Abstract
Objectives: To assess the relation between white coat hypertension and alterations of left ventricular structure and function.
Design: Cross sectional survey.
Setting: Augsburg, Germany.
Subjects: 1677 subjects, aged 25 to 74 years, who participated in an echocardiographic substudy of the monitoring of trends and determinants in cardiovascular disease Augsburg study during 1994-5.
Outcome measures: Blood pressure measurements and M mode, two dimensional, and Doppler echocardiography. After at least 30 minutes’ rest blood pressure was measured three times by a technician, and once by a physician after echocardiography. Subjects were classified as normotensive (technician <140/90 mm Hg, physician <160/95 mm Hg; n=849), white coat hypertensive (technician <140/90 mm Hg, physician ⩾160/95 mm Hg; n=160), mildly hypertensive (technician ⩾140/90 mm Hg, physician <160/95 mm Hg; n=129), and sustained hypertensive (taking antihypertensive drugs or blood pressure measured by a technican ⩾140/90 mm Hg, and physician ⩾160/95 mm Hg; n=538).
Results: White coat hypertension was more common in men than women (10.9% versus 8.2% respectively) and positively related to age and body mass index. After adjustment for these variables, white coat hypertension was associated with an increase in left ventricular mass and an increased prevalence of left ventricular hypertrophy (odds ratio 1.9, 95% confidence interval 1.2 to 3.2; P=0.009) compared with normotensive patients. The increase in left ventricular mass was secondary to significantly increased septal and posterior wall thicknesses whereas end diastolic diameters were similar in both groups with white coat hypertension or normotension. Additionally, the systolic white coat effect (difference between blood pressures recorded by a technician and physician) was associated with increased left ventricular mass and increased prevalence of left ventricular hypertrophy (P<0.05 each). Values for systolic left ventricular function (M mode fractional shortening) were above normal in subjects with white coat hypertension whereas diastolic filling and left atrial size were similar to those in normotension.
Conclusion: About 10% of the general population show exaggerated inotropic and blood pressure responses when mildly stressed. This is associated with an increased risk of left ventricular hypertrophy.
Key messages
About 10% of the general population display white coat hypertension
After adjustment for age, body mass index, and baseline blood pressure, white coat hypertension is associated with increased left ventricular mass and increased risk of left ventricular hypertrophy
In white coat hypertension, after adjustment for covariates, systolic function has values above normal whereas diastolic filling is unchanged
White coat hypertension cannot be dismissed as a benign condition
Introduction
A physical examination by a physician may cause a rise in the patient’s blood pressure. Individuals showing such responses are considered to have white coat hypertension if their blood pressure reaches a hypertensive level when measured in the doctor’s practice but remains normal in an informal setting.1 The clinical implications of white coat hypertension are unclear and the subject of an ongoing debate.2 Compared with patients with sustained hypertension, individuals with white coat hypertension have less end organ damage3,4 and a better prognosis.5 It should not, however, be assumed that white coat hypertension is similar to normotension and therefore harmless to the heart.6 In fact more recent studies including larger numbers of normotensive individuals have raised doubts about white coat hypertension as a benign condition.7–10 This is supported by an epidemiological study that showed an unfavourable risk profile in young adults with white coat hypertension including a high prevalence of familial, haemodynamic, and metabolic risk factors.11
Cardiac structure and function in subjects with white coat hypertension have not been studied at a population based level. Previous studies on this topic are not conclusive, probably because (a) the study population was small,12,13 (b) analyses did not adjust for anthropometric characteristics of subjects with white coat hypertension, and, (c) different definitions of white coat hypertension were used.3,4,6,8–10 Perhaps most importantly these studies did not address the risk of left ventricular hypertrophy in patients with white coat hypertension. As echocardiographic evidence of left ventricular hypertrophy is an independent predictor of overall mortality,14 it has been proposed as a pathophysiological marker for white coat hypertension.2 We investigated the association of white coat hypertension with left ventricular hypertrophy, and echocardiographic variables of left ventricular systolic and diastolic function, in a population based setting.
Subjects and methods
Augsburg study
The monitoring of trends and determinants in cardiovascular disease (MONICA) Augsburg study was conducted as part of the international collaborative World Health Organisation MONICA project. This study investigated cardiovascular risk factors of randomly selected subjects from Augsburg in cross sectional surveys.15 We performed echocardiographic examinations in 845 men and 832 women, aged 25 to 74 years, who participated in an echocardiographic substudy of the third Augsburg survey during 1994-5 (participation rate 70.6%).
All participants were interviewed to ascertain details of their personal and family medical history, life style and nutrition, health behaviour, and psychosocial factors. The interview and examination room contained armchairs and a table to disguise the clinical setting.16 Technicians were trained and certified in accordance with the MONICA protocol.16 They did not wear white coats and were trained to avoid tension and anxiety in the participants. Frequent standardised quality controls of blood pressure measurements were undertaken. Technicians were retrained and recertified if they showed weaknesses. Physicians were also trained to obtain standardised blood pressure measurements. Before the first blood pressure measurement, subjects remained in a sitting position for at least 30 minutes. Blood pressure was measured under standardised conditions at the right arm with a random zero manometer. Participants were told the results only after the third reading had been taken. The mean of the second and third measurement was used for the present analyses. Previous studies, including the first and second Augsburg MONICA surveys, showed that this technique allows a good estimation of blood pressure at rest.1,15–17
Heart rate was obtained by electrocardiography, performed by a technician before echocardiography. After the echocardiographic examination a single blood pressure measurement was taken by a physician wearing a white coat who was introduced to the participants as a cardiologist. Blood pressure measurements by both technicians and physicians were carried out on the same day, with a maximum of 60 minutes between the measurements.
As a standard definition of white coat hypertension is lacking we classed subjects as normotensive if their blood pressures were <140/90 mm Hg when measured by a technician and <160/95 mm Hg when measured by a physician.2,4,8 These cut off values were chosen according to the WHO criteria for normotension, borderline hypertension, and sustained hypertension.18 We classed subjects as mildly hypertensive if their systolic or diastolic blood pressures were ⩾140/90 mm Hg when measured by a technician and <160/95 mm Hg when measured by a physician, and subjects as white coat hypertensive if their blood pressure was <140/90 mm Hg when measured by a technician and systolic or diastolic blood pressure was ⩾160/95 mm Hg when measured by a physician. Subjects were classed as sustained hypertensive if they were taking an antihypertensive drug or had a systolic or diastolic blood pressure ⩾140/90 mm Hg when measured by a technician and ⩾160/95 mm Hg when measured by a physician.
Echocardiography
Two dimensional and two dimensionally guided M mode echocardiography (Hewlett Packard, Sonos 1500, Andover, MA) were performed on each subject by two sonographers with a 2.5 or 3.5 MHz transducer. M mode tracings were recorded at 50 mm/s. M mode echocardiograms were only suitable for analysis in 1404 (84%) participants. To reduce interobserver variability all M mode tracings were analysed by a single cardiologist. Measurements of left ventricular mass were taken just below the tips of the mitral valve. Internal end diastolic and end systolic diameters and septal and posterior wall thicknesses of the left ventricle were measured according to the guidelines of the Penn convention.19 Relative wall thickness was calculated at end diastole as the ratio of 2 × (posterior wall thickness/end diastolic diameter). Left ventricular mass was calculated according to the formula of Penn as left ventricular mass (g)=1.04 ((end diastolic diameter+septal wall thickness+posterior wall thickness)3−(end diastolic diameter)3)−13.6 g.17 Left ventricular mass was indexed to height in grams per metre.20 Left ventricular hypertrophy was defined as a left ventricular mass >138 g/m for men and >106 g/m for women. These partition values are close to the Framingham criteria and represent 2 SDs above the mean of healthy subjects in the Augsburg echocardiographic substudy of MONICA.
Left ventricular volumes were calculated from two dimensional echocardiograms obtained in short axis view at the midpapillary muscle, and long axis images obtained in the apical four chamber view. Two dimensional echocardiograms were recorded on a cine loop so that at least three measurements of the cavity and myocardium could be taken in cross section, and long axis diameters measured at end diastole and end systole. Endocardial contours of the left ventricle were obtained from parasternal short axis views at the level of the papillary muscles. Left ventricular systolic and diastolic volumes were calculated from two dimensional echocardiograms by the area length method using a formula that has been described elsewhere.21 Cardiac output was calculated from stroke volume and heart rate. Left atrial volume was obtained at end systole in the apical four chamber view.22
Doppler echocardiograms were recorded at 100 mm/s using pulsed wave Doppler with the sample volume at the tips of the mitral valve in the apical four chamber view. Early and late diastolic filling velocities, velocity time integrals, and ratios of early and late diastolic filling velocities (E/A ratio) and velocity time integrals were determined as previously reported.23 Isovolumetric relaxation time was the time interval between the end of the aortic outflow and the start of the mitral inflow signal. Doppler mitral profiles enabled diastolic filling velocities to be determined in 1297 (77%) participants and isovolumetric relaxation time in 970 (58%) participants. Variables of Doppler filling were corrected for heart rate by multiplying by the RR interval from the electrocardiogram. No systematic differences were detected with age, sex, body mass index, and systolic blood pressure between subjects with complete and incomplete diastolic filling data sets.
Statistical methods
Crude baseline data in each hypertensive group were compared with normotensive subjects, and the statistical significance of differences assessed by unpaired t tests. The mean values of echocardiographic variables in the three hypertensive groups were compared with normotensive subjects after adjustment for the covariates of age, sex, and body mass index in multiple linear regression analyses. Other factors such as physical activity, alcohol consumption, and diabetes mellitus had no major impact on left ventricular mass and were excluded from further analyses. Hypertensive groups were included as a four level class variable, and adjusted means obtained with PROC GLM (version 6.11, SAS Institute, Cary, NC). Means for variables of diastolic filling were additionally adjusted for heart rate. Differences in cardiac size were further analysed for magnitude of the white coat effect. Multiple logistic regression was applied to estimate the odds ratio of left ventricular hypertrophy in hypertensive groups compared with the normotensive group. P values <0.05 were considered statistically significant.
Results
Anthropometry
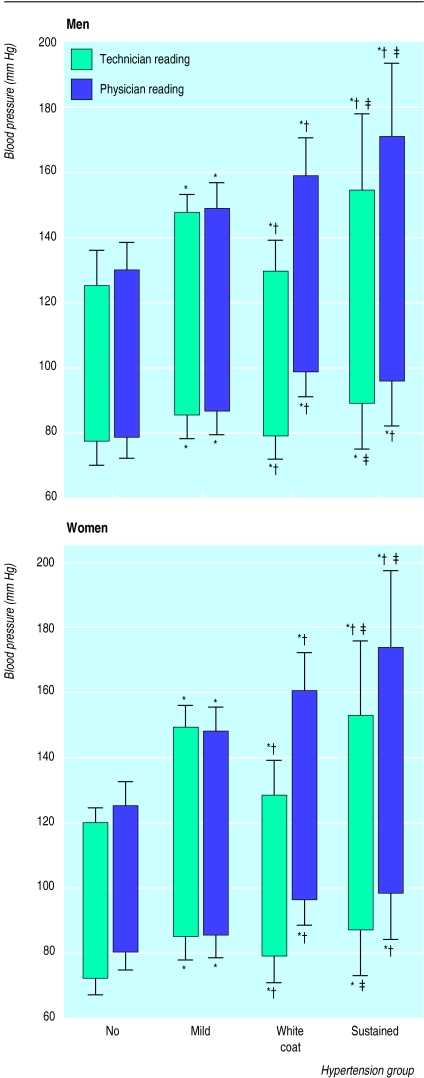
Table 1 and the figure show the anthropometric data and mean technician and physician blood pressure measurements for the blood pressure groups. Subjects were classed as white coat hypertensive if they had normotensive blood pressure measurements when taken by a technician and hypertensive measurements when taken by a physician. Although both systolic and diastolic blood pressures measured by a technician were in the normotensive range they were slightly higher in subjects with white coat hypertension compared with normotensive individuals. Mean technician and physician blood pressure readings were similar in men and women. Compared with normotensive subjects, patients with hypertension, and white coat hypertension in particular, were older and had high body mass indices. Furthermore, more men than women had white coat hypertension or mild hypertension, and more women than men had normotension. Consequently, the prevalence of white coat hypertension was higher in men than in women in this cross sectional sample (10.9% versus 8.2%; P<0.01).
Table 1.
Baseline characteristics of subjects (mean values (SD) according to blood pressure category)
| No hypertension (n=849) | Mild hypertension (n=129) | White coat hypertension (n=160) | Sustained hypertension (n=538) | |
|---|---|---|---|---|
| No of men (%) | 397 (46.8) | 83 (64.3*) | 92 (57.5*) | 272 (50.6*) |
| Age (years) | 46 (13) | 55 (13)* | 51 (13)* | 61 (10)* |
| Body mass index (kg/m2) | 25.0 (3.5) | 26.6 (3.6)* | 27.8 (3.5)* | 28.8 (4.4)* |
| Heart rate (beats/min) | 69 (11) | 73 (11)* | 70 (11) | 72 (14)* |
| White coat effect (mm Hg)†: | ||||
| Systolic | 7.5 (10.3) | −0.4 (9.5)* | 30.5 (15.3)* | 15.0 (20.4)* |
| Diastolic | 4.1 (8.4) | 1.5 (8.4) | 17.5 (9.8)* | 9.0 (11.7)* |
P<0.05 versus no hypertension (anthropomorphic characteristics compared in men and women).
Difference between systolic and diastolic blood pressure taken by physician and technician.
Cardiac structure
Because of variations in anthropometry between the blood pressure groups, structural and functional variables of the left ventricle were adjusted for age, sex, and body mass index to analyse whether differences were related to blood pressure groups independently of these potential confounders (table 2). Analyses showed that subjects with white coat hypertension or sustained hypertension had increased left ventricular mass indices. The increase in cardiac mass in subjects with white coat hypertension (7.0 g/m, 95% confidence interval 1.8 to 12.2; P=0.009) was similar for both sexes (data not shown) and due to an increase of left ventricular septal (0.4 mm, 0.2 to 0.7; P=0.004) and posterior (0.4 mm, 0.2 to 0.6; P=0.001) wall thicknesses. Diastolic diameters of the left ventricle were similar in all blood pressure groups; accordingly, relative wall thicknesses were increased in the hypertensive groups.
Table 2.
Echocardiographic characteristics of subjects. Means (SE) adjusted for confounders (sex, age, and body mass index). Heart rate added in matches of diastolic filling
| No hypertension (n=849) | Mild hypertension (n=129) | White coat hypertension (n=160) | Sustained hypertension (n=538) | |
|---|---|---|---|---|
| Thickness: | ||||
| Septal wall (mm) | 10.2 (0.06) | 10.2 (0.17) | 10.6 (0.14)* | 11.5 (0.09)* |
| Posterior wall (mm) | 8.5 (0.05) | 8.7 (0.14) | 8.9 (0.11)* | 9.4 (0.08)* |
| Left ventricular end diastolic diameter (mm) | 47.7 (0.17) | 47.5 (0.42) | 47.5 (0.34) | 48.0 (0.23) |
| Relative wall thickness (%) | 39 (3) | 40 (8)* | 41 (7)* | 44 (4)* |
| Left ventricular mass (g/m) | 96.3 (1.1) | 96.6 (2.9) | 103.2 (2.4)* | 114.6 (1.6)* |
| Left atrial volume (ml) | 42.1 (0.5) | 42.4 (1.4) | 43.5 (1.1) | 45.9 (0.7) |
| Fractional shortening (%) | 35.3 (0.2) | 37.0 (0.6)* | 36.5 (0.5)* | 35.5 (0.3) |
| Cardiac output (l/min) | 4.5 (0.1) | 4.7 (0.2) | 4.5 (0.2) | 4.8 (0.1) |
| E/A ratio‡ | 1.28 (0.01) | 1.26 (0.04) | 1.28 (0.03) | 1.22 (0.02)* |
| Int E/A ratio§ | 2.03 (0.07) | 1.95 (0.08) | 1.94 (0.06) | 1.88 (0.04)* |
| Isovolumetric relaxation time (ms) | 76.3 (0.7) | 78.7 (1.9) | 78.0 (1.6) | 84.1 (1.1)* |
P<0.05 versus no hypertension.
Ratio of early to late diastolic filling velocity.
Ratio of integrals of early and late diastolic velocity.
To determine differences between normotensive and white coat hypertensive subjects left ventricular mass index was further adjusted for differences in systolic blood pressure as measured by a technician (table 3). Analysis showed that the increase in wall thicknesses and left ventricular mass was not affected by differences in baseline blood pressure but related to the white coat effect. Likewise, a regression model performed on the whole population showed that both systolic and diastolic white coat effects were significantly associated with adjusted left ventricular mass index (P<0.05). In particular, a systolic white coat effect of 10 mm Hg was associated with an increase in the adjusted prevalence of left ventricular hypertrophy (odds ratio 1.2, 1.1 to 1.3; P=0.015) and with an increase of the adjusted left ventricular mass of 1.6 g/m (P=0.016). Finally, the prevalence of left ventricular hypertrophy was more than doubled in subjects with white coat hypertension compared with normotension (table 4).
Table 3.
Echocardiographic variables (means (SEM)) after adjustment for age, sex, body mass index, and systolic blood pressure taken by technician
| No hypertension (n=849) | Mild hypertension (n=129) | White coat hypertension (n=160) | Sustained hypertension (n=538) | |
|---|---|---|---|---|
| Wall thickness (mm) | ||||
| Septum | 10.4 (0.07) | 10.0 (0.2)* | 10.7 (0.1)* | 11.1 (0.1)* |
| Posterior | 8.6 (0.06) | 8.5 (0.2) | 9.0 (0.1)* | 9.2 (0.1)* |
| Left ventricular mass (g/m) | 99.2 (1.3) | 93.5 (3.0) | 104.7 (2.4)* | 110.5 (1.9)* |
| Fractional shortening (%) | 35.4 (0.2) | 36.8 (0.6)* | 36.6 (0.5)* | 35.2 (0.4) |
P<0.05 versus no hypertension.
Table 4.
Prevalence and odds ratio of left ventricular hypertrophy according to blood pressure group, after adjustment for sex, age, and body mass index by logistic regression (normotensive subjects used as reference group)
| No hypertension (n=849) | Mild hypertension (n=129) | White coat hypertension (n=160) | Sustained hypertension (n=538) | |
|---|---|---|---|---|
| No (%) with left ventricular hypertrophy | 78 (10.3) | 17 (18.1) | 39 (27.7) | 217 (53.1) |
| Odds ratio | 1.0 | 1.4 | 1.9 | 3.7 |
| 95% CI | — | 0.7 to 2.6 | 1.2 to 3.2 | 2.5 to 5.3 |
| P value | — | 0.30 | 0.009 | 0.001 |
Unadjusted left atrial volume differed greatly across the blood pressure groups (data not shown). However, adjustment, as carried out for left ventricular mass index, resulted in loss of significant associations between white coat hypertension and atrial volume (table 2). Similarly, both the systolic and diastolic white coat effects were not associated with an increase in left atrial volumes (data not shown).
Systolic function
—Systolic function of the left ventricle, assessed by M mode fractional shortening, was within normal limits for both sexes in each blood pressure group. Fractional shortening was, however, enhanced in subjects with white coat hypertension (1.3%, 0.2 to 2.4; P=0.017) (table 2). In the white coat hypertensive group significantly increased fractional shortening persisted after adjustment for age, sex, and body mass index, and systolic blood pressure measured by a technician (table 3). However, a systolic or diastolic white coat effect of 10 mm Hg was not associated with a significant increase in fractional shortening (data not shown).
Diastolic filling—
Compared to normotensive or mildly hypertensive subjects, variables of diastolic filling were similar in subjects with white coat hypertension when adjusted for sex, age, and body mass index (table 2). In contrast, subjects with sustained hypertension had a prolonged isovolumetric relaxation time and a decreased E/A ratio due to an increase in atrial filling velocity (table 2). An increase of 10 mm Hg for systolic or diastolic white coat effects had no impact on variables of diastolic filling (data not shown).
Discussion
An exaggerated rise in a patient’s blood pressure seems to be a common phenomenon after an echocardiographic examination by a physician. This response to mild stress was found to be related to structural alterations of the heart including a significant increase in left ventricular mass and an increased prevalence of left ventricular hypertrophy. Moreover, the extent of blood pressure rise seems to be independently associated with left ventricular mass and left ventricular hypertrophy.
As previous studies have shown that left ventricular hypertrophy may lead to increased morbidity and mortality in both patients with uncomplicated essential hypertension and the general population,20 the present data may indicate that white coat hypertension confers an increased cardiovascular risk. The increased risk of left ventricular hypertrophy may add to the poor haemodynamic and metabolic profiles reported in subjects with white coat hypertension.11 White coat hypertension has also been shown to advance frequently into sustained hypertension.7 Taken together, these data raise doubts about white coat hypertension as a benign condition.6 Rather, white coat hypertension may identify those individuals at increased risk of cardiovascular disease who may benefit from primary preventive strategies such as non-pharmacological intervention to lower blood pressure.
White coat hypertension and left ventricular mass
Our study does not explain the underlying mechanism between white coat hypertension and left ventricular hypertrophy, but the literature does provide substantial evidence for left ventricular hypertrophy not being confined to subjects with sustained hypertension.24,25 In fact, transient increases in blood pressure, such as during physical exercise, may have an independent effect on left ventricular mass.26 One study in dogs showed that concentric left ventricular hypertrophy could be produced by intermittently compressing the dogs’ hindlimbs to increase blood pressure.27 Likewise, in our study relative wall thickness was increased in subjects with white coat hypertension suggesting the predominance of a concentric pattern of hypertrophy. Furthermore, experimental studies have shown that short episodes of cardiac pressure overload are sufficient to induce growth related genes and protein synthesis in the heart.28 Thus it may be speculated that intermittent blood pressure spikes caused by exaggerated responses to mild stress may augment mechanisms of cardiac growth and thus the risk of hypertrophy.
White coat effect and left ventricular mass
To further analyse this hypothesis, we correlated the white coat effect—that is, the absolute difference in systolic or diastolic blood pressure as measured by a technician and physician—with variables of cardiac mass and function. The association between white coat effect and left ventricular mass persisted after adjustment for age, sex, body mass index, and blood pressure levels as measured by a technician. Thus the rise in blood pressure in a situation of mild stress may be as informative as the diagnosis of white coat hypertension. This finding is highly relevant as the term white coat hypertension lacks defined diagnostic criteria.2 Most clinical investigators have contrasted ambulatory blood pressure measurements taken automatically with those taken by the physician,2 whereas population based surveys have contrasted blood pressure measurements taken by a nurse,29 or self measurements,7 with measurements taken by a physician. Neither ambulatory blood pressure measurements nor those taken in the doctor’s practice have been performed uniformly,2 and definitions of the upper normal limits of daytime blood pressure or physician blood pressure in white coat hypertensive subjects greatly vary between studies.2 As a result some investigators have proposed that the association between left ventricular mass and white coat hypertension is largely affected by cut off points of baseline blood pressure.2 Our study of a large sample size does not concur with this as it shows that a rise in blood pressure by itself is related to left ventricular hypertrophy. We used a standardised triple sphygmomanometric measurement to assess baseline systolic and diastolic blood pressure values after an extensive resting period. These values were compared with a single sphygmomanometric measurement taken by a physician within 60 minutes of the baseline measurement. We believe this method validly reflects the individual’s blood pressure response to mild stress and avoids misinterpretations caused by diurnal blood pressure variation and different measurement techniques.
Potential limitations
Our study may be challenged as baseline systolic and diastolic blood pressure measurements were already higher in the white coat hypertensive patients compared with normotensive subjects. Previous investigators have made similar observations.4,8–10,30 As even a slightly higher blood pressure than normal may result in a chronic increase in haemodynamic load of the heart26 it may be hypothesised that the increase in left ventricular mass in the white coat hypertensive group is exclusively related to differences in baseline blood pressure rather than related to the white coat effect. However, in contrast to previous studies we corrected for the baseline (technician) blood pressure by multivariate analysis. We also observed that the white coat effect was related to left ventricular mass and hypertrophy independent of differences in baseline blood pressure. We therefore believe that stress related increases in blood pressure can be regarded as an independent determinant of left ventricular mass.
White coat hypertension and left ventricular function
Our study agrees with previous investigations of reported normal left ventricular systolic function in subjects with white coat hypertension.26 In fact we observed left ventricular function slightly above normal in the white coat hypertensive group. It may be hypothesised that in addition to reduced peripheral arterial compliance,13 enhanced left ventricular contractility may contribute to the increase in blood pressure observed in white coat hypertensive patients. The findings are consistent with enhanced activity or sensitivity, or both, of the sympathetic nervous system resulting in increases in blood pressure and augmented left ventricular contractility during mild stress. We were, however, unable to detect any independent association between white coat hypertension and variables of diastolic filling or left atrial size.
Conclusion
Our study shows that white coat hypertension is common in the general population and that it may be associated with an increased risk of left ventricular hypertrophy and concentric remodelling of the heart. It would seem premature to dismiss white coat hypertension as a benign variant of blood pressure regulation, rather it may indicate the need for intensified monitoring and control of cardiovascular risk factors.
Figure.
Mean blood pressure values (SD) measured by a technician and a physician for men and women in different blood pressure groups. *P<0.05 versus no hypertension; †P<0.05 versus mild hypertension; ‡P<0.05 versus white coat hypertension
Footnotes
Funding: The investigation was supported by grants from the Deutsche Forschungsgemeinschaft (672/3-1, 672/9-1, and 672/10-1) and the Bundesministerium für Forschung und Technologie (HS and HWH). This paper was presented in part at the 46th scientific sessions of the American College of Cardiology.
Conflict of interest: None.
References
- 1.Mancia G, Pevali G, Pomidossi G, Grassi G, Casadei R, Zanchetti A. Alerting reaction and rise in blood pressure during measurement by physician and nurse. Hypertension. 1987;9:209–215. doi: 10.1161/01.hyp.9.2.209. [DOI] [PubMed] [Google Scholar]
- 2.Mancia G, Zanchetti A. White coat hypertension: misnomers, misconceptions, and misunderstandings. What should we do next? J Hypertens. 1996;14:1049–1052. doi: 10.1097/00004872-199609000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Hoegholm A, Kristensen K, Bang L, Nielsen J, Nielsen W, Madsen H. Left ventricular mass and geometry in patients with established hypertension and white coat hypertension. Am J Hypertens. 1993;6:282–286. doi: 10.1093/ajh/6.4.282. [DOI] [PubMed] [Google Scholar]
- 4.Cavallini MC, Roman M, Pickering T, Schwartz J, Pini R, Devereux RB. Is white coat hypertension associated with arterial disease or left ventricular hypertrophy? Hypertension. 1995;26:413–419. doi: 10.1161/01.hyp.26.3.413. [DOI] [PubMed] [Google Scholar]
- 5.Perloff D, Sokolow M, Cowan R. The prognostic value of ambulatory blood pressure. JAMA. 1983;229:2892–2898. [PubMed] [Google Scholar]
- 6.Gosse P, Promax H, Durandet P, Clementy J. White coat hypertension. No harm to the heart. Hypertension. 1993;22:766–770. doi: 10.1161/01.hyp.22.5.766. [DOI] [PubMed] [Google Scholar]
- 7.Bidlingmeyer I, Burnier M, Bindlingmeyer M, Waeber B, Brunner H. Isolated office hypertension: a prehypertensive state? J Hypertens 1996:327-32. [DOI] [PubMed]
- 8.Kuwajima I, Suzuki Y, Fujisawa A, Kuramoto K. Is white coat hypertension innocent? Structure and function of the heart in the elderly. Hypertension. 1993;22:826–831. doi: 10.1161/01.hyp.22.6.826. [DOI] [PubMed] [Google Scholar]
- 9.Cardillo C, De Felice F, Campia U, Folli G. Psychophysiological reactivity and cardiac end organ changes in white coat hypertension. Hypertension. 1993;21:836–844. doi: 10.1161/01.hyp.21.6.836. [DOI] [PubMed] [Google Scholar]
- 10.Soma J, Wideroe TE, Dahl K, Rossvoll O, Skjaerpe T. Left ventricular systolic and diastolic function assessed with two-dimensional and Doppler echocardiography in “white coat” hypertension. J Am Coll Cardiol. 1996;28:190–196. doi: 10.1016/0735-1097(96)00129-5. [DOI] [PubMed] [Google Scholar]
- 11.Julius S, Mejia A, Jones K, Krause L, Schork N, van de Ven C, et al. “White coat” versus “sustained” borderline hypertension in Techumseh, Michigan. Hypertension. 1990;16:617–623. doi: 10.1161/01.hyp.16.6.617. [DOI] [PubMed] [Google Scholar]
- 12.Siegel WC, Blumenthal JA, Divine GW. Physiological, psychological, and behavioral factors and white coat hypertension. Hypertension. 1990;16:140–146. doi: 10.1161/01.hyp.16.2.140. [DOI] [PubMed] [Google Scholar]
- 13.Glen SK, Elliott H, Gurzio J, Lees K, Reid J. White coat hypertension as a cause of cardiovascular dysfunction. Lancet. 1996;348:654–658. doi: 10.1016/S0140-6736(96)02303-3. [DOI] [PubMed] [Google Scholar]
- 14.Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med. 1990;323:1706–1707. doi: 10.1056/NEJM199005313222203. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organisation monitoring of trends and determinants in cardiovascular disease project: WHO MONICA project: objectives and design. Int J Epidem. 1989;18(suppl 1):29–37S. [Google Scholar]
- 16.Hense HW, Koivisto AM, Kuulasmaa K, Zarborskis A, Kupusc W, Tuomilehto J. Assessment of blood pressure measurement quality in the baseline surveys of the WHO MONICA Project. J Human Hypertens. 1995;9:935–946. [PubMed] [Google Scholar]
- 17.Keil U, Stieber J, Döring A, Chambless L, Härtel U, Filipiak B, et al. The cardiovascular risk factor profile in the study area of Augsburg. Results from the first MONICA survey 1984/85. Acta Med Scand 1988;(suppl 728):119-28. [DOI] [PubMed]
- 18.Report of the World Health Organisation Scientific Group. Geneva: WHO technical report; 1983. Primary prevention of essential hypertension; p. 686. [PubMed] [Google Scholar]
- 19.Devereux RB, Reichek N. Echocardiographic determination of left ventricular mass in man: anatomic validation of the method. Circulation. 1977;55:613–618. doi: 10.1161/01.cir.55.4.613. [DOI] [PubMed] [Google Scholar]
- 20.Levy D, Savage DD, Garrison RJ, Anderson KM, Kannel WB, Castelli WP. Echocardiographic criteria for left ventricular hypertrophy. The Framingham Heart Study. Am J Cardiol. 1987;59:956–960. doi: 10.1016/0002-9149(87)91133-7. [DOI] [PubMed] [Google Scholar]
- 21.Wallerson DC, Ganau A, Roman MJ, Devereux RB. Measurement of cardiac output by M-mode and two-dimensional echocardiography: application to patients with hypertension. Eur Heart J. 1990;11(suppl 1):67–78. doi: 10.1093/eurheartj/11.suppl_i.67. [DOI] [PubMed] [Google Scholar]
- 22.Hirashi S, DiSessa TG, Jarmakani JM, Nakanishi T, Isabel-Jones J, Friedman WF. Two-dimensional echocardiographic assessment of left atrial size in children. Am J Cardiol. 1983;52:1249–1257. doi: 10.1016/0002-9149(83)90582-9. [DOI] [PubMed] [Google Scholar]
- 23.Muscholl M, Dennig K, Kraus F, Rudolph W. Echocardiographic and Doppler-echocardiographic characterization of left ventricular diastolic function. Herz. 1990;15:377–392. [PubMed] [Google Scholar]
- 24.Levy D, Anderson KM, Savage DD, Kannel WB, Christiansen JC, Castelli WP. Echocardiographically detected left ventricular hypertrophy: prevalence and risk factors. The Framingham Heart Study. Ann Int Med. 1988;108:7–13. doi: 10.7326/0003-4819-108-1-7. [DOI] [PubMed] [Google Scholar]
- 25.Schunkert H, Hense HW, Holmer SR, Stender K, Perz S, Keil U, et al. Association between a deletion polymorphism of the angiotensin-converting-enzyme gene and left ventricular hypertrophy. N Engl J Med. 1994;330:1634–1638. doi: 10.1056/NEJM199406093302302. [DOI] [PubMed] [Google Scholar]
- 26.Hammond IW, Devereux RB, Alderman MH, Laragh JH. Relation of blood pressure and body build to left ventricular mass in normotensive and hypertensive employed adults. J Am Coll Cardiol. 1988;12:996–1004. doi: 10.1016/0735-1097(88)90467-6. [DOI] [PubMed] [Google Scholar]
- 27.Kingwell BA, Krause L, Julius S. The effect of hypertensive episodes and cardiac hypertrophy on the canine cardiac baroreflex. Clin Exp Phamacol Physiol. 1994;21:31–39. doi: 10.1111/j.1440-1681.1994.tb02433.x. [DOI] [PubMed] [Google Scholar]
- 28.Schunkert H, Sandoshima JI, Kagaya Y, Weinberg EO, Izumo S, Riegger G. Angiotensin II induced growth responses in isolated adult rat hearts. Evidence for load independent induction of cardiac protein synthesis by angiotensin II. Circ Res. 1995;76:489–497. doi: 10.1161/01.res.76.3.489. [DOI] [PubMed] [Google Scholar]
- 29.Cuspidi C, Marabini M, Lonati L, Sampieri L, Comerio G, Pelizzoli S, et al. Cardiac and carotid structure in patients with established hypertension and white coat hypertension. J Hypertens. 1995;13:1707–1711. [PubMed] [Google Scholar]
- 30.Hoegholm A, Bang L, Kristensen KS, Nielson JW, Holm J. Microalbuminuria in 411 untreated individuals with established hypertension, white coat hypertension, and normotension. Hypertension. 1994;24:101–105. doi: 10.1161/01.hyp.24.1.101. [DOI] [PubMed] [Google Scholar]