Abstract
Background
Secondary prevention improves survival, yet implementation is suboptimal. We tested the impact of a systematic hospital-based educational intervention vs. usual care to improve rates of adherence to secondary prevention guidelines among women hospitalized with coronary heart disease (CHD), according to their ethnic status.
Methods
Women (n = 304, 52% minorities) hospitalized with CHD were randomly assigned to a systematic secondary prevention educational intervention vs. usual care. Adherence to goals for smoking cessation, weight management, physical activity, blood pressure <140/90 mm Hg, low-density lipoprotein cholesterol (LDL-C) <100 mg/dL (2.59 mmol/L), and use of aspirin/anticoagulants, beta-blockers, and angiotensin-converting enzyme (ACE) inhibitors were assessed at 6 months.
Results
On admission, minority women were less likely than white women to meet the goals for blood pressure (OR = 0.46, 95% CI 0.26-0.80), LDL-C (OR = 0.57, CI 0.33-0.94), and weight management (OR = 0.40, 95% CI 0.20-0.82). There was no difference between the intervention and usual care groups in a summary score of goals met at study completion; however, minority women in the intervention group were 2.4 times more likely (95% CI 1.13-5.03) to reach the blood pressure goal at 6 months compared with minority women in usual care. White women in the intervention group were 2.86 times more likely (95% CI 1.06-7.68) to report use of beta-blockers at 6 months compared with white women in usual care. In a logistic regression model, the interaction term for ethnic status and group assignment was significant for achieving the blood pressure goal (p = 0.009).
Conclusions
A healthcare systems approach to educate women about secondary prevention and blood pressure control may differentially benefit ethnic minority women compared with white women.
Introduction
Secondary prevention strategies for coronary heart disease (CHD), such as cholesterol and blood pressure management, have been shown to extend survival and to reduce recurrent cardiovascular events and the need for revascularization in both men and women.1 Despite the documented efficacy of risk-reducing strategies, many patients with CHD do not receive optimal preventive therapy and do not reach target goals.2–4 Women are less likely than men to participate in comprehensive secondary prevention programs or formal cardiac rehabilitation and to meet national standards for risk factor management.5,6 Moreover, minority women are less likely than white women to have adequate risk factor control, despite a greater recurrent CHD event rate.7 These data underscore the importance of developing systematic approaches to improve adherence with secondary prevention strategies, especially among women of ethnic minorities.
Prior studies have shown that hospital-based programs to increase adherence to lifestyle and medical therapy for CHD prevention have mixed results. Systemwide protocols to initiate aspirin, beta-blocker, angiotensin-converting enzyme (ACE) inhibitors, and cholesterol-lowering medication during hospitalization for an acute CHD event have demonstrated increased use of some therapies after discharge. Prior studies provided proof of concept; however, secular trends may have influenced the results because of the uncontrolled design of the studies.8,9 Well-designed studies of physician or nurse-directed case management interventions to improve lifestyle and risk factor control have shown benefits among intensive interventions but not consistently among more moderate interventions that may be more readily implemented in practice.10–15 Studies to evaluate the impact of systems approaches in real world settings on the quality of preventive care are very limited, especially among high-risk and ethnically diverse populations.
The purpose of the Secondary Prevention Beyond Hospital Walls Intervention Trial In Women (WITTI Women) Study was to evaluate the impact of a systematic educational intervention among women hospitalized with CHD on attainment of American Heart Association/American College of Cardiology (AHA/ACC) secondary prevention guidelines compared with usual care at 6 months after discharge and to determine if the effect varied by ethnic status.1,16
Materials and Methods
Subjects
The study was a randomized controlled clinical trial of 304 women with CHD admitted to the NewYork-Presbyterian Hospital (Columbia and Weill Cornell Campuses) or the University of North Carolina Health System between October 2001 and February 2003. Inclusion criteria were a diagnosis of acute myocardial infarction (MI) (ICD-9 410.0), unstable angina (ICD-9 411.1), stable angina (ICD-9 413.9), prior CHD (ICD-9 412.0), or a cardiac revascularization procedure (catheter-based ICD-9 36.0, 36.09, 36.3 or coronary artery bypass grafting [CABG] 414.02). Exclusion criteria were a life expectancy of <6 months, pregnancy, non-English or non-Spanish speaking, and an inability or unwillingness to follow up or give informed consent. Consent from a physician to participate was required. The institutional review boards of each participating institution approved the protocol.
Potential subjects were identified through systematic review of hospital admission logs, operating room schedules, cardiac catheterization laboratory schedules, and hospital chart review.
Intervention and usual care
Participants were randomized according to a blocked design (by site and halfway point to recruitment) using a central dial-in web-based system to assign subjects to the intervention or usual care group. The intervention group received education and counseling by a prevention facilitator/educator during hospitalization and during phone visits at 2, 4, and 12 weeks and a phone or clinic visit at 6 weeks postdischarge. Prevention facilitators were nonphysician, nonnurse health professionals who had formal training in health education, nutrition, medical technology, or public health and underwent standardized training by the NewYork-Presbyterian Hospital Preventive Cardiology Program professional staff.
The initial educational session included 1 hour of structured counseling before discharge that reviewed smoking, exercise, nutrition, weight, and blood pressure and cholesterol goals for secondary prevention based on the AHA/ACC guidelines and provided information on how to achieve them based on social learning theory and the five A's construct (ask, advise, agree, assist, arrange).1,16–19 Specifically, after completion of an assessment of secondary prevention goal attainment status, participants received feedback on their goals and health behaviors. They were advised on recommendations for behavior change personalized to their specific needs. Prevention facilitators and participants agreed on specific, achievable goals. Facilitators assisted the participants in developing action plans to accomplish their goals and provided referrals as needed. Dates and times for follow-up visits and phone calls were arranged at the end of the initial educational session for the purpose of obtaining feedback, monitoring progress, and encouraging preventive action.
All patients were encouraged to attend cardiac rehabilitation and to exercise a minimum of 3–5 days/week. The facilitator instructed the patient on heart rate guidelines and Borg perceived exertion levels based on treadmill test results as outlined by the American College of Sports Medicine's Guidelines for Exercise Testing and Prescription.20 The exercise prescription was tailored to individual preferences, orthopedic limitations, weather conditions, equipment availability, and other barriers identified by the prevention facilitator. Body mass index (BMI) was calculated, and participants were advised of their BMI and the desirable BMI range of 18.5–24.9 kg/m2. Nutrition counseling was based on the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III).21 Participants were advised to reduce saturated fat intake (<7% of calories/day), reduce dietary cholesterol (<200 mg/day), moderate alcohol consumption, reduce sodium intake, increase fruits and vegetables, and incorporate low-fat dairy products in their diets. Smoking cessation counseling was initiated in smokers in the hospital using relapse prevention materials based on the U.S. Department of Health and Human Services recommendations.22 Patients were encouraged to stop smoking and avoid secondhand smoke and were referred to formal smoking cessation programs as appropriate. All subjects were informed that use of beta-blockers, aspirin or antiplatelet agents, and ACE inhibitors often is recommended for patients with CHD, and criteria for contraindications were reviewed.1
Before discharge, each subject reviewed a personalized checklist of prevention goal status with the prevention facilitator and received an educational booklet in English or Spanish that discussed each target in detail, including the rationale for risk factor modification and strategies to attain each goal. All women in the intervention group were systematically referred to cardiac rehabilitation and were assisted with locating a program if needed. During follow-up phone calls, the prevention facilitator systematically inquired about challenges and barriers to adherence to secondary prevention goals. The prevention facilitator problem solved with the participant for any goals that were not met at baseline or attained at each contact point. For example, if a woman could not attend a formal cardiac rehabilitation program because of lack of transportation, the prevention facilitator assisted with finding transportation, or a home-based walking program was prescribed.
The physicians of participants randomized to the intervention group received standardized progress reports about personalized goal attainment at discharge and 6 weeks. The report included the current level of risk factor control and medication use as well as minimum and optimal targets. A cover letter to the physicians outlined in bold bullet points a list of prevention goals that their patients were currently not meeting according to AHA/ACC standards.1,16
Definition of adherence to goals
Adherence to eight prevention goals was defined as (1) complete smoking cessation, (2) blood pressure <140/90 mm Hg, (3) low-density lipoprotein cholesterol (LDL-C) <100 mg/dL (<2.59 mmol/L), (4) physical activity at least 30 minutes three times per week or enrollment in formal cardiac rehabilitation, (5) BMI 18.5–24.9 kg/m2 and waist circumference <35 inches (<88 cm), (6) use of aspirin or clopidogrel or warfarin if aspirin was contraindicated, (7) use of ACE inhibitor unless contraindicated or creatinine >2.0 documented, and (8) use of beta-blocker unless contraindicated.
Baseline and outcome assessments
Standardized examinations and interviewer-assisted questionnaires were obtained at baseline to assess adherence to prevention goals by a trained research assistant. Blood pressure, height, weight, and waist circumference were determined using standard procedures.23,24 Smoking status was determined by self-report and validated with exhaled carbon monoxide levels at 6 weeks and 6 months.25 Lipid levels drawn within 24 hours of admission were used for the baseline values, and if they were not available, outpatient measures within 6 months of admission were documented. Follow-up lipid and lipoprotein levels were obtained by fingerstick and analyzed using Cholestech (Hayward, CA) technology or performed locally.26
We encouraged all intervention and control subjects to have outcome measures determined at their respective clinical site. Because of the tertiary referral nature of the hospitals and the real world design of the study, if women could not return for outcome assessment, local physician records and self-report were systematically obtained in the control and intervention groups to determine adherence to prevention goals. Women were called up to three times and sent a letter, and physicians were contacted by staff to obtain outcome information. Electronic hospital records and laboratory data were also reviewed.
Sample size and statistical analysis
The attainment of secondary prevention goals between the intervention and usual care groups was the primary objective of the study and was used to determine the sample size. We devised a summary score of secondary prevention goals (each goal attained equal to 1 point) to evaluate overall adherence. The study was designed to have 80% power to detect a difference in a mean summary score of 1 between the two groups, assuming a common standard deviation (SD) of 3.0 (based on pilot data) using a two-group t test and 0.05 two-sided significance level, assuming an attrition of 5% over a 6-month follow-up period.
The intention-to-treat analysis was a t test comparison of the summary score at 6 months between the intervention group and the usual care group. We then stratified by ethnic status and repeated the analysis at 6 weeks and 6 months. Potential confounding was evaluated using linear regression models that included clinical site, education level (>high school education vs. not), marital status (married vs. unmarried), revascularization status (surgical or nonsurgical vs. neither), age (≥65 vs. <65 years), and ethnic status (white vs. minority) in addition to group assignment. We tested for interaction using an ethnic status × group assignment term in the model. In secondary analyses, we compared the proportion of women who met each of the eight prevention goals in the intervention and usual care groups using a chi-square test. We conducted the analysis for women overall by site and by CHD diagnosis and stratified by ethnic status; we also compared proportions of minorities and whites achieving goals within each treatment arm at 6 months. We performed logistic regression that included the independent variables outlined, with each prevention goal (achieved or not) as the dependent variable. To evaluate the potential impact of missing data and lost to follow-up, we imputed the 6-month follow-up summary score with the baseline score (assumed no change) for each subject and repeated the main analysis. Statistical analyses were conducted using the SAS version 8.2 (Cary, NC). Statistical significance was set at p < 0.05.
Results
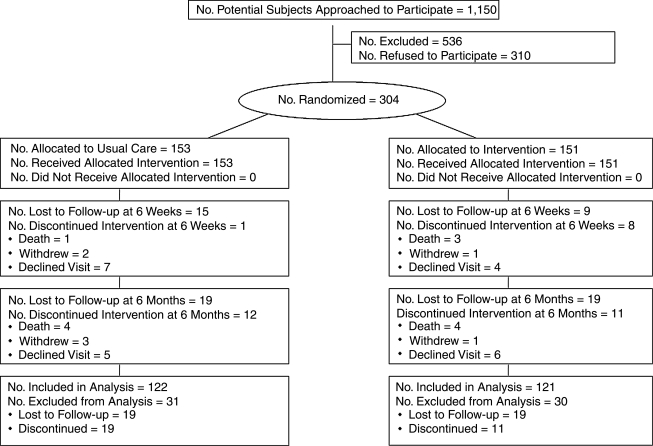
As shown in Figure 1, there were 1150 women approached to participate, and 536 were excluded, primarily because of an inability or unwillingness for follow-up. Of the 614 subjects who were eligible for participation, 50% (n = 304) agreed and signed the informed consent. The reasons for nonparticipation were (1) felt too old or too sick (n = 165), (2) felt no need for education (n = 90), (3) felt too stressed (n = 26), (4) were opposed to research (n = 21), or (5) family objected to participation (n = 8).
FIG. 1.
Study flow diagram.
At the 6-week and 6-month follow-up visits, 86% and 80% of subjects, respectively, had outcome measures available for analysis. Overall, intervention subjects were not more likely than usual care subjects to have follow-up information available, although at 6 weeks and 6 months, minorities were more likely than white women to return for a visit. At 6 months, 56% of the subjects with follow-up data had measurements determined at the clinical site, and 44% were obtained from local physician records/self-report that was not differential with respect to intervention and controls. There was a trend for higher follow-up rates among those with a history of CHD prior to admission compared to those with newly diagnosed CHD (OR = 1.4, 95% CI 0.9-2.2).
Baseline characteristics of the study participants are listed in Table 1. The mean age of women with CHD in this study was 62.3 ± 12.4 years (range 29–90 years); 47.7% were white, 33.6% were black, and 15.1% were Hispanic. There were no significant differences in any major characteristic based on group assignment, suggesting randomization was successful. Of note was that minority women were significantly less likely to have an education beyond high school (p = 0.0004) or be married (p = 0.006) and were significantly more likely to have a history of diabetes (p = 0.03) or history of hypertension (p = 0.0008), or be <65 years (p = 0.008) on admission compared with white women. Approximately half of the women were admitted with an acute coronary syndrome, and 55% of the participants underwent a revascularization procedure (30% of women had CABG). Overall, 74% of women had a prior history of CHD documented.
Table 1.
Baseline Characteristics of Women Hospitalized with Coronary Heart Disease, by Group Assignment and Ethnicity
| |
Group assignment |
Ethnicity |
||
|---|---|---|---|---|
| Characteristic | Intervention (n = 151) n (%) | Usual care (n = 153) n (%) | White (n = 145) n (%) | Minority (n = 159) n (%) |
| Age ≥ 65 years | 59 (39) | 67 (44) | 72 (50) | 54 (34)* |
| White | 74 (49) | 71 (46) | 145 (100) | 0 (0) |
| >High school education | 73 (49) | 61 (40) | 79 (55) | 55 (35)* |
| Married | 64 (42) | 64 (42) | 73 (50) | 55 (35)* |
| With dependents | 40 (27) | 33 (22) | 33 (23) | 40 (25) |
| Employed | 39 (26) | 35 (23) | 38 (27) | 36 (23) |
| Prior history of CHD | 106 (70) | 118 (77) | 106 (73) | 118 (74) |
| Current ACS | 73 (48) | 72 (47) | 77 (53) | 68 (43) |
| Current revascularization | 80 (53) | 86 (56) | 87 (60) | 79 (50) |
| History of DM | 63 (42) | 68 (44) | 53 (37) | 78 (49)* |
| History of hypertension | 116 (78) | 122 (80) | 102 (71) | 136 (87)* |
| History of dyslipidemia | 108 (73) | 114 (75) | 109 (76) | 113 (72) |
p < 0.05 between group comparison (white vs. minority).
CHD, coronary heart disease; ACS, acute coronary syndrome; DM, diabetes mellitus.
There were no significant differences in baseline prevention goals between the intervention and usual care groups (Table 2). Of note is that overall, only 13% of women met the weight management goal, 20% met the exercise goal, and less than half (41%) had an optimal LDL-C, <100 mg/dL (2.59 mmol/L). The intervention group did not differ with respect to the usual care group for the summary score (mean goals achieved) at 6 weeks or 6 months, before and after imputing missing data. The rate of smoking was greater in the intervention arm compared with the usual care group at 6 months, although both groups had more nonsmokers at follow-up than at baseline. In a multiple logistic regression model adjusted for confounders, group assignment was not predictive of smoking status or any other prevention goal at the 6-month follow-up.
Table 2.
Baseline and Follow-up Secondary Prevention Goals Met Among Women Hospitalized with Coronary Heart Disease by Group Assignmenta
| Prevention goal | Intervention (n = 151) n (%) | Usual care (n = 153) n (%) |
|---|---|---|
| Blood pressure <140/90 mm Hg | ||
| Baseline | 114 (75) | 118 (77) |
| (n) | 151 | 153 |
| 6 weeks | 84 (65) | 73 (60) |
| (n) | 129 | 121 |
| 6 months | 74 (64) | 66 (59) |
| (n) | 116 | 111 |
| LDL-C <100 mg/dL | ||
| Baseline | 51 (42) | 49 (40) |
| (n) | 121 | 121 |
| 6 weeks | 36 (45) | 48 (58) |
| (n) | 80 | 83 |
| 6 months | 54 (57) | 50 (60) |
| (n) | 95 | 84 |
| Nonsmoker | ||
| Baseline | 119 (79) | 131 (86) |
| (n) | 151 | 153 |
| 6 weeks | 105 (86) | 102 (93) |
| (n) | 122 | 110 |
| 6 months | 95 (85) | 101 (94)* |
| (n) | 112 | 108 |
| Exercise/cardiac rehabilitation | ||
| Baseline | 29 (20) | 29 (20) |
| (n) | 144 | 148 |
| 6 weeks | 27 (23) | 27 (25) |
| (n) | 119 | 108 |
| 6 months | 41 (38) | 32 (30) |
| (n) | 108 | 105 |
| BMI 18.5–24.9 kg/m2 and waist circumference <35 inches | ||
| Baseline | 24 (17) | 15 (10) |
| (n) | 143 | 150 |
| 6 weeks | 28 (22) | 21 (17) |
| (n) | 126 | 121 |
| 6 months | 22 (20) | 20 (18) |
| (n) | 108 | 109 |
| Aspirin/antiplatelet therapy | ||
| Baseline | 127 (85) | 133 (88) |
| (n) | 149 | 151 |
| 6 weeks | 115 (87) | 101 (82) |
| (n) | 132 | 123 |
| 6 months | 102 (89) | 99 (84) |
| (n) | 115 | 118 |
| ACE inhibitor therapy | ||
| Baseline | 93 (67) | 98 (66) |
| (n) | 139 | 149 |
| 6 weeks | 79 (76) | 79 (84) |
| (n) | 104 | 94 |
| 6 months | 77 (81) | 67 (75) |
| (n) | 95 | 89 |
| Beta-blocker therapy | ||
| Baseline | 118 (80) | 118 (81) |
| (n) | 147 | 146 |
| 6 weeks | 114 (86) | 96 (79) |
| (n) | 132 | 122 |
| 6 months | 98 (84) | 89 (76) |
| (n) | 116 | 117 |
| Summary score | Mean ± SD number of goals attained | |
|---|---|---|
| Baseline | 4.7 (1.2) | 4.7 (1.2) |
| (n) | 103 | 111 |
| 6 weeks | 4.7 (1.3) | 5.1 (1.2) |
| (n) | 59 | 54 |
| 6 months | 5.1 (1.1) | 5.1 (1.0) |
| (n) | 69 | 58 |
p < 0.05 between group comparison (intervention vs. usual care).
To convert values for cholesterol from mg/dL to mmol/L, multiply by 0.02586. To convert values in inches to centimeters, multiply by 2.54.
CHD, coronary heart disease; ACE, angiotensin-converting enzyme.
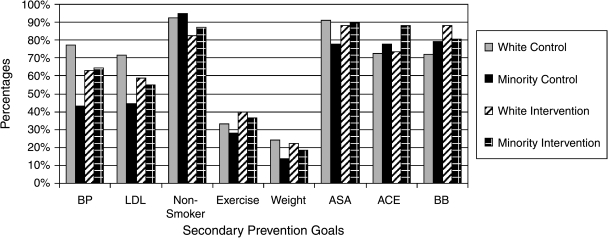
Subgroup analysis by ethnic status is depicted in Figure 2. Baseline data demonstrate that minority women were significantly less likely than white women to meet the goals for blood pressure (OR = 0.46, 95% CI 0.26-0.80), LDL-C (OR = 0.56, CI 0.33-0.94), and weight management (OR = 0.40, 95% CI 0.20-0.82). A similar pattern was observed at 6 months. In stratified analyses, white women randomized to the intervention had increased use of beta-blockers at 6 months compared with white controls (OR = 2.86, 95% CI 1.06-7.68), and minority women who received the intervention were more likely to be at the blood pressure target than minority women in usual care (OR = 2.39, 95% CI 1.13-5.03).
FIG. 2.
Proportion of white and minority women achieving secondary prevention goals at 6 months, by group assignment. BP, blood pressure; LDL, low-density lipoprotein; ASA, antiplatelet/anticoagulant therapy; ACE, angiotensin-converting enzyme inhibitor therapy; BB, beta-blocker therapy.
Interestingly, within the intervention arm, minority were equally likely as white women to meet the eight prevention goals; however, within the usual care group, white women were significantly more likely than minority women to reach target for blood pressure (p = 0.0002) and LDL-C (p = 0.012) and had a trend toward increased use of aspirin/antiplatelet agents (p = 0.053). A formal test of interaction between ethnic status and group assignment was significant for achieving the blood pressure goal at 6 months (p = 0.009). Among minorities, regression models adjusted for age, education, marital status, employment, and site reveal that minority women assigned to the intervention had a 2.29-fold increased likelihood of being at blood pressure goal compared with minority women who received usual care.
Discussion
This controlled study of a systematic hospital-based educational intervention among high-risk women to improve adherence to AHA/ACC secondary prevention goals demonstrated that (1) minority women were less likely to meet national standards for risk factor management upon hospitalization, (2) although a systematic educational intervention was not associated with significant benefits in the overall study population, minority women who received the intervention had significant improvements in blood pressure control compared with usual care, and white women who received the intervention were more likely to use beta-blockers compared with the usual care group, and (3) secular trends in the control group showed that rates of nonsmoking, lipid control, exercise, and use of ACE inhibitors improved substantially 6 months after hospitalization. Despite the positive trends, our research documents exceptionally low compliance with lifestyle recommendations.
Our data are consistent with other studies that have evaluated modest interventions to improve risk factor control among patients with CHD.13,15,27 In a randomized trial of 201 patients with an acute coronary event assigned to either case management with counseling by a physician or usual care, there were no significant differences in lipids, blood pressure, glucose, BMI, or number of smokers between the two groups after 18 months of follow-up.13 Although counseling was provided by a physician in contrast to a nonphysician as used in our study, both designs preserved the patient and primary care physician relationship by providing summarized reports of progress toward standard goals. Similarly, among 540 smokers hospitalized with CHD, a brief nursing intervention with support and reinforcement was not associated with greater smoking cessation compared with usual care.15 Among 375 patients with CHD randomized to a nurse-based educational intervention that focused on patient empowerment, knowledge of LDL-C targets increased, but cholesterol management was not improved compared with a usual care group of 381 patients 1 year after hospitalization.27 Unlike our trial, these studies were conducted in primarily white populations and did not evaluate subgroup interactions.
Interventions that included a nurse practitioner to augment physician care by providing counseling and prescriptions for lipid-lowering medications have resulted in improved lipids and lifestyle factors.11,14 A comprehensive, multifactorial residential program with systematic maintenance was associated with significant improvements in lipid levels, exercise capacity, and BMI in patients with a recent history of an acute coronary event or revascularization procedure.28 These data suggest that interventions more intensive than that we employed or that have the flexibility to prescribe therapy may be more effective in improving adherence to secondary prevention goals than educational and patient enabling strategies.
Hospital protocols structured to uniformly prescribe preventive medications have shown success with improved adherence at discharge; however, most of these have not been randomized and controlled.8,9,29 The Cardiac Hospitalization Atherosclerosis Management Program (CHAMP) study was one of the first attempts to evaluate a systems approach to improve secondary prevention.8 The intervention focused on initiation of preventive therapies during hospitalization using standard algorithms. A before and after CHAMP analysis showed significant improvement in rates of compliance at discharge, with a sustained effect of 58% of patients achieving an LDL goal ≤100 mg/dL (≤2.59 mmol/L) compared with 6% in the pre-CHAMP period (p < 0.001). The Guidelines Applied in Practice (GAP) Initiative showed that an intervention using standard orders, clinical pathways, pocket guides, chart stickers, performance charts, and patient information and discharge forms increased rates of aspirin use but not other preventive care quality indicators in participating hospitals compared with hospitals that volunteered for the program but were not selected.9 A decentralized chest pain unit with standardized optional admission orders for aspirin, beta-blockers, ACE inhibitor, and statin therapy significantly increased rates of statin therapy at discharge compared with the pre-intervention period.29 A lack of significant improvement in other preventive medications may have reflected high baseline rates of use. Likewise, in our study, the majority of women admitted were prescribed aspirin/antiplatelet therapy, beta-blockers, and ACE inhibitors, and the lack of impact of our intervention may also have been due to a ceiling effect.
Our baseline data documenting that minority women with CHD are less likely to meet preventive standards than are white women are consistent with data from the Heart and Estrogen/Progestin Replacement Study (HERS) showing black women with CHD had higher rates of hypertension, diabetes, and hypercholesterolemia and were less likely to receive aspirin and statins than white women.7 The HERS analysis was limited to postmenopausal black women and recruited subjects between 1993 and 1994. Our recruitment occurred nearly 10 years later and extends their findings to a more diverse and contemporary cohort.
The results of our analysis between minority and white women suggested that there was a differential impact of the intervention between subpopulations related to blood pressure control and medication adherence. The observation that 6-month blood pressure levels were worse than baseline levels for all groups should be interpreted with caution, as many patients were treated aggressively during hospitalization for an acute event, and lower baseline blood pressure likely reflects intensive monitoring and treatment with blood pressure medication or sedatives during hospitalization. It may also be reflective of the finding that sicker women (i.e., participants with a documented history of CHD) were more likely to complete the trial. We hypothesize that less access to care among minorities and poorer background rates of preventive care may have enhanced the efficacy of our intervention in this population. A meta-analysis of cardiac education programs prior to 1990 demonstrated a measurable impact on blood pressure and other risk factors related to lifestyle.30 These studies were conducted before the release of many major prevention trials and suggest that education interventions to improve risk factor control may be useful against a background of minimal preventive medical management, lending support to a differential impact among minorities in our study, where lower rates of preventive care were clearly documented.
A major strength of our trial was the high participation rate, with >50% representation by minorities; however, our study had limitations. We had poor rates of compliance with return visits and did not have complete data available on a substantial proportion of subjects. Although the follow-up was nondifferential with respect to group assignment, our power to demonstrate a significant impact of the intervention was reduced; however, several positive trends were observed. Incomplete data are a common problem in lifestyle intervention trials, and there are no adequate analytic methods to address the problem that do not introduce potential bias.31 Therefore, we maintained an intention-to-treat approach to the analysis. Not all subjects had follow-up measurements conducted at the clinical site, but given the real world nature of the study, the outcomes assessed by local physicians were important. Moreover, the categorical nature of prevention goals makes it unlikely that measurement error would lead to significant change in goal status. The likelihood of differential misclassification is small because rates of central and local measurements were similar between intervention and usual care groups. The difficulty in having subjects return for follow-up in our study despite multiple attempts underscores the challenges of studies that include older women and ethnic minorities. Barriers to follow-up should be addressed in future research, as this may have important implications for clinical outcomes in high-risk populations.
Conclusions
We demonstrated that minority women hospitalized with CHD are less likely than white women to meet national standards for prevention and that a systematic intervention to improve secondary prevention guideline adherence was not significantly better than usual care for women overall at 6 months, although minority women benefited to a greater degree than white women with respect to blood pressure control. CHD remains the leading killer of women and disproportionately affects minorities, as does hypertension.32,33 The AHA has recently published professional and lay Evidence-Based Guidelines for the Prevention of Cardiovascular Disease in Women to help physicians and the public improve lifestyle and risk factor control.34 Our findings suggest that education about prevention and the guidelines is particularly important among ethnic minorities.
Acknowledgments
This study was funded by Aetna and the Quality Care Research Fund and supported by the NIH-funded General Clinical Research Centers at Columbia University and Weill Medical College of Cornell University at NewYork-Presbyterian Hospital. L.M. was supported by an NIH research career award (K08 03681). We thank Cholestech Corporation, Hayward, California, for donating cholesterol measurement supplies. We appreciate the input of Melvin Rubenfire, M.D., Carole McGillen, R.N., Laura Melton, R.N., Robert Allan, Ph.D., and Abby Jacobson, R.N., into the study design and the efforts of Maria Cornelio, M.A., for medical translation. We also acknowledge Alison Keenan, M.D., Johanny Almonte, and Aline Nguyen, M.P.H., for their significant contributions as prevention facilitators. The assistance of Lisa Rehm to the study team is greatly appreciated.
Disclosure Statement
The authors have no conflicts of interest to report.
References
- 1.Smith S. Blair S. Bonow R, et al. American Heart Association/American College of Cardiology Scientific Statement: AHA/ACC guidelines for preventing heart attack and death in patients with atherosclerotic cardiovascular disease: 2001 update. A statement for health care professionals from the American Heart Association and the American College of Cardiology. Circulation. 2001;104:1577–1579. doi: 10.1161/hc3801.097475. [DOI] [PubMed] [Google Scholar]
- 2.EUROASPIRE I and II Group. Clinical reality of coronary prevention guidelines: A comparison of EUROASPIRE I and II in nine countries. Lancet. 2001;357:995–1001. doi: 10.1016/s0140-6736(00)04235-5. [DOI] [PubMed] [Google Scholar]
- 3.Pearson TA. Laurora I. Chu H. Kafonek S. The Lipid Treatment Assessment Project (L-TAP): A multicenter survey to evaluate the percentages of dyslipidemic patients receiving lipid-lowering therapy and achieving low-density lipoprotein cholesterol goals. Arch Intern Med. 2000;160:459–467. doi: 10.1001/archinte.160.4.459. [DOI] [PubMed] [Google Scholar]
- 4.Benjamin E. Smith S. Cooper R. Hill M. Luepker R. Task Force #1—Magnitude of the prevention problem: Opportunities and challenges. 33rd Bethesda Conference. J Am Coll Cardiol. 2002;40:588–602. doi: 10.1016/s0735-1097(02)02082-x. [DOI] [PubMed] [Google Scholar]
- 5.Thomas R. Miller N. Lamendola C, et al. National survey on gender differences in cardiac rehabilitation programs: Patient characteristics and enrollment patterns. J Cardiopulm Rehabil. 1995;16:402–412. doi: 10.1097/00008483-199611000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Miller M. Bryington R. Hunninghake D, et al. for the Prospective Randomized Evaluation of the Vascular Effects of Norvasc Trial (PREVENT) Investigators. Sex bias and underutilization of lipid-lowering therapy in patients with coronary artery disease at academic medical centers in the United States and Canada. Arch Intern Med. 2000;160:343–347. doi: 10.1001/archinte.160.3.343. [DOI] [PubMed] [Google Scholar]
- 7.Jha A. Varosy P. Kanaya A, et al. Differences in medical care and disease outcomes among black and white women with heart disease. Circulation. 2003;108:1089–1094. doi: 10.1161/01.CIR.0000085994.38132.E5. [DOI] [PubMed] [Google Scholar]
- 8.Fonarow GC. Gawlinski A. Moughrabi S. Tillisch JH. Improved treatment of coronary heart disease by implementation of a Cardiac Hospitalization Atherosclerosis Management Program (CHAMP) Am J Cardiol. 2001;87:819–822. doi: 10.1016/s0002-9149(00)01519-8. [DOI] [PubMed] [Google Scholar]
- 9.Mehta RH. Montoye CK. Gallogly M, et al. Improving quality of care for acute myocardial infarction: The Guidelines Applied in Practice (GAP) Initiative. JAMA. 2002;287:1269–1276. doi: 10.1001/jama.287.10.1269. [DOI] [PubMed] [Google Scholar]
- 10.Allen JK. Coronary risk factor modification in women after coronary artery bypass surgery. Nurs Res. 1996;45:260–265. doi: 10.1097/00006199-199609000-00002. [DOI] [PubMed] [Google Scholar]
- 11.DeBusk RF. Miller NH. Superko HR, et al. A case-management system for coronary risk factor modification after acute myocardial infarction. Ann Intern Med. 1994;120:721–729. doi: 10.7326/0003-4819-120-9-199405010-00001. [DOI] [PubMed] [Google Scholar]
- 12.Carlsson R. Lindberg G. Westin L. Israelsson B. Influence of coronary nursing management follow up on lifestyle after acute myocardial infarction. Heart. 1997;77:256–259. doi: 10.1136/hrt.77.3.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nordmann A. Heilmbauer I. Walker T. Martina B. Battegay E. A case-management program of medium intensity does not improve cardiovascular risk factor control in coronary artery disease patients: The Heartcare I trial. Am J Med. 2001;110:543–550. doi: 10.1016/s0002-9343(01)00682-9. [DOI] [PubMed] [Google Scholar]
- 14.Allen JK. Blumenthal RS. Margolis S. Young DR. Miller ER., 3rd Kelly K. Nurse case management of hypercholesterolemia in patients with coronary heart disease: Results of a randomized clinical trial. Am Heart J. 2002;144:678–686. doi: 10.1067/mhj.2002.124837. [DOI] [PubMed] [Google Scholar]
- 15.Hajek P. Taylor TZ. Mills P. Brief intervention during hospital admission to help patients to give up smoking after myocardial infarction and bypass surgery: Randomised controlled trial. BMJ. 2002;324:87–89. doi: 10.1136/bmj.324.7329.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mosca L. Grundy S. Judelson J, et al. AHA/ACC Consensus Panel Statement: A guide to preventive cardiology for women. Circulation. 1999;99:2480–2484. doi: 10.1161/01.cir.99.18.2480. [DOI] [PubMed] [Google Scholar]
- 17.Bandura A. Self-efficacy mechanism in physiological activation and health-promoting behavior. In: Madden J, editor. Neurobiology of learning, emotion and affect. IV. New York: Raven; 1991. pp. 229–269. [Google Scholar]
- 18.Bandura A. Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. Self-efficacy; pp. 393–398. [Google Scholar]
- 19.Goldstein MG. DePue J. Kazuira A. Models for provider-patient interaction: Applications to health behavior change. In: Shumaker SA, editor; Schon EB, editor; Ockene JK, editor; McBeem WL, editor. The handbook of health behavior change. 2nd. New York: Springer; 1998. pp. 85–113. [Google Scholar]
- 20.American College of Sports Medicine's guidelines for exercise testing and prescription. 5th. Baltimore: Williams & Wilkins; 1995. [Google Scholar]
- 21.Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III), final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 22.Fiore MC. Bailey WC. Cohen SJ, et al. Quick reference guide for clinicians. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service; 2000. Treating tobacco use and dependence. [Google Scholar]
- 23.The sixth report of the Joint National Committee on prevention detection, evaluation, and treatment of high blood pressure. Washington: National Institutes of Health Publication; 1997. National Health Institute, National Heart, Lung and Blood Institute, Program National High Blood Pressure Education. [Google Scholar]
- 24.Lohman TC. Roche AF. Martorell R. Anthropometric standardization reference manual. Champaign, IL: Human Kinetics Books; 1988. [Google Scholar]
- 25.Middleton E. Morice A. Breath carbon monoxide as an indication of smoking habit. Chest. 2000;117:758–763. doi: 10.1378/chest.117.3.758. [DOI] [PubMed] [Google Scholar]
- 26.Cobbaert C. Boerma GJ. Lindemans J. Evaluation of the Cholestech L.D.X. desktop analyser for cholesterol, HDL-cholesterol, and triacylglycerols in heparinized venous blood. Eur J Clin Chem Clin Biochem. 1994;32:391–394. [PubMed] [Google Scholar]
- 27.Lichtman JH. Amatruda J. Yaari S, et al. A clinical trial of an educational intervention to achieve recommended cholesterol levels in patients with coronary artery disease. Am Heart J. 2004;147:522–528. doi: 10.1016/j.ahj.2003.06.003. [DOI] [PubMed] [Google Scholar]
- 28.Lisspers J. Hofman-Bang C. Nordlander R, et al. Multifactorial evaluation of a program for lifestyle behavior change in rehabilitation and secondary prevention of coronary artery disease. Scand Cardiovasc J. 1999;33:9–16. doi: 10.1080/14017439950141975. [DOI] [PubMed] [Google Scholar]
- 29.Biviano A. Rabbani L. Paultre F, et al. Usefulness of an acute coronary syndrome pathway to improve adherence to secondary prevention guidelines. Am J Cardiol. 2003;91:1248–1250. doi: 10.1016/s0002-9149(03)00276-5. [DOI] [PubMed] [Google Scholar]
- 30.Mullen PD. Mains DA. Velez R. A meta-analysis of controlled trials of cardiac patient education. Patient Educ Couns. 1992;19:143–162. doi: 10.1016/0738-3991(92)90194-n. [DOI] [PubMed] [Google Scholar]
- 31.Ware JH. Interpreting incomplete data in studies of diet and weight loss. N Engl J Med. 2003;348(21):2136–2137. doi: 10.1056/NEJMe030054. [DOI] [PubMed] [Google Scholar]
- 32.Cooper R. Cutler J. Desvigne-Nickens P, et al. Trends and disparities in coronary heart disease, stroke, and other cardiovascular diseases in the United States: Findings of the National Conference on CVD Prevention. Circulation. 2000;102:3137–3147. doi: 10.1161/01.cir.102.25.3137. [DOI] [PubMed] [Google Scholar]
- 33.American Heart Association. Heart and stroke statistical update. 2003. www.americanheart.org www.americanheart.org
- 34.Mosca L. Banka CL. Benjamin EJ, et al. Evidence-based guidelines for cardiovascular disease prevention in women: 2007 update. Circulation. 2007;115:1481–1501. doi: 10.1161/CIRCULATIONAHA.107.181546. [DOI] [PubMed] [Google Scholar]