Abstract
The motor car is a ubiquitous feature of modern life, and most of us spend significant amounts of time in a car, behind the wheel. Driving a vehicle requires complex coordination of cognitive, motor, and sensory skills. All of these aspects can be affected adversely by diabetes per se, with hypoglycemia being the main concern for people with diabetes who drive. Here we introduce the concept of using the motor vehicle as a device to collect and deliver physiological and clinical information, which, in turn, may enable more people to drive more safely by reducing the chances of medical mishaps behind the wheel. This is particularly relevant for people living with diabetes who are at risk from a number of medical conditions that have the potential to have an impact on safe driving. The development of in-vehicle medical monitoring presents a new opportunity for novel collaborations between two industries, which have safety as a core value.
Keywords: diabetes, hypoglycemia, in-vehicle medical monitoring, driving, driving mishaps, obstructive sleep apnea
Background
The internal combustion engine is a ubiquitous feature of modern life. Estimates suggest that there are in excess of 800 million four-wheeled vehicles in use worldwide with the number expected to double by 2050. Moreover, there appears to be a strong link among economic growth, quality of life, and the use of motorized vehicles.1 In the United States, the nationwide average drive time approximates to 24 minutes, with Americans spending more than 100 hours a year commuting to work.2 In the United Kingdom, the time spent traveling by car averages 383 hours per person per year, or around 38 minutes a day.3
Driving a motor vehicle safely requires coordination of a highly complex set of physiological, anatomical, and behavioral systems. It is generally recognized that the human factor, as opposed to vehicle and environmental factors, is the predominant contributor in approximately 95% of motor vehicle collisions.4 People who drive for a living are more likely to be involved in accidents compared to the background population. The reasons for this are complex but appear to be related to time pressure exposure, work schedule fatigue, larger engine size, reduced personal costs of accidents, and psychological traits including aggression or extraversion.5
Much less common causes of road traffic accidents are medical conditions (Table 1), although a number of drivers with chronic medical conditions may give up using their motor vehicles because of a perceived risk to them while at the wheel.6,7
Table 1.
Medical Conditions Associated with Road Traffic Accidents
| Epilepsy | 38% |
| Insulin treatment | 18% |
| Myocardial infarction | 8% |
| Stroke | 8% |
| Other | 21% |
Diabetes and Driving
In the United States, many states restrict licenses for people with diabetes (see www.diabetes.org/advocacy-and-legalresources/discrimination/drivers/pvt-licensemap.jsp). In 1971, the U.S. Supreme Court held that driving is an “important interest” that may not be taken away from a licensed driver without a government agency providing procedural due process. In 1993, a court of appeals in California noted that a person with insulin-treated diabetes is not automatically subject to license forfeiture or nonrenewal unless diabetes affects the driver's safe operation of a motor vehicle. Californian doctors are, however, required to inform authorities about sudden loss of consciousness due to hypoglycemia.8 In contrast, the state of New York has no specific policies about licensing of drivers with diabetes other than if loss of consciousness occurs while driving.
In the United Kingdom, the Road Traffic Act 1988 defines diabetes as a prospective disability, i.e., one that is not relevant at the moment but may, at some time in the future, affect safe driving. Although it is the duty of the patient to inform the national Driver Vehicle Licensing Authority (DVLA) and their vehicle insurer, it is the duty of the doctor to ensure that the patient knows this.9 British patients with diabetes requiring insulin treatment are usually issued with a licence for 1–3 years and must demonstrate satisfactory control, recognize warning symptoms of hypoglycemia, and meet the required visual standards. The assessment of who is at risk of hypoglycemia is left at the discretion of the clinician. Depending on the type of driving license a person holds, certain restrictions may be applied, and patients are often given conditional licenses, which are subject to regular reviews.
Diabetes may impact on an individual's ability to drive safely by a number of mechanisms (Table 2).
Table 2.
Potential Cause of Driving Impairment Associated with Diabetes
| Acute hypoglycemia |
| Hypoglycemia unawareness |
| Retinopathy causing visual impairment |
| Neuropathy and foot problems affecting ability to use the pedals |
| Ischemic heart disease |
| Cerebrovascular disease |
| Obesity associated with somnolence and sleep disorders |
| Iatrogenic, e.g., use of antidepressant or pain-relieving medication |
| Comorbid conditions, e.g., cognitive dysfunction |
Strict driving restrictions are also in place for the issuance of vocational driving licenses to people with diabetes treated with insulin. In the United States, insulin-treated individuals are automatically denied an interstate commercial driving license in most states, although temporary waivers have been granted in the last decade. In the United States, estimates suggest an additional 42 accidents/year as a result of mild and moderate hypoglycemia in people with insulin-treated diabetes if allowed to drive commercial vehicles, with a 20-fold increase in risk if there is a history of severe hypoglycemia.10 In a large telephone survey involving >1000 commercial drivers identified from databases of the Quebec Automobile Insurance Society, a significant increase in the number of road traffic accidents involving drivers with diabetes was reported.11 This increase was not seen with larger articulated trucks. A follow-up analysis by the same researchers on the same cohort showed that this increased risk was only in drivers with a license for single (unarticulated) trucks not treated with insulin and without diabetic complications.12 In the United Kingdom, a clinical need for insulin excludes diabetic individuals from driving trucks, heavy good vehicles, and buses except under exceptional circumstances.9
It is also recognized that driving as an occupation can be physically hazardous, which may be relevant for people with diabetes. Previous studies have shown high rates of absenteeism, illness, and death among urban bus drivers. In particular, there is a significantly increased risk from premature cardiovascular diseases and hypertension among bus drivers.13
Hypoglycemia and Driving
Driving is a complex skill requiring good visuospatial function, rapid information processing, vigilance, and satisfactory judgment. Hypoglycemia results in cognitive impairment and psychomotor retardation, which can lead to functional impairment affecting driving performance.14 Furthermore, driving per se imparts a metabolic demand on the brain that can provoke hypoglycemia under certain circumstances.15 The potential of individuals with diabetes to develop hypoglycemia during insulin treatment presents a possible risk to them and others in certain safety-critical tasks, such as driving. Restrictions for insulin-treated drivers may limit this risk, but the evidence upon which such restrictions are based is limited.
Although some studies have demonstrated that insulin-treated patients as a group do not pose an increased risk to road safety,16,17 this view is not supported by all studies.18 The criticism of studies that have failed to show an increase risk/incidence of road traffic accidents in people with insulin-treated diabetes is that there might have been underreporting of accidents because of fear of losing their licenses; also, the retrospective nature of some of the studies allows for recall biases. In addition, such studies have been limited to selective groups of the population. It, however, remains contentious if there is an increased risk of accidents among insulin-treated individuals.
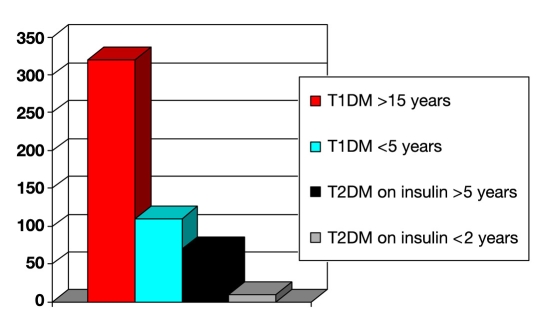
The frequency and type of hypoglycemia in different groups of individuals with diabetes were examined prospectively using self-reported questionnaires and continuous glucose monitoring (Figure 1). In that study there appeared to be no significant differences in rates of low interstitial glucose (LIG) or rates of self-reported mild and severe hypoglycemia in those with type 2 diabetes treated with sulfonylureas compared to patients with type 2 diabetes started on insulin over the previous 2 years.19 In contrast, episodes of hypoglycemia and LIG in those with type 1 diabetes of short duration were generally much more frequent (around 10-fold higher) than in those with type 2 diabetes recently started on insulin.
Figure 1.
Frequency of hypoglycemia (per 100 patient years) related to type and duration of diabetes. T1DM, type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus.
Symptom perception as an estimation of the blood glucose level can be unreliable.20 Furthermore, while driving at normal blood glucose levels, adrenomedullary catecholamine levels can be increased, leading to enhanced autonomic arousal and a false hypoglycemia alert.15
Worryingly, data from driving simulator studies also suggest that patients with type 1 diabetes with impaired hypoglycemia awareness and patients with type 2 diabetes and normal hypoglycemia awareness can make decisions to continue to drive despite biochemical hypoglycemia and the perception that glucose levels have fallen.21
In the United Kingdom, the DVLA recommends that insulin-treated drivers should carry fast-acting carbohydrate and their blood glucose meter with them. These drivers are advised not to consider driving if the finger stick glucose level is <4 mmol/liter and that they should always test before driving.22 If a hypoglycemic event occurs, they are advised to wait at least 45 minutes after recovery before considering driving. However, questionnaire surveys have indicated that this advice is not widely known, adhered to, and not agreed with by drivers with diabetes.23
Doctors and diabetes specialist nurses also often give conflicting and inconsistent advice to patients about driving and diabetes.24 Compared to individuals with no history of accident involvement, drivers who have had driving mishaps are those less likely to test their blood glucose level before driving and also those who allow their blood glucose level to decline to a low level before deciding not to drive.25 Giving insulin by subcutaneous injection as compared to continuous subcutaneous insulin infusion is also more common among individuals who have been involved in accidents.
Obstructive Sleep Apnea (OSA)
There appears to be a strong association between OSA and type 2 diabetes, which is not invariably a consequence of obesity.26 In the United States, over 40,000 crash-related injuries and 1500 deaths are attributed annually to sleepy driving.27 Although the majority of these would probably occur in otherwise healthy drivers, drivers with preexisting sleep disorders are likely to account for a significant proportion. In a recent meta-analysis, the average crash risk ratio in drivers with OSA was increased almost threefold compared to the background population.28
People with OSA also have impaired vigilance and may, consequently, experience sleepiness-related cognitive impairment, which would potentially further increase the chance of a traffic accident occurring.
In-Vehicle Medical Monitoring
As mentioned earlier, in addition to the threat from unheralded hypoglycemia, diabetic individuals may also be at risk from other medical conditions that can impair driving performance, including visual and lower limb problems, as well as occlusive coronary and cerebrovascular disease. It is also relevant that the reduction of risk of diabetes-related complications is very focused on lowering blood pressure as well as glycemic control.
With these observations in mind, it may be worthwhile to consider developing the concept of in-vehicle medical monitoring. This would involve transforming the motor vehicle into a mobile physiological monitoring system to enhance driver safety. The concept would be to collect measurable physiological data and integrate these into the driving systems. Data could be used to enhance safe driving and also provide clinicians with important clinical data on which to base therapy decisions. Potential areas of clinical usefulness relevant to diabetic individuals who drive might include:
Real-time continuous interstitial glucose monitoring
Real-time blood pressure monitoring
Heart rate and rhythm monitoring
In-vehicle circulating oxygen levels. This may be relevant for individuals with hypoventilatory conditions associated with obesity
Breath alcohol levels
The method of data transmission could be wirelessly via infrared, radio frequency, or Bluetooth, with data displayed as part of the dashboard or satellite navigation system. With further embodiments, automobile electronics may have default maximum and minimum thresholds added to prevent ignition if certain clinical characteristics are not met. The vehicle dashboard could also display early warning signals, sound alarms, or produce tactile alerts to highlight to drivers changes in physiological variables. Certain measurements may also allow the technology to predict future changes to enhance driver safety by warning individuals to stop driving safely in advance of physiological deterioration.
The destination of data obtained from within the motor vehicle may be stored for use by the driver or at a later date by health care professionals for clinical management or could be transferred immediately via technologies such as On-Star systems to a third party distant from the vehicle. The technology could be either placed independently of the workings of the vehicle or become an integral part of the normal workings, i.e., certain criteria would need to be met, e.g., a glucose level >4 mmol/liter or alcohol levels within legal limits for driving before the engine can be started. Subsequently, if interstitial glucose levels start to fall, alarm systems can activate along with a satellite navigation system to advise drivers about safe places to exit highways to allow correction of low glucose levels (Figure 2).
Figure 2.
Prototype display for in-car interstitial glucose monitoring from Medtronic.
Incorporation of in-vehicle medical monitoring systems could also provide important information for clinicians:
Multiple measurements of blood pressure from sensors within the steering wheel to assess the efficacy of hypotensive therapies
Multiple measurements of heart rate and rhythm and ST segment monitoring for patients with ischemic heart disease
Thus it may be possible for drivers with chronic medical conditions and their relatives and carers to “feel safer” at the wheel by using these devices. Additionally, as this concept has the potential to improve driver safety, there may be positive implications for driver licensing and insurance and perhaps to open up new areas for employment previously not applicable for people with diabetes.
Plans are already underway to create online health records through a collaboration of major search engines and software manufacturers. The plan is for data to be uploaded from an individual's home or elsewhere and for this to be available to health care professionals or relatives.29 However, the technology used for in-vehicle medical monitoring may also be subject to misuse. Mobile telephone companies are already experimenting with the incorporation of biosensors into handsets to monitor various physiological parameters. The concern is that data may remain accessible despite attempts to erase it, thus leaving individuals vulnerable to “phishing.” Although the most likely target is to obtain commercial and personal financial information illegally, the methods used could allow unscrupulous individuals to access personal medical information.30
The concept of in-vehicle medical monitoring is likely to be of value for specific populations, e.g., drivers with diabetes. However, as mentioned earlier, most road traffic accidents are caused by human factors unrelated to medical conditions. Physiological monitoring systems incorporated into vehicle mechanics could be used to impact on alcohol and drug use as contributory factors and may even be considered mandatory for individuals falling foul of the law to allow them to return to driving. Linking alcohol detectors to ignition systems (ignition interlock devices) is already occurring and used by courts of law to enforce antidrink driving legislation.31
In summary, it is a fact of modern life that many individuals spend significant portions of their waking hours inside a motor vehicle. Driving remains a potentially hazardous pastime, although most accidents occur as a consequence of human factors rather than directly as a result of medical events. Technologies associated with physiological monitoring continue to develop at a rapid pace. Perhaps the time has come to collaborate directly with the motor industry to provide opportunities for improving driver safety further and also deliver potentially useful information for clinical decision making.
Abbreviations
- DVLA
Driver Vehicle Licensing Authority
- LIG
low interstitial glucose
- OSA
obstructive sleep apnea
References
- 1.Gott P. Is mobility as we know it sustainable? Available from: http://www.ihsglobalinsight.com/gcpath/AutoSustainabilityWhitePaper.pdf.
- 2.Longley R. Americans now spend over 100 hours a year commuting. Available from: http://usgovinfo.about.com/od/censusandstatistics/acommutetimes.htm.
- 3.UK Department of Transport. Transport trends 2008. Available from: http://www.dft.gov.uk/pgr/statistics/datatablespublications/trends/current/transporttrends2008.
- 4.UK Department of Transport. A safer way: consultation on making Britain's roads the safest in the world. Available from: http://www.dft.gov.uk/consultations/closed/roadsafetyconsultation/roadsafetyconsultation.pdf.
- 5.Clarke D, Ward P, Bartle C, Truman W. Road Safety Research report No. 58. An in-depth study of work-related road traffic accidents. Available from: http://www.dft.gov.uk/pgr/roadsafety/research/rsrr/theme5/anindepthstudyofworkrelated.pdf.
- 6.Taylor J. Diabetes and driving ordinary motor vehicles. Pract Diabetes. 1985;2:35–37. [Google Scholar]
- 7.Stork A, van Haeften T, Veneman T. Diabetes and driving: desired data, research methods and their pitfalls, current knowledge, and future research. Diabetes Care. 2006;29(8):1942–1949. doi: 10.2337/dc05-2232. [DOI] [PubMed] [Google Scholar]
- 8.Halpern K. Diabetes and driving responsibilities. Available from: http://www.diabeteshealth.com/read/1999/10/01/1645/diabetes-and-driving-responsibilities/
- 9.Drivers Medical Group. Driving and Vehicle Licensing Agency. At a glance guide to the current medical standards of fitness to drive [cited 2009 Sep]. Available from: http://www.dft.gov.uk/dvla/medical/ataglance.aspx.
- 10.Songer TJ, Lave LB, LaPorte RE. The risk of licensing persons with diabetes to drive trucks. Risk Anal. 1993;13(3):319–326. doi: 10.1111/j.1539-6924.1993.tb01083.x. [DOI] [PubMed] [Google Scholar]
- 11.Dionne G, Desjardins D, Laberge-Nadeau C, Maag U. Medical conditions, risk exposure, and truck drivers' accidents: an analysis with count data regression models. Accid Anal Prev. 1995;27(3):295–305. doi: 10.1016/0001-4575(94)00071-s. [DOI] [PubMed] [Google Scholar]
- 12.Laberge-Nadeau C, Dionne G, Maag U, Desjardins D, Vanasse C, Ekoe JM. Medical conditions and the severity of commercial motor vehicle drivers' road accidents. Accid Anal Prev. 1996;28(1):43–51. doi: 10.1016/0001-4575(95)00044-5. [DOI] [PubMed] [Google Scholar]
- 13.Winkleby MA, Ragland DR, Fisher JM, Syme SL. Excess risk of sickness and disease in bus drivers: a review and synthesis of epidemiological studies. Int J Epidemiol. 1988;17(2):255–262. doi: 10.1093/ije/17.2.255. [DOI] [PubMed] [Google Scholar]
- 14.Cox DJ, Gonder-Frederick LA, Kovatchev BP, Julian DM, Clarke WL. Progressive hypoglycemia's impact on driving simulation performance. Occurrence, awareness and correction. Diabetes Care. 2000;23(2):163–170. doi: 10.2337/diacare.23.2.163. [DOI] [PubMed] [Google Scholar]
- 15.Cox DJ, Gonder-Frederick LA, Kovatchev BP, Clarke WL. The metabolic demands of driving for drivers with type 1 diabetes mellitus. Diabetes Metab Res Rev. 2002;18(5):381–385. doi: 10.1002/dmrr.306. [DOI] [PubMed] [Google Scholar]
- 16.Lonnen KF, Powell RJ, Taylor D, Shore AC, MacLeod KM. Road traffic accidents and diabetes: insulin use does not determine risk. Diabet Med. 2008;25(5):578–584. doi: 10.1111/j.1464-5491.2008.02409.x. [DOI] [PubMed] [Google Scholar]
- 17.Eadington DW, Frier BM. Type 1 diabetes and driving experience: an eight year cohort study. Diabet Med. 1989;6(2):137–141. doi: 10.1111/j.1464-5491.1989.tb02101.x. [DOI] [PubMed] [Google Scholar]
- 18.Koepsell T, Wolf M, McCloskey L. Medical conditions and motor vehicle collision injuries in older adults. J Am Geriatr Soc. 1994;42(7):695–700. doi: 10.1111/j.1532-5415.1994.tb06526.x. [DOI] [PubMed] [Google Scholar]
- 19.UK Hypoglycaemia Study Group. Risk of hypoglycaemia in types 1 and 2 diabetes: effects of treatment modalities and their duration. Diabetologia. 2007;50(6):1140–1147. doi: 10.1007/s00125-007-0599-y. [DOI] [PubMed] [Google Scholar]
- 20.Pramming S, Thorsteinsson B, Bendtson I, Binder C. The relationship between symptomatic and biochemical hypoglycaemia in insulin-dependent diabetic patients. J Intern Med. 1990;228(6):641–646. doi: 10.1111/j.1365-2796.1990.tb00292.x. [DOI] [PubMed] [Google Scholar]
- 21.Stork AD, Van Haeften TW, Veneman TF. The decision not to drive during hypoglycemia in patients with type 1 and type 2 diabetes according to hypoglycemia awareness. Diabetes Care. 2007;30(11):2822–2826. doi: 10.2337/dc06-1544. [DOI] [PubMed] [Google Scholar]
- 22.DVLA. A guide to insulin treated diabetes and driving. Available from: http://www.diabetes-support.org.uk/dvla_6240.pdf.
- 23.Bodansky D, Bodansky H. Understanding, knowledge and attitudes towards current UK driving advice in insulin treated diabetic patients. Pract Diabetes Int. 2009;26:318–321. [Google Scholar]
- 24.Flanagan D, Watson J, Everett J, Cavan D, Kerr D. Driving and insulin–consensus, conflict or confusion? Diabet Med. 2000;17(4):316–320. doi: 10.1046/j.1464-5491.2000.00279.x. [DOI] [PubMed] [Google Scholar]
- 25.Cox DJ, Penberthy JK, Zrebiec J. Diabetes and driving mishaps: frequency and correlations from a multinational survey. Diabetes Care. 2003;26(8):2329–2334. doi: 10.2337/diacare.26.8.2329. [DOI] [PubMed] [Google Scholar]
- 26.Elmasry A, Lindberg E, Berne C, Janson C, Gislason T, Awad Tageldin M, Boman G. Sleep-disordered breathing and glucose metabolism in hypertensive men: a population-based study. J Intern Med. 2001;249(2):153–161. doi: 10.1046/j.1365-2796.2001.00787.x. [DOI] [PubMed] [Google Scholar]
- 27.Knipling RR, Wang JS. Research note: from the Office of Crash Avoidance Research. Washington DC: U.S. DOT/National Highway Traffic Safety Administration; 1994. Crashes and fatalities related to driver drowsiness/fatigue; pp. 1–8. [Google Scholar]
- 28.Sassani A, Findley LJ, Kryger M, Goldlust E, George C, Davidson TM. Reducing motor-vehicle collisions, costs, and fatalities by treating obstructive sleep apnea syndrome. Sleep. 2004;27(3):453–458. doi: 10.1093/sleep/27.3.453. [DOI] [PubMed] [Google Scholar]
- 29. http://www.technewsworld.com/story/healthcare/66096.html.
- 30.Forensic mobile phone work reveals threat to all of us. Available from: http://www.computerweekly.com/Articles/2009/10/20/238193/forensic-mobile-phone-work-reveals-threat-to-all-of.htm.
- 31. http://www.guardianinterlock.com/LegislationStudies.php.