Abstract
Background
B cells and antibodies are involved not only in controlling the spread of blood circulating Trypanosoma cruzi, but also in the autoreactive manifestations observed in Chagas disease. Acute infection results in polyclonal B cell activation associated with hypergammaglobulinemia, delayed specific humoral immunity and high levels of non-parasite specific antibodies. Since TNF superfamily B lymphocyte Stimulator (BAFF) mediates polyclonal B cell response in vitro triggered by T. cruzi antigens, and BAFF-Tg mice show similar signs to T. cruzi infected mice, we hypothesized that BAFF can mediate polyclonal B cell response in experimental Chagas disease.
Methodology/Principal Findings
BAFF is produced early and persists throughout the infection. To analyze BAFF role in experimental Chagas disease, Balb/c infected mice were injected with BR3:Fc, a soluble receptor of BAFF, to block BAFF activity. By BAFF blockade we observed that this cytokine mediates the mature B cell response and the production of non-parasite specific IgM and IgG. BAFF also influences the development of antinuclear IgG and parasite-specific IgM response, not affecting T. cruzi-specific IgG and parasitemia. Interestingly, BAFF inhibition favors the parasitism in heart.
Conclusions/Significance
Our results demonstrate, for the first time, an active role for BAFF in shaping the mature B cell repertoire in a parasite infection.
Author Summary
Chagas disease, caused by the protozoan Trypanosoma cruzi, is endemic in Central and South America. It affects 20 million people and about 100 million people are at risk of infection in endemic areas. Some cases have been identified in non-endemic countries as a consequence of blood transfusion and organ transplantation. Chagas disease presents three stages of infection. The acute phase appears one to two weeks after infection and includes fever, swelling around the bite site, enlarged lymph glands and spleen, and fatigue. This stage is characterized by circulating parasites and many immunological disturbances including a massive B cell response. In general, the acute episode self-resolves in about 2 months and is followed by a clinically silent indeterminate phase characterized by absence of circulating parasites. In about one-third of the cases, the indeterminate phase evolves into a chronic phase with clinically defined cardiac or digestive disturbances. Current knowledge suggests that the persistence of parasites coupled with an unbalanced immune response sustain inflammatory response in the chronic stage. We believe that an effective treatment for chronic Chagas disease should combine antiparasitic drugs with immunomodulators aimed at reducing inflammation and autoreactive response. Our findings enlighten a new role of BAFF-BAFF-R signaling in parasite infection that partially controls polyclonal B cell response but not parasitespecific class-switched primary effectors B cells.
Introduction
Chagas disease is a chronic disease caused by infection with Trypanosoma cruzi. Initially, the disease goes through an acute episode which is characterized by circulating parasites and immunological disturbances that, at the level of B cell compartment, are mature and immature B cell apoptosis [1], [2] as well as massive B cell response [3]. This polyclonal response [4]–[6], which results in hipergammaglobulinemia [7] and delayed parasite specific humoral response [8], [9], may be the original cause for the autoimmune phenomena that have been described in chronic phases of infection [10], [11]. It is well known that polyclonal activation of B lymphocytes is invariably accompanied by autoantibody production [12], [13].
The polyclonal B cell activation that occurs during infection, induced by the host response (T cell response, cytokines) or parasite antigens, may disrupt normal immune regulatory mechanisms and cause autoimmunity [14] It has been reported that polyclonal B cell response in T. cruzi infected mice is predominantly helper T-cell dependent [15]. However, Ig-secreting plaque-forming cells are recorded in athymic (nude) mice after T. cruzi infection [5] suggesting that T-independent mechanisms can also mediate polyclonal B cell response. Several parasite-encoded proteins have been identified as B cell mitogens [13], [16]–[18] and some of these T. cruzi antigens trigger in vitro polyclonal B cell activation and differentiation in a T-independent way [16], [17]. We have reported that macrophages from normal mice cultured with T. cruzi glutamate dehydrogenase, a T-independent type II polyclonal B cell activator, secrete high level of BAFF that mediates B cell polyclonal activation [17], suggesting that BAFF may mediate the polyclonal B cell response in vivo during T. cruzi infection.
BAFF is a crucial factor for the survival of peripheral B cells [19]–[21]. But, in excess, BAFF leads to the development of autoimmune disorders in animal models. It has been described that BAFF transgenic mice show clear signs of B cell hyperplasia and hyperglobulinemia. These mice have enlarged spleen, Peyer's patches and lymph nodes, circulating immune complexes, rheumatoid factors, and anti-DNA Abs [22]. In addition, high levels of BAFF have been detected in the serum of patients with various autoimmune disorders [23], [24]. Based on the fact that BAFF transgenic and T. cruzi infected mice share many immunological features like polyclonal activation, autoantibody production and autoimmunity, we hypothesized that BAFF can participate in the polyclonal B cell response observed in experimental Chagas disease. In the present study, we quantified the levels of BAFF and analyzed the participation of BAFF on B cell response by blocking its activity with a soluble BAFF-receptor in T. cruzi infected mice.
Methods
Infection with T. cruzi and treatment with BR3:Fc or control IgG2a
BALB/c mice were originally obtained from School of Veterinary, La Plata National University (La Plata, Argentina) and housed in our animal facility where all experiments were performed in compliance with the Institutional Review Board and Ethical Committee of the School of Chemical Sciences, National University of Cordoba. BALB/c mice 6–8 wk old were intraperitoneally (i.p.) infected with 500 trypomastigotes from T. cruzi (Tulahuén strain) diluted in physiological solution, as previously described [2], [25]. Non-infected normal littermates were injected i.p. with physiological solution and processed in parallel. For BAFF activity blocking, one day after infection, mice were injected i.p. with 150 ug of BR3:Fc (Genentech Inc., South San Francisco, CA, USA) three times per week. As control, infected mice were injected with 150 ug of IgG2a or physiological solution. Non-infected normal littermates were injected i.p. with physiological solution and injected i.p. with 150 ug of BR3:Fc or 150 ug of IgG2a or physiological solution with the same schedule described above and processed in parallel. At 15 days after infection, mice (number indicated in each figure) were killed by cervical dislocation, blood was collected and lymphoid organs were removed.
BR3:Fc efficacy of BAFF neutralization was tested in vivo evaluating the reduction of splenic B cell subsets according to Lin et al [26]. Also, BR3:Fc neutralizing BAFF activity was evaluated in an in vitro assay measuring IgA concentration in the supernatant of peritoneal B cells cultured with CpG plus recombinant BAFF [27], [28] in presence or in absence of BR3:Fc (data not shown).
Parasitemia counts
Blood was collected by retro-orbital bleeding, erythrocytes were lysed in a 0.87% ammonium chloride buffer, and viable trypomastigotes counted in a Neubauer counting chamber [2].
Cell preparation
Spleen and inguinal lymph nodes were obtained and homogenized through a tissue strainer. Peritoneal cells were obtained by peritoneal washouts and bone marrow cells were isolated by flushing femurs and tibias of mice with RPMI 1640. When it was necessary, red blood cells were lysed for 5 min in Tris-ammonium chloride buffer. Viable mononuclear cell numbers were determined by trypan blue exclusion using a Neubauer counting chamber. Cell suspensions were processed for Flow cytometry studies or culture as indicated below.
Purification of splenic cell population by cell sorting
To obtain B cells, T cells, dendritic cells and F 4/80+ macrophages, splenic cells from infected mice were stained with anti-B220 APC, anti-CD3 FITC, anti-CD11c PE, anti-F4/80 Biotin followed by Streptavidin Per-CP purchased from BD, and sorted by positive selection with FACSAria Cell Sorter (Becton Dickinson) to enrich populations to 98% for B and T cells and 88% for CD11c+ and F 4/80+.
Reverse transcription of mRNA and its relative quantification by real time
Cells were incubated with TRIzol reagents (Life Technologies) and RNA was extracted according to the manufacturer's recommendation and stored at −70°C. RNA was reverse transcribed using Moloney murine leukemia virus reverse transcriptase (Invitrogen, USA) at 42°C for 60 min. One microgram of RNA was used to generate first cDNA strain. Real Time PCR reactions for mouse BAFF and β-Actin detection were performed using the following primers pairs: BAFF (Mm00446347_m1, Applied Biosystems) and HPRT (HPRT-F: 5′-AAGCTTGCTGGTGAAAAGGA-3′; and HPRT R: 5′-TCCAACAAAGTCTGGCCTGT-3′). The reaction mixtures contained: TaqMan Universal PCR Master Mix in the case of BAFF or 2X SYBR Green PCR Master Mix, 800 nM of HPRT primers, and 50 ng of cDNA. All reactions were performed in triplicate and were cycled as follows: 95°C for 10 min, 1 cycle; 95°C 15 s, 60°C 1 min, 40 cycles; 95°C 15 s, 1 cycle, 60°C 1 min, 1 cycle, followed by a melting curve rising from 60 to 95°C incrementally using in a 7500 System apparatus (Applied Biosystems). HPRT was used as standard to normalize cDNA loading [29].
Flow cytometry studies
Cell suspensions were washed twice in ice-cold FACS buffer (Physiological solution with 2% fetal bovine serum (FBS, Gibco)) and preincubated with anti-mouse CD32/CD16 mAb (Fc block) for 30 min at 4°C. The cells were then incubated with each PE-, FITC-, or biotinylated Ab (e-Bioscience, San Diego, USA) for 30 min at 4°C and washed with FACS buffer: PE-anti B220, FICT-anti IgM and biotin-anti IgD to identify mature B cells; PE-anti CD138 and FICT-anti B220 to identify plasma cells; PE-anti B220, FICT-anti CD24 and biotin anti IgD to identify mature B cells in bone marrow, and biotin anti B220 to identify peritoneal B cells. Data were acquired on a FACSCanto II cytometer (Becton Dickinson) and analyzed using Flow Jo (Tree Star) software.
Soluble BAFF determination
BAFF concentration (ng/ml) was determined in sera and culture supernatant of mononuclear cells from lymphoid organs from normal or T. cruzi infected mice by ELISA following manufacturer's instructions (Axxora, USA).
Total immunoglobulin determination
Mononuclear cells from lymphoid organs from normal or T. cruzi infected mice treated with physiological solution or BR3:Fc or IgG2a control obtained at day 15 post infection (p.i.) were cultured with media for 30 h. IgM and IgG concentrations (ng/ml) were determined by ELISA as previously described [17]. In brief, plates were coated with 2.5 ug/ml of the type-specific goat anti-mouse Ab (IgM, IgG; Sigma-Aldrich Chemical Co) overnight at 4°C, and blocked with 1% Bovine serum albumin (BSA). Culture supernatants were incubated overnight at 4°C. Peroxidase-conjugated anti-mouse IgG or anti-mouse IgM (2.5 µg/ml) were added and incubated for 1 h at 37°C. The reaction was developed with TMB Substrate Reagent (BD OptEIA™). The concentration was measured with reference to standard curves using known amounts of the respective murine Ig (Sigma-Aldrich Chemical Co.).
Parasite specific serum Ab determination
The titers of T. cruzi specific seric IgM and IgG were determined by ELISA [30], [31] using T. cruzi trypomastigotes recombinant Ags following manufacturer instruction (Wiener lab, Argentina). ELISA test sera were considered positive if the mean OD value was two standard deviations above the mean value for control sera assayed in parallel.
ANA serum IgG determination
Amount of antinuclear specific IgG Ab (ng/ml) and IgG1, IgG2a and IgG3 (OD) was determined by ELISA using a ANA ELISA kit (Alpha Diagnostic, San Antonio, TX, USA) following the manufacturer's instructions in sera from T. cruzi infected mice treated with physiological solution or BR3:Fc or IgG2a control.
Histopathology studies
Hearts were fixed in formaldehyde and embedded in paraffin blocks, after which 5 to 20-µm-thick transverse sections were mounted on slides and subsequently stained with hematoxylin and eosin. Photographs were taken using a Nikon Eclipse TE 2000 U equipped with a digital video camera. The grade of heart parasitism was evaluated analyzing the number of nests containing amastigotes per section.
Statistical analysis
Statistical significance of comparisons of mean values was assessed by a two-tailed Student's t test or nonparametric Mann-Whitney U test using Graph pad software. In the case of T. cruzi specific Abs, mean values was assessed by a one way non parametric Kruskal-Wallis test. p≤0.05 was considered significant.
Results
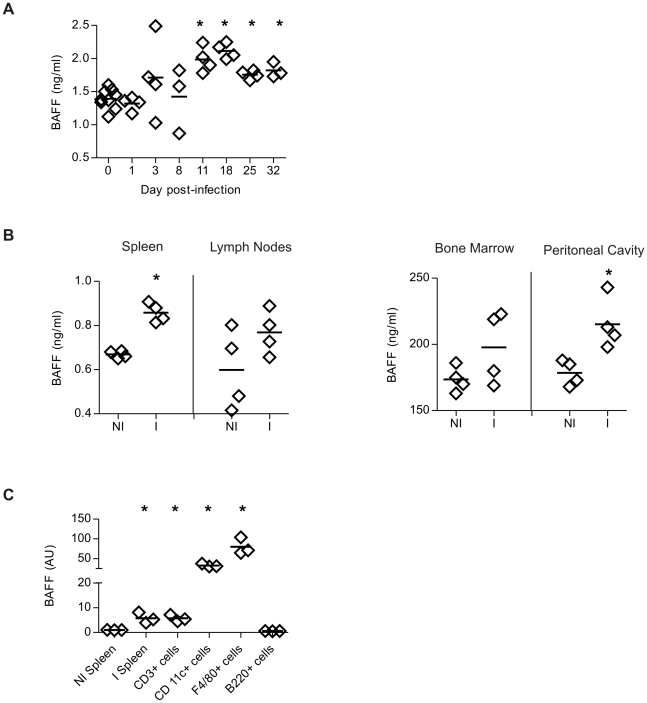
BAFF concentration increased as a consequence of T. cruzi infection
To investigate systemic BAFF concentration during T. cruzi infection, serum samples were collected at different times p.i. and analyzed for levels of circulating BAFF by ELISA. During an ongoing T. cruzi infection, a significant increase in the seric levels of BAFF was detected at 11 days p.i. BAFF concentration presented the highest value at the peak of parasitemia (day 11–15 p.i, [2]) and persisted elevated until the last day analyzed (day 32 p.i) (Fig 1A). Additionally, cells from the spleen and bone marrow, but not from the lymph nodes and peritoneal cavity, obtained from 15-day infected mice and cultured in the absence of stimuli, released higher concentrations of BAFF than cells from non-infected mice (Fig 1B).
Figure 1. BAFF production in T. cruzi infected mice.
BAFF concentration (ng/ml) was determined by ELISA in: A, Sera from non-infected (day 0) or T. cruzi infected mice obtained at different times of infection, B, culture supernatant of cells from spleen, bone marrow, lymph nodes and peritoneal cavity from non-infected (NI) or T. cruzi infected (I) mice obtained at 15 days p.i. C, Splenic CD3+, CD11c+, F4/80+ and B220+ cells from T. cruzi infected mice were purified by cell sorting. mRNAs were obtained from these populations from total splenic cells from I mice. Spleen cells from NI and I mice were used as control. BAFF mRNA levels were quantified by Real Time PCR. The amounts of transcripts were normalized to HPRT transcripts and were expressed relative to the amount in splenic cells from NI mice. Diamonds represent the value obtained from each mouse. The lines represent the media value in each analyzed group. *, p≤0.05. Results are representative for two individual experiments.
To identify which mononuclear cells produced BAFF in T. cruzi infected mice, CD3+cells, CD11c+cells, F4/80+ cells and B220+ cells were obtained by cell sorting from the spleen of infected mice. By real-time PCR we determined that F4/80+ cells and CD11c+ cells showed high levels of mRNA coding for BAFF. The transcript for BAFF was present at low levels in T cells and undetectable in B cells. mRNA from total spleen cells from T. cruzi infected mice was used as positive control (Fig 1C).
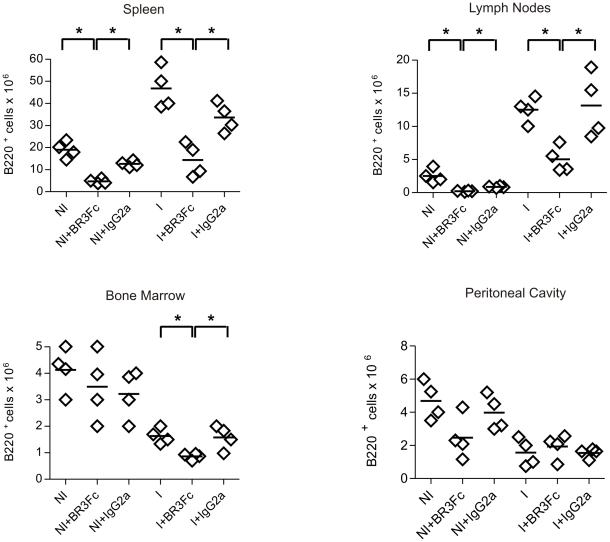
BAFF blockade resulted in a diminution of mature B cells in lymphoid organs
In order to analyze the potential role of BAFF in the massive B cell response in experimental Chagas disease, BAFF activity was blocked by injecting BR3:Fc, a soluble BAFF receptor, into T. cruzi infected mice. Considering that the different B cell compartments are dissimilarly affected by T. cruzi infection [2], [32], [33], we evaluated how the BAFF blockade affected each B cell compartment individually.
We observed that treatment with BR3:Fc resulted in a significant reduction of splenic and lymph nodes B220+ cell number in non-infected and in T. cruzi infected mice (Fig 2). We determined that the reduction affected mature B220+IgD+IgM+ spleen cells but did not induce significant changes in the number of B220+IgD−IgM+ spleen cells (phenotype compatible with immature, marginal zone and activated B cell) (Fig S1 A). BAFF inhibition reduced the already low number of B cells present in the bone marrow of T. cruzi infected but did not affect the number of B cells in the bone marrow of normal mice (Fig 2). This result could be explained by the fact that BAFF blockade affected mature B220+ IgD+CD24+ but not immature B220+ IgD− CD24hi B cells from bone marrow (Fig S1 B). Immature B cells are the major B cell population in the bone marrow of normal mice but are almost absent in T. cruzi infected mice that present only mature B cells [2]. In addition, we determined that BAFF blockade did not change the number of peritoneal B220+ cells observed in T. cruzi infected mice (Fig 2) that were reduced as a consequence of infection [34]. Mice injected with control isotype non-blocking Ab presented no significant difference in B cell number in comparison to non-treated non infected (NI) or infected (I) mice (Fig 2).
Figure 2. B cell number in non-infected or T. cruzi infected mice treated with BR3:Fc.
Cells from spleen, lymph nodes, bone marrow and peritoneal cavity from non-infected (NI) or T. cruzi infected (day 15 p.i.) mice treated with physiological solution (I) or BR3:Fc (I+BR3:Fc) or IgG2a control (I+IgG2a) were obtained, stained with anti-B220 and analyzed by flow cytometry. Graphs show the number of B220+ cells in different lymphoid compartments. Diamonds represent the value obtained from each mouse. The lines represent the media value.*, p≤0.05. Results are representative for three individual experiments.
Next, we analyzed if B cell reduction observed in lymphoid organs as a consequence of BAFF blockade also affected plasma cell number. B220+CD138+ cell number declined markedly in the spleen but remained unchanged in lymph nodes of BR3:Fc treated-T. cruzi infected mice (Fig 3). T. cruzi infection per se induced a severe reduction of plasma cell number in bone marrow (Fig 3) and no further reduction was observed after BAFF blockade.
Figure 3. Plasma cell number in non-infected or T. cruzi infected mice treated with BR3:Fc.
Cells from spleen, lymph nodes and bone marrow from non-infected (NI) or T. cruzi infected (day 15 p.i.) mice treated with physiological solution (I) or BR3:Fc (I+BR3:Fc) or IgG2a control (I+IgG2a) were obtained, stained with anti-B220 and anti-CD138 and analyzed by flow cytometry. Graphs show the number of B220+CD138+cells analyzed in each experimental group. Diamonds represent the value obtained from each mouse. The lines represent the media value in each condition.*, p≤0.05. Results are representative for three individual experiments.
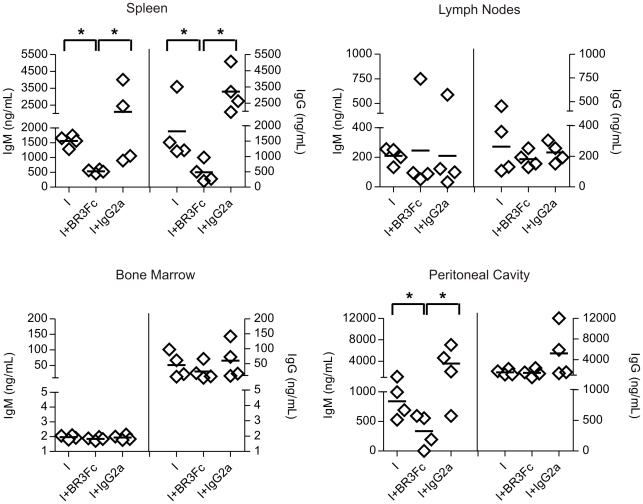
BAFF inhibition partly impairs humoral immune response in T. cruzi infected mice
The reduction of plasma cell number in T. cruzi infected mice treated with BR3:Fc correlated with a significant reduction in IgM and IgG concentration in culture supernatant of splenic cells (Fig 4). Interestingly, while the concentration of IgG was maintained, a reduction of IgM concentration was detected in the culture supernatant of cells from peritoneum of T. cruzi infected mice with blocked BAFF activity. According to plasma cell number results, no differences were detected in IgM and IgG concentrations produced by cells from lymph nodes and bone marrow from treated and untreated infected mice (Fig 4).
Figure 4. Immunoglobulin concentration in T. cruzi infected mice treated with BR3:Fc.
Cells from spleen, lymph nodes, bone marrow and peritoneal cavity from T. cruzi infected (day 15 p.i.) mice treated with physiological solution (I) or BR3:Fc (I+BR3:Fc) or IgG2a control (I+IgG2a) were obtained and cultured with media without any stimulus for 30 h. IgM and IgG concentration (ng/ml) was determined in culture supernatants by ELISA. Diamonds represent the value obtained from each mouse. The lines represent the media value in each condition.*, p≤0.05. Results are representative for three individual experiments.
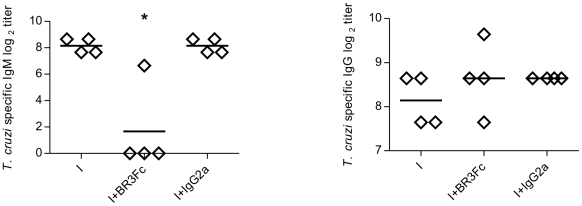
To analyze the biological significance of the reduced Ab response observed in BR3:Fc treated T. cruzi infected mice, we evaluated the levels of parasite specific Abs in sera. We observed that preventing BAFF binding drastically diminished trypomastigotes T. cruzi-specific IgM titers while T. cruzi-specific IgG titers did not change (Fig 5). Parasite-specific Abs were practically undetectable in the culture supernatants of the lymphoid organs obtained from infected mice indicating a low frequency of T. cruzi antigen-specific B cells as reported [8], [9] and a high frequency of non-parasite specific Abs (data not shown).
Figure 5. Parasite specific immunoglobulins in sera from T. cruzi infected mice treated with BR3:Fc.
Sera from T. cruzi infected mice treated with physiological solution (I) or BR3:Fc (I+BR3:Fc) or IgG2a control (I+IgG2a) were obtained at day 15 p.i. and analyzed by ELISA to determine T. cruzi specific IgM and IgG Ab titers. Diamonds represent the value obtained from each mouse. The lines represent the media value in each case. *, p≤0.05. Results are representative for two individual experiments.
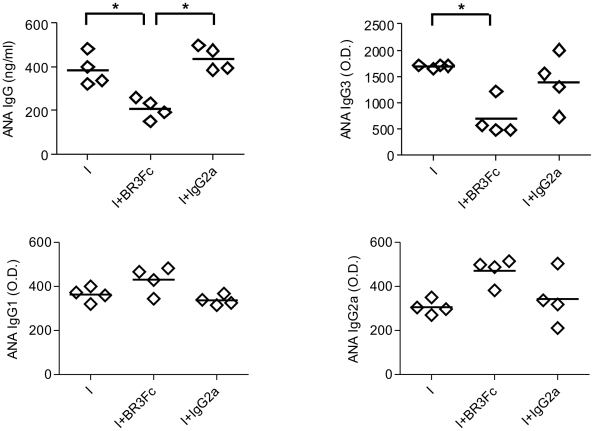
To address the role of BAFF in the autoreactive humoral response, we evaluated autoreactive Abs in the sera of treated and control infected mice at 15 days p.i.. It has been described that autoreactive Abs such as anti-actin, anti-myosin, anti-myoglobin and antinuclear Abs (ANA) among others are present in the acute and chronic phase of the pathology [35]–[37]. However, we were unable to detect autoreactive Abs others than ANA at the acute phase of the infection (day 15 p.i.). Therefore, ANA were tested as markers of the effect of BR3:Fc treatment on the autoreactive B cell population during acute phase of infection. We observed that BAFF blockade prevented the production of ANA of IgG isotype in T. cruzi infected mice. The isotype of IgG involved in this reaction was IgG3 but not IgG2a or IgG1 (Fig 6).
Figure 6. Autoreactive immunoglobulins in sera from T. cruzi infected mice treated with BR3:Fc.
Sera from T. cruzi infected mice treated with physiological solution (I) or BR3:Fc (I+BR3:Fc) or IgG2a control (I+IgG2a) were obtained at day 15 p.i. and analyzed by ELISA to determine the levels of antinuclear (ANA) specific IgG (ng/mL) or ANA IgG3, IgG1 and IgG2a (O. D.) Diamonds represent the value obtained from each mouse. The lines represent the media value in each case. *, p≤0.05. Results are representative for two individual experiments.
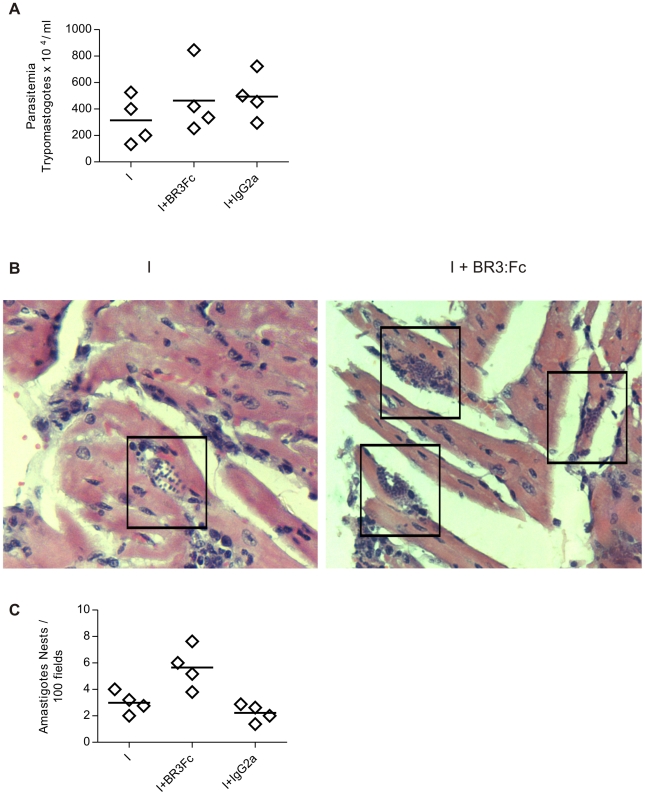
BAFF inhibition influences parasite replication in the heart
To analyze if B cell reduction and the decrease of IgM parasite-specific Abs affected the parasite replication, we measured the number of circulating trypomastigotes in blood of infected mice and the grade of tissue parasitism by evaluating amastigote niches in heart. Parasitemia was similar in T. cruzi infected mice treated with physiological solution, BR3:Fc or IgG2a control (Fig 7A), while cardiac parasitism was increased in BR3:Fc treated infected mice in comparison to untreated infected mice (Fig 7B,C). Thus, the hearts of infected mice in which BAFF activity was blocked had higher number of nest of amastigotes in the myocardial fibers of the auricle than non-treated infected mice (Fig 7B,C).
Figure 7. Circulating and tissue parasites in T. cruzi infected mice treated with BR3:Fc.
A, Number of circulating parasites in blood samples from T. cruzi infected mice treated with physiological solution (I) or BR3:Fc (I+BR3:Fc) or IgG2a control (I+IgG2a) was determined at days 15 p.i. by counting in Neubauer chamber. B, Photomicrographs from heart sections obtained from T. cruzi infected mice treated with physiological solution (I) or BR3:Fc (I+BR3:Fc) stained with hematoxilina/eosina (400X). Amastigote nests are demarcated with squares. Inset shows one of them (1000X). C, Number of amastigote nests counted in 100 histological fields of hearts. Diamonds represent the value obtained from each mouse. The lines represent the media value in each day p.i. Results are representative for two individual experiments.
Discussion
Most of the information about BAFF in disease is linked to autoimmune pathologies [38], but little information is available about BAFF in infectious diseases [39], [40]. Previously, we reported that BAFF is involved in the polyclonal B cell activation triggered in vitro by a T. cruzi antigen [17]. Here, we extended these data showing that BAFF increased early in T. cruzi infected mice and persisted at high levels throughout the infection. Our data show that cells from immune system as macrophages and dendritic cells which are susceptible to be infected by T. cruzi and in which the parasite can replicate intracellularly [41], [42] are an important source of BAFF. It has been reported that BAFF is mainly produced by innate immune cells such as neutrophils, macrophages, monocytes, dendritic cells (DCs) and follicular DCs [43] stimulated by cytokines often produced during inflammation and infections [43], [44], as well as by the Toll-like receptors ligands [45]. Then, it is possible that IL-10 and/or IFNγ, which increase during infection [46]–[48], as well as TLR ligands expressed by T. cruzi [49], [50] or parasite antigens [17] trigger BAFF secretion.
To analyze the role of BAFF in T. cruzi infection, infected mice were treated with a soluble BAFF-R, BR3:Fc, to block BAFF activity. The use of BAFF-R Fc considerably reduced mature peripheral B cell numbers in T. cruzi infected mice. As it was previously reported for normal mice [21], [51], [52], we observed that mature B cells from T. cruzi infected mice have different BAFF requirements than peritoneal mature B cells and/or immature B cells for their survival. Reduction in mature B cells was also observed in the bone marrow of infected mice, probably as a consequence of the diminution of peripheral mature B cells.
Following B cell depletion, BAFF blockade resulted in a reduction of splenic B220+CD138+ plasma cells. When we analyzed the proportion of plasma cells with respect to the number of total B cells we observed similar values in BR3:Fc treated or untreated infected mice (data not shown). These results suggest that during T. cruzi infection, BAFF apparently controls plasma cell numbers by reducing the pool of mature B cells. Concomitantly with plasma cell diminution, a reduction of total IgM and IgG production by splenic cells was observed in BR3:Fc treated infected mice. Since most of the Abs produced by splenic B cells are non-parasite specific [8], our results suggest that BAFF is regulating polyclonally activated B cells rather than antigen-specific activated B cells. In agreement, parasite-specific IgG titers were not affected by BAFF blockade while parasite-specific IgM almost disappeared in BR3:Fc treated infected mice. Similar behaviour was observed in three different independent experiments analyzed at 15 and 22 days p.i. Our results confirm and complete previously reported findings on the role of BAFF-BAFF-R signalling in the survival and maintenance of the mature B cell compartments [reviewed in 53], and that BAFF inhibition had a markedly small effect on IgG+ B cells and long-lived plasma cells. Scholz et al [54] reported that IgM-bearing memory cells are sensitive to BAFF depletion whereas IgG-bearing memory cells are not.
Chagas disease pathology is associated to autoimmunity [55]–[57]. There are several mechanisms to explain autoimmunity induced by infectious agents [58]. All are based on the observation that an immunocompetent host possesses circulating autoreactive T and B cells that are normally tolerant to self antigens [59]. As a consequence of the favorable proinflammatory environment induced by microorganisms, an unspecific activation may occur [60]. Excess BAFF may lower the threshold for BCR signaling and maintain survival when a normal autoreactive B cell would undergo death [61]. In agreement with reports showing evidences of BAFF participation in autoreactive response [62]–[67], BAFF blockade decreases the ANA IgG in T. cruzi infected mice. According to our results, it has been previously reported that a 4-week course of BAFF-R–Ig prevents the emergence of IgG anti-DNA antibodies in NZB/W mice [68].
The presence of anti-self antibodies was reported at the acute and chronic phase of T. cruzi infection [35], [37]. However, in our infection model, probably as consequence of different experimental conditions and the parasite and mouse strain used, we were unable to detect, by ELISA, anti-myosin, anti- myoglobin and anti-skeletal muscle antibodies in sera of acutely-infected mice (day 15 p.i.). Consequently, we ignore whether BAFF blockade affects the production of other autoreactive Abs different from ANA. Our data analyzed together indicated that autoreactive IgG3+ B cells activated during the infection and the parasite specific IgG+ B cells induced by T. cruzi show a differential requirement of BAFF to proliferate and/or differentiate and/or survive. This difference is probably related to the nature of B cell response: T-independent, extrafolicular or from germinal center [53]. Probably IgG3 ANA are produced during a pre-germinal center response [69]–[71] while anti-T. cruzi IgG Abs are produced in the course of a germinal center response (Bermejo et al. unpublished observation). Importantly, this differential requirement of BAFF may become an important target of manipulation to control a possible pathological autoreactive response without dampening the protective parasite specific response.
Interestingly, blocking BAFF is apparently not affecting the Abs involved in the control of circulating trypomastigotes. It seems that the conserved levels of IgG are sufficient to control parasite replication, or that, other populations different from B cells and not affected by BAFF inhibition, may be controlling parasite spreading. However, BAFF blockade does impact in T. cruzi replication in the heart, favoring the appearance of T. cruzi pseudocyts. The increase in the parasite replication in target tissues observed in BR3:Fc treated mice could be consequence of the markedly reduced mature B cell numbers that affect not only the production of Abs but also the development of protective cellular responses [72]. Strikingly, in spite of the high number of T. cruzi pseudocyts observed in the hearts of infected mice, preliminary data showed that BR3:Fc treated mice survive longer than non-treated infected mice (data not shown). Our findings enlighten a new role of BAFF-BAFF-R signalling in a parasite infection where it controls mature B cell numbers, polyclonal B cell activation and self-reactive response but does not affect protective anti-parasite IgG response.
Supporting Information
Immature and mature B cell number in non-infected or T. cruzi infected mice treated with BR3:Fc. Cells from spleen and bone marrow from non-infected (NI) or T. cruzi infected (day 15 p.i.) mice treated with physiological solution (I) or BR3:Fc (I+BR3:Fc) or IgG2a control (I+IgG2a) were obtained. Cells from spleen were stained with anti-B220, anti-IgD and anti-IgM, and cells from bone marrow were stained with anti-B220, anti-IgD and anti-CD24 and analyzed by flow cytometry. Graphs show the number of: A) B220+ IgD+IgM+ (mature B cells) and B220+IgD-IgM+ in spleen and B) B220+IgD+CD24+ (mature B cells) and B220+IgD-CD24hi (immature B cells) in bone marrow. Diamonds represent the value obtained from each mouse. The lines represent the media value. *, p<0.05. Results are representative for three individual experiments.
(0.58 MB TIF)
Acknowledgments
We thank Genentech Inc. for providing us BR3:Fc and IgG2a control. We are grateful to Renata Defago for language corrections.
Footnotes
The authors have declared that no competing interests exist.
This work received financial support from CONICET, ANPCyT, SECYT-UNC to AG, and Fundacion Bunge y Born to EVAR. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Zuniga E, Motran CC, Montes CL, Yagita H, Gruppi A. Trypanosoma cruzi infection selectively renders parasite-specific IgG+ B lymphocytes susceptible to Fas/Fas ligand-mediated fratricide. J Immunol. 2002;168:3965–3973. doi: 10.4049/jimmunol.168.8.3965. [DOI] [PubMed] [Google Scholar]
- 2.Zuniga E, Acosta-Rodriguez E, Merino MC, Montes C, Gruppi A. Depletion of immature B cells during Trypanosoma cruzi infection: involvement of myeloid cells and the cyclooxygenase pathway. Eur J Immunol. 2005;35:1849–1858. doi: 10.1002/eji.200526005. [DOI] [PubMed] [Google Scholar]
- 3.Minoprio P, Bandeira A, Pereira P, Mota ST, Coutinho A. Preferential expansion of Ly-1 B and CD4- CD8- T cells in the polyclonal lymphocyte responses to murine T. cruzi infection. Int Immunol. 1989;1:176–184. doi: 10.1093/intimm/1.2.176. [DOI] [PubMed] [Google Scholar]
- 4.Ortiz-Ortiz L, Parks DE, Rodriguez M, Weigle WO. Polyclonal B lymphocyte activation during Trypanosoma cruzi infection. J Immunol. 1980;124:121–126. [PubMed] [Google Scholar]
- 5.D'Imperio Lima MR, Joskowicz M, Coutinho A, Kipnis T, Eisen H. Very large and isotypically atypical polyclonal plaque-forming cell responses in mice infected with Trypanosoma cruzi. Eur J Immunol. 1985;15:201–203. doi: 10.1002/eji.1830150219. [DOI] [PubMed] [Google Scholar]
- 6.D'Imperio Lima MR, Eisen H, Minoprio P, Joskowicz M, Coutinho A. Persistence of polyclonal B cell activation with undetectable parasitemia in late stages of experimental Chagas' disease. J Immunol. 1986;137:353–356. [PubMed] [Google Scholar]
- 7.Schmunis GA, Szarfman A, Coarasa L, Vainstok C. Immunoglobulin concentration in treated human acute Chagas disease. A follow-up study. Am J Trop Med Hyg. 1978;27:473–477. doi: 10.4269/ajtmh.1978.27.473. [DOI] [PubMed] [Google Scholar]
- 8.Minoprio P, Burlen O, Pereira P, Guilbert B, Andrade L, et al. Most B cells in acute Trypanosoma cruzi infection lack parasite specificity. Scand J Immunol. 1988;28:553–561. doi: 10.1111/j.1365-3083.1988.tb01487.x. [DOI] [PubMed] [Google Scholar]
- 9.Minoprio P, Itohara S, Heusser C, Tonegawa S, Coutinho A. Immunobiology of murine T. cruzi infection: the predominance of parasite-nonspecific responses and the activation of TCRI T cells. Immunol Rev. 1989;112:183–207. doi: 10.1111/j.1600-065x.1989.tb00558.x. [DOI] [PubMed] [Google Scholar]
- 10.Khoury EL, Ritacco V, Cossio PM, Laguens RP, Szarfman A, et al. Circulating antibodies to peripheral nerve in American trypanosomiasis (Chagas' disease). Clin Exp Immunol. 1979;36:8–15. [PMC free article] [PubMed] [Google Scholar]
- 11.Leon JS, Daniels MD, Toriello KM, Wang K, Engman DM. A cardiac myosin-specific autoimmune response is induced by immunization with Trypanosoma cruzi proteins. Infect Immun. 2004;72:3410–3417. doi: 10.1128/IAI.72.6.3410-3417.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lanzavecchia A, Sallusto F. Toll-like receptors and innate immunity in B-cell activation and antibody responses. Curr Opin Immunol. 2007;19:268–274. doi: 10.1016/j.coi.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 13.Montes CL, Vottero-Cima E, Gruppi A. Trypanosoma cruzi cytosolic alkaline antigens (FI) induce polyclonal activation in murine normal B cells. Scand J Immunol. 1996;44:93–100. doi: 10.1046/j.1365-3083.1996.d01-285.x. [DOI] [PubMed] [Google Scholar]
- 14.Minoprio P. Parasite polyclonal activators: new targets for vaccination approaches? Int J Parasitol. 2001;31:588–591. doi: 10.1016/s0020-7519(01)00171-0. [DOI] [PubMed] [Google Scholar]
- 15.Minoprio P, Eisen H, Joskowicz M, Pereira P, Coutinho A. Suppression of polyclonal antibody production in Trypanosoma cruzi-infected mice by treatment with anti-L3T4 antibodies. J Immunol. 1987;139:545–550. [PubMed] [Google Scholar]
- 16.Gao W, Wortis HH, Pereira MA. The Trypanosoma cruzi trans-sialidase is a T cell-independent B cell mitogen and an inducer of non-specific Ig secretion. Int Immunol. 2002;14:299–308. doi: 10.1093/intimm/14.3.299. [DOI] [PubMed] [Google Scholar]
- 17.Montes CL, Acosta-Rodriguez EV, Mucci J, Zuniga EI, Campetella O, et al. A Trypanosoma cruzi antigen signals CD11b+ cells to secrete cytokines that promote polyclonal B cell proliferation and differentiation into antibody-secreting cells. Eur J Immunol. 2006;36:1474–1485. doi: 10.1002/eji.200535537. [DOI] [PubMed] [Google Scholar]
- 18.Reina-San-Martin B, Degrave W, Rougeot C, Cosson A, Chamond N, et al. A B-cell mitogen from a pathogenic trypanosome is a eukaryotic proline racemase. Nat Med. 2000;6:890–897. doi: 10.1038/78651. [DOI] [PubMed] [Google Scholar]
- 19.Moore PA, Belvedere O, Orr A, Pieri K, LaFleur DW, et al. BLyS: member of the tumor necrosis factor family and B lymphocyte stimulator. Science. 1999;285:260–263. doi: 10.1126/science.285.5425.260. [DOI] [PubMed] [Google Scholar]
- 20.Schneider P, Mackay F, Steiner V, Hofmann K, Bodmer JL, et al. BAFF, a novel ligand of the tumor necrosis factor family, stimulates B cell growth. J Exp Med. 1999;189:1747–1756. doi: 10.1084/jem.189.11.1747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Batten M, Groom J, Cachero TG, Qian F, Schneider P, et al. BAFF mediates survival of peripheral immature B lymphocytes. J Exp Med. 2000;192:1453–1466. doi: 10.1084/jem.192.10.1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mackay F, Woodcock SA, Lawton P, Ambrose C, Baetscher M, et al. Mice transgenic for BAFF develop lymphocytic disorders along with autoimmune manifestations. J Exp Med. 1999;190:1697–1710. doi: 10.1084/jem.190.11.1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gross JA, Johnston J, Mudri S, Enselman R, Dillon SR, et al. TACI and BCMA are receptors for a TNF homologue implicated in B-cell autoimmune disease. Nature. 2000;404:995–999. doi: 10.1038/35010115. [DOI] [PubMed] [Google Scholar]
- 24.Zhang J, Roschke V, Baker KP, Wang Z, Alarcon GS, et al. Cutting edge: a role for B lymphocyte stimulator in systemic lupus erythematosus. J Immunol. 2001;166:6–10. doi: 10.4049/jimmunol.166.1.6. [DOI] [PubMed] [Google Scholar]
- 25.Zuniga E, Motran C, Montes CL, Diaz FL, Bocco JL, et al. Trypanosoma cruzi-induced immunosuppression: B cells undergo spontaneous apoptosis and lipopolysaccharide (LPS) arrests their proliferation during acute infection. Clin Exp Immunol. 2000;119:507–515. doi: 10.1046/j.1365-2249.2000.01150.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lin WY, Gong Q, Seshasayee D, Lin Z, Ou Q, et al. Anti-BR3 antibodies: a new class of B-cell immunotherapy combining cellular depletion and survival blockade. Blood. 2007;110:3959–3967. doi: 10.1182/blood-2007-04-088088. [DOI] [PubMed] [Google Scholar]
- 27.Genestier L, Taillardet M, Mondiere P, Gheit H, Bella C, et al. TLR agonists selectively promote terminal plasma cell differentiation of B cell subsets specialized in thymus-independent responses. J Immunol. 2007;178:7779–7786. doi: 10.4049/jimmunol.178.12.7779. [DOI] [PubMed] [Google Scholar]
- 28.Tezuka H, Abe Y, Iwata M, Takeuchi H, Ishikawa H, et al. Regulation of IgA production by naturally occurring TNF/iNOS-producing dendritic cells. Nature. 2007;448:929–933. doi: 10.1038/nature06033. [DOI] [PubMed] [Google Scholar]
- 29.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 30.Laderach D, Cerban F, Motran C, Vottero de CE, Gea S. Trypanosoma cruzi: the major cysteinyl proteinase (cruzipain) is a relevant immunogen of parasite acidic antigens (FIII). Int J Parasitol. 1996;26:1249–1254. doi: 10.1016/s0020-7519(96)00099-9. [DOI] [PubMed] [Google Scholar]
- 31.Zuniga E, Montes C, Barbieri G, Gruppi A. Antibodies against Trypanosoma cruzi alkaline antigens are elicited in sera from acute but not chronic human chagasic patients. Clin Immunol. 1999;93:81–89. doi: 10.1006/clim.1999.4744. [DOI] [PubMed] [Google Scholar]
- 32.Acosta Rodriguez EV, Zuniga EI, Montes CL, Merino MC, Bermejo DA, et al. Trypanosoma cruzi infection beats the B-cell compartment favouring parasite establishment: can we strike first? Scand J Immunol. 2007;66:137–142. doi: 10.1111/j.1365-3083.2007.01968.x. [DOI] [PubMed] [Google Scholar]
- 33.de Meis J, Morrot A, Farias-de-Oliveira DA, Villa-Verde DM, Savino W. Differential regional immune response in Chagas disease. PLoS Negl Trop Dis. 2009;3(7):e417. doi: 10.1371/journal.pntd.0000417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Merino M, Montes C, Acosta-Rodriguez E, Bermejo D, Amezcua-Vesely M, et al. Peritoneum from Trypanosoma cruzi infected mice is a homing site of Syndecan-1neg plasma cells which mainly provide non-parasite specific antibodies. International Immunology. 2009 doi: 10.1093/intimm/dxq019. In Press. [DOI] [PubMed] [Google Scholar]
- 35.Gazzinelli R, Galvao LM, Dias JC, Gazzinelli G, Brener Z. Anti-laminin and specific antibodies in acute Chagas disease. Trans R Soc Trop Med Hyg. 1988;82:574–576. doi: 10.1016/0035-9203(88)90513-5. [DOI] [PubMed] [Google Scholar]
- 36.Spinella S, Liegeard P, Hontebeyrie-Joskowicz M. Trypanosoma cruzi: predominance of IgG2a in nonspecific humoral response during experimental Chagas' disease. Exp Parasitol. 1992;74:46–56. doi: 10.1016/0014-4894(92)90138-z. [DOI] [PubMed] [Google Scholar]
- 37.Milei J, Sanchez J, Storino R, Yu ZX, Denduchis B, et al. Antobodies to laminin and immunohistochemical localization of laminin in chronic chagasic cardiomyopathy: a review. Mol Cell Biochem. 1993;129(2):161–170. doi: 10.1007/BF00926364. [DOI] [PubMed] [Google Scholar]
- 38.Mackay F, Groom JR, Tangye SG. An important role for B-cell activation factor and B cells in the pathogenesis of Sjogren's syndrome. Curr Opin Rheumatol. 2007;19:406–413. doi: 10.1097/BOR.0b013e328277ef4c. [DOI] [PubMed] [Google Scholar]
- 39.He B, Qiao X, Klasse PJ, Chiu A, Chadburn A, et al. HIV-1 envelope triggers polyclonal Ig class switch recombination through a CD40-independent mechanism involving BAFF and C-type lectin receptors. J Immunol. 2006;176:3931–3941. doi: 10.4049/jimmunol.176.7.3931. [DOI] [PubMed] [Google Scholar]
- 40.Tarantino G, Marco VD, Petta S, Almasio PL, Barbaria F, et al. Serum BLyS/BAFF predicts the outcome of acute hepatitis C virus infection. J Viral Hepat. 2009;16:397–405. doi: 10.1111/j.1365-2893.2009.01093.x. [DOI] [PubMed] [Google Scholar]
- 41.Bogdan C, Rollinghoff M. How do protozoan parasites survive inside macrophages? Parasitol Today. 1999;15:22–28. doi: 10.1016/s0169-4758(98)01362-3. [DOI] [PubMed] [Google Scholar]
- 42.Van OL, Vanderheyde N, Verhasselt V, Ismaili J, De VL, et al. Trypanosoma cruzi infects human dendritic cells and prevents their maturation: inhibition of cytokines, HLA-DR, and costimulatory molecules. Infect Immun. 1999;67:4033–4040. doi: 10.1128/iai.67.8.4033-4040.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mackay F, Schneider P, Rennert P, Browning J. BAFF AND APRIL: a tutorial on B cell survival. Annu Rev Immunol. 2003;21:231–264. doi: 10.1146/annurev.immunol.21.120601.141152. [DOI] [PubMed] [Google Scholar]
- 44.Scapini P, Nardelli B, Nadali G, Calzetti F, Pizzolo G, et al. G-CSF-stimulated neutrophils are a prominent source of functional BLyS. J Exp Med. 2003;197:297–302. doi: 10.1084/jem.20021343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Boule MW, Broughton C, Mackay F, Akira S, Marshak-Rothstein A, et al. Toll-like receptor 9-dependent and -independent dendritic cell activation by chromatin-immunoglobulin G complexes. J Exp Med. 2004;199:1631–1640. doi: 10.1084/jem.20031942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Abrahamsohn IA. Cytokines in innate and acquired immunity to Trypanosoma cruzi infection. Braz J Med Biol Res. 1998;31:117–121. doi: 10.1590/s0100-879x1998000100015. [DOI] [PubMed] [Google Scholar]
- 47.Antunez MI, Cardoni RL. Early IFN-gamma production is related to the presence of interleukin (IL)-18 and the absence of IL-13 in experimental Trypanosoma cruzi infections. Immunol Lett. 2001;79:189–196. doi: 10.1016/s0165-2478(01)00283-8. [DOI] [PubMed] [Google Scholar]
- 48.Cuna WR, Encina JL, Cuna CR. Interferon- or interleukin-10 production is induced by related Trypanosoma cruzi antigens. J Parasitol. 2000;86:295–299. doi: 10.1645/0022-3395(2000)086[0295:IOIPII]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 49.Corral RS, Petray PB. CpG DNA as a Th1-promoting adjuvant in immunization against Trypanosoma cruzi. Vaccine. 2000;19:234–242. doi: 10.1016/s0264-410x(00)00172-9. [DOI] [PubMed] [Google Scholar]
- 50.Gazzinelli RT, Denkers EY. Protozoan encounters with Toll-like receptor signalling pathways: implications for host parasitism. Nat Rev Immunol. 2006;6:895–906. doi: 10.1038/nri1978. [DOI] [PubMed] [Google Scholar]
- 51.Meyer-Bahlburg A, Andrews SF, Yu KO, Porcelli SA, Rawlings DJ. Characterization of a late transitional B cell population highly sensitive to BAFF-mediated homeostatic proliferation. J Exp Med. 2008;205:155–168. doi: 10.1084/jem.20071088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rauch M, Tussiwand R, Bosco N, Rolink AG. Crucial role for BAFF-BAFF-R signaling in the survival and maintenance of mature B cells. PLoS One. 2009;4(5):e5456. doi: 10.1371/journal.pone.0005456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mackay F, Schneider P. Cracking the BAFF code. Nat Rev Immunol. 2009;9:491–502. doi: 10.1038/nri2572. [DOI] [PubMed] [Google Scholar]
- 54.Scholz JL, Crowley JE, Tomayko MM, Steinel N, O'Neill PJ, et al. BLyS inhibition eliminates primary B cells but leaves natural and acquired humoral immunity intact. Proc Natl Acad Sci U S A. 2008;105:15517–15522. doi: 10.1073/pnas.0807841105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Golgher D, Gazzinelli RT. Innate and acquired immunity in the pathogenesis of Chagas disease. Autoimmunity. 2004;37:399–409. doi: 10.1080/08916930410001713115. [DOI] [PubMed] [Google Scholar]
- 56.Kierszenbaum F. Views on the autoimmunity hypothesis for Chagas disease pathogenesis. FEMS Immunol Med Microbiol. 2003;37:1–11. doi: 10.1016/S0928-8244(03)00097-X. [DOI] [PubMed] [Google Scholar]
- 57.Tarleton RL. Chagas disease: a role for autoimmunity? Trends Parasitol. 2003;19:447–451. doi: 10.1016/j.pt.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 58.Malkiel S, Kuan AP, Diamond B. Autoimmunity in heart disease: mechanisms and genetic susceptibility. Mol Med Today. 1996;2:336–342. doi: 10.1016/1357-4310(96)81799-0. [DOI] [PubMed] [Google Scholar]
- 59.Dighiero G, Rose NR. Critical self-epitopes are key to the understanding of self-tolerance and autoimmunity. Immunol Today. 1999;20:423–428. doi: 10.1016/s0167-5699(99)01509-1. [DOI] [PubMed] [Google Scholar]
- 60.Talvani A, Ribeiro CS, Aliberti JC, Michailowsky V, Santos PV, et al. Kinetics of cytokine gene expression in experimental chagasic cardiomyopathy: tissue parasitism and endogenous IFN-gamma as important determinants of chemokine mRNA expression during infection with Trypanosoma cruzi. Microbes Infect. 2000;2:851–866. doi: 10.1016/s1286-4579(00)00388-9. [DOI] [PubMed] [Google Scholar]
- 61.Mackay F, Browning JL. BAFF: a fundamental survival factor for B cells. Nat Rev Immunol. 2002;2:465–475. doi: 10.1038/nri844. [DOI] [PubMed] [Google Scholar]
- 62.Ramanujam M, Davidson A. The current status of targeting BAFF/BLyS for autoimmune diseases. Arthritis Res Ther. 2004;6:197–202. doi: 10.1186/ar1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sutherland AP, Mackay F, Mackay CR. Targeting BAFF: immunomodulation for autoimmune diseases and lymphomas. Pharmacol Ther. 2006;112:774–786. doi: 10.1016/j.pharmthera.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 64.Zekavat G, Rostami SY, Badkerhanian A, Parsons RF, Koeberlein B, et al. In vivo BLyS/BAFF neutralization ameliorates islet-directed autoimmunity in nonobese diabetic mice. J Immunol. 2008;181:8133–8144. doi: 10.4049/jimmunol.181.11.8133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fletcher CA, Sutherland AP, Groom JR, Batten ML, Ng LG, et al. Development of nephritis but not sialadenitis in autoimmune-prone BAFF transgenic mice lacking marginal zone B cells. Eur J Immunol. 2006;36:2504–2514. doi: 10.1002/eji.200636270. [DOI] [PubMed] [Google Scholar]
- 66.Jacob CO, Pricop L, Putterman C, Koss MN, Liu Y, et al. Paucity of clinical disease despite serological autoimmunity and kidney pathology in lupus-prone New Zealand mixed 2328 mice deficient in BAFF. J Immunol. 2006;177:2671–2680. doi: 10.4049/jimmunol.177.4.2671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Stohl W, Xu D, Kim KS, Koss MN, Jorgensen TN, et al. BAFF overexpression and accelerated glomerular disease in mice with an incomplete genetic predisposition to systemic lupus erythematosus. Arthritis Rheum. 2005;52:2080–2091. doi: 10.1002/art.21138. [DOI] [PubMed] [Google Scholar]
- 68.Kayagaki N, Yan M, Seshasayee D, Wang H, Lee W, et al. BAFF/BLyS receptor 3 binds the B cell survival factor BAFF ligand through a discrete surface loop and promotes processing of NF-kappaB2. Immunity. 2002;17:515–524. doi: 10.1016/s1074-7613(02)00425-9. [DOI] [PubMed] [Google Scholar]
- 69.Herlands RA, William J, Hershberg U, Shlomchik MJ. Anti-chromatin antibodies drive in vivo antigen-specific activation and somatic hypermutation of rheumatoid factor B cells at extrafollicular sites. Eur J Immunol. 2007;37:3339–3351. doi: 10.1002/eji.200737752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hsu MC, Toellner KM, Vinuesa CG, Maclennan IC. B cell clones that sustain long-term plasmablast growth in T-independent extrafollicular antibody responses. Proc Natl Acad Sci U S A. 2006;103:5905–5910. doi: 10.1073/pnas.0601502103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Oliver AM, Martin F, Gartland GL, Carter RH, Kearney JF. Marginal zone B cells exhibit unique activation, proliferative and immunoglobulin secretory responses. Eur J Immunol. 1997;27:2366–2374. doi: 10.1002/eji.1830270935. [DOI] [PubMed] [Google Scholar]
- 72.Cardillo F, Postol E, Nihei J, Aroeira LS, Nomizo A, et al. B cells modulate T cells so as to favour T helper type 1 and CD8+ T-cell responses in the acute phase of Trypanosoma cruzi infection. Immunology. 2007;122:584–595. doi: 10.1111/j.1365-2567.2007.02677.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Immature and mature B cell number in non-infected or T. cruzi infected mice treated with BR3:Fc. Cells from spleen and bone marrow from non-infected (NI) or T. cruzi infected (day 15 p.i.) mice treated with physiological solution (I) or BR3:Fc (I+BR3:Fc) or IgG2a control (I+IgG2a) were obtained. Cells from spleen were stained with anti-B220, anti-IgD and anti-IgM, and cells from bone marrow were stained with anti-B220, anti-IgD and anti-CD24 and analyzed by flow cytometry. Graphs show the number of: A) B220+ IgD+IgM+ (mature B cells) and B220+IgD-IgM+ in spleen and B) B220+IgD+CD24+ (mature B cells) and B220+IgD-CD24hi (immature B cells) in bone marrow. Diamonds represent the value obtained from each mouse. The lines represent the media value. *, p<0.05. Results are representative for three individual experiments.
(0.58 MB TIF)