comorbid BPD and OCD than with either disorder without reciprocal comorbidity. Furthermore, in the comorbid state, the primary disorder of ascertainment was associated with earlier onset and greater impairment.
In our sample the overlap between BPD and OCD was bidirectional and symmetrical, with reciprocal comorbidity present in 21% of the youth with BPD and 15% of those diagnosed with OCD, suggesting that the observed comorbidity is not an effect of referral and/or ascertainment bias (29). This substantial overlap between BPD and OCD is consistent with an emerging body of literature documenting significant prevalence of comorbid OCD and BPD as high as 44% (8, 24) in BPD populations, similar to the comorbidity—as high as 45% (24)—reported in the OCD populations.
Clinical features of comorbid OCD and BPD
In this study, the age at onset of BPD and OCD did not vary by the presence of reciprocal comorbidity. Our results are consistent with the previous findings by Masi et al. (24, 26), who report no change in the age at onset of BPD, but are in contrast to their finding of earlier age at onset of OCD in the presence of BPD comorbidity.
More than half (61%) of the youth with the comorbidity were concurrently experiencing symptoms of both mania and OCD at ascertainment. This overlap of symptoms suggests that more often than not, when comorbid, the clinical presentation of BPD and OCD symptoms occurs concurrently. In general, symptom profile (number and frequency) of OCD and BPD in youth was strikingly homologous, with the sole exception of hoarding/saving obsessions and compulsions that were significantly more frequent in the presence of BPD comorbidity. Irrespective of the comorbidity with OCD, mania often presented with chronic course with predominant symptoms (> 90%) of irritable mood, psychomotor agitation, distractibility, and poor judgment (Fig. 1). OCD with and without BPD were similar in course and presented with predominant (> 65%) symptoms of aggressive and contamination obsessions and with compulsions of checking and washing/cleaning (Figs. 2 and 3). Our study failed to show difference based on comorbidity with BPD in the frequency of superstitious obsessions and ordering compulsions as reported in youth (24), or in the rates of sexual and religious obsessions or checking compulsions as documented in adult populations (17, 22).
Higher rates of obsessions and compulsion of hoarding/saving associated with BPD comorbidity is noteworthy, as a putative hoarding/saving subtype of OCD has been described with distinct clinical correlates, treatment outcome, neuroimaging and neurocognitive findings, and a link with a chromosomal region that differ from typical features of OCD (36). Our findings of significant association of hoarding/saving OCD with BPD comorbidity are replicated by a recent naturalistic study where high comorbidity with BPD was reported in OCD youth with the symptom of hoarding (26). Whether this observed association between the hoarding/saving subtype of OCD and BPD is suggestive of higher risk for BPD in youth with the hoarding/saving subtype of OCD needs to be further examined through familial risk analysis and prospective longitudinal risk analysis of BPD in this population.
Pattern of psychiatric comorbidity in youth with comorbid OCD and BPD
Barring few exceptions, the comorbidity profile of BPD and OCD was strikingly similar irrespective of the reciprocal comorbidity. Compared to OCD youth without comorbid BPD, significantly larger number of comorbidities, including ODD, MDD, and psychosis, were associated with BPD youth irrespective of ascertainment and comorbidity status with OCD (BPD, BPD+OCD, OCD+BPD); this suggests that in the presence of BPD, youth with OCD are at a higher risk for certain comorbidities that are characteristically associated with BPD.
Contrary to the expected greater association of other anxiety disorders with OCD rather than BPD (24), in this study rates of anxiety disorders are equally high in youth with either BPD or OCD. However, multiple anxiety disorders (≥3), especially GAD and SP, occur at a notably higher frequency in the comorbid presence of BPD and OCD than otherwise, suggesting that the lifetime risk of comorbid multiple anxiety disorders is significantly higher in youth with comorbid BPD and OCD than in youth with either disorder without reciprocal comorbidity.
Lack of meaningful association between OCD and BPD comorbidity with panic disorder and agoraphobia is discrepant with patterns of comorbidity observed in previous clinical (17, 37) and epidemiological (18, 38) studies in adults, where OCD comorbidity with BPD was associated with increased risk of lifetime comorbidity with panic disorder and agoraphobia, a finding which led Birmaher et al. (39) to suggest that the association between BPD and panic disorder in children and adolescents might be unique and specific. On the contrary, our findings are consistent with the recent emerging literature indicating high prevalence of various anxiety disorders—including but not limited to panic disorder—in pediatric (4, 8, 9) and adult (40–43) populations with BPD, challenging the specific link between BPD and panic disorder.
Level of functioning and treatment history in youth with comorbid OCD and BPD
Youth with BPD (with or without comorbid OCD) had significantly worse past and present level of global functioning and higher rate of hospitalization than OCD youth without comorbid BPD. Consistent with the findings reported by Masi and colleagues (24), it appears that in the presence of BPD comorbidity, youth with OCD also experience other correlates of poorer level of functioning and higher rate of hospitalizations that are characteristic of BPD.
In brief, our findings suggest that BPD and OCD in the comorbid state present with a clinical profile that is typical of these disorders, along with certain clinical features that emerge exclusively in the presence of comorbidity than otherwise. Higher prevalence of symptoms of hoarding/saving and multiple anxiety disorders, especially GAD and SP, are observed when OCD and BPD are comorbid than when either disorder occurs without reciprocal comorbidity. On the other hand, greater prevalence of comorbidities with ODD, MDD, and psychosis and higher level of morbidity (poorer functioning and more frequent hospitalization) recorded in the context of comorbidity with BPD in youth ascertained for OCD is reflective of the morbidity that is characteristically associated with BPD.
Clinical correlates of comorbid OCD and BPD in the context of ascertainment status
When comorbid presentation of BPD and OCD is compared based on the ascertainment status, youth with comorbid BPD and OCD, regardless of whether ascertained for BPD or OCD, share to a significant extent similar clinical correlates. Ascertainment status in the comorbid cases correlates strongly with the sequence of onset, duration, and severity of BPD and OCD. Onset of OCD precedes the onset of BPD at a higher rate in probands ascertained for OCD, and similarly, onset of BPD precedes the onset of OCD in probands ascertained for BPD. The association of primary disorder of ascertainment with worse severity—which is suggestive of referral bias—and longer duration is more evident with OCD (statistically significant) than BPD (numerically but not statistically significant).
To further understand this relationship between relative onset and severity of these disorders in the comorbid state, we examined the severity of BPD and OCD in the context of the sequence of onset of these disorders in the combined comorbid groups (Table 4). In youth with the onset of BPD earlier than OCD, the level of impairment of BPD was more often severe (70%) and worse than comorbid OCD (80%). On the other hand, earlier onset of OCD was more often associated with severe impairment (63%) and was equally impairing in severity as the comorbid BPD (63%). This suggests that when onset of BPD precedes OCD there is high probability of presentation of BPD to be severe and worse than comorbid OCD, and that when onset of OCD precedes BPD, the presentation of OCD is often severe and equally impairing as comorbid BPD, though this observed association may be related to the duration of illness. Besides the noted difference in sequence of onset, level of severity, and duration of illness, we did not observe any other clinically meaningful differences in the clinical characteristics of comorbid BPD and OCD in youth ascertained for either BPD or OCD.
Limitations
Our findings should be evaluated in the light of some methodological limitations. This is a secondary analysis of data collected for family genetic studies of BPD and OCD in children and adolescents. Children were primarily ascertained for BPD or OCD and comorbid diagnoses were established by structured diagnostic interview. The relatively small sample size of the subjects with comorbid BPD and OCD (n = 36) is an added limitation of this study. Generalizability of our results to the population at large is limited by selection biases. Since we studied children referred to child psychiatry services, our findings should generalize to similar clinics, but may not generalize to other psychiatric sampling frames or to community samples.
Conclusion
Despite these limitations, our findings indicate that bidirectional BPD and OCD comorbidity can be identified in a substantial minority of youth with OCD or BPD, and in the comorbid state symptoms of BPD and OCD often present concurrently. Consistent with our hypothesis, these results suggest that when comorbid, OCD and BPD present with clinical characteristics that are typical of the disorders, though there is an increased risk for comorbidities with multiple anxiety disorders, especially GAD and SP, and selective increase in frequency of obsession and compulsion of hoarding/saving when BPD and OCD are comorbid than otherwise. Furthermore, clinical characteristics of comorbid BPD and OCD remained substantially unaltered irrespective of whether youth were ascertained for BPD or OCD, though ascertainment status determined the sequence of presentation and severity of the disorders.
Whether hoarding/saving could emerge as a ‘symptom marker’ for BPD comorbidity in youth with OCD requires further investigation in larger populations. Although our findings require confirmation, they draw attention to the importance of carefully evaluating patients with BPD and OCD for reciprocal comorbidity, and in the presence of comorbidity, giving consideration to treatment interventions specific to each disorder. Considering the extreme severity of juvenile mania, its emergence in children with OCD seriously complicates their treatment, as anti-OCD agents have the risk of exacerbating mood symptoms and precipitating mania (44) and antimanic agents show marginal efficacy in treating OCD symptoms (45). Antidepressant induced (hypo)mania—suggestive of bipolar diathesis (44, 46)—has been reported in one-third of the OCD youth with comorbid BPD; this reported risk for pharmacologic (hypo)mania, although high, is not different than noted in BPD youth without OCD (24). Thus, previous literature along with our findings suggest that youth with OCD should be closely screened and monitored for the emergence of (hypo)mania, as the presence of BPD has serious implications for psychopharmacological management of both disorders. Future studies examining the patterns of familial aggregation of OCD and BPD, along with longitudinal studies addressing the impact of comorbidity on the clinical presentation, course, and response to treatment, would assist in further defining this comorbid condition.
Acknowledgments
This work has been funded in part by the Dupont Warren Fellowship Award, the Norma Fine Pediatric Psychopharmacology Fellowship Fund, and the Pediatric Psychopharmacology Council Fund, as well as NIMH K08 MH01481 (DG) and NIMH K08 MH01503-05 (JW).
Footnotes
Disclosures
GJ has received research support from Bristol-Myers Squibb as the site principal investigator on a multi-centered trial; has received support from the Ethel DuPont Warren Fellowship (2005–2006) and a Pilot Research Award from the American Academy of Child and Adolescent Psychiatry (2005); has received CME sponsored support from McNeil Pediatrics; and is a co-investigator for clinical trials sponsored by Shire, Johnson & Johnson, Pfizer, Merck, Cephalon, McNeil, Eli Lilly & Co., Abbott, Novartis, Bristol-Meyers Squibb, Organon, Otsuka, Takeda, and New River Pharmaceuticals. JW receives royalties as author of Is Your Child Bipolar?, published by Bantam Books; her spouse receives research support from Boehringer-Ingelheim, GlaxoSmithKline, UCB (Schwarz) Pharma, and Sepracor; has served as a speaker for Boehringer-Ingelheim, GlaxoSmithKline, Sanofi-aventis, Sepracor, and Takeda; and has served on the advisory boards for Axon Labs, Boehringer-Ingelheim, GlaxoSmithKline, Jazz Pharmaceuticals, Novarts, Neurogen, Pfizer, UCB (Schwarz) Pharma, and Takeda. JB currently receives research support from Alza, AstraZeneca, Bristol-Myers Squibb, Eli Lilly & Co., Janssen, McNeil, Merck, Organon, Otsuka, Shire, NIMH, and NICHD; and in previous years received research support, consultation fees, or speakers fees from Abbott, AstraZeneca, Celltech, Cephalon, Eli Lilly & Co., Esai, Forest, GlaxoSmithKline, Gliatech, Janssen, McNeil, NARSAD, NIDA, New River, Novartis, Noven, Neurosearch, Pfizer, Pharmacia, The Prechter Foundation, Shire, The Stanley Foundation, UCB Pharma, Inc., and Wyeth. DG has received research support from Eli Lilly & Co., Forest, GlaxoSmithKline, The Obsessive Compulsive Foundation, Tourette Syndrome Association, Wallace Foundation, McIngvale Family Foundation and NIH; has received speaker honoraria from Alza, Bristol-Myers Squibb, Eli Lilly & Co., Forest, GlaxoSmithKline, Novartis, Pfizer, Shire, and Wyeth; and has had advisory or consulting relationships with Eli Lilly & Co., Solvay, Lundbeck and GlaxoSmithKline. CP, FV, and DY have no conflicts of interest to report.
References
- 1.McClellan J, Kowatch R, Findling RL Workgroup on Quality Issues. Practice Parameter for the Assessment and Treatment of Children and Adolescents with Bipolar Disorder. J Am Acad Child and Adolesc Psychiatry. 2007;46:107–125. doi: 10.1097/01.chi.0000242240.69678.c4. [DOI] [PubMed] [Google Scholar]
- 2.Douglass HM, Moffitt TE, Dar R, McGee R, Silva P. Obsessive-compulsive disorder in a birth cohort of 18-year-olds: Prevalence and predictors. J Am Acad Child Adolesc Psychiatry. 1995;34:1424–1431. doi: 10.1097/00004583-199511000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Flament MF, Whitaker A, Rapaport JL, et al. Obsessive compulsive disorder in adolescence: An epidemiological study. J Am Acad Child Adolesc Psychiatry. 1988;27:764–771. doi: 10.1097/00004583-198811000-00018. [DOI] [PubMed] [Google Scholar]
- 4.Harpold T, Wozniak J, Kwon A, et al. Examining the association between pediatric bipolar disorder and anxiety disorders in psychiatrically referred children and adolescents. J Affect Disord. 2005;88:19–26. doi: 10.1016/j.jad.2005.05.016. [DOI] [PubMed] [Google Scholar]
- 5.Faedda GL, Baldessarini RJ, Glovinsky IP, Austin NB. Pediatric bipolar disorder: Phenomenology and course of illness. Bipolar Disord. 2004;6:305–313. doi: 10.1111/j.1399-5618.2004.00128.x. [DOI] [PubMed] [Google Scholar]
- 6.Tillman R, Geller B, Bolhofner K, Craney JL, Williams M, Zimerman B. Ages of onset and rates of syndromal and subsyndromal comorbid DSM-IV diagnoses in a prepubertal and early adolescent bipolar disorder phenotype. J Am Acad Child Adolesc Psychiatry. 2003;42:1486–1493. doi: 10.1097/00004583-200312000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Wozniak J, Biederman J, Monuteaux MC, Richards J, Faraone SV. Parsing the comorbidity between bipolar disorder and anxiety disorders: A familial risk analysis. J Child Adolesc Psychopharmacol. 2002;122:101–111. doi: 10.1089/104454602760219144. [DOI] [PubMed] [Google Scholar]
- 8.Masi G, Toni C, Perugi G, Mucci M, Millepiedi S, Akiskal HS. Anxiety disorders in children and adolescents with bipolar disorder: A neglected comorbidity. Can J Psychiatry. 2001;46:797–802. doi: 10.1177/070674370104600902. [DOI] [PubMed] [Google Scholar]
- 9.Johnson JG, Cohen P, Brook JS. Associations between bipolar disorder and other psychiatric disorders during adolescence and early adulthood: A community-based longitudinal investigation. Am J Psychiatry. 2000;157:1679–1681. doi: 10.1176/appi.ajp.157.10.1679. [DOI] [PubMed] [Google Scholar]
- 10.Biederman J, Faraone SV, Hatch M, Mennin D, Taylor A, George P. Conduct disorder with and without mania in a referred sample of ADHD children. J Affect Disord. 1997;44:177–188. doi: 10.1016/s0165-0327(97)00043-8. [DOI] [PubMed] [Google Scholar]
- 11.Faraone SV, Biederman J, Wozniak J, Mundy E, Mennin D, O’Donnell D. Is comorbidity with ADHD a marker for juvenile onset mania? J Am Acad Child Adolesc Psychiatry. 1997;36:1046–1055. doi: 10.1097/00004583-199708000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Morel BA. Traite de Maladies Mentales. Paris: Libairie Victor Masson; 1860. [Google Scholar]
- 13.Winokur G, Clayton PG, Reich T. Manic Depressive Illness. St. Louis: C. V. Mosby; 1969. [Google Scholar]
- 14.Goodwin F, Jamison K. Manic-Depressive Illness. New York: Oxford University Press; 1990. [Google Scholar]
- 15.Jenike MA, Rasmussen SA. Recent advances in bipolar disorder and obsessive compulsive disorder. J Clin Psychiatry Suppl. 1990;6:123–124. [Google Scholar]
- 16.Robins L, Price RK. Adult disorders predicted by childhood conduct problems: Results from the NIMH epidemiologic catchment area project. Psychiatry. 1991;54:116–132. doi: 10.1080/00332747.1991.11024540. [DOI] [PubMed] [Google Scholar]
- 17.Perugi G, Akiskal HS, Pfanner C, et al. The clinical impact of bipolar and unipolar affective comorbidity on obsessive-compulsive disorder. J Affect Disord. 1997;461:15–23. doi: 10.1016/s0165-0327(97)00075-x. [DOI] [PubMed] [Google Scholar]
- 18.Chen YW, Dilsaver SC. Comorbidity for obsessive-compulsive disorder in bipolar and unipolar disorders. Psychiatry Res. 1995;59:57–64. doi: 10.1016/0165-1781(95)02752-1. [DOI] [PubMed] [Google Scholar]
- 19.Krüger S, Cooke RG, Hasey GM, Jorna T, Persad E. Comorbidity of obsessive compulsive disorder in bipolar disorder. J Affect Disord. 1995;34:117–120. doi: 10.1016/0165-0327(95)00008-b. [DOI] [PubMed] [Google Scholar]
- 20.Tükel R, Meteris H, Koyuncu A, Tecer A, Yazici O. The clinical impact of mood disorder comorbidity on obsessive-compulsive disorder. Eur Arch Psychiatry Clin Neurosci. 2006;256:240–245. doi: 10.1007/s00406-006-0632-z. [DOI] [PubMed] [Google Scholar]
- 21.Hantouche EG, Angst J, Demonfaucon C, Perugi G, Lancrenon S, Akiskal HS. Cyclothymic OCD: A distinct form? J Affect Disord. 2003;75:1–10. doi: 10.1016/s0165-0327(02)00461-5. [DOI] [PubMed] [Google Scholar]
- 22.Perugi G, Toni C, Frare F, Travierso MC, Hantouche E, Akiskal HS. Obsessive-compulsive-bipolar comorbidity: A systematic exploration of clinical features and treatment outcome. J Clin Psychiatry. 2002;63:1129–1134. [PubMed] [Google Scholar]
- 23.Zutshi A, Kamath P, Reddy YC. Bipolar and nonbipolar obsessive-compulsive disorder: A clinical exploration. Compr Psychiatry. 2007;48:245–251. doi: 10.1016/j.comppsych.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 24.Masi G, Perugi G, Toni C, et al. Obsessive-compulsive bipolar comorbidity: Focus on children and adolescents. Dutch J Affect Disord. 2004;78:175–183. doi: 10.1016/S0165-0327(03)00107-1. [DOI] [PubMed] [Google Scholar]
- 25.Geller DA, Biederman J, Griffin S, Jones J, Lefkowitz TR. Comorbidity of juvenile obsessive-compulsive disorder with disruptive behavior disorders: A review and a report. J Am Acad Child Adolesc Psychiatry. 1996;35:1637–1646. doi: 10.1097/00004583-199612000-00016. [DOI] [PubMed] [Google Scholar]
- 26.Masi G, Perugi G, Millepiedi S, et al. Bipolar co-morbitity in pediatric obsessive-compulsive disorder: Clinical and treatment implications. J Child Adolesc Psychopharmacol. 2007;17:475–486. doi: 10.1089/cap.2006.0107. [DOI] [PubMed] [Google Scholar]
- 27.Diagnostic and Statistical Manual of Mental Disorders: Fourth Edition Text Revision (DSM-IV-TR) 4. Washington, D.C: American Psychiatric Association; 2000. [Google Scholar]
- 28.McConaughy SH, Achenbach TM. Comorbidity of empirically based syndromes in matched general population and clinical samples. J Child Psychol Psychiatry. 1994;35:1141–1157. doi: 10.1111/j.1469-7610.1994.tb01814.x. [DOI] [PubMed] [Google Scholar]
- 29.Angold A, Costello EJ, Erkanli A. Comorbidity. J Child Psychol Psychiatry. 1999;40:57–87. [PubMed] [Google Scholar]
- 30.Geller D, Petty C, Vivas F, Johnson J, Pauls D, Biederman J. Further evidence for co-segregation between pediatric obsessive compulsive disorder and attention deficit hyperactivity disorder: A familial risk analysis. Biol Psychiatry. 2007;61:1388–1394. doi: 10.1016/j.biopsych.2006.09.026. [DOI] [PubMed] [Google Scholar]
- 31.Wozniak J, Faraone SV, Mick E, Monuteaux M, Coville A, Biederman J. A controlled family study of children with DSM-IV bipolar-I disorder and psychiatric co-morbidity. Psychol Med. 2009;6:1–10. doi: 10.1017/S0033291709991437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Orvaschel H. Schedule for Affective Disorder and Schizophrenia for School-Age Children Epidemiologic Version. 5. Ft. Lauderdale: Nova Southeastern University, Center for Psychological Studies; 1994. [Google Scholar]
- 33.Goodman WK, Price LH, Rasmussen SA, et al. The Yale-Brown Obsessive Compulsive Scale: I. Development, use, and reliability. Arch Gen Psychiatry. 1989;46:1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- 34.Endicott J, Spitzer RL, Fleiss JL, Cohen J. The global assessment scale. A procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry. 1976;33:766–771. doi: 10.1001/archpsyc.1976.01770060086012. [DOI] [PubMed] [Google Scholar]
- 35.Hollingshead AB. Four Factor Index of Social Status. New Haven, CT: Yale Press; 1975. [Google Scholar]
- 36.Saxena S. Is compulsive hoarding a genetically and neurobiologically discrete syndrome? Implications for diagnostic classification. Am J Psychiatry. 2007;164:380–384. doi: 10.1176/ajp.2007.164.3.380. [DOI] [PubMed] [Google Scholar]
- 37.Perugi G, Akiskal HS, Rossi L, et al. Chronic mania. Family history, prior course, clinical picture and social consequences. Br J Psychiatry. 1998;173:514–518. doi: 10.1192/bjp.173.6.514. [DOI] [PubMed] [Google Scholar]
- 38.Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychol Med. 1997;27:1101–1119. doi: 10.1017/s0033291797005588. [DOI] [PubMed] [Google Scholar]
- 39.Birmaher B, Kennah A, Brent D, Ehmann M, Bridge J, Axelson D. Is bipolar disorder specifically associated with panic disorder in youths? J Clin Psychiatry. 2002;63:414–419. doi: 10.4088/jcp.v63n0507. [DOI] [PubMed] [Google Scholar]
- 40.Freeman MP, Freeman SA, McElroy SL. The comorbidity of bipolar and anxiety disorders: Prevalence, psychobiology, and treatment issues. J Affect Disord. 2002;68:1–23. doi: 10.1016/s0165-0327(00)00299-8. [DOI] [PubMed] [Google Scholar]
- 41.McElroy SL, Altshuler LL, Suppes T, et al. Axis I psychiatric comorbidity and its relationship to historical illness variables in 288 patients with bipolar disorder. Am J Psychiatry. 2001;158:420–426. doi: 10.1176/appi.ajp.158.3.420. [DOI] [PubMed] [Google Scholar]
- 42.Kessler RC, Stang P, Wittchen HU, Stein M, Walters EE. Lifetime co-morbidities between social phobia and mood disorders in the US National Comorbidity Survey. Psychol Med. 1999;29:555–567. doi: 10.1017/s0033291799008375. [DOI] [PubMed] [Google Scholar]
- 43.Cassano GB, Pini S, Saettoni M, Dell’Osso L. Multiple anxiety disorder comorbidity in patients with mood spectrum disorders with psychotic features. Am J Psychiatry. 1999;156:474–476. doi: 10.1176/ajp.156.3.474. [DOI] [PubMed] [Google Scholar]
- 44.Diler RS, Avci A. SSRI-induced mania in obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry. 1999;38:6–7. doi: 10.1097/00004583-199901000-00010. [DOI] [PubMed] [Google Scholar]
- 45.Connor KM, Payne VM, Gadde KM, Zhang W, Davidson JR. The use of aripiprazole in obsessive-compulsive disorder: Preliminary observations in 8 patients. J Clin Psychiatry. 2005;66:49–51. doi: 10.4088/jcp.v66n0107. [DOI] [PubMed] [Google Scholar]
- 46.Klein D, Depue R, Slater J. Cyclothymia in the adolescent offspring of parents with bipolar affective disorder. J Abnorm Psychol. 1985;94:115–127. doi: 10.1037//0021-843x.94.2.115. [DOI] [PubMed] [Google Scholar]