Abstract
Objective
To determine whether visual acuity improvement with Bangerter filters is similar to improvement with patching as initial therapy for children with moderate amblyopia.
Design
Randomized clinical trial.
Participants
186 children, 3 to <10 years old, with moderate amblyopia (20/40 to 20/80).
Methods
Children were randomly assigned to receive either daily patching or to use a Bangerter filter on the spectacle lens in front of the fellow eye. Study visits were scheduled at 6, 12, 18 and 24 weeks.
Main outcome measure
Visual acuity in amblyopic eye at 24 weeks.
Results
At 24 weeks, amblyopic eye improvement averaged 1.9 lines in the Bangerter group and 2.3 lines in the patching group (difference in mean visual acuities between groups adjusted for baseline acuity = 0.38 line). The upper limit of a 1-sided 95% confidence interval was 0.76 line, which slightly exceeded a pre-specified non-inferiority limit of < 0.75 line. Similar percentages of subjects in each group improved ≥3 lines (Bangerter group 38% versus patching group 35%, P=0.61) or had 20/25 or better amblyopic eye acuity (36% versus 31%, respectively, P=0.86). There was a lower treatment burden in the Bangerter group as measured with the Amblyopia Treatment Index. With Bangerter filters, neither a fixation switch to the amblyopic eye nor induced blurring in the fellow eye to worse than that of the amblyopic eye was required for visual acuity improvement.
Conclusion
Because the average difference in visual acuity improvement between Bangerter filters and patching was less than half a line, and there was lower burden of treatment on the child and family, Bangerter filter treatment is a reasonable option to consider for initial treatment of moderate amblyopia.
Although patching and atropine are well established as effective treatments for amblyopia1–3 Bangerter filters or foils (Ryser Optik AG, St. Gallen, Switzerland), placed on the spectacle lens of the fellow eye, have also been used. These transparent filters, available since the 1960s, were designed as a method to modulate the degree of deprivation from occlusion, by producing diffuse image defocus that degrades the fellow eye visual acuity to predicted levels.4, 5 Bangerter filters have been used mostly as secondary treatment following either patching or atropine.5, 6 The potential advantages of using Bangerter filters compared with patching include: the ability to change the density of the filter to modulate the degree of deprivation, the possibility of better compliance since the filter is applied to the glasses and not the skin, the possibility of higher parental and child acceptance since the filter is not readily apparent to casual observers, and the possibility that the filter may be less disruptive to binocular function. Potential disadvantages of the filters are that glasses must always be worn properly during treatment as peeking around the filters is relatively easy, and the filters may not uniformly degrade visual acuity to the predicted level reported by the manufacturer.
The effectiveness of the filters as primary treatment for amblyopia has not yet been rigorously studied. Iacobucci et al6 reported successful treatment in a small case series and Bonsall found similar improvement with patching and filters in a small, randomized trial (Bonsall, unpublished data). We designed a randomized trial to determine whether visual acuity improvement with Bangerter filters was similar to daily patching when initiating therapy for moderate amblyopia in children ages 3 to less than 10 years.
Methods
The study was supported through a cooperative agreement with the National Eye Institute of the National Institutes of Health and was conducted by the Pediatric Eye Disease Investigator Group (PEDIG) at 39 clinical sites. The protocol and Health Insurance Portability and Accountability Act (HIPAA) compliant informed consent forms were approved by institutional review boards, and a parent or guardian (referred to subsequently as “parent”) of each study subject gave written informed consent. The subject gave assent as required. Study oversight was provided by an independent data and safety monitoring committee. The study is listed on www.clinicaltrials.gov, under identifier NCT00525174 (accessed September 10, 2009). The protocol, which is available on the PEDIG website (www.pedig.net, accessed September 10, 2009), is summarized below.
Synopsis of Study Design
Screening/Eligibility
At baseline, visual acuity was measured in each eye, without cycloplegia using optimal spectacle correction, by a study-certified examiner using either the Amblyopia Treatment Study single–surround HOTV protocol (ATS-HOTV) for children aged 3 to < 7 years7 or the Electronic Early Treatment Diabetic Retinopathy Study (E-ETDRS) protocol for subjects aged 7 to < 10 years.8 Additional testing at enrollment included an ocular examination; a cycloplegic refraction using cyclopentolate 1%; measurement of ocular alignment with a simultaneous prism and cover test (SPCT) at distance and near; assessment of binocularity with the Randot Preschool Stereoacuity Test (Stereo Optical Co., Chicago, IL); fixation preference with and without a Bangerter filter; and the fellow eye visual acuity through a Bangerter filter.
Major eligibility criteria for the trial included the following: age 3 to <10 years, visual acuity in the amblyopic eye 20/40 – 20/80 (54–71 letters if E-ETDRS used), fellow eye visual acuity 20/40 or better (≥69 letters if E-ETDRS used), inter-ocular acuity difference ≥3 lines (≥15 letters if E-ETDRS used), and the presence of or a history of an amblyogenic factor meeting study-specified criteria for strabismus and/or anisometropia. In addition, all subjects had to be currently wearing spectacles. Spectacles had to provide optimal correction for a minimum of 16 weeks or until stability of visual acuity was documented (no improvement in amblyopic eye visual acuity at 2 consecutive visits at least 4 weeks apart). Exclusion criteria included myopia >6.00 D spherical equivalent in either eye, treatment for amblyopia (other than spectacle correction) within the 6 months prior to enrollment, or inability to complete either the ATS- HOTV test (3 to < 7 years old) or the E-ETDRS test (7 to < 10 years old). A complete list of eligibility and exclusion criteria is listed in Table 1 (available at http://aaojournal.org).
Table 1.
Eligibility and Exclusion Criteria
Eligibility Criteria
|
Exclusion Criteria
|
D = diopters; ATS = Amblyopia Treatment Study; E-ETDRS = Electronic Early Treatment of Diabetic Retinopathy; logMAR = logarithm of the minimum angle of resolution.
Randomization
Each subject was randomly assigned with equal probability, using a permutated block design stratified by age group (3 to < 7 years and 7 to <10 years) and site, to receive either daily patching or a Bangerter filter over the fellow eye spectacle lens.
Follow-up Visits
Follow-up visits were conducted at 6, 12, 18, and 24 weeks (± 2 weeks), with the 24-week visit specified as the primary outcome visit. At each visit, visual acuity was measured in each eye by a study-certified examiner using the same testing protocol used at enrollment (ATS-HOTV or E-ETDRS). The examiner was masked to treatment group at the 24-week visit. The fellow eye visual acuity was evaluated through a Bangerter filter for all subjects at baseline and for subjects randomized to the Bangerter filter group at follow-up visits using the previously prescribed Bangerter filter. Ocular alignment was assessed at each visit and stereoacuity was measured at the 24-week outcome visit using the Randot Preschool Stereoacuity Test (Stereo Optical Co., Chicago, IL).
Treatment
Subjects in the patching group initially were assigned 2 hours of daily patching (Coverlet/3M Opticlude/Ortopad). Subjects assigned to the Bangerter group had a Bangerter filter density of 0.3 (for 20/40 to 20/63 amblyopic visual acuity) or 0.2 (for 20/80 amblyopic acuity) placed on the spectacle lens over the fellow eye, and the spectacles were to be worn full-time. A Grade-Level Reading Assessment Test was administered to subjects ≥7 years old to ensure that they could read grade–appropriate text while using the filter (all subjects could). At each follow-up visit, children in the Bangerter group received a new filter. In both groups, parents were instructed to have their child spend at least one hour each day performing near activities while wearing the Bangerter filter or during patching.
A refraction was performed and new spectacles prescribed if indicated at the 12-week visit when amblyopic eye acuity had not improved from baseline by at least one line. If the refraction was unchanged, then the treatment intensity was increased to 6 hours of patching a day in the patching group or to a higher density filter in the Bangerter group (0.2 density filter for subjects using the 0.3 filter and 0.1 for subjects using the 0.2 filter.) At the 18-week visit if visual acuity had not improved ≥ 2 lines from baseline and treatment had not been increased at the 12-week visit, treatment was increased similarly. If Bangerter filter density was increased during the study, subjects again had a reading test and were given glasses without a filter for school work when needed.
Parents recorded the child’s level of compliance with the treatment and spectacle use on calendars, which were returned at each visit. Investigators judged compliance as excellent (76%–100%), good (51%–75%), fair (26%–50%) or poor (≤25%) based on the calendars and conversations with the child’s parent at each visit. At each visit, the parent was queried about any potential side effects of treatment. At the 6- and 24-week visits, parents completed the Amblyopia Treatment Index questionnaire,9, 10 consisting of 18 Likert-type questions with five choices ranging from “strongly agree” to “strongly disagree,” that evaluate the impact of treatment on the child and family using predefined subscales consisting of adverse effects, compliance, and social stigma.
Statistical Methods
The trial was designed as a non-inferiority study. The sample size was computed to be 170 subjects to have 90% power and a type 1 error rate of 5% for a non-inferiority limit of 0.075 logarithm of the minimum angle of resolution (logMAR), equivalent to 0.75 line, based on the following assumptions from prior PEDIG studies:1, 11–13 a standard deviation of 24-week visual acuity scores of 0.16 logMAR, a correlation between baseline and final acuities of 0.20, and 10% non-completion of the study primary outcome examination.
The primary outcome measure was the masked 24-week amblyopic eye visual acuity score. An analysis of covariance (ANCOVA) model, in which the logMAR acuity scores were adjusted for baseline amblyopic eye acuity, was used to compute the upper limit of a 1-sided 95% confidence interval constructed on the difference between adjusted mean visual acuity scores for both treatment groups. If the upper limit of this 95% confidence interval was less than the pre-determined non-inferiority limit, the conclusion of the primary outcome would be that Bangerter filters are non-inferior to patching. To be included in the primary analysis, the 24-week exam must have been completed between 20 and 28 weeks (inclusive).
Secondary analyses were conducted using logistic regression for the following 24-week success definitions: amblyopic visual acuity 20/25 or better, amblyopic eye acuity improvement ≥3 lines (≥15 letters for E-ETDRS testing) from baseline, and amblyopic eye acuity within one line (≤ +4 letters for E-ETDRS testing) of the fellow eye or better. One subject in the patching group who was treated with a Bangerter filter was considered a failure in these analyses. A similar analysis (posthoc) was performed comparing the proportions of patients in each group who had no improvement or worsening in amblyopic eye acuity from baseline to 24 weeks (change from baseline ≤+4 letters for E-ETDRS testing).
Methods used to analyze the amblyopic eye acuity scores in subgroups and at the 6, 12, and 18-week visits paralleled the analysis conducted on the 24-week outcome visit data. In addition the treatment group difference in the rate of improvement was evaluated using a population averaged linear mixed model after performing an inverse transformation of time to obtain linearity14 and in the time to first achieve 20/25 or better acuity was evaluated using a Cox proportional hazard model.15
In the Bangerter filter group, the association of fixation preference while the Bangerter filter was over the fellow eye at baseline (amblyopic eye, fellow eye, alternates) with 24-week amblyopic eye acuity was evaluated in an ANCOVA model. Similarly, the relationship between the fellow eye blur from the Bangerter filter at baseline and amblyopic improvement at the 24-week outcome was evaluated with an ANCOVA model with the acuity in the fellow eye being categorized as better than versus equal to or worse than the acuity in the amblyopic eye.
A treatment group difference in the fellow eye visual acuity at 24 weeks was evaluated in an ANCOVA model, adjusted for the baseline fellow eye acuity. Wilcoxon rank sum tests were used to evaluate change in Randot Preschool stereoacuity levels (from baseline to the 24-week outcome examination) by treatment group and t-tests were used to evaluate the parent questionnaire at 6 weeks and at 24 weeks by treatment group using overall and individual subscale scores.
Analyses followed the intent-to-treat principle and were conducted using SAS Version 9.1 (SAS Institute, Cary, NC).
Results
Baseline Characteristics
Between November 2007 and July 2008, 39 sites enrolled 186 subjects (average age 6.3 years), with 89 randomized to the Bangerter group and 97 to the patching group. The cause of amblyopia was strabismus in 27%, anisometropia in 44%, and a combination of strabismus and anisometropia in 30%. Table 2 provides the baseline characteristics according to treatment group.
Table 2.
Baseline Data According to Treatment Group
| Bangerter (N=89) | Patching (N=97) | |
|---|---|---|
| n (%) | n (%) | |
| Gender: Female | 36 (40%) | 48 (49%) |
| Race/Ethnicity | ||
| White | 69 (78%) | 67 (69%) |
| African-American | 1 (1%) | 13 (13%) |
| Hispanic or Latino | 15 (17%) | 11 (11%) |
| Asian | 0 | 3 (3%) |
| More than one race | 3 (3%) | 2 (2%) |
| Unknown/Not reported | 1 (1%) | 1 (1%) |
| Age at Enrollment | ||
| 7 to <10years | 32 (36%) | 35 (36%) |
| Mean (SD) | 6.3 (1.67) | 6.3 (1.62) |
| Prior Treatment for Amblyopia at Enrollment | ||
| None | 72 (81%) | 83 (86%) |
| Patching | 5 (6%) | 8 (8%) |
| Atropine | 3 (3%) | 2 (2%) |
| Patching and Atropine | 9 (10%) | 4 (4%) |
| Cause of Amblyopia | ||
| Strabismus | 23 (26%) | 27 (28%) |
| Anisometropia | 39 (44%) | 42 (43%) |
| Strabismus and anisometropia | 27 (30%) | 28 (29%) |
| Distance Visual Acuity in Amblyopic Eye | ||
| 20/80 (0.62 to 0.56 logMAR) | 16 (18%) | 23 (24%) |
| 20/63 (0.54 to 0.46 logMAR) | 27 (30%) | 31 (32%) |
| 20/50 (0.44 to 0.36 logMAR) | 24 (27%) | 22 (23%) |
| 20/40 (0.34 to 0.28 logMAR) | 22 (25%) | 21 (22%) |
| Mean (SD) logMAR | 0.44 (0.10) | 0.46 (0.10) |
| Distance Visual Acuity in Fellow Eye | ||
| 20/40 (0.32 to 0.26 logMAR) | 3 (3%) | 2 (2%) |
| 20/32 (0.24 to 0.16 logMAR) | 9 (10%) | 16 (16%) |
| 20/25 (0.14 to 0.06 logMAR) | 19 (21%) | 17 (18%) |
| 20/20 (0.04 to −0.04 logMAR) | 40 (45%) | 42 (43%) |
| 20/16 (−0.06 to −0.14 logMAR) | 18 (20%) | 20 (21%) |
| Mean (SD) logMAR | 0.03 (0.10) | 0.04 (0.10) |
| Intereye Acuity Difference | ||
| Mean (SD) lines | 4.1 (1.1) | 4.2 (1.1) |
| Spherical Equivalent in Amblyopic Eye | ||
| <0.00D | 8 (9%) | 3 (3%) |
| 0 to < +1.00D | 2 (2%) | 2 (2%) |
| +1.00 to <+2.00D | 1 (1%) | 8 (8%) |
| +2.00 to <+3.00D | 10 (11%) | 6 (6%) |
| +3.00 to <+4.00D | 13 (15%) | 10 (10%) |
| ≥+4.00D | 55 (62%) | 68 (70%) |
| Mean (SD) Sph Equivalent | +4.15 (2.57) | +4.41 (2.21) |
| Spherical Equivalent in Fellow Eye | ||
| <0.00D | 5 (6%) | 1 (1%) |
| 0 to < +1.00D | 16 (18%) | 18 (19%) |
| +1.00 to <+2.00D | 21 (24%) | 25 (26%) |
| +2.00 to <+3.00D | 12 (13%) | 13 (13%) |
| +3.00 to <+4.00D | 13 (15%) | 8 (8%) |
| ≥+4.00D | 22 (25%) | 32 (33%) |
| Mean (SD) Sph Equivalent | +2.49 (2.13) | +2.81 (2.14) |
SD = standard deviation; logMAR = logarithm of the minimum angle of resolution; D = diopters; Sph Equivalent = spherical equivalent.
Visit Completion
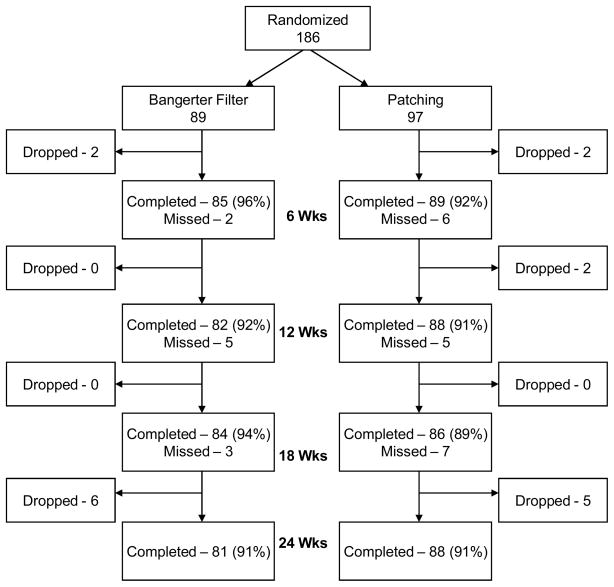
The 24-week primary outcome exam was completed by 81 of 89 (91%) subjects in the Bangerter group and 88 of 97 (91%) subjects in the patching group (Figure 1). The vision tester was masked to treatment group for 96% of these examinations (95% in the Bangerter group and 98% in the patching group). Visit completion rates were similar between the two treatment groups at the 6, 12, and 18-week exams (Figure 1).
Figure 1. Visit Completion by Treatment Group.
Flow chart showing study completion in each treatment group.
Treatment
In the Bangerter group, spectacles were changed at the 12-week or 18-week visit in 14 (16%) subjects. The density of the filter was increased in 14 (16%) subjects at the 12-week visit and in 29 (33%) at the 18-week visit (in 3 of these subjects the filter density was increased even though amblyopic eye acuity had improved, Table 3 (available at http://aaojournal.org). Adherence with the prescribed regimen using the Bangerter filter over follow-up was judged by the investigator to be excellent in 88%, good in 8%, fair in 4%, and poor in 1% of subjects, and adherence with wearing spectacles over follow-up was judged by the investigator to be excellent in 90%, good in 6%, and fair in 4% of subjects.
Table 3.
Treatment Prescribed over Follow-up
| Bangerter N=89 | Patching N=97 | |
|---|---|---|
| Treatment Per Protocol | ||
| No change in assigned treatment intensity | 46 (52%) | 62 (64%) |
| Increased treatment intensity* | 40 (45%) | 26 (27%) |
| 12 weeks | 12 (14%) | 5 (5%) |
| 18 weeks | 28 (31%) | 21 (22%) |
| Treatment Not Per Protocol | 3 (3%) | 9 (9%) |
| Treatment increased when amblyopic eye acuity improved† | 3 | 2 |
| Treatment not increased when amblyopic eye acuity was improved not | 0 | 6 |
| Crossover** | 0 | 1 |
Increase density of the filter in the Bangerter group and increased patching hours in the patching group
Four subjects increased treatment intensity at 12 weeks (2 Bangerter and 2 patching) and one Bangerter subject increased treatment intensity at 18 weeks.
Switched to Bangerter filter immediately following randomization
In the patching group, spectacles were changed at either the 12-week or 18-week visit in 11 (11%) subjects. Patching was increased to 6 hours per day for 7 (7%) subjects at the 12-week visit and 21 (22%) at the 18-week visit (in 2 of these subjects patching was increased even though amblyopic eye acuity had improved and in 6 additional subjects, patching hours were not increased even though visual acuity had not improved, Table 3 (available at http://aaojournal.org). Adherence with the prescribed patching was judged by the investigator to be excellent in 82%, good in 14%, fair in 3%, and poor in 1% of subjects, and adherence with wearing spectacles over follow-up was judged to be excellent in 94% and good in 6% of subjects.
Amblyopic Eye Visual Acuity
At 24 weeks, visual acuity was improved from baseline by an average of 1.9 lines in the Bangerter group and 2.3 lines in the patching group (Table 4). The mean difference between groups adjusted for baseline acuity was 0.38 line favoring the patching group. The upper limit of the 1-sided 95% confidence interval was computed to be 0.76 line, which exceeded the predefined upper limit of non-inferiority of 0.75 line. However, patching was not statistically superior to Bangerter treatment (95% confidence interval for difference between groups = −0.06 to +0.83 line, p = 0.09). Results of exploratory subgroup analyses are shown in Table 5 (available at http://aaojournal.org).
Table 4.
Visual Acuity in the Amblyopic Eye at Each Study Visit
| 6-Week Exam | 12-Week Exam | 18-Week Exam | 24-Week Exam | |||||
|---|---|---|---|---|---|---|---|---|
| Bangerter N=85 n (%) | Patching N=89 n (%) | Bangerter N=82 n (%) | Patching N=88 n (%) | Bangerter N=84 n (%) | Patching N=86 n (%) | Bangerter N=81 n (%) | Patching N=88 n (%) | |
| Distribution of Visual Acuity* | ||||||||
| 20/125 | 0 | 1 (1%) | 1 (1%) | 0 | 0 | 0 | 1 (1%) | 0 |
| 20/100 | 2 (2%) | 0 | 0 | 1 (1%) | 3 (4%) | 1 (1%) | 3 (4%) | 0 |
| 20/80 | 6 (7%) | 4 (4%) | 5 (6%) | 0 | 2 (2%) | 3 (3%) | 3 (4%) | 1 (1%) |
| 20/63 | 7 (8%) | 18 (20%) | 9 (11%) | 8 (9%) | 7 (8%) | 7 (8%) | 7 (9%) | 8 (9%) |
| 20/50 | 17 (20%) | 14 (16%) | 8 (10%) | 14 (16%) | 8 (10%) | 9 (10%) | 5 (6%) | 12 (14%) |
| 20/40 | 28 (33%) | 21 (24%) | 18 (22%) | 16 (18%) | 25 (30%) | 16 (19%) | 19 (23%) | 19 (22%) |
| 20/32 | 20 (24%) | 20 (22%) | 24 (29%) | 24 (27%) | 15 (18%) | 18 (21%) | 14 (17%) | 20 (23%) |
| 20/25 | 4 (5%) | 7 (8%) | 13 (16%) | 16 (18%) | 18 (21%) | 19 (22%) | 20 (25%) | 17 (19%) |
| 20/20 | 1 (1%) | 4 (4%) | 4 (5%) | 8 (9%) | 5 (6%) | 12 (14%) | 9 (11%) | 7 (8%) |
| 20/16 | 0 | 0 | 0 | 1 (1%) | 1 (1%) | 1 (1%) | 0 | 4 (5%) |
| Mean (SD) logMAR | 0.33 (0.14) | 0.32 (0.16) | 0.28 (0.17) | 0.25 (0.16) | 0.26 (0.17) | 0.23 (0.17) | 0.25 (0.19) | 0.23 (0.16) |
| Snellen Equivalent | 20/40−1 | 20/40−1 | 20/40+1 | 20/32−2 | 20/40+2 | 20/32−1 | 20/32−2 | 20/32−1 |
| Change from Baseline* | ||||||||
| ≥3 lines worse | 0 | 0 | 1 (1%) | 0 | 1 (1%) | 0 | 1 (1%) | 0 |
| 2 lines worse | 1 (1%) | 1 (1%) | 1 (1%) | 0 | 0 | 0 | 2 (2%) | 0 |
| 1 line worse | 7 (8%) | 1 (1%) | 3 (4%) | 2 (2%) | 3 (4%) | 2 (2%) | 5 (6%) | 1 (1%) |
| 0 lines | 15 (18%) | 15 (17%) | 11 (13%) | 4 (5%) | 10 (12%) | 6 (7%) | 8 (10%) | 4 (5%) |
| 1 line better | 33 (39%) | 31 (35%) | 22 (27%) | 18 (20%) | 19 (23%) | 19 (22%) | 12 (15%) | 19 (22%) |
| 2 lines better | 21 (25%) | 27 (30%) | 18 (22%) | 29 (33%) | 25 (30%) | 20 (23%) | 20 (25%) | 27 (31%) |
| ≥3 lines better | 8 (9%) | 14 (16%) | 26 (32%) | 35 (40%) | 26 (31%) | 39 (45%) | 33 (41%) | 37 (42%) |
| Mean (SD) Lines change | 1.1 (1.2) | 1.4 (1.1) | 1.6 (1.4) | 2.1 (1.2) | 1.8 (1.4) | 2.3 (1.4) | 1.9 (1.6) | 2.3 (1.3) |
| Proportion 20/25 or better (78 or more letters) | 5 (6%) | 11 (12%) | 17 (21%) | 25 (28%) | 24 (29%) | 32 (37%) | 29 (36%) | 28 (32%) |
| Mean (SD) IOD (Lines) | 2.9 (1.4) | 2.9 (1.6) | 2.4 (1.9) | 2.3 (1.6) | 2.4 (1.8) | 2.2 (1.7) | 2.3 (2.0) | 2.3 (1.5) |
| Proportion IOD < 1 line (resolved) | 2 (2%) | 3 (3%) | 13 (16%) | 12 (14%) | 12 (14%) | 13 (15%) | 15 (19%) | 11 (13%) |
logMAR = logarithm of the minimum angle of resolution; SD = standard deviation; IOD = inter-ocular difference
Values are rounded to nearest logMAR line.
Table 5.
Change in Visual Acuity in the Amblyopic Eye at 24-week Outcome Examination According to Baseline Patient Characteristics
| Bangerter N=81 | Patching N=88 | |||
|---|---|---|---|---|
| n | Mean Change in Lines (SD) | n | Mean Change in Lines (SD) | |
| Sex | ||||
| Female | 34 | 2.1 (1.7) | 43 | 2.4 (1.3) |
| Male | 47 | 1.7 (1.6) | 45 | 2.2 (1.3) |
| Race/Ethnicity* | ||||
| White, non-Hispanic | 63 | 1.8 (1.7) | 61 | 2.3 (1.3) |
| Non-white or Hispanic | 17 | 2.1 (1.4) | 26 | 2.4 (1.3) |
| Age at Enrollment | ||||
| 3 to <5 years | 21 | 2.1 (1.9) | 23 | 2.7 (1.4) |
| 5 to <7 years | 31 | 2.1 (1.7) | 34 | 2.5 (1.2) |
| 7 to <10years | 29 | 1.5 (1.3) | 31 | 1.8 (1.2) |
| Prior Treatment for Amblyopia at Enrollment | ||||
| No | 65 | 1.9 (1.7) | 75 | 2.4 (1.3) |
| Yes | 16 | 2.0 (1.4) | 13 | 1.7 (1.0) |
| Cause of Amblyopia | ||||
| Strabismus | 21 | 2.2 (1.5) | 23 | 2.4 (1.3) |
| Anisometropia | 36 | 1.5 (1.7) | 39 | 2.4 (1.4) |
| Strabismus and anisometropia | 24 | 2.2 (1.5) | 26 | 2.1 (1.2) |
| Distance Visual Acuity in Amblyopic Eye at Baseline | ||||
| 20/80 (53 to 57 letters) | 15 | 2.3 (2.0) | 22 | 2.3 (1.3) |
| 20/63 (58 to 62 letters) | 25 | 1.8 (1.7) | 29 | 2.5 (1.5) |
| 20/50 (63 to 67 letters) | 20 | 1.7 (1.7) | 17 | 2.3 (1.4) |
| 20/40 (68 to 72 letters) | 21 | 1.9 (1.0) | 20 | 2.0 (1.1) |
SD = standard deviation.
Two subjects (one in each treatment group) were excluded due to Unknown/Not reported ethnicity classification
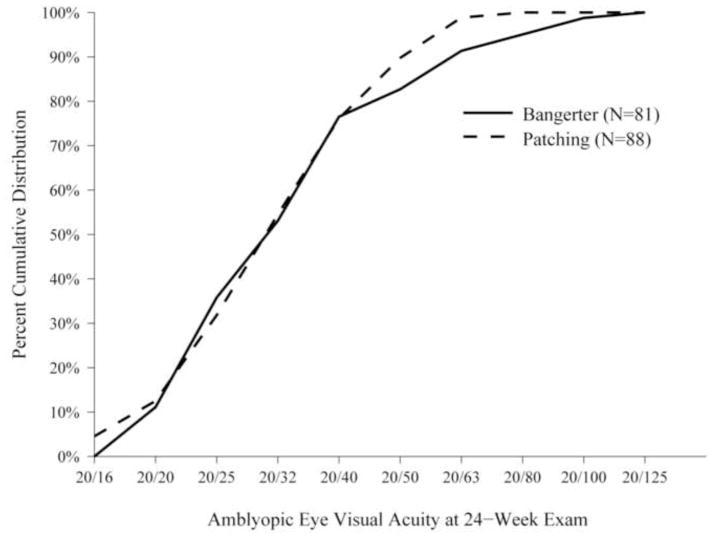
Five subjects in the Bangerter group had acuity ≥1 line worse at 24 weeks than at baseline and 13 had the same acuity at both time points compared with 1 and 7, respectively in the patching group (P=0.02 for difference in proportions of subjects not improved between treatment groups adjusting for baseline acuity). This is reflected in Figure 2 by noting that a few more subjects in the Bangerter group than patching group had 24-week amblyopic eye acuity of 20/63 or worse.
Figure 2. Cumulative Distribution of Visual Acuity at 24-week Masked Exam.
Cumulative distribution of amblyopic eye visual acuity scores at 24-week outcome exam according to treatment group.
For the pre-specified secondary 24-week outcomes, 20/25 or better amblyopic eye acuity was achieved by 29 subjects (36%) in the Bangerter group and 27 subjects (31%) in the patching group (P=0.86); ≥3 lines improvement occurred in 31 subjects (38%) and 31 subjects (35%) in the two groups, respectively (P=0.61); and an inter-ocular difference < 1 line was present in 15 (19%) and 10 (11%), respectively (P=0.27). The rate of amblyopic eye improvement (Figure 3) and time to 20/25 or better amblyopic eye acuity were not statistically different between treatment groups (p=0.20 and 0.28, respectively).
Figure 3. Mean Visual Acuity in Amblyopic Eyes from Baseline to 24 Weeks.
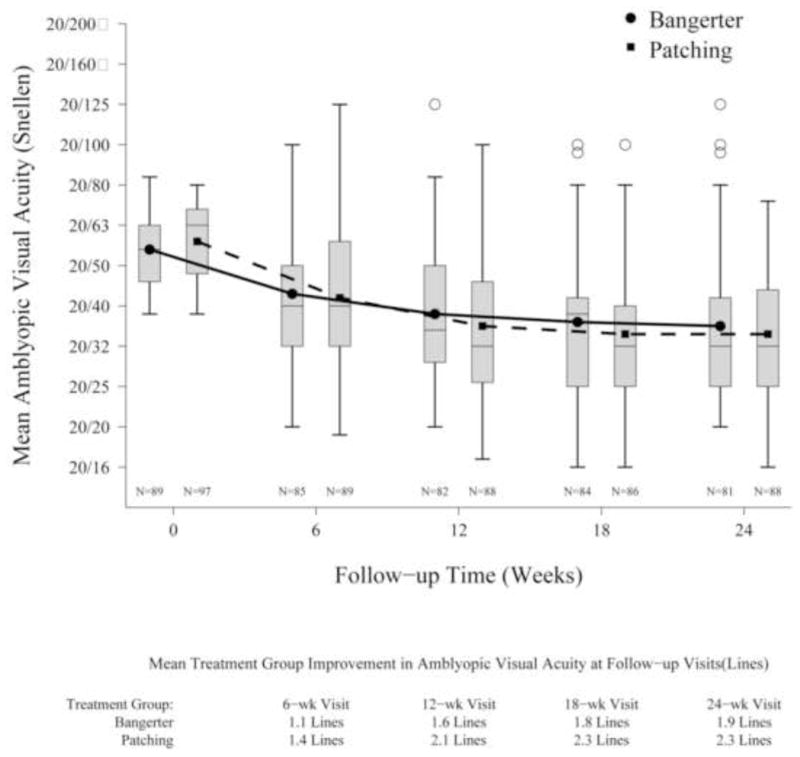
At each time point, the box on the left is the distribution of amblyopic eye visual acuity scores for the Bangerter group and the one on the right represents the patching group. The top and bottom of each box represents the 25th and 75th percentiles of the data and the line in the box is the median. The treatment group means are represented by a dot (Bangerter) or a square (patching) and are connected across the visits with lines. The bars extending above and below each box represent 1.5 times the interquartile range (difference between the 25th and 75th percentiles), and the open circles are outlier values.
Factors Predictive of Improvement in Bangerter Group
Mean visual acuity improvement from baseline to 24 weeks was 1.8 lines in the 53 subjects whose fellow eye acuity with the Bangerter filter at enrollment was equal to or worse than the amblyopic eye and 2.1 lines in the 28 subjects with the fellow eye acuity still better than the amblyopic eye (P=0.49). However, variability in the degree of the fellow eye degradation induced by the Bangerter filter at baseline was evident as only 111 (60%) of 186 enrolled children were blurred within 1 line of the predicted manufacturer’s visual acuity. Similarly, with baseline fixation preference testing while the filter was in front of the fellow eye, mean acuity improvement was 1.6 lines when the amblyopic eye was preferred (n=20), 1.7 lines when the fellow eye was preferred (n=33), and 2.3 lines when fixation preference alternated (n=28), (P=0.21).
Amblyopia Treatment Index
The Parental Amblyopia Treatment Index was completed by 79 of 89 (89%) in the Bangerter group and by 81 of 97 (84%) of the parents in the patching group at the 6-week visit and by 75 of 89 (84%) and 75 of 97 (77%), respectively, at the 24-week visit (Table 6, available at http://aaojournal.org). Overall, the negative impact of treatment was less among the Bangerter group compared to the patching group at both the 6-week visit (2.1 versus 2.3, P=0.03) and at the 24-week visit (1.9 versus 2.3, P<0.001). Questionnaire scores on the adverse effects subscale were similar between treatment groups at 6 weeks (mean = 2.2 versus 2.2, P=0.90), but favored the Bangerter group at 24 weeks (mean = 1.9 versus 2.2, P=0.01). Questionnaire scores for the compliance subscale were not significantly different at 6 weeks (mean = 2.3 versus 2.5, P=0.12), but favored the Bangerter group at 24 weeks (mean= 2.1 versus 2.6, P=0.001). The questionnaire scores favored the Bangerter group at both time points on the social stigma treatment subscale (at 6 weeks, mean = 1.7 versus 2.4, P<0.001, and at 24 weeks, mean = 1.6 versus 2.4, P<0.001).
Table 6.
Parent Amblyopia Treatment Index Response at 24-week Outcome Examination (Higher scores reflect negative impact of treatment)
| Bangerter N=75 (Mean = 1.9) | Patching N=75 (Mean = 2.3) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Strongly Disagree |
Disagree | Neither Agree nor Disagree |
Agree | Strongly Agree |
Bangerter Avg. Response |
Patching Avg. Response |
Strongly Disagree |
Disagree | Neither Agree nor Disagree |
Agree | Strongly Agree |
||
| 1 | 2 | 3 | 4 | 5 | (1–5) | (1–5) | 1 | 2 | 3 | 4 | 5 | ||
| Item (abbreviated) | % | % | |||||||||||
| 1 Child seems to mind treatment | 56 | 27 | 4 | 12 | 1 | 1.8 | 2.4 | 15 | 56 | 7 | 19 | 4 | |
| 2 Worry child may miss out on fun activities | 41 | 51 | 4 | 1 | 3 | 1.7 | 2.0 | 31 | 48 | 16 | 4 | 1 | |
| 3 Treatment affects child’s learning | 37 | 41 | 12 | 8 | 1 | 1.9 | 1.8 | 37 | 49 | 9 | 4 | 0 | |
| 4 Treatment makes it hard for child to play | 40 | 45 | 4 | 9 | 1 | 1.9 | 2.5 | 19 | 44 | 16 | 16 | 5 | |
| 5 Trouble applying treatment to child | 52 | 28 | 8 | 12 | 0 | 1.8 | 2.3 | 29 | 37 | 12 | 17 | 4 | |
| 6 Treatment is a source of tension for me | |||||||||||||
| a. with child | 55 | 32 | 1 | 12 | 0 | 1.7 | 2.2 | 33 | 39 | 11 | 13 | 4 | |
| b. with another family member* | 55 | 38 | 5 | 1 | 0 | 1.5 | 1.8 | 36 | 49 | 12 | 3 | 0 | |
| c. with my child’s teacher** | 53 | 37 | 7 | 1 | 1 | 1.6 | 1.8 | 30 | 58 | 11 | 0 | 0 | |
| 7 Difficult for child to draw, color, or write | 33 | 40 | 13 | 12 | 1 | 2.1 | 2.4 | 20 | 44 | 16 | 17 | 3 | |
| 8 Worry child will be injured on treatment | 48 | 43 | 5 | 4 | 0 | 1.7 | 1.9 | 31 | 55 | 7 | 8 | 0 | |
| 9 My child cannot see well while on treatment | 27 | 44 | 21 | 7 | 1 | 2.1 | 2.6 | 9 | 47 | 19 | 25 | 0 | |
| 10 Child complains when it is time for treatment | 41 | 29 | 8 | 17 | 4 | 2.1 | 3.3 | 13 | 16 | 17 | 39 | 15 | |
| 11 Worry that child not getting enough treatment | 47 | 32 | 8 | 11 | 3 | 1.9 | 2.7 | 9 | 48 | 15 | 23 | 5 | |
| 12 Child clumsy on treatment | 37 | 39 | 12 | 11 | 1 | 2.0 | 2.2 | 17 | 56 | 13 | 13 | 0 | |
| 13 Other children stare at child | 49 | 44 | 4 | 3 | 0 | 1.6 | 2.6 | 12 | 44 | 23 | 15 | 7 | |
| 14 Treatment will not improve my child’s vision | 44 | 44 | 8 | 1 | 3 | 1.7 | 1.7 | 48 | 43 | 5 | 3 | 1 | |
| 15 Treatment makes it difficult for child to play | 44 | 40 | 7 | 7 | 3 | 1.8 | 2.1 | 21 | 57 | 13 | 7 | 1 | |
| 16 Sometimes forget to apply treatment to child | 55 | 33 | 4 | 8 | 0 | 1.7 | 2.9 | 9 | 40 | 3 | 47 | 1 | |
| 17 Worry that child feels different | 48 | 40 | 7 | 5 | 0 | 1.7 | 2.3 | 17 | 55 | 13 | 13 | 1 | |
| 18 Notice child peeking over filter/pulling off patch | 13 | 19 | 12 | 37 | 19 | 3.3 | 2.6 | 15 | 48 | 8 | 21 | 8 | |
“not applicable” responses appeared on 9 questionnaires (1 Bangerter and 8 Patching)
“not applicable” responses appeared on 29 questionnaires (7 Bangerter and 22 Patching)
Stereoacuity
There was no difference between treatment groups in Randot Preschool Stereoacuity scores at the 24-week outcome relative to baseline either overall or among those with anisometropic amblyopia (P=0.90 and P=0.88, respectively Table 7 (available at http://aaojournal.org).
Table 7.
Randot Preschool Stereoacuity at Baseline and at the 24-week Outcome Exam by Treatment Group All Subjects
| All Subjects | ||||
|---|---|---|---|---|
| Randot Preschool | Baseline | 24 Weeks | ||
| Stereoacuity (arc second) | Bangerter (N=89) | Patching (N=97) | Bangerter (N=81) | Patching (N=87) |
| Failed pretest | 6 (7%) | 6 (6%) | 2 (2%) | 2 (2%) |
| >800 | 45 (51%) | 45 (46%) | 40 (49%) | 36 (41%) |
| 800 | 11 (12%) | 8 (8%) | 6 (7%) | 10 (11%) |
| 400 | 10 (11%) | 7 (7%) | 4 (5%) | 11 (13%) |
| 200 | 9 (10%) | 11 (11%) | 15 (19%) | 12 (14%) |
| 100 | 5 (6%) | 12 (12%) | 9 (11%) | 9 (10%) |
| 60 | 3 (3%) | 6 (6%) | 3 (4%) | 4 (5%) |
| 40 | 0 | 2 (2%) | 2 (2%) | 3 (3%) |
| Change in Stereoacuity (Levels) | Treatment Group | |
|---|---|---|
| Bangerter (N=76) | Patching (N=80) | |
| 2 or more levels improved | 12 (16%) | 15 (19%) |
| Within 1 level | 61 (80%) | 58 (73%) |
| 2 or more levels worsened | 3 (4%) | 7 (9%) |
| Subjects with Anisometropia and No Strabismus* | ||||
|---|---|---|---|---|
| Randot Preschool | Baseline | 24 Weeks | ||
| Stereoacuity (arc second) | Bangerter (N=39) | Patching (N=42) | Bangerter (N=36) | Patching (N=38) |
| Failed pretest | 5 (13%) | 3 (7%) | 1 (3%) | 1 (3%) |
| >800 | 13 (33%) | 9 (21%) | 10 (28%) | 6 (16%) |
| 800 | 3 (8%) | 2 (5%) | 2 (6%) | 2 (5%) |
| 400 | 6 (15%) | 5 (12%) | 2 (6%) | 5 (13%) |
| 200 | 5 (13%) | 8 (19%) | 11 (31%) | 9 (24%) |
| 100 | 5 (13%) | 8 (19%) | 5 (14%) | 8 (21%) |
| 60 | 2 (5%) | 5 (12%) | 3 (8%) | 4 (11%) |
| 40 | 0 | 2 (5%) | 2 (6%) | 3 (8%) |
| Change in Stereoacuity (Levels) | Treatment Group | |
|---|---|---|
| Bangerter (N=33) | Patching (N=34) | |
| 2 or more levels improved | 7 (21%) | 9 (26%) |
| Within 1 level | 25 (76%) | 21 (62%) |
| 2 or more levels worsened | 1 (3%) | 4 (12%) |
Cause of amblyopia at time of randomization
P= 0.90 from Wilcoxon Rank Sum Test for difference between treatment groups in distribution of levels of change from baseline to 24 weeks
P= 0.88 from Wilcoxon Rank Sum Test for difference between treatment groups in distribution of levels of change from baseline to 24 weeks
Adverse Events
At 24 weeks the mean change in the fellow eye visual acuity from baseline was 0.09 line in the Bangerter group and 0.36 line in the patching group (p=0.07 for difference between treatment groups in the mean fellow eye acuity, adjusted for baseline acuity, Table 8). One subject (1%) in the Bangerter group and 5 (6%) subjects in the patching group tested 2 or more logMAR lines worse in the fellow eye at 24 weeks compared with baseline (Fisher’s Exact test, P=0.21). Follow-up beyond the end of the study revealed that the fellow eye was 20/25 or better in 4 of the 6 subjects (all in the patching group), while no further follow-up was available in the remaining 2 subjects (1 in the patching group and 1 in the Bangerter group.)
Table 8.
Fellow Eye Visual Acuity at 24-weeks by Treatment Group
| Bangerter N=81 n (%) | Patching N=88 n (%) | |
|---|---|---|
| Distribution of Visual Acuity | ||
| 20/50 | 1 (1%) | 0 |
| 20/40 | 2 (2%) | 0 |
| 20/32 | 9 (11%) | 11 (13%) |
| 20/25 | 15 (19%) | 16 (18%) |
| 20/20 | 29 (36%) | 25 (28%) |
| 20/16 | 25 (31%) | 36 (41%) |
| Mean (SD) logMAR | 0.02 (0.11) | 0.00 (0.10) |
| Snellen Equivalent | 20/20−1 | 20/20 |
| Lines Change from Baseline | ||
| 3 lines or worse | 0 | 0 |
| 2 lines worse | 1 (1%) | 5 (6%) |
| 1 line worse | 17 (21%) | 8 (9%) |
| 0 lines | 39 (48%) | 40 (45%) |
| 1 line better | 20 (25%) | 23 (26%) |
| 2 lines better | 4 (5%) | 11 (13%) |
| 3 lines or better | 0 | 1 (1%) |
| *Mean (SD) logMAR lines change | 0.09 (0.84) | 0.36 (1.1) |
Note: Change from baseline represented rounded values
P = 0.07 from an analysis of covariance model in which the logMAR fellow eye acuity scores were adjusted for baseline acuity
logMAR = logarithm of the minimum angle of resolution; SD = standard deviation.
During the study there were no differences between treatment groups in the number of subjects who developed new-onset strabismus or had an increase or decrease in a pre-existing strabismus (data not shown). There were no subjects diagnosed with reverse amblyopia or constant symptomatic diplopia.
Discussion
The current study compared visual acuity improvement using a Bangerter filter with daily patching when initiating therapy for moderate amblyopia (20/40 to 20/80) over a 24-week period in children ages 3 to <10 years. The study was designed to determine whether Bangerter filters provide essentially the same therapeutic benefit as patching with respect to visual acuity. In a non-inferiority study, to use the correct statistical terminology, ‘essentially the same’ must be a priori defined by selecting a non-inferiority limit. For this study, a non-inferiority limit of 0.75 line was chosen based on consensus from the study planning committee. For the Bangerter filter treatment to meet this definition of non-inferiority to patching, the end of the 95% one-sided confidence interval on the mean difference in change in visual acuity between treatment groups would need to be less than this limit. In our study, although the mean difference between groups was only 0.38 line, the end of the confidence interval on the difference was 0.76 line, and thus, treatment with Bangerter filters did not quite meet the pre-specified definition of non-inferiority to patching when initiating therapy for moderate amblyopia. However, we also did not find that patching was statistically superior to Bangerter filters. Therefore, we cannot conclude that the Bangerter filter treatment effect is similar to that seen with patching (based on our predefined definition of non-inferiority), but we also cannot conclude that patching is definitely better. Compliance assessment was based on parents’ diaries and judgment by the researchers. As we did not use an objective method to measure occlusion or spectacle wear, we cannot guarantee that the patients adhered to their prescribed regimens. For secondary outcomes, the proportions of subjects in the two groups for three definitions of success (≥20/25 acuity, ≥3 line improvement, and amblyopic eye within one line of the fellow eye or better) were similar. Burden of treatment, assessed with the Amblyopia Treatment Index, was less in the Bangerter group than the patching group with respect to adverse events, compliance, and social stigma subscales after 24 weeks of treatment. There was no clear impact of treatment on the fellow eye; more eyes in the patching group had a 2 or more line improvement in acuity but more in the patching group had a 2 or more line worsening. There also was no difference between treatment groups in the worsening or improvement in stereoacuity.
The slightly better mean amblyopic eye acuity at 24 weeks in the patching group compared with the Bangerter group was largely due to more subjects in the Bangerter group having one or more logMAR lines worse acuity (n=5) or no improvement (n=13) at 24 weeks compared with baseline acuity than in the patching group (n=1 and 7, respectively). Of interest, all 5 Bangerter subjects whose acuity worsened one or more lines had significant anisometropia ranging from 3 to 6 D and 4 had poor compliance scores for the question specifically relating to the child peeking over the filter on the 6-week or 24-week Amblyopia Treatment Index. Thus, it seems plausible that in these subjects, amblyopia worsened because of the substantial refractive error in the amblyopic eye, which was not being corrected when the child either did not wear the spectacles or looked over them. When prescribing Bangerter filters for amblyopic patients with high anisometropia, clinicians should carefully monitor spectacle compliance since visual acuity might worsen if the spectacles are either looked over or not worn.
For subjects in the Bangerter group, amblyopic eye visual acuity improvement did not require that the filter reduce the fellow eye acuity to be worse than the amblyopic eye acuity and did not require a shift in fixation from the fellow eye to the amblyopic eye with the Bangerter filter over the fellow eye. These findings were analogous to those that we have reported with atropine,1, 16 where neither fixation switch to the amblyopic eye, nor reduction of visual acuity in the fellow eye to worse than that of the amblyopic eye, are necessary for amblyopic eye improvement. The reasons for this phenomenon are not clear. It is possible that the amblyopic eye is used preferentially for some activities while wearing the Bangerter filter or while using atropine. The topic of improvement in amblyopic eye acuity despite no detectable fixation switch is worthy of further study.
The fact that amblyopic eye acuity can improve with a Bangerter filter over the fellow eye even when the visual acuity is not reduced to below that of the amblyopic eye is reassuring considering the reported variability of blur induced with the filters. Filters of the same manufacturer-labeled density have considerable individual variability in the degree of reduction in acuity, possibly due to nonuniformity from one filter to the next (Repka MX, Gramatikov BI. The reproducibility of blur with a Bangerter filter. J AAPOS 2006:10;80). In addition, there is also variability in reduction of visual acuity with the same filter, possibly due to non-uniformity across the surface of an individual filter or due to individual patient differences in response to blur.17(Bustos DE, Donahue SP. Evaluation of Bangerter filters as a predictable means of blurring vision. Invest Ophthalmol Vis Sci 2006;47:E-Abstract 2457) The present study confirms marked variability of blur induced with a Bangerter filter, with 111 (60%) of 186 enrolled children blurred within 1 line of the manufacturer’s predicted visual acuity at baseline.
The lower negative impact with Bangerter treatment, as measured on the Amblyopia Treatment Index, indicates that the filters were better accepted by the parents and children in our study when compared with part-time patching. This finding is similar to our previous findings favoring atropine over patching.1, 2, 18 Unlike atropine,1, 2 the differences between Bangerter filter treatment and patching in the compliance and adverse effects subscales were not seen at 6 weeks. However, the differences were seen at 24 weeks.
A recent study by Agervi et al19 compared spectacle correction alone to spectacle correction with Bangerter filters in 80 children with untreated anisometropic amblyopia and found a more rapid visual acuity recovery when Bangerter filters were used, but no difference after 12 months. The investigators suggested that using Bangerter filters may accelerate visual acuity improvement in some children with amblyopia. However, these results do not contribute to our understanding of the results of the current study since we compared Bangerter filters to patching in children only after visual acuity had been maximized with best spectacle correction.
In summary, Bangerter filter treatment did not meet our pre-specified criterion to consider the 24-week improvement non-inferior to patching when initiating treatment of moderate amblyopia. We believe that failure to meet the pre-specified criterion was largely influenced by several subjects in the Bangerter group with anisometropic amblyopia that did not improve during the study, likely due to poor compliance. Parental-reported negative impact of treatment with respect to adverse effects, compliance, and social stigma was lower with the filters than with patching. When clinicians consider what treatment to prescribe for moderate amblyopia, the impact of the treatment should be considered. Because the average difference in visual acuity improvement between Bangerter filters and patching was less than half a line, and there was less burden of treatment on the child and family, Bangerter filter treatment is a reasonable option to consider when initiating treatment of moderate amblyopia.
Acknowledgments
Supported by National Eye Institute of National Institutes of Health, Department of Health and Human Services EY011751. The funding organization had no role in the design of the study. It provided external oversight through an independent data and safety monitoring committee.
The Pediatric Eye Disease Investigator Group
Clinical Sites that Participated in this Protocol
Sites are listed in order by number of patients enrolled into the study. Personnel are listed as (I) for Investigator, (C) for Coordinator, and (V) for Visual Acuity Examiner.
Cranberry TWP PA - Everett and Hurite Ophthalmic Association (18)
Darren L. Hoover, (I); Pamela A. Huston, (C); Christine J. Deifel, (V); Barbara R. Fuchs, (V); Pamela M. Racan, (V); Jasbir K. Sayal, (V)
Norfolk VA - Eastern Virginia Medical School (17)
Earl R. Crouch, (I); Eric R. Crouch III, (I); Gaylord G. Ventura, (C); Cynthia M Carlton, (V)
Erie PA - Pediatric Ophthalmology of Erie (16)
Nicholas A. Sala, (I); Benjamin H. Whitling, (I); Rhonda M. Hodde, (C); Veda L. Zeto, (C); Cindy E. Tanner, (V)
Miami FL - Bascom Palmer Eye Institute (15)
Susanna M. Tamkins, (I); Adam S. Perlman, (I); Eva M. Olivares, (C); Yaidy Exposito, (V); Mirna Garcia, (V)
Rockville MD - Stephen R. Glaser, M.D., P.C. (12)
Stephen R. Glaser, (I); Christen Y. Addison, (C); Tracey L. Coussens, (C); Meghan E. Emory, (C)
Birmingham AL - University of Alabama at Birmingham School of Optometry (9)
Robert P. Rutstein, (I); Marcela Frazier, (I); Kristine T. Hopkins, (I); Wendy L. Marsh-Tootle, (I); Katherine K. Weise, (I); Cathy H. Baldwin, (C); Michael P. Hill, (C); Tiffany M. Rhyne, (V)
Lancaster PA - Family Eye Group (7)
David I. Silbert, (I); Noelle S. Matta, (C); Darlene R. Crick, (V); Tiffiny D. Gilmore, (V)
Lisle IL - Progressive Eye Care (7)
Patricia L. Davis, (I); Katie R. Hulett, (C); Carrie S. Bloomquist, (V)
West Des Moines IA - Wolfe Clinic (7)
Donny W. Suh, (I); Marilee McNeece, (C); Autumn Swallow, (C); Rhonda J. Countryman, (V); Shannon L. Craig, (V); Lisa M Fergus, (V)
Concord NH - Concord Eye Care P.C. (6)
Christie L. Morse, (I); Maynard B. Wheeler, (I); Caroline C. Fang, (C); Linda E. Smith, (V)
Streamwood IL - Advanced Vision Center (6)
Ingryd J. Lorenzana, (I); Efigenia Ojeda, (C); Claudia I. Ortiz, (V)
Boise ID - Intermountain Eye Centers (5)
Katherine A. Lee, (I); Bonita R. Schweinler, (C); Derek Beck, (V); Larry W. Plum, (V)
Fullerton CA - Southern California College of Optometry (5)
Susan A. Cotter, (I); Carmen N. Barnhardt, (I); Raymond H. Chu, (I); Kristine Huang, (I); Tawna L. Roberts, (I); Erin Song, (I); Sue M. Parker, (C)
South Charleston WV - Children’s Eye Care & Adult Strabismus Sugery (5)
Deborah L. Klimek, (I); Bounthavy Lisa Greenlee, (C); Lisa L. Winter, (C)
Chicago IL - Illinois College of Optometry (ICO) (4)
Yi Pang, (I); Christine L. Allison, (I); Sandra S. Block, (I); Geoffrey W. Goodfellow, (C); Alicia E. Feis, (V); Jessica L. Schara, (V)
Colorado Springs CO - The Children’s Eye Center (4)
Dave H. Lee, (I); Nieca D. Caltrider, (I); Kelly A. Martinez, (C); Colleen M. Schwanz, (V); Maria M. Busemeyer, (V)
Salt Lake City UT - Rocky Mountain Eye Care Associates (4)
David B. Petersen, (I); J. Ryan McMurtrey, (C); Kristin L. Sylvester, (C)
Boston MA - Tufts New England Medical Center (3)
Nicole B. Quinn, (I); Noopur N. Agarwal-Batra, (C); Vicki M Chen, (V)
Columbus OH - The Ohio State University (3)
Marjean T. Kulp, (I); Freda D. Dallas, (C); Nancy E. Stevens, (C); Michelle J. Buckland, (V); Michael J. Earley, (V)
Durham NC - Duke University Eye Center (3)
Laura B. Enyedi, (I); David K. Wallace, (I); Sarah K. Jones, (C); Courtney E. Fuller, (V)
Philadelphia PA - Salus University/Pennsylvania College of Optometry (3)
Mitchell M. Scheiman, (I); Karen E. Pollack, (C)
Portland OR - Pacific University College of Optometry (3)
Richard London, (I); James J. Kundart, (I); Jayne L. Silver, (C); Garnet M. Yokoi, (V)
Wilmington DE - Delaware Vision Academy, L.L.C. (3)
Don D. Blackburn, (I); Tracy Tunis, (C); Florence Greene, (V)
Wilmington NC - Eye Associates of Wilmington (3)
David A. Johnson, (I); Kellie Drake, (C); Kelly L. Moulton, (V)
Grand Rapids MI - Pediatric Ophthalmology, P.C. (2)
Patrick J. Droste, (I); Robert J. Peters, (I); Jan Hilbrands, (C); Misha K. Mennega, (V); Jennifer L. Mooney, (V)
Minneapolis MN - University of Minnesota (2)*
C. Gail Summers, (I); Ann M. Holleschau, (C); Kathy M. Hogue, (V); Kim S. Merrill, (V)
Nashville TN - Vanderbilt Eye Center (2)*
Sean P. Donahue, (I); David G. Morrison, (I); Lisa A. Fraine, (C); Christine C. Franklin, (C); Neva J. Fukuda, (C); Ronald J. Biernacki, (V)
Albuquerque NM - Children’s Eye Center of New Mexico (1)
Todd A. Goldblum, (I); Angela Alfaro, (C); Chastity R. Escobedo, (V)
Atlanta GA - The Emory Eye Center (1)
Scott R. Lambert, (I); Rachel A. Robb, (C); Marla J. Shainberg, (C)
Baltimore MD - Greater Baltimore Medical Center (1)
Mary Louise Z. Collins, (I); Allison A. Jensen, (I); Maureen A. Flanagan, (C); Cheryl L. McCarus, (C); Dorotea R. Maranto, (V)
Dallas TX - Pediatric Ophthalmology (1)
David R. Stager, (I); Mary K. Alters, (C); Joost Felius, (C)
Dallas TX - Pediatric Ophthalmology, P.A. (1)
Priscilla M. Berry, (I); Mary K. Alters, (C); Joost Felius, (C); June M. Gartlir, (V)
Houston TX - University of Houston College of Optometry (1)
Ruth E. Manny, (I); Karen D. Fern, (I); Gabynely G. Solis, (C); Gloria L Hentz, (V)
Marlton NJ - Michael F. Gallaway, O.D., P.C. (1)
Michael F. Gallaway, (I); Debbie L. Killion, (C)
Philadelphia PA - Children’s Hospital of Philadelphia (1)
Brian J. Forbes, (I); Tina Alvarado Taylor, (C); Malinda A. News, (V)
Rochester NY - University of Rochester Eye Institute (1)
Matthew D. Gearinger, (I); Doreen M. Francis, (C); Lynne M. Addams, (V); Dan A. Castillo, (V)
Saint Paul MN - Associated Eye Care (1)
Susan Schloff, (I); Valori E. Host, (C); E. Denise Daffron, (C)
Waterbury CT - Eye Care Group, PC (1)
Andrew J. Levada, (I); Tabitha L. Walker, (C); MaryJane J. Abrams, (V)
Wilmette IL - Pediatric Eye Associates (1)
Deborah R. Fishman, (I); Lisa C. Verderber, (I); JoAnn Spieker, (C); Sarah Ahn, (V)
*Center received support utilized for this project from an unrestricted grant from Research to Prevent Blindness Inc., New York, New York.
Amblyopia Treatment Study Steering Committee
Roy W. Beck, Eileen E. Birch, Susan A. Cotter, Donald F. Everett, Richard W. Hertle, Jonathan M. Holmes, Pamela A. Huston, Don W. Lyon, Graham E. Quinn, Michael X. Repka, Robert P. Rutstein, Mitchell M. Scheiman, David K. Wallace, David R. Weakley
PEDIG Coordinating Center
Roy W. Beck (Director 2007–2008), Raymond T. Kraker (Director 2009), Nicole M. Boyle, Christina Cagnina-Morales, Danielle L. Chandler, Laura E. Clark, Quayleen Donahue, Brooke P. Fimbel, Heidi A. Gillespie, Elizabeth L. Lazar, Stephanie Lee, Lee Anne Lester, B. Michele Melia, Justice L. Pitts, Nicole T. Reese, Diana E. Rojas, Sydney L. Shrader
National Eye Institute - Bethesda, MD
Donald F. Everett
PEDIG Executive Committee
Michael X. Repka (Chair 2007–2008), Jonathan M. Holmes (Chair 2009), Roy W. Beck, Eileen E. Birch, Stephen P. Christiansen, Donald F. Everett, Darren L. Hoover, Raymond T. Kraker, Katherine A. Lee, Noelle S. Matta, Mitchell S. Scheiman, David K. Wallace
PEDIG Data and Safety Monitoring Committee
Marie Diener-West (Chair), John Baker, Barry Davis, Velma Dobson, Stephen Poff, Dale Phelps, Richard Saunders, Lawrence Tychsen
Footnotes
Writing Committee: Lead authors: Robert P. Rutstein, OD; Graham E. Quinn, MD. Additional authors (alphabetical): Roy W. Beck, MD, PhD; Dean J. Bonsall, MD; Susan A. Cotter, OD; Eric R. Crouch, III, MD; Jonathan M. Holmes, BM, BCh; Darren L. Hoover, MD; Elizabeth L. Lazar, MS, MPH; David A. Leske, MS; Ingryd J. Lorenzana, OD; Michael X. Repka, MD; Donny W. Suh, MD.
This article contains additional online-only materials. The following should appear online only: Table 1, Table 3, Table 5, Table 6, Table 7, and PEDIG Study Group Listing.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Pediatric Eye Disease Investigator Group. A randomized trial of atropine vs patching for treatment of moderate amblyopia in children. Arch Ophthalmol. 2002;120:268–78. doi: 10.1001/archopht.120.3.268. [DOI] [PubMed] [Google Scholar]
- 2.Pediatric Eye Disease Investigator Group. Patching vs atropine to treat amblyopia in children aged 7 to 12 years: a randomized trial. Arch Ophthalmol. 2008;126:1634–42. doi: 10.1001/archophthalmol.2008.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pediatric Eye Disease Investigator Group. Pharmacological plus optical penalization treatment for amblyopia: results of a randomized trial. Arch Ophthalmol. 2009;127:22–30. doi: 10.1001/archophthalmol.2008.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bangerter A. Occlusion in pleoptics and orthoptics [in German] Klin Monatsblatter Augenheilkd Augenarztl Fortbild. 1960;136:305–31. [PubMed] [Google Scholar]
- 5.Lang J. An efficient treatment and new criteria for cure of strabismic amblyopia: reading and Bangerter foils. Binocul Vis Strabismus Q. 1999;14:9–10. [PubMed] [Google Scholar]
- 6.Iacobucci IL, Archer SM, Furr BA, et al. Bangerter foils in the treatment of moderate amblyopia. Am Orthopt J. 2001;51:84–91. doi: 10.3368/aoj.51.1.84. [DOI] [PubMed] [Google Scholar]
- 7.Holmes JM, Beck RW, Repka MX, et al. Pediatric Eye Disease Investigator Group. The Amblyopia Treatment Study visual acuity testing protocol. Arch Ophthalmol. 2001;119:1345–53. doi: 10.1001/archopht.119.9.1345. [DOI] [PubMed] [Google Scholar]
- 8.Beck RW, Moke PS, Turpin AH, et al. A computerized method of visual acuity testing: adaptation of the Early Treatment of Diabetic Retinopathy Study testing protocol. Am J Ophthalmol. 2003;135:194–205. doi: 10.1016/s0002-9394(02)01825-1. [DOI] [PubMed] [Google Scholar]
- 9.Cole SR, Beck RW, Moke PS, et al. Pediatric Eye Disease Investigator Group. The Amblyopia Treatment Index. J AAPOS. 2001;5:250–4. doi: 10.1067/mpa.2001.117097. [DOI] [PubMed] [Google Scholar]
- 10.Holmes JM, Strauber S, Quinn GE, et al. Pediatric Eye Disease Investigator Group. Further validation of the Amblyopia Treatment Index parental questionnaire. J AAPOS. 2008;12:581–4. doi: 10.1016/j.jaapos.2008.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pediatric Eye Disease Investigator Group. A randomized trial of patching regimens for treatment of moderate amblyopia in children. Arch Ophthalmol. 2003;121:603–11. doi: 10.1001/archopht.121.5.603. [DOI] [PubMed] [Google Scholar]
- 12.Pediatric Eye Disease Investigator Group. Randomized trial of treatment of amblyopia in children aged 7 to 17 years. Arch Ophthalmol. 2005;123:437–47. doi: 10.1001/archopht.123.4.437. [DOI] [PubMed] [Google Scholar]
- 13.Pediatric Eye Disease Investigator Group. A randomized trial to evaluate 2 hours of daily patching for strabismic and anisometropic amblyopia in children. Ophthalmology. 2006;113:904–12. doi: 10.1016/j.ophtha.2006.01.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Verbeke G, Molenberghs G. Linear Mixed Models for Longitudinal Data. New York: Springer; 2000. pp. 41–2. [Google Scholar]
- 15.Cox DR. Regression models and life-tables. J R Stat Soc Ser B. 1972;34:187–220. [Google Scholar]
- 16.Pediatric Eye Disease Investigator Group. A randomized trial of atropine regimens for treatment of moderate amblyopia in children. Ophthalmology. 2004;111:2076–85. doi: 10.1016/j.ophtha.2004.04.032. [DOI] [PubMed] [Google Scholar]
- 17.Odell NV, Leske DA, Hatt SR, et al. The effect of Bangerter filters on optotype acuity, Vernier acuity, and contrast sensitivity. J AAPOS. 2008;12:555–9. doi: 10.1016/j.jaapos.2008.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pediatric Eye Disease Investigator Group. Impact of patching and atropine treatment on the child and family in the Amblyopia Treatment Study. Arch Ophthalmol. 2003;121:1625–32. doi: 10.1001/archopht.121.11.1625. [DOI] [PubMed] [Google Scholar]
- 19.Agervi P, Kugelberg U, Kugelberg M, et al. Treatment of anisometropic amblyopia with spectacles or in combination with translucent Bangerter filters. Ophthalmology. 2009;116:1475–80. doi: 10.1016/j.ophtha.2009.02.023. [DOI] [PubMed] [Google Scholar]