Summary
Background
It is well known that citizens of developed countries are more likely to be overweight than they were 20 years ago. The most serious health problems are not associated with overweight or moderate obesity, however, but with clinically severe or morbid obesity (e.g. more than 100 pounds (45 kg) overweight). There is no reason to expect that morbid obesity trends parallel overweight or moderate obesity. If morbid obesity is a rare pathological condition that has biological causes, the more than 10-fold increase in bariatric surgery procedures over the past eight years in the USA could have even lowered the prevalence of morbid obesity—and may very well stem the problem in other countries.
Objective
To estimate trends for extreme weight categories (BMI>40 and >50) for the period between 1986 and 2005 in the USA, and to investigate whether trends have changed since 2000.
Methods
Data from The Behavioral Risk Factor Surveillance System (a random-digit telephone survey of the household population of the USA), for the period from 1986 to 2005, were analysed. The main outcome measure was body mass index (BMI), calculated from self-reported weight and height.
Results
From 2000 to 2005, the prevalence of obesity (self-reported BMI over 30) increased by 24%. However, the prevalence of a (self-reported) BMI over 40 (about 100 pounds (45 kg) overweight) increased by 50% and the prevalence of a BMI over 50 increased by 75%, two and three times faster, respectively. The heaviest BMI groups have been increasing at the fastest rates for 20 years.
Conclusions
The prevalence of clinically severe obesity is increasing at a much faster rate among adults in the USA than is the prevalence of moderate obesity. This is consistent with the public health idea that the population weight distribution is shifting, which disproportionately increases extreme weight categories. Because comorbidities and resulting service use are much higher among severely obese individuals, the widely published trends for overweight/obesity underestimate the consequences for population health. The aggressive and costly expansion of bariatric surgery in recent years has had no visible effect on containing morbid obesity rates in the USA.
Keywords: Obesity, Morbid obesity, Obesity trends, Public health, BMI, Bariatric
Introduction
In the USA, different studies have documented that most Americans are overweight (a body mass index (BMI) over 25) or obese (BMI≥30). About one in four adult Americans would be classified as obese, based on self-reported weight; more than one in three would be classified as obese, based on objectively measured weight. These rates have roughly tripled in the past 20 years.1–4 In England, one in five adults are obese and that rate has also tripled over the last 20 years, although starting from lower levels of prevalence than the USA.5,6
The typical definition of obesity, a BMI of over 30 (which is 35 pounds (16 kg) overweight at a height of 5′9″ (175 cm)), obscures the heterogeneity of this group. Severely obese individuals who are 100 or 200 pounds (45 or 90 kg) or more overweight have much more serious health problems and they encounter very different challenges in the health-care system than the majority of obese individuals. For a person 5′9″ (175 cm) tall, being 100 pounds (45 kg) overweight translates into a BMI of 40. Among middle-aged adults, a BMI of 35–40 is associated with twice the increase in healthcare expenditure above normal weight (about a 50% increase) than a BMI of 30–35 (about a 25% increase); a BMI of over 40 doubles healthcare costs (about 100% higher costs above those of normal weight).7
Does severe obesity simply parallel the general trend in obesity? Or is there something fundamentally different about clinically severe or morbid obesity? While trends for lower weight categories have been published repeatedly, there are no similar updates for severe obesity, partly because such estimates require large population samples. An earlier study reported that before 2000, the prevalence of higher levels of obesity increased faster in the USA than the prevalence of moderate obesity.8 This paper updates estimates through 2005. Recent years are of particular interest, given the dramatic expansion of bariatric surgery, which so far is the only effective treatment for morbid obesity. In the USA, the number of bariatric surgical procedures increased from 13 000 in 1998, to over 100 000 in 2003.9 The president of the American Society for Bariatric Surgery, estimates that 175 000–200 000 weight-loss procedures will be performed in 2006,10 more than a 10-fold increase in eight years.
There are two conflicting opinions about trends in clinically severe or morbid obesity. Clinicians tend to consider morbid obesity a rare pathological condition that is not affected by behavioural changes in the general population. This view would suggest that the incidence of morbid obesity changes little over time and that a new efficacious treatment could make a large difference in the prevalence of this condition. Epidemiologists tend to lean towards the opposite view, namely that severe obesity is part of the general population distribution and small increases in the population BMI would have proportionally larger effects in the extreme tail.11 Which of those views better describes reality is an empirical question, but the answer has major ramifications for public health and healthcare systems. If the epidemiological view is correct, then a medical approach to treating morbid obesity in order to reduce its prevalence will be futile. In contrast, a public health approach that focuses on reducing weight gain across the whole population is more likely to contain morbid obesity as well, even without explicitly targeting it.
Methods
This study analysed data from the Behavioral Risk Factor Surveillance System (BRFSS), a cross-sectional telephone survey of non-institutionalized adults in the USA, for the period between 1986 and 2005. The BRFSS has been used for tracking health behaviours over time and study details are documented elsewhere.12
Individuals were classified into weight categories based on their BMI (weight in kilograms divided by the square of height in meters) calculated from self-reported weight and height. In addition to the standard ‘obese’ category, defined as a BMI of greater than or equal to 30 kg/m2, the main groups of interest were more extreme categories: BMI≥35, BMI≥40 (often referred to as morbid obesity and roughly corresponding to 100 pounds (45 kg) overweight), BMI≥45, and BMI≥50 (sometimes referred to as super obesity). There is a well-known tendency towards under-reporting weight and over-reporting height.13–15 The under-reporting of weight increases with weight and absolute levels of prevalence are therefore lower than if BMI were calculated by independent measurement. The effect on trends is probably minor, but the bias will underestimate the increase among the heaviest groups.
The statistical analysis used individual-level logistic regression with an indicator of a specific weight category as the dependent variable. Time trend was measured as a linear spline (in the log odds) with knots at 1991 and 1996, and 2001 (i.e., linear trends within each 5-year period, but trends can differ between 1986 and 1990, 1991 and 1995, 1996 and 2000, 2001 and 2005). The spline function smoothes estimates compared to year indicators, and was mainly needed because of the small sample sizes in the early years and in the heaviest BMI groups. The results were adjusted for socio-demographic changes to isolate the unique trend in obesity rates. Regressors included: age (in 5-year intervals), educational achievement (less than high school, high school, some college, college degree), racial group (white, black, Hispanic, other), and gender. State indicators were included to control for the changing survey participation by states over time. Tests were based on the regression model and all results were considered statistically significant at P<0.01 unless indicated otherwise. The adjusted results were based on the sociodemographic characteristics in the year 2005 survey.
The study design implies several limitations. First, telephone coverage varies by state and also by subpopulation. Telephone coverage averaged 97.6% for US states as a whole in 2003 (the midpoint of the new analysis), but non-coverage ranges from 1.1% in Connecticut and New Hampshire, to 6.6% in Mississippi.12 The second limitation, inherent in every form of survey data, is non-response. Biases may change over time and noticeable declines in participation or response rates have been reported, especially since the mid-1990s.16,17 A meta-analysis of research papers in epidemiology and public health found that participation rates during 1970–2003 changed between −0.54% and −0.67% per year in similar studies.17 The BRFSS was not exempt from this trend and the cooperation rate (median across states) dropped from 69.8% in 1996 to 53.2% in 2000.12 Since then, aggressive attempts to stem this decline raised the cooperation rate to 58.7% in 2005. Because sociodemographic characteristics of responders differ from the underlying population, post-stratification weights are used to adjust for telephone non-coverage and non-response.12 Despite strong sociodemographic patterns in response rates, biases from non-response were found to be minor in a nutritional survey.18 In another study of non-responders, sedentary lifestyle was found to be higher among initial non-responders.19 To the extent that this bias is relevant, it would suggest that the results here underestimate trends.
A subtler issue is that the social acceptability of obesity may change and alter biases in self-reported weight. This hypothesis can be tested with the National Health and Nutrition Examination Survey (NHANES), which collects both self-report and objectively measured height and weight over time.20 Because the sample size is much smaller (about 5000 versus 300 000 in BRFSS), NHANES cannot be used to estimate changes in morbid obesity rates. However, there is no evidence that people have become more willing to report higher weights. Instead, the gap between self-report and objective measured BMI is increasing over time and was 0.51 units in 1999/2000 and 0.56 units in 2003/2004. This increase in the gap remains statistically significant (P<0.05) even after controlling for objectively measured BMI. Thus, if anything, the results here underestimate the increases in each weight category compared to data based on objectively measured height and weight.
Results
Table 1 gives adjusted estimates of prevalence from 2001 to 2005 and percentage increases compared to 2000; the higher the BMI group, the faster the increase. The prevalence of a BMI>30 increased by 24% between 2000 and 2005, but the prevalence of a BMI over 40 increased twice as fast (52% higher in 2005 than in 2000) and the prevalence of a BMI over 50 increased three times as fast (75% higher in 2005 than in 2000). The numbers differ slightly from descriptive statistics because they are adjusted for changes in population demographics.
Table 1.
Prevalence of different levels of obesity and percentage increase since 2000.
| Year | Prevalence in percent |
Increase over prevalence in 2000 (%) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| BMI>30 | BMI>35 | BMI>40 | BMI>45 | BMI>50 | BMI>30 | BMI>35 | BMI>40 | BMI>45 | BMI>50 | |
| 2001 | 20.7 | 6.54 | 2.20 | 0.75 | 0.27 | 4.6 | 6.9 | 8.9 | 10.6 | 12.5 |
| 2002 | 21.6 | 6.98 | 2.39 | 0.83 | 0.30 | 9.2 | 14.1 | 18.3 | 22.2 | 25.0 |
| 2003 | 22.6 | 7.45 | 2.60 | 0.92 | 0.34 | 14.0 | 21.7 | 28.7 | 35.5 | 41.7 |
| 2004 | 23.6 | 7.95 | 2.83 | 1.02 | 0.38 | 19.0 | 29.9 | 40.1 | 50.2 | 58.3 |
| 2005 | 24.6 | 8.48 | 3.07 | 1.13 | 0.42 | 24.0 | 38.6 | 52.0 | 66.4 | 75.0 |
Source: Behavioral Risk Factor Surveillance Survey; results adjusted for changes in population demographics to be comparable to 2005 demographics.
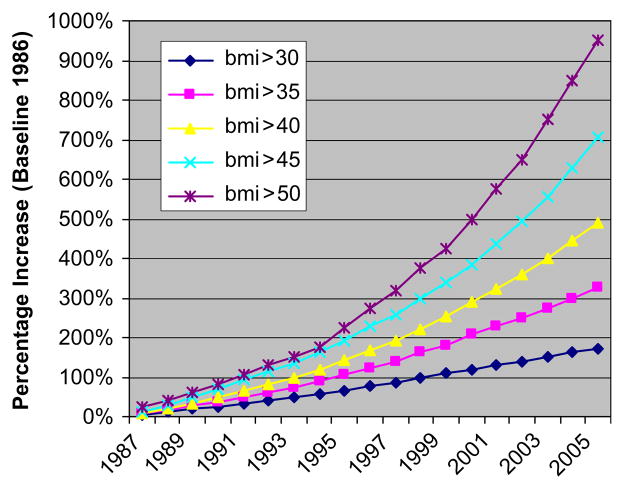
Figure 1 shows the long-term picture over the last two decades. The time trend for the BMI>30 group is significantly lower than for the BMI>40 group, which in turn is significantly lower than for the BMI>50 group. For the BMI>30 group, the time trend has become significantly smaller since 2000, although the difference is so small that plotting obesity rates still looks like constant exponential growth. In contrast, there is no significant change in the time trend for any of the severe BMI groups (BMI>40, BMI>45, BMI>50) before and after 2000.
Figure 1.
Percentage increase in BMI categories since 1986 (source: Behavioral Risk Factor Surveillance Survey; results adjusted for changes in population demographics to be comparable to 2005 demographics).
Discussion
Reports that the majority of adults are now overweight or obese have raised the public profile of the obesity epidemic in Europe and the USA. Milestones included governmental reports such as Tackling obesity in England by the National Audit Office, or the Call to action by the Surgeon General in the USA.5,21 Nevertheless, the most dramatic part of the ‘obesity epidemic’ has received very little attention in either those reports or the public press, namely that the prevalence of morbid obesity is increasing much faster than the prevalence of obesity.
Morbid obesity, far from being a pathological condition that only affects a fixed percentage of genetically vulnerable individuals, appears to be an integral part of the USA population’s weight distribution. As the whole population shifts to the right, i.e., toward higher weight, the extreme categories grow the fastest. The traditional clinical approach of targeting high-risk cases, in particular bariatric surgery, is only temporary and palliative from a population perspective in this situation, but cannot stem the trend. This offers new business opportunities for providers specializing in treating severe obesity, but the social costs are large. The explosive increase in bariatric surgical procedures has made no noticeable dent in the prevalence of morbid obesity. Indeed, since 2000, the growth rate in the prevalence of a BMI>40 has been twice the growth rate of the prevalence of moderate obesity, whereas the growth rate of the prevalence of a BMI>50 has been three times the growth rate of the prevalence of moderate obesity.
Can this trend be reversed? Achieving lasting health behaviour change is difficult and rarely achieved by exhorting individuals to exercise more, eat healthier, stop smoking, or drink responsibly. Car-friendly (and bike/pedestrian–hostile) urban developments, desk jobs, television viewing, and relatively cheap calorie-dense foods, are some of the recent environmental changes that have changed relative prices of caloric intake and physical activity. Arguably, environmental interventions to counter the obesity epidemic, similar to tobacco and alcohol policy, would be needed. However, this appears to be politically less feasible at the moment than expanding bariatric surgery programmes or treating the ensuing complications of obesity.
References
- 1.Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289:76–9. doi: 10.1001/jama.289.1.76. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 3.National Center for Health Statistics. [accessed 13 September 2006];Health, United States. 2005 Available at: < http://www.cdc.gov/nchs/hus.htm>.
- 4.Sturm R. The effects of obesity, smoking and drinking on medical problems and costs. Health Aff. 2002;21:245–53. doi: 10.1377/hlthaff.21.2.245. [DOI] [PubMed] [Google Scholar]
- 5.National Audit Office. Report by the Comptroller and Auditor General. London: The Stationary Office; Feb, 2001. Tackling obesity in England. [Google Scholar]
- 6.Rennie KL, Jebb SA. Prevalence of obesity in Great Britain. Obes Rev. 2005;6:11–2. doi: 10.1111/j.1467-789X.2005.00164.x. [DOI] [PubMed] [Google Scholar]
- 7.Andreyeva T, Sturm R, Ringel JS. Moderate and severe obesity have large differences in health care costs. Obes Res. 2004;12:1936–43. doi: 10.1038/oby.2004.243. [DOI] [PubMed] [Google Scholar]
- 8.Sturm R. Increases in clinically severe obesity in the United States, 1986–2000. Arch Intern Med. 2003;163:2146–8. doi: 10.1001/archinte.163.18.2146. [DOI] [PubMed] [Google Scholar]
- 9.Santry HP, Gillen DL, Lauderdale DS. Trends in bariatric surgical procedures. JAMA. 2005;294:1909–17. doi: 10.1001/jama.294.15.1909. [DOI] [PubMed] [Google Scholar]
- 10.Pear R. Obesity surgery often leads to complications, study says. New York Times. 2006 July 24; [Google Scholar]
- 11.Rose G. Sick individuals and sick populations. Int J Epidemiol. 1985;14:32–8. doi: 10.1093/ije/14.1.32. reprinted in Int J Epidemiol 2001;30:427–32. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control. [accessed 26 November 2006];Behavioral Risk Factor Surveillance Survey. Available at: < http://www.cdc.gov/brfss/>.
- 13.Palta M, Prineas RJ, Berman R, Hannan P. Comparison of self-reported and measured height and weight. Am J Epidemiol. 1982;115:223–30. doi: 10.1093/oxfordjournals.aje.a113294. [DOI] [PubMed] [Google Scholar]
- 14.Stunkard AJ, Albaun JM. The accuracy of self-reported weights. Am J Clin Nutr. 1981;34:1593–9. doi: 10.1093/ajcn/34.8.1593. [DOI] [PubMed] [Google Scholar]
- 15.Kuczmarski MF, Kuczmarski RJ, Najjar M. Effects of age on validity of self-reported height, weight, and body mass index: findings from the Third National Health and Nutrition Examination Survey, 1988–1994. J Am Diet Assoc. 2001;101:28–34. doi: 10.1016/S0002-8223(01)00008-6. [DOI] [PubMed] [Google Scholar]
- 16.Curtin R, Presser S, Singer E. Changes in telephone survey nonresponse over the past quarter century. Public Opin Q. 2005;69:87–98. [Google Scholar]
- 17.Morton LM, Cahill J, Hartge P. Reporting participation in epidemiologic studies: a survey of practice. Am J Epidemiol. 2006;163:197–203. doi: 10.1093/aje/kwj036. [DOI] [PubMed] [Google Scholar]
- 18.Turrell G, Patterson C, Oldenburg B, Gould T, Roy MA. The socio-economic patterning of survey participation and non-response error in a multilevel study of food purchasing behaviour: area- and individual-level characteristics. Public Health Nutr. 2003;6:181–9. doi: 10.1079/PHN2002415. [DOI] [PubMed] [Google Scholar]
- 19.Hill A, Roberts J, Ewings P, Gunnell D. Non-response bias in a lifestyle survey. J Public Health Med. 1997;19:203–7. doi: 10.1093/oxfordjournals.pubmed.a024610. [DOI] [PubMed] [Google Scholar]
- 20.National Center for Health Statistics. [accessed 27 November 2006];National Health and Nutrition Examination Survey. Available at: < http://www.cdc.gov/nchs/nhanes.htm>.
- 21.US Department of Health and Human Services. The Surgeon General’s call to action to prevent and decrease overweight and obesity. Rockville, MD: US Department of Health and Human Services, Public Health Service, Office of the Surgeon General; 2001. [PubMed] [Google Scholar]