Abstract
Objective
To describe the development, implementation, and assessment of a geriatric pharmacotherapy elective course emphasizing a patient-centered approach and active, self-directed learning strategies.
Design
The course content included fundamental concepts in aging, geriatric syndromes, activities involving assessment of medically complex older adults, presentation of controversies in clinical geriatrics, book and film clubs, an Adopt-a-Patient project, and scientific and reflective writing. Students participated in site visits to interview and interact with older adults.
Assessment
Student evaluation of the course was assessed with the teaching evaluation tool, an end-of-semester survey, a follow-up P4 survey, and reflective writings. Students strongly agreed that course goals were achieved. Learning how to communicate with older adults and assess complex medication regimens were the areas of highest importance to students. P4 students strongly agreed that skills learned in the course were important to their success in advanced pharmacy practice experiences (APPEs).
Conclusion
A pharmacotherapy course emphasizing active and self-directed learning in geriatrics through innovative teaching was adaptable to doctor of pharmacy (PharmD) students at various stages of their training and improved students' perceptions of aging.
Keywords: pharmacotherapy, geriatrics, active learning
INTRODUCTION
The drug therapy needs of older adults present unique challenges. Although some older adults are healthy and live independently into their 90s and beyond, others have a significant burden of comorbid conditions and require treatment with complex drug regimens. All pharmacists, regardless of their practice site, must have a thorough knowledge of the diverse biological, medical, and psychosocial factors essential in providing quality care to older adults. As the proportion of US adults over 60 years of age continues to increase, pharmacists will have a critical and expanding role in the clinical care of these older adults. The Institute of Medicine (IOM) emphasized this in a report stating that the number of older adults will double between 2005 and 2030, and the United States is not prepared to meet the healthcare needs of this population .1
Traditionally, pharmacy students have learned about diseases and drug therapy used to treat older adults as part of a standard pharmacy curriculum. This approach often limits discussion to examples of patients with a single disease and limited drug therapy. Previously at this institution, an elective course had focused on the pharmacotherapy needs of both pediatric and geriatric patients. When the pediatrics component became a separate elective course, a separate Pharmacotherapy in Geriatrics elective also was formed in September 2007.
Publications on geriatric pharmacy education have stressed the importance of including geriatric therapy competency nationally within college of pharmacy curricular content.3 The Accreditation Council for Pharmacy Education (ACPE) competencies also stress the importance of developing appropriate communication skills, which are difficult to teach in the classroom. Thus, a mix of teaching and learning methods that reflected the ACPE standards on the importance of lifelong learning and emphasize patient safety, cultural competence, health literacy, health care disparities, and interdisciplinary teamwork was included in the course.2 This innovative course combined both geriatrics and gerontology to provide students with a broad approach to the biological, medical, psychological, and sociological issues associated with aging.
DESIGN
Course Philosophy and Objectives
A primary goal of the course was to encourage active, self-directed learning by students, as well as to enhance their communication skills with older adults. Students were encouraged to use a patient-centered approach to care in healthy as well as frail older adults. Diverse teaching techniques and active-learning strategies were employed to strengthen students' understanding of age-related physiologic changes influencing pharmacokinetics and pharmacodynamics, as well as assessment techniques for evaluating functional status and complex drug regimens. The importance of interdisciplinary teams in the provision of care, issues in evaluating evidence from clinical trials, and recognition of the limitations of evidence-based practice in geriatrics were also discussed and applied through various course activities. In this course, students took their learning outside of the classroom and interacted directly with older adults to apply these principles. Students were provided with many opportunities to practice and refine their communication skills with older adults prior to their APPEs. Assignments such as interviewing patients, discussing medication regimens, and participating in activities at older adult care sites offered opportunities to enhance intergenerational communication.
The course incorporated problem-based learning approaches. Students were expected to dedicate time outside of class to prepare patient cases, develop care plans, and complete the assigned readings. Course faculty members guided students in their individual learning, but expected students to be self-motivated in their learning regarding diseases and drug therapy that may not have been covered in the PharmD curriculum prior to enrolling in the geriatrics elective. The course size was deliberately kept small, ranging from 8 to 30 students to ensure interactive projects and activities were successfully implemented.
Early in the semester, the focus was on the fundamental principles in geriatrics. Evaluating and discussing patient cases, writing assignments and presentations, group activities, site visits, and development of a patient project were integrated throughout the semester to further the learning objectives of the course. The learning objectives for the course were:
Identify physiological changes in older adults that influence the pharmacokinetic and pharmacodynamic parameters of medications;
Demonstrate the use of common geriatric assessment tools;
Analyze the respective roles of different health professionals on interdisciplinary teams caring for older adults;
Discuss models of care for older adults including adult day care, assisted living, and skilled nursing home;
Identify issues in communicating effectively with older adults and caregivers especially with respect to medication adherence;
Describe cultural competency and health literacy including their potential influence on working effectively with older adults and caregivers;
Evaluate the impact of common geriatric syndromes, their presentation, and management in older adults;
Develop optimal drug therapy regimens in older adults with complex medical histories and justify therapies using an evidence-based approach; and
Identify and establish treatment priorities in older adults with complex medical histories.
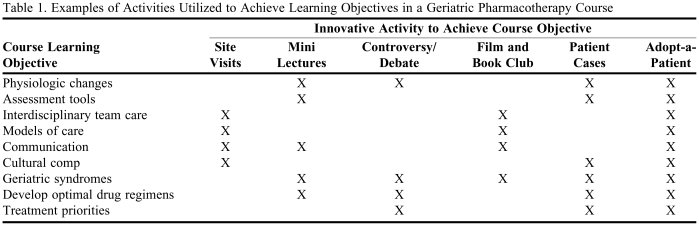
Each of the major course activities fostered learning in multiple course objectives (Table 1). The innovative activities were intentionally designed so that multiple interactive teaching techniques could be employed and the use of traditional lecturing minimized.
Table 1.
Examples of Activities Utilized to Achieve Learning Objectives in a Geriatric Pharmacotherapy Course
One of the major resources of the course was an older adult living community, South Bay Manor, in close proximity to the University that housed 100 skilled, assisted, and independent living residents. Over the 3 semesters that the course was offered, these residents participated in many aspects of the course, including site visits, the Adopt-a-Patient project, assessment tools, and film club.
Course Components
Geriatric assessment.
Students were introduced to assessments tools commonly used in geriatric practice early in the course so that they would be comfortable utilizing them for later activities. These tools included the Folstein Mini Mental State Examination (MMSE), the Tinetti Balance Assessment Tool, and the Braden Scale.4-6 Several approaches were used to assess complex drug regimens such as the Medication Appropriateness Index and discussion of Beer's criteria drugs.7-8 In addition, case sessions on decision making regarding medication appropriateness for medically complex older adults used key primary literature so that students would become more familiar with evidence-based practice. These articles were challenging for the students to fully appreciate. Initially they felt that in individuals with a condition such as hyperlipidemia, for which drug therapy was available, everyone should be treated without regard to factors such as life expectancy, time to expected benefit, or comorbid conditions such as advanced Alzheimer's disease. Exercises involving decision-making when only limited evidence from clinical practice guidelines and research studies was available also were incorporated into the course. The goal of these activities was to encourage direct exposure to diverse assessment methods and issues that would be needed for the case studies and other projects.
Individuals from South Bay Manor have been involved with this course since the first offering and enjoy the opportunity to interact with students. They volunteer to attend class on campus so that the students can learn and practice geriatric assessment on older adults rather than using a mock activity on other students. The MMSE, fall risk assessment, and the Medi-Cog were discussed in terms of strengths and limitations in practice.4,5,9 The Medi-Cog was used by students during the Adopt-a-Patient project as a cognitive screening tool to identify patients at risk for mismanaging their pillboxes.9 The use of this tool generated valuable discussions about the appropriateness of some individuals to reside in independent and assisted living facilities.
Mini-lectures.
Beginning midway through the semester, 6 mini-lectures (20 to 25 minutes in length) that focused on key geriatric syndromes including urinary incontinence, pressure ulcers, delirium, behavioral and psychiatric symptoms in dementia, pain management, and frailty in older adults were presented by course faculty members. Required readings were assigned and students were expected to participate in the class discussion, with an emphasis on applying the material to the care of individual patients.
Patient case discussions.
In all semesters, 5 to 10 medically complex older adult case studies were discussed in the course. The goal of this activity was to encourage problem-based and active learning, especially in identifying and prioritizing problems in the setting of multiple diseases and drugs. Because students had varying levels of knowledge about the diseases, students worked in pairs with each group presenting their care plans for class discussion. Course faculty members facilitated a discussion on how to problem-solve the patient's different issues, establish priorities in the care plan, and make decisions to ensure optimal care. A rubric was developed for standardized grading.
Current controversies in geriatrics.
The goal of this activity was to encourage students to recognize many of the controversies that exist in treating older adults and the questionable evidence supporting some common beliefs in geriatric practice. Each semester, questions related to current controversies in geriatrics were identified. In the first 2 course offerings, groups of 3 students were formed and assigned a controversy to evaluate and present the evidence in the form of a debate in class. In a later semester, with a smaller class, each student chose a controversy and presented a 10-minute discussion of the major issues. Student discussants were assigned to each debate/presentation to facilitate class participation. Example topics included: Should mirtazapine be used for unintentional weight loss in the elderly? Should acetylcholinesterase inhibitors be discontinued in late stage dementia?
Teaching Activities to Promote Empathy
Film and book club.
In the second and third course offerings, film and book club discussions were added to the course. The goal of these activities was to encourage students to become more empathetic to older adults and caregivers, as well as discuss the scientific evidence appropriate to both a health professional and lay person. The film Iris (2001) was viewed in class and students submitted a reflective paper focusing on one or more issues portrayed in the film.
In fall 2008, students read the book, Aging With Grace…What the Nun Study Teaches Us About Leading Longer, Healthier, and More Meaningful Lives.10 Each student chose a principle or theory about aging that was discussed in the book and related to Alzheimer's disease and wrote a paper evaluating that theory based on the scientific evidence available in the literature. Examples of topics included the effects of education, idea density, nutrition, leisure activities, cardiovascular risk, and apolipoprotein E on the risk of Alzheimer's disease. Students then presented their papers to the class, and merged some of the scientific evidence with a more casual “book club” discussion format prompted by questions posed by students and course faculty members.
Also during fall 2008, students visited South Bay Manor as a class to watch the recently released documentary Young at Heart (2008) with the residents, followed by a group discussion. Students were required to write a reflective essay about the experience of viewing the film with the older adults.
Teaching with Direct Patient Contact
Teaching activities at care sites.
Visits to a care site were incorporated into the course to give students direct exposure to different opportunities and issues in geriatric pharmacy practice. The primary challenge was scheduling the student activities. Examples included shadowing a pharmacist to observe nursing home consulting activities, participating in a patient care conference, learning Tai chi with a group of older adults, assisting with the fall risk assessment of a patient, attending presentations given by older adults about their travels or investment strategies, providing Medicare Part D counseling at senior centers, teaching computer skills to older adults, and visiting a long-term care pharmacy. Students also used the Nintendo Wii gaming system with groups of older adults as a way to encourage communication. This system offers various games providing mental, physical, and social benefits that both students and older adults can appreciate. After participating in each activity, students wrote a 1-page reflection and discussed their experience with the class.
Adopt-a-Patient project.
In the second and third course offerings, an Adopt-a-Patient project was initiated with an assisted care facility. The goal of this activity was to increase students' one-on-one interactions with older adults in independent and assisted living settings. The primary challenge presented by this activity was student inexperience with interviewing older adults resulting in their initial apprehension and lack of confidence. This was addressed by discussing communication styles and interview techniques in class. In addition, 3 P4 students completing an APPE in geriatrics developed a video with an actual patient demonstrating how to conduct a patient interview. These APPE students also accompanied each student group during their initial patient interview. These 3 students had taken the elective during the previous year, so they were familiar with the expectations of the project and able to assist the junior students in conducting the interview.
Students worked in pairs and were assigned an older adult to interview during the third week of the semester. Students were encouraged to meet with the older adult several times during the semester. Students initially presented their patient case to the class for discussion mid-semester and then more formally at the end of the semester.
The students' recommendations for the patient and nursing staff were first discussed with the course instructors. Once approved, the recommendations were discussed with the patient and a written copy was provided to both the patient and the director of nurses. The patient recommendations were written in larger font for easier reading and provided at an appropriate health literacy level. A sample of selected Adopt-a-Patient materials is included in Appendix 1.
EVALUATION AND ASSESSMENT
Assessment of Student Performance
Student achievement of course goals and objectives was evaluated through multiple methods. The course grade was based on the following: 2 examinations (30 points total), formal pharmacotherapy plans (20 points), debate/older adult controversy (10 points), book club scientific paper (10 points), the film club and other reflective papers (10 points total), and the Adopt-a-Patient project (20 points).
Course Assessment
All students completed a standardized evaluation, the Student Evaluation of Teaching (SET), which consisted of questions with Likert-style responses based on a scale of 1-5 on which 1 = strongly disagree and 5 = strongly agree. The scores were summarized into 4 components including analytic/synthesis of approach, organizational clarity, instructor group interaction, and instructor student interaction. The results received for this course were higher than those collected over all semesters when compared with the university's statistics for similar courses. Students' ratings of the course ranged from 4.5 - 4.9 out of a maximum of 5 in the 4 component areas (analytic/synthesis of approach, organizational clarity, instructor group interaction, and instructor student interaction) assessed during the first 3 semesters the course was offered.
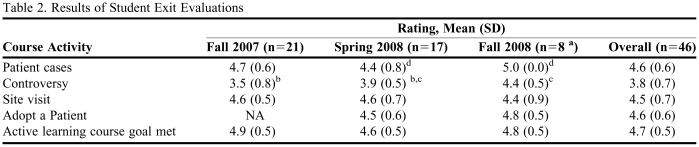
Students also completed an exit evaluation that included both quantitative and qualitative assessments. Results are presented in Table 2. Students provided positive feedback about evaluating the complex medication regimens in the patient case studies, but suggested that the number of cases should be decreased and spread out over the semester. To assess for the effects of course change over time, differences in component scores were evaluated using a student's t test. This data showed that all students in all semesters highly valued the patient cases, Adopt-a-Patient activity, and site visits, and felt the active-learning course goal was met. Student satisfaction with the controversy activity improved over the 3 semesters that the course was offered as modifications were made to the design.
Table 2.
Results of Student Exit Evaluations
a Smaller “n” because the course was offered to the same graduating class in fall 2007 (as P2s) and again in fall 2008 (as P3s).
b Difference between fall 2007 and spring 2008, p = 0.03
c Difference between spring 2008 and fall 2008, p = 0.04
d Difference between spring 2008 and fall 2008, p = 0.004
On the qualitative section of the evaluation, students indicated that improving patient communication and increasing knowledge/comfort in evaluating patient cases using a SOAP format (subjective/objective/assessment/plan) were the 2 most highly valued skills learned in the course. The P2 students in the first offering of the course consistently commented that the class was beneficial because of the discussion component, which had not been present in their first-year coursework.
Follow-up Assessment Survey
In April 2009, a survey containing 12 questions was e-mailed to the 21 P4 students who took the course as P3 students during spring 2008. The survey assessed their perceptions of the value of different components of the geriatrics elective course on their performance during their APPEs. Fifteen surveys were returned, with the graduating P4 students indicating that the course provided them with knowledge and skills applicable to their subsequent APPEs.
Qualitative Assessment
Reflective writing exercises have been used in the course and represent a unique opportunity to write in a method other than the scientific style. Students had the opportunity to write about site visits, the Adopt-a-Patient project, and specific activities occurring both in and out of the classroom by reflecting on the experience and how it affected them directly.
DISCUSSION
By 2030, an estimated 71 million adults, or approximately 1 in every 5 Americans, will be 65 years of age or older; thus, health professionals must be proficient in caring for older adults, and pharmacists are ideal to participate in this role.1 The communication skills of pharmacists must be strengthened to enable them to work effectively with older adults. Creating learning experiences for pharmacy students at independent and assisted living facilities provides opportunities for students to have direct contact with older adults. Although colleges of pharmacy have been involved in senior centers and other outreach programs for many years, additional opportunities exist among the newer models of care. This can broaden the exposure of students to older adults, with patients ranging from those living independently to those needing sub-acute levels of care.
This course is transferable to other PharmD programs, regardless of the structure of the individual curriculum. Three classes of PharmD students have successfully completed the course even when significant gaps in core knowledge of major diseases and drugs existed. Although the students appreciated the small class size, the course can be modified to work in a larger class setting due to the use of multiple interactive teaching activities.
This course is also transferable because it uses available teaching resources in a creative manner. The course was developed by 3 faculty members with diverse experiences in geriatrics, thereby providing different perspectives. To provide consistency to the students, 1 instructor coordinated the activities and served as the primary student contact, but all 3 contributed to the course content and delivery. This team teaching approach offered a sharing of expertise and was valued by the students based on their feedback.
Of the many active-learning strategies used in the class, the Adopt-a-Patient activity was the most innovative. Although all students had direct patient contact from introductory practice experiences, it was sometimes quite limited. This project was the students' first opportunity to meet with patients as a student in the health professions and to use skills that they had acquired. Students gained confidence by talking with the individual, administering assessments such as screening for their risk of falling, using the Medi-Cog tool,9 measuring blood pressure, and providing recommendations about the appropriate use of their medications. Some patients' medical problems were so complex that students were concerned about the ability of the individual to safely self-medicate. This led to discussions about the appropriateness of particular living situations and the implications to older adults, caregivers, and health professionals. For example, one elderly patient was confused about how to administer and store her medications. Another patient had vision changes that made it impossible to self-administer her own medications. These concerns were shared with the nursing staff and the ramifications were discussed. Students began to think more about the consequences to the individuals if a change in independence were to happen because now there was a real person involved.
The feedback provided on the student exit evaluations is valuable when modifying the course for future semesters. Feedback included spacing out the cases differently and providing more opportunities for site visits. P2 students appeared to benefit most from the active-learning style of the course, while P3 students found the course to be especially helpful in preparing them for APPEs in their P4 year.
Based on the data compiled from the student exit evaluations, modifications that were made within the case discussions (from spring 2008 to fall 2008) and within the older adult controversy format (spring 2008 vs. fall 2008) were successful. In addition, the knowledge deficits regarding specific content areas for the younger P2 students were recognized as contributing to dissatisfaction with some of the activities for fall 2007. All of these changes were made based on information provided by student exit evaluations.
When the Adopt-a-Patient project was first implemented, it was conducted from mid-semester through the end of the course. This was a short period of time to gather necessary patient information when combined with the other course requirements. Changing the timeframe to encompass the entire semester allowed the students more time to visit and check on the status of their patient and address some of the changes that occurred in the patient's health and living situation from the first visit through the last. As a result, students were more knowledgeable about their patient and able to join in class discussion about patient issues, and felt more like a valued member of a health care team.
Based on student performance, one issue noticed by faculty members and students was that students improved their ability to establish priorities in their care plans for medically complex older adults. This especially was enforced by the case discussions that were assigned as part of the course, but also the cases that were integrated within the lectures and presented by the P4 students as part of their APPEs.
Overall, the most notable success story was changing student attitudes towards older adults. This was most evident from the student reflections that were submitted after the site visits and Adopt-a-Patient project, but also on the index card reflections submitted each week in class. Students began to appreciate the diversity of older adults and felt better prepared to interact with them both professionally and personally. Throughout the semester, this continued to improve.
A future goal for this course is to track students' performance in other didactic core courses and APPEs to determine whether student self-directed learning of new core topics will improve performance in subsequent courses. Also, the impact of the Adopt-a-Patient project on their overall confidence and ability to communicate with older adults needs to be further explored.
Integrating an interdisciplinary design by offering the course in a modified form to other health disciplines is another consideration for the future. Nursing, nutrition, physical therapy, and pharmacy students working together in the Adopt-a-Patient project, for example, would provide an excellent exercise demonstrating the value of the healthcare team in practice. Interdisciplinary student learning is an area of focus within many of the colleges at the University of Rhode Island.
The positive student feedback and comments to other students has resulted in maximum enrollment for the next offering with requests for course enrollment overrides. Related to this, pharmacy students are actively interested in working with older adults as part of community programs. A new chapter of the American Society of Consultant Pharmacists (ASCP) has been formed within the college to provide an organized group to continue the intergenerational outreach events within the community. Attendance at initial group meetings has been high, indicating a strong interest in embracing these activities.
The active-learning components within this elective are consistent with other courses at other colleges of pharmacy focusing on simulation exercises and interactive tools.11,12 The Mylan School of Pharmacy reported on their successful elective sequence with a geriatric concentration as a way to introduce students to the pharmaceutical care needs of older adults, provide exposure to career options, and encourage students to pursue advanced training and education in geriatrics.13 These examples are in line with ACPE's required inclusion of special populations within the pharmacy curriculum, further emphasizing the need to provide education in the area of geriatrics.2
The most rewarding part of teaching this course is harnessing the enthusiasm that exists between the generations into a valuable learning experience for everyone involved. Participation continues to grow and this unexpected element enhances the intergenerational value of the course for both students and the older adult volunteers. The most common question from the residents at South Bay Manor is, “When are the students coming back?” – a sure sign that the relationship will continue.
SUMMARY
The objectives of this course were to promote students' understanding of age-related physiologic changes influencing pharmacokinetics and pharmacodynamics, as well as of assessment techniques for evaluating functional status and complex drug regimens. The course objectives also stressed the importance of interdisciplinary teams in the provision of care, issues in evaluating evidence from clinical trials, and recognition of the limitations of evidence-based practice in geriatrics. Through this course, students became more confident and willing to interact with older adults, and hopefully this will translate into potential career paths in geriatrics. Similarly, older adults were impressed by the knowledge and caring nature of these future pharmacists.
ACKNOWLEDGMENTS
We acknowledge the individuals from South Bay Manor for their continued enthusiasm and participation with the students within this course offering. Their involvement has made this course a truly positive experience for everyone involved. Also a special thank you to the staff at South Bay Manor, specifically, Kyle Ellis, Administrator; Heather Beauchemin, RN, Director of Wellness; and Christine Sheil, Resident Program Manager, for embracing the opportunity to collaborate in this intergenerational learning endeavor.
Appendix 1.
Adopt-a-Patient Project: EXAMPLE
Patient XX is a 79-year-old man presenting with no current complaints. He is receiving treatment for hypertension and hyperlipidemia and self-treats for osteoarthritis, constipation, and seasonal allergies. Patient also takes a daily multivitamin and nutritional supplement for macular degeneration. The patient lives in an assisted living facility and ambulates with two canes.
Adopt-a-Patient Project: Student counseling points (for patient volunteer) – SAMPLE
Dear Mr. XX,
We really appreciate having the opportunity to visit with you. We thoroughly enjoyed our time talking with you. Here is a list of some suggestions for you to think about:
- Make sure you have enough space in your room for you to move around.
- When filling pill container for the week it may be helpful to sit down while filling the container. Placing a plate under the pill container will help prevent dropping pills on the floor.
- Be sure to space apart taking your ibuprofen from your aspirin and daily vitamins by at least two hours.
- When taking ibuprofen be sure to take with food to prevent stomach upset. If you find your pain is becoming worse, there are other options available if you speak with your doctor or pharmacist.
- Try to make healthy eating choices and try to control portion sizes.
- Be sure to visit your doctors frequently.
Once again, thank you for welcoming us into your home.
Sincerely,
___________&___________, PharmD Students
University of Rhode Island College of Pharmacy
Note: Once the recommendations were reviewed and approved by the instructors, a summary was also provided to the Wellness Director and there is an opportunity to discuss the findings at that time.
EXAMPLE : Adopt-a-Patient Project: Student recommendations to the Wellness Director
To: Director of Wellness
After speaking with Mr. XX, we have a few suggestions regarding his care:
His apartment has a lot of clutter so be sure that he has adequate room to ambulate around his room with his two canes.
He reported that he has difficulty seeing his pills when they fall on the ground while filling his pill container weekly. We suggested that he stay seated while filling the container and to place a plate underneath the pill container to prevent them from falling on the floor.
His medications were not expired and he is taking all of his medications correctly.
Patient reports eating too much but enjoys the meals that are served.
Patient seems to visit his doctors regularly and should continue to do so.
Mr. XX is in good health and seems to be very happy at his residence.
Thank you for allowing us to speak with Mr. XX . We hope these suggestions are helpful to you.
Sincerely,
_______&__________, PharmD Students
University of Rhode Island College of Pharmacy
REFERENCES
- 1.Institute of Medicine. Retooling for an Aging America: Building the Health Care Workforce. Washington, DC: National Academy Press; 2008. [PubMed] [Google Scholar]
- 2. Accreditation Council on Pharmaceutical Education Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree, Chicago, IL 2006. Available at: http://www.acpe-accredit.org/standards/default.asp. Accessed March 20, 2010.
- 3.Odegard PS, Breslow RM, Koronkowski MJ, William BR, Hudgins GA. Geriatric pharmacy education: A strategic plan for the future. Am J Pharm Educ. 2007;71(3) doi: 10.5688/aj710347. Article 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Folstein MF, Folstein SE, McHugh PR. Mini-Mental State: A practical method for grading cognitive state for patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 5.Tinetti ME, Williams TF, Mayewski R. Fall Risk Index for elderly patients based on number of chronic disabilities. Am J Med. 1986;80(3):429–434. doi: 10.1016/0002-9343(86)90717-5. [DOI] [PubMed] [Google Scholar]
- 6.Bergstrom N, Braden BJ, Laguzza A, Holman V. The Braden Scale for predicting pressure sore risk. Nurs Res. 1987;36(4):205–210. [PubMed] [Google Scholar]
- 7.Hanlon JT, Schmader KE, Samsa GP, et al. A method for assessing drug therapy appropriateness. J Clin Epidemiol. 1992;45(10):1045–1051. doi: 10.1016/0895-4356(92)90144-c. [DOI] [PubMed] [Google Scholar]
- 8.Fick DM, Cooper JW, Wade WE, et al. Updating the Beer's Criteria for potentially inappropriate medication use in older adults. Arch Intern Med. 2003;163(22):2716–2724. doi: 10.1001/archinte.163.22.2716. [DOI] [PubMed] [Google Scholar]
- 9.Anderson K. Identifying patients at risk for medication mismanagement: using cognitive screens to predict a patient's accuracy in filling a pillbox. Consult Pharm. 2008;23(6):459–472. doi: 10.4140/tcp.n.2008.459. [DOI] [PubMed] [Google Scholar]
- 10.Snowdon D. Aging with Grace: What the Nun Study Teaches Us About Leading Longer, Healthier, and More Meaningful Lives. New York, NY: Bantam; 2001. [Google Scholar]
- 11.Divine HS, Cain J. Assessing the effect of a polypharmacy medication adherence simulation project in a geriatrics course in a college of pharmacy. J Am Geriatr Soc. 2009;57(8):1487–1491. doi: 10.1111/j.1532-5415.2009.02364.x. [DOI] [PubMed] [Google Scholar]
- 12.Kennedy DH, Fanning KD, Thornton PL. The age game: an interactive tool to supplement course material in a geriatrics elective. Am J Pharm Educ. 2004;68(5) Article 115. [Google Scholar]
- 13.Keys PA, O'Neil C, Maher R. Geriatric concentration: a new elective sequence in an entry level doctor of pharmacy program. Am J Pharm Educ. 2004;68(1) Article 7. [Google Scholar]