Abstract
Background
Heart disease is the leading cause of death for women in the United States. Research has identified that women are less likely than men to receive medical interventions for the prevention and treatment of heart disease.
Methods and Results
As part of a campaign to educate healthcare professionals, 1245 healthcare professionals in 11 states attended a structured 1-hour continuing medical education (CME) program based on the 2004 AHA Evidence-Based Guidelines for Cardiovascular Disease Prevention in Women and completed a pretest and posttest evaluation. We identified significant knowledge deficits in the pretest: 45% of attendees would initially recommend lifestyle changes alone, rather than statin therapy, for women diagnosed with coronary artery disease (CAD); 38% identified statin therapy as less effective in women compared with men for preventing CAD events; 27% identified Asian American women at low risk (rather than high risk) for type 2 diabetes mellitus (DM); and 21% identified processed meat (rather than baked goods) as the principal dietary source of trans fatty acids. Overall, healthcare professionals answered 5.1 of 8 knowledge questions correctly in the pretest, improving to 6.8 questions in the posttest (p < 0.001). Family physicians, obstetrician/gynecologists, general internists, nurse practitioners/physician assistants, and registered nurses all statistically significantly improved knowledge and self-assessed skills and attitudes as measured by the posttest.
Conclusions
Significant knowledge deficits are apparent in a cross-section of healthcare providers attending a CME lecture on women and heart disease. A 1-hour presentation was successful in improving knowledge and self-assessed skills and attitudes among primary care physicians, nurse practitioners, physician assistants, and registered nurses.
Introduction
The Heart Truth Professional Education Campaign was developed by the National Heart, Lung, and Blood Institute (NHLBI) in conjunction with the U.S. Department of Health and Human Services Office on Women's Health (DHHS/OWH), the American Heart Association (AHA), and other partner organizations to address the lack of heart disease awareness among women. This campaign was based on recommendations from experts who convened in 2001 to develop a national action plan to reduce heart disease in women.1 The action plan recommended that women speak with their healthcare provider about specific risks that women have for cardiovascular disease (CVD); therefore, a provider education campaign component was commissioned by the NHLBI through the U.S. DHHS/OWH in 2003.
Lack of healthcare provider knowledge of the guidelines for prevention of CVD in women has been identified as a barrier to reducing morbidity and mortality in this population. Historically, studies have shown that women receive less cholesterol screening, less lipid-lowering therapies, less use of heparin, beta-blockers and aspirin during myocardial infarction (MI), and fewer referrals to cardiac rehabilitation compared with men. These studies suggest that women are less likely than men to receive guideline-recommended care across the spectrum of CVD prevention and treatment, including those within the scope of primary care.2–5 There is further evidence that minority women may be less likely to receive appropriate treatment than white women even when access to care is similar or identical.6–10 We conducted the following study to assess healthcare providers' baseline knowledge of CVD and to determine the effects of a structured educational program on provider knowledge and self-assessed skills.
Materials and Methods
The Heart Truth Professional Education Campaign was developed by a consortium of federally designated National Centers of Excellence in Women's Health, based at academic medical centers, and National Community Centers of Excellence in Women's Health, based in community health centers, community hospitals, and other community-based organizations providing healthcare. The Heart Truth Professional Education Campaign educational objectives were based on the 2004 Guidelines for the Prevention of Cardiovascular Disease in Women developed by the AHA in consultation with NHLBI and other stakeholders.11 Educational materials development was informed by an advisory panel including experts from multiple medical associations and federal expert panels, as well as focus groups of women consumers who commented on information they wanted their healthcare providers to know and communicate.
Provider education materials included continuing medical education (CME) lectures, additional slide resources, web-based CME modules posted on Medscape®, standardized patient and problem-based learning materials for medical and nursing students, printed guides to web-based resources for diagnosis, prevention, and treatment of CVD in women, a bibliography, and a static website providing access to the materials. Versions of these materials (updated to reflect the 2007 AHA/NHLBI Evidence-Based Guidelines for the Prevention of Cardiovascular Disease in Women) can be accessed at www.womenshealth.gov/hearttruth/.
The CME lecture component was developed as a 1-hour lecture. Lecturers selected a slide set from three standardized sets of materials, all with the same 31 essential slides addressing guidelines for the prevention of heart disease in women (Appendix). The essential slides were supplemented with 15–20 slides that provided additional information on guidelines topics. At each lecture, the presenter chose which supplemental slides to include based on the presenter's assessment of the audience's knowledge base and interests. This format was based on expert recommendations that presentations should be available to address the interests of three main groups: (1) healthcare professionals who do not themselves prescribe medications for heart disease (expanded information on counseling and lifestyle information), (2) healthcare professionals judged to have average interest and experience in preventing, diagnosing and treating heart disease (expanded information most relevant to basic guidelines), and (3) healthcare professionals judged to have above-average interest and experience in preventing, diagnosing and treating heart disease (expanded information on recent controversies, e.g., folic acid use, high-sensitivity C-reactive protein (hsCRP) testing). Lecture materials included annotated discussion of the information on each slide and references to support facts presented. Presenters were instructed not to deviate from the lecture format in order to standardize the material presented.
The CME lecture was delivered by a local or regional expert on heart disease and women. The choice of qualifications for the speaker was made based on the expected composition of the audience. These expert speakers included generalist and specialist physicians, advanced practice nurses, and registered nurses with cardiovascular expertise. CME venues included grand rounds presentations and other clinic and hospital-based CME programs as well as free-standing CME programs. Sixty-eight presentations were made in 11 states (Arizona, Connecticut, Delaware, Massachusetts, Minnesota, Missouri, Ohio, Pennsylvania, Rhode Island, Vermont, and Wisconsin) during an 18-month period from July 2005 through December 2006.
Participants were prompted by the presenter and a slide to complete a pretest form before the lecture and a posttest form after the lecture. The pretest-posttest evaluation questions were formulated by experts and pilot tested by groups of healthcare providers of varying background and expertise. The pretest form contained five demographic questions, five self-assessment of knowledge and preparedness (skills) questions, and eight multiple-choice knowledge assessment questions. The posttest contained four questions soliciting feedback on the program in addition to the original five self-assessment of knowledge and preparedness (skills) questions and eight multiple choice knowledge assessment questions from the pretest. Knowledge questions were drawn from content addressing the following curricular objectives: risk stratification, lifestyle modification, pharmacotherapy, and implications of race and ethnicity in CVD prevention in women.
Following the lecture, participants were asked to complete a pretest-posttest evaluation form containing information about the research portion of the evaluation. This form was completed anonymously, and participants were given the option to exclude their information from being used for research. The research portion of the project received Institutional Review Board approval or exemption from all participating institutions. Statistical analyses were carried out with SPSS version 15.0 (SPSS, Chicago, IL).
Results
Of the 2155 healthcare professionals attending the CME lectures, 1285 (59.6%) completed and returned the pretest-posttest form. No information is available about the 40% of CME attendees who did not return the pretest-posttest form. One CME lecture was excluded from our data analysis because no attendance information or pretest forms were obtained. Practice characteristics of providers are shown in Table 1. Subgroup analysis was performed for family physicians, general internists, obstetrician/gynecologists, nurse practitioners/physician assistants, and registered nurses. Nurse practitioners and physician assistants are grouped for purposes of reporting because no significant differences were found between these two groups.
Table 1.
Practice Characteristics of Lecture Attendees: The Heart Truth Professional Education Campaign Continuing Medical Education
| Specialty | Number | % |
|---|---|---|
| Family physician | 162 | 13 |
| General internist | 131 | 10 |
| Obstetrician/gynecologist | 151 | 12 |
| Cardiologist | 9 | 0.7 |
| Other M.D. or D.O.a | 94 | 7 |
| Nurse midwife | 29 | 2 |
| Nurse practitioner | 151 | 12 |
| Physician assistant | 25 | 2 |
| Registered nurse | 346 | 27 |
| Other | 181 | 14 |
| Missing | 6 | 0.5 |
| Weekly clinical activity of attendees | ||
| 0–25 patients | 37 | |
| 26–50 patients | 23 | |
| 51–75 patients | 19 | |
| 76–99 patients | 13 | |
| >99 patients | 8 | |
| Percentage of patients who are women | ||
| 0–25% | 9 | |
| 26–50% | 28 | |
| 51–75% | 31 | |
| 75–99% | 24 | |
| 100% | 9 | |
| Total | 1285 | 100 |
M.D., Doctor of Medicine; D.O., Doctor of Osteopathic Medicine.
Knowledge assessment
Table 2 shows the pretest and posttest results for all healthcare professionals. Subgroups included family physicians, obstetrician/gynecologists, general internists, nurse practitioners/physician assistants, and registered nurses. A mixed-model ANOVA demonstrated a significant interaction effect between subgroups and a gain in knowledge as well as baseline differences.
Table 2.
Pretest-Posttest Knowledge Scores by Specialty: % Correct by Learning Objective: The Heart Truth Professional Education Campaign
| |
All |
General internist |
Family practitioner |
OB/GYNa |
PA/NP |
RN |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Objective | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post |
| Identify factors that place women at high risk (>20% over 10 years) for CVD event | 89.3 | 94.3 | 91.3 | 92.1 | 91.6 | 98.1 | 85.6 | 95.2 | 88.3 | 96.6 | 91.2 | 94.0 |
| Identify correct information about use of statins in women to prevent CVD events | 30.2 | 64.6 | 50.8 | 77.0 | 55.5 | 72.9 | 28.1 | 69.9 | 39.0 | 70.7 | 13.6 | 55.3 |
| Identify that African Americans, Latinas, and Asian Americans are not at low risk of type 2 DM | 59.4 | 89.7 | 68.3 | 86.5 | 66.5 | 92.9 | 54.8 | 89.0 | 66.3 | 95.1 | 58.6 | 90.0 |
| Identify primary dietary source of trans fatty acids | 62.6 | 86.8 | 55.6 | 69.8 | 67.7 | 89.7 | 55.5 | 87.0 | 74.6 | 91.2 | 58.0 | 88.5 |
| Identify that postmenopausal hormone therapy and antioxidant vitamin supplements are not recommended for CVD prevention | 64.3 | 91.6 | 89.7 | 96.8 | 87.1 | 92.9 | 78.0 | 96.6 | 77.6 | 95.1 | 41.7 | 88.8 |
| Identify that African Americans are most likely to die from heart disease among women of all races and ethnicities | 76.5 | 96.3 | 81.7 | 96.8 | 82.6 | 96.1 | 84.9 | 96.6 | 81.5 | 96.6 | 70.1 | 97.3 |
| Identify facts related to smoking cessation in women | 55.9 | 75.6 | 59.5 | 75.4 | 65.2 | 78.7 | 64.4 | 81.5 | 56.6 | 79.0 | 47.4 | 67.4 |
| Identify facts about treatment of HTN in women | 62.3 | 82.3 | 74.6 | 85.7 | 78.1 | 81.3 | 61.6 | 85.6 | 65.4 | 83.9 | 56.5 | 84.0 |
OB/GYN, obstetrician/gynecologist; PA, NP, Physicians assistant/nurse practitioner; RN, registered nurse; CVD, cardiovascular diseases; DM, diabetes mellitus; HTN, hypertension.
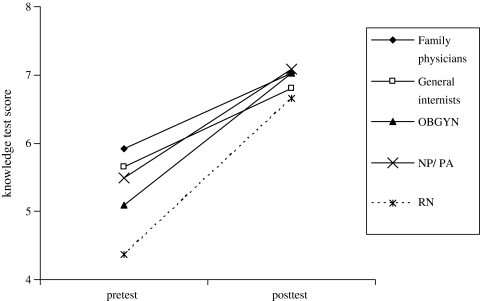
Overall, healthcare professionals answered 5.1 of 8.0 knowledge questions correctly in the pretest. Family physicians were significantly more knowledgeable than obstetrician/gynecologists at pretest (p < 0.001). Registered nurses were significantly less knowledgeable than other groups (p < 0.001). Healthcare professionals improved their knowledge scores at posttest to 6.8 of 8.0 questions; this is a 28% increase over the pretest knowledge scores (p < 0.001) (Fig. 1). The increase in posttest over pretest scores was significantly improved for each of the subgroups (p < 0.001). At posttest, there was one statistically significant difference between subgroups: registered nurses were significantly less knowledgeable than family physicians, obstetrician/gynecologists, and nurse practitioners/physician assistants (p < 0.001).
FIG. 1.
Knowledge test scores on the pretest and posttest: The Heart Truth Professional Education Campaign. Knowledge test scores on the pretest and posttest for family physicians, general internists, obstetrician/gynecologists, nurse practitioners/physicians assistants, and registered nurses. The test scores indicate the number of questions answered correctly out of 8.0 questions. All subgroups showed a significant improvement in knowledge scores between pretest and posttest (p < 0.001).
The pretest revealed significant knowledge deficits (defined as ≥20% of attendees endorsing a specific wrong answer) before the CME lecture. These deficits included the following: 45% of attendees would initially recommend lifestyle changes alone (rather than statin therapy) for women diagnosed with CVD; 38% identified statin therapy as less effective in women compared with men for preventing CVD events; 27% identified Asian American women as having a lower risk (rather than higher risk) for type 2 diabetes mellitus (DM); and 21% identified processed meat (rather than baked goods) as the principal dietary source of trans fatty acids.
At posttest, there was a significant improvement in the knowledge deficits for all questions; however, 30% of attendees continued to endorse lifestyle changes alone initially, rather than statin therapy, for women diagnosed with CVD, and 22% identified statin therapy as less effective in women compared with men for preventing CVD events.
Prior to the CME lecture, attendees who indicated they treat patients with heart disease in clinical practice were significantly more knowledgeable than attendees who indicated they do not treat patients with heart disease (p < 0.001). After the CME lecture, there was no significant difference in knowledge between these two subgroups.
Self-assessment of knowledge
Self-assessment of knowledge was judged on a 5-point Likert scale from Not at all knowledgeable to Very knowledgeable for two issues: (1) knowledge about current approaches to smoking cessation, exercise, weight management, and diet to reduce risk for CVD in women and (2) knowledge about goals for major risk factor interventions to prevent CVD in women, including goals for management of blood pressure, lipids, and DM. Mean results for the pretest and posttest are presented in Table 3. All subgroups showed a highly significant improvement in self-assessed knowledge after the CME session (p <0.001). At pretest, family physicians rated themselves as more knowledgeable than the other subgroups. This difference disappeared at posttest, with the exception of registered nurses; they continued to rate themselves as less knowledgeable than other groups despite their improvement after the CME session.
Table 3.
Pretest-Posttest Self-Assessment of Knowledge and Preparedness: The Heart Truth Professional Education Campaigna
| n | Pretest Mb | Posttest SD | M | SD | ||
|---|---|---|---|---|---|---|
| Self-assessment of knowledge question | ||||||
| How knowledgeable are you about current approaches to smoking cessation, exercise, weight management and diet to reduce risk for CVD in women? | Family physician | 155 | 3.9 | ±0.6 | 4.1 | ±0.7 |
| General internist | 121 | 3.7 | ±0.8 | 4.0 | ±0.7 | |
| OB/GYN | 143 | 3.4 | ±0.8 | 3.8 | ±0.7 | |
| NP/PA | 200 | 3.8 | ±0.8 | 4.1 | ±0.7 | |
| RN | 324 | 3.2 | ±0.9 | 3.7 | ±0.8 | |
| Total | 943 | 3.5 | ±0.9 | 3.9 | ±0.8 | |
| How knowledgeable are you about goals for major risk factor interventions to prevent CVD in women? | Family physician | 152 | 4.0 | ±0.6 | 4.3 | ±0.6 |
| General internist | 120 | 3.8 | ±0.9 | 4.3 | ±0.7 | |
| OB/GYN | 141 | 3.1 | ±0.8 | 3.8 | ±0.7 | |
| NP/PA | 198 | 3.6 | ±1.0 | 4.0 | ±0.8 | |
| RN | 316 | 3.0 | ±0.9 | 3.5 | ±0.9 | |
| Total | 927 | 3.4 | ±1.0 | 3.9 | ±0.8 | |
| Self-assessment of preparedness question | ||||||
| How prepared are you to assess and stratify women into high, intermediate, lower, and optimal risk categories for CVD? | Family physician | 155 | 3.6 | ±0.8 | 4.1 | ±0.7 |
| General internist | 123 | 3.5 | ±0.8 | 4.0 | ±0.7 | |
| OB/GYN | 142 | 2.9 | ±0.9 | 3.7 | ±0.7 | |
| NP/PA | 198 | 3.2 | ±1.0 | 3.8 | ±0.8 | |
| RN | 320 | 2.5 | ±1.0 | 3.4 | ±0.8 | |
| Total | 938 | 3.0 | ±1.0 | 3.7 | ±0.8 | |
| How prepared are you to counsel a woman who asks about the use of hormone therapy, antioxidant supplements, or aspirin to reduce coronary disease event risk with up-to-date information? | Family physician | 149 | 3.5 | ±0.8 | 4.1 | ±0.7 |
| General internist | 121 | 3.4 | ±0.9 | 4.1 | ±0.7 | |
| OB/GYN | 141 | 3.1 | ±1.0 | 3.9 | ±0.8 | |
| NP/PA | 197 | 3.0 | ±1.0 | 3.9 | ±0.8 | |
| RN | 316 | 2.2 | ±1.0 | 3.4 | ±0.9 | |
| Total | 924 | 2.9 | ±1.0 | 3.8 | ±0.9 | |
| How prepared are you to prevent, evaluate, and treat heart disease in women of diverse racial and ethnic backgrounds? | Family physician | 152 | 3.2 | ±0.8 | 4.0 | ±0.7 |
| General internist | 120 | 3.3 | ±0.9 | 4.0 | ±0.7 | |
| OB/GYN | 141 | 2.4 | ±0.9 | 3.4 | ±0.9 | |
| NP/PA | 198 | 2.7 | ±1.0 | 3.6 | ±0.9 | |
| RN | 316 | 2.2 | ±0.9 | 3.2 | ±1.0 | |
| Total | 927 | 2.6 | ±1.0 | 3.6 | ±0.9 | |
Mean scores are based on a 5-point Likert scale, with 1 defined as Not at all knowledgeable, and 5 defined as Very knowledgeable.
M, mean; SD, standard deviation; CVD, cardiovascular diseases; OB/GYN, obstetrician/gynecologist; RN, registered nurse; NP/PA, nurse practioner/physician assistant.
Self-assessment of preparedness (skills)
Self-assessment of skills was judged on a 5-point Likert scale from Not at all prepared to Completely prepared for three issues: (1) preparedness to assess and stratify women into high, intermediate, low, and optimal risk categories for heart disease, (2) preparedness to counsel women about the use of hormone therapy, antioxidant supplements, and aspirin to reduce CVD event risk with up to date information, and (3) preparedness to prevent, evaluate, and treat heart disease in women of diverse racial and ethnic backgrounds. Mean results for the pretest and posttest are presented in Table 3. Family physicians and general internists felt better prepared to stratify women into risk categories and to prevent, evaluate, and treat heart disease before and after the CME session compared with the other groups. All groups, however, showed a significant posttest improvement (p < 0.001) on all three items.
Program feedback
Attendees ranked the program highly. On a 5-point Likert scale with 1 defined as Strongly disagree and 5 defined as Strongly agree, the mean score was 4.4 (±0.6) that the information was credible, 4.0 (±0.8) that the information presented would change how they treated their patients, 4.3 (±0.7) that they felt more knowledgeable about heart disease in women, and 4.2 (±0.8) that the information presented will help them better care for patients of diverse racial and ethnic backgrounds.
Discussion
A standardized 1-hour didactic session with evidence-based materials tailored toward the presenter's assessment of audience needs improved healthcare providers' knowledge of gender-specific prevention and treatment issues in CVD. The session also increased providers' self-assessed efficacy in addressing heart disease in women. The educational program was widely accepted by a range of healthcare professionals, including primary care physicians of various specialties, nurses, and nurse practitioners and physician assistants. Despite knowledge gains, significant knowledge gaps persisted after CME training.
CVD remains the most common reason for death in women in the United States. To reduce the incidence of CVD in women, efforts have focused on educating healthcare consumers about risk and supporting gender-specific research about CVD. Knowledge gaps identified in this study demonstrate that specific strategies to disseminate knowledge of CVD in women to healthcare professionals are urgently needed.
The baseline knowledge assessment revealed some interesting gaps in knowledge. For example, a third or more of respondents were unaware that statins are recommended for all women with known CVD and that statins have specific benefits for women. Few studies have systematically assessed gender-specific gaps in provider knowledge. In one study, 300 primary care physicians, 100 obstetrician/gynecologists, and 100 cardiologists were asked to respond to experimental cases of CVD in women and men; this study found that women in the experimental cases were more likely to be inappropriately assigned to low-risk categories than men. Women who were inappropriately identified as low risk were less likely to receive appropriate recommendations for lifestyle change and preventive pharmacotherapy.12 More information is needed about gender-specific gaps in provider knowledge to better understand how to tailor gender-specific information in CME programs to ensure that women receive evidence-based care from their providers.
Healthcare providers in our study demonstrated knowledge of the greater prevalence of risk factors for CVD in the African American population; however, they had less knowledge about risk factors in Asian American women. Other studies have shown racial disparities in care even after controlling for socioeconomic status (SES), including one study that found cholesterol-lowering drugs are less commonly used after MI by African Americans than by whites, even after controlling for socioeconomic status.9 Another study assessing racial disparities in clinical evaluation of CVD practice found that when presented with identical case histories deemed by experts to warrant further cardiac testing, physicians were significantly less likely to suggest cardiac evaluation for an African American woman than for either a white or African American man or a white woman. In this study, clinicians evaluated identical case histories presented by videotaped actors, so that the scenario varied only by the apparent race and gender of the patient.10
Providers' lack of knowledge about trans fatty acids may reflect the timing of the intervention. CME presentations occurred before the announcement of proposed government regulations to reduce dietary trans fatty acids, which were publicized at the end of 2006.13 However, lack of knowledge about dietary trans fatty acids may also accurately reflect healthcare providers' current lack of knowledge and training about dietary issues.
A limitation of the study was the use of self-assessment to measure providers' preparedness and skills. Providers self-selected to attend the program; this may have resulted in a group that was more knowledgeable or less knowledgeable than providers as a whole. The effectiveness of the program might be different if it were made mandatory or if presenters were more or less expert in the topic area or skilled as educators. Because presentations were made by different presenters and the presenters were standardized only in core elements, some groups may have had repetitions in materials or more effective verbal explanations than others. The decision to test knowledge gained using an identical pretest and posttest could have introduced bias, as participants likely had heightened interest in hearing information about questions initially posed.
Because of the short-term follow-up period, the study did not reassess provider knowledge after a period of time had lapsed to demonstrate that the information learned at the CME lecture was retained. The study lacks data on actual clinical practice as pretest and whether the practice of the providers changes after the CME program. Efforts to study long-term effects of The Heart Truth CME programs are underway.
Conclusions
Significant knowledge deficits are apparent in a cross-section of healthcare providers attending a CME lecture on women and heart disease. A 1-hour presentation was successful in improving knowledge and self-assessed skills and attitudes among primary care physicians, nurse practitioners/physician assistants, and registered nurses.
Appendix: Guidelines-Based Content for The Heart Truth CME Presentations
All CME presentations contained 31 identical core slides and an additional 15–20 slides that varied based on the knowledge and interests of the audience. This list reflects the information contained in the core slides.
Background
Cardiovascular disease mortality trends for males and females
Cardiovascular disease ranking for cause of death among women of different racial and ethnic groups
Association between race/ethnicity and high risk for diabetes
Process
Five-step approach to prevention: assessment of level of risk, lifestyle approaches for coronary artery disease prevention; treatment of hypertension, diabetes, lipid abnormalities; highest priority is for intervention in high-risk patients; avoid therapies that lack benefit or where risks outweigh benefits
Risk stratification, including definition of metabolic syndrome
Interventions
Smoking cessation and avoidance of environmental tobacco
Encourage physical activity
Weight maintenance/reduction goals
Treatment of hypertension, including lifestyle approaches
Optimal lipid levels; dietary and medication interventions to reach goals
Recommended HbA1C target for diabetics
Use of aspirin in high-risk, intermediate-risk, and lower-risk women
Hormone therapy should not be given for primary or secondary prevention of heart disease
Antioxidant supplements should not be given for primary or secondary prevention of heart disease
References
- Mosca L. Appel LJ. Benjamin EJ, et al. Evidence-based guidelines for cardiovascular disease prevention in women. circ.ahajournals.org/cgi/content/short/109/5/672. Circulation. 2004;109:672–695. doi: 10.1161/01.CIR.0000114834.85476.81. [DOI] [PubMed] [Google Scholar]
- The Heart Truth Professional Education Campaign. www.nhlbi.gov/health/hearttruth/press/nhlbi_04_campaign.htm www.nhlbi.gov/health/hearttruth/press/nhlbi_04_campaign.htm
Acknowledgments
We thank the following organizations for their support and advice in development of the educational materials: the American Academy of Physician Assistants, the American College of Cardiology, the American College of Family Physicians, the American College of Obstetricians and Gynecologists, the American College of Physicians, the American Heart Association, the Association of Black Cardiologists, the Asian and Pacific Islander American Health Forum, the Association of Women's Health, Obstetric, and Neonatal Nurses, the National Hispanic Medical Association, the National Medical Association, and the Department of Health and Human Services Office on Women's Health Minority Women's Health Panel of Experts. The listing of these organizations does not imply their endorsement of this article. We further wish to acknowledge the work and support of the following individuals who contributed to the dissemination portion of The Heart Truth Professional Education Campaign: Eileen P. Newman, M.S., R.D., Ann M. Taubenheim, Ph.D., M.S.N, Gladys Ruiz, R. Ann Abercrombie, M.L.S., Kathy W. Beenen, M.B.A, Rachna Chaudhari, M.P.H., Mary Dortenzo, M.S.N., N.P.C, Jo Jean Elenes, Denise Flinn, Gina Gilliland, R.N.C., WHNP, Mandy Herleth, Dixie Horning, Anna L. Kindermann, J.D., Katherine Kolb, R.N., B.S.N, M.S., Jennifer Lennon, Terry Long, Melissa McNeil, M.D., Celisse Morris-Miller, M.S., Susan M. Nappi, Elizabeth O'Neill, B.A., Michele Ondeck, R.N., M.E.d., Abigail L. Reese, C.N.M., M.S.N., Tara Rizzo, M.P.H., Susan Samuels, R.N., B.S.N., Kimberly D. Sanders, Robert F. Schwartz, Stephanie Singer, Ying Studebaker, M.S., R.N, C.N.S., Elizabeth C. Thul, L.S.W., Margaret Trautz, Elisabeth von der Lohe, M.D., Esther Yasui, Erika Graves, and Robin Lam.
This work was supported by the Department of Health and Human Services Office on Women's Health (order number HHSP233200400916P). Additional support for manuscript preparation was provided by the Executive Advisory Board of the Iris Cantor-UCLA Women's Health Center.
The views expressed within are solely those of the authors and do not necessarily represent the views of the Department of Health and Human Services. The authors had full access to the data and take responsibility for its integrity. All authors have read and agree to the article as written.
All authors received funding support from the Department of Health and Human Services Office of Women's Health for development or dissemination of the Heart Truth Professional Education Campaign. S.G. is the recipient of a DHHS grant, Advancing System Targets for HP2010 To Improve Cardiovascular Health of Women in Rural Illinois. C.R. and A.E.N. are recipients of a K-08 NHLBI Cultural Medical Education Curriculum grant. M.D. is the recipient of NIDA R01, Exercise and Nicotine Replacement for Female Smokers, receives honoraria as a member of the Massachusetts Public Health Council, and owns stock in Pfizer Inc.
Disclosure Statement
The authors have no conflicts of interest to report.
References
- 1.National Heart, Lung, and Blood Institute. The Heart Truth Campaign overview. www.nhlbi.nih.gov/health/hearttruth/press/nhlbi_04_campaign.htm. [Aug 1;2007 ]. www.nhlbi.nih.gov/health/hearttruth/press/nhlbi_04_campaign.htm
- 2.Chandra NC. Ziegelstein RC. Rogers WJ, et al. Observations of the treatment of women in the United States with myocardial infarction: A report from the National Registry of Myocardial Infarction-I. Arch Intern Med. 1998;158:981–988. doi: 10.1001/archinte.158.9.981. [DOI] [PubMed] [Google Scholar]
- 3.Nohria A. Vaccarino V. Krumholz HM. Gender differences in coronary artery disease in women: Gender differences in mortality after myocardial infarction: Why women fare worse than men. Cardiol Clin. 1998;16:45–57. doi: 10.1016/s0733-8651(05)70383-0. [DOI] [PubMed] [Google Scholar]
- 4.Scott LB. Allen JK. Providers' perceptions of factors affecting women's referral to outpatient cardiac rehabilitation programs: an exploratory study. J Cardiopulm Rehabil. 2004; 24:387–391. doi: 10.1097/00008483-200411000-00005. [DOI] [PubMed] [Google Scholar]
- 5.O'Meara JG. Kardia SL. Armon JJ. Brown CA. Boerwinkle E. Turner ST. Ethnic and sex differences in the prevalence, treatment, and control of dyslipidemia among hypertensive adults in the GENOA study. Arch Intern Med. 2004;164:1313–1318. doi: 10.1001/archinte.164.12.1313. [DOI] [PubMed] [Google Scholar]
- 6.Curtis LH. Al-Khatib SM. Shea AM. Hammill BG. Hernandez AF. Schulman KA. Sex differences in the use of implantable cardioverter-defibrillators for primary and secondary prevention of sudden cardiac death. JAMA. 2007; 298:1517–1524. doi: 10.1001/jama.298.13.1517. [DOI] [PubMed] [Google Scholar]
- 7.Hernandez AF. Fonarow GC. Liang L, et al. Sex and racial differences in the use of implantable cardioverter-defibrillators among patients hospitalized with heart failure. JAMA. 2007;298:1525–1532. doi: 10.1001/jama.298.13.1525. [DOI] [PubMed] [Google Scholar]
- 8.Hendrix KH. Riehle JE. Egan BM. Ethnic, gender, and age-related differences in treatment and control of dyslipidemia in hypertensive patients. Ethn Dis. 2005;15:11–16. [PubMed] [Google Scholar]
- 9.Ayanian JZ. Landon BE. Landrum MB. Grana JR. McNeil BJ. Use of cholesterol-lowering therapy and related beliefs among middle-aged adults after myocardial infarction. J Gen Intern Med. 2002;17:95–102. doi: 10.1046/j.1525-1497.2002.10438.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schulman KA. Berlin JA. Harless W, et al. The effect of race and sex on physicans' recommendations for cardiac catheterization. N Engl J Med. 1999;340:618–626. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- 11.Mosca L. Appel LJ. Benjamin EJ, et al. Evidence-based guidelines for cardiovascular disease prevention in women. Circulation. 2004;109:672–693. doi: 10.1161/01.CIR.0000114834.85476.81. [DOI] [PubMed] [Google Scholar]
- 12.Mosca L. Linfante AH. Benjamin EJ, et al. National study of physician awareness and adherence to cardiovascular disease prevention guidelines. Circulation. 2005;111:499–510. doi: 10.1161/01.CIR.0000154568.43333.82. [DOI] [PubMed] [Google Scholar]
- 13.New York City passes trans fat ban. MSNBC.com. www.msnbc.msn.com/id/16051436/ [Sep 5;2007 ]. MSNBC.comwww.msnbc.msn.com/id/16051436/ December 5, 2006.