Abstract
Objectives
To determine the impact of active-learning strategies in a medication therapy management (MTM) elective on pharmacy students' preparedness to participate in real-life MTM counseling sessions.
Design
The elective included active-learning assignments such as patient cases, group discussions, role playing, and use of actual patients to prepare students for MTM services.
Assessment
A survey was administered before (week 11) and after (week 15) completing a face-to-face comprehensive medication review (CMR) to evaluate achievement of course objectives and students' preparedness to participate in MTM. In the pre-CMR survey, 66.7% of the students strongly agreed that the course prepared them to provide MTM services. In the post-CMR survey, 88.9% of the students strongly agreed (p = 0.046).
Conclusion
The active-learning strategies used in the MTM elective course provided students with the skills necessary to participate in MTM counseling sessions. Face-to-face CMRs better prepared pharmacy students to provide MTM services.
Keywords: medication therapy management, elective, active learning, comprehensive medication review
INTRODUCTION
With the cost of medication-related morbidity and mortality totaling more than $177 billion, a tremendous need exists for identifying, addressing, and preventing medication-related problems.1 Pharmacists as medication experts are well positioned to lead these efforts. Pharmacist-led medication therapy management (MTM) sessions have proven to be valuable, showing improvements in clinical, economic, and humanistic outcomes.2-7
Prior to the Medicare Prescription Drug, Improvement, and Modernization Act (MMA) of 2003, most pharmacies were not engaged in providing clinical patient care services.8-10 The MMA required MTM programs to be a part of the Medicare Part D and Medicare Advantage prescription drug plans, which in turn led to a profession-wide consensus statement to define MTM as a distinct service or group of services, provided by a pharmacist or other qualified health care provider, that optimizes therapeutic outcomes for individual patients.8,11-13 Since 2006, when the MMA was implemented, many pharmacists have embraced the opportunity to become involved in MTM14; however, barriers exist for them to participate, including lack of understanding of the components of MTM services, and lack of availability and accessibility of MTM educational resources.15
With the increased opportunities for MTM, pharmacists and pharmacy students will require MTM-specific education. Continuing education and training programs, such as the American Pharmacists Association's Delivering Medication Therapy Management Services in the Community certificate training program, have been developed to assist with pharmacist education on MTM. According to the Accreditation Council for Pharmaceutical Education (ACPE) accreditation standards and the Center for the Advancement of Pharmacy Education (CAPE) outcomes, pharmacy education must prepare students to provide patient-centered care.16,17 Pharmacy students should be able to design, implement, monitor, evaluate, and adjust pharmaceutical care plans that are patient specific.17 In addition, ACPE requires instructors to incorporate teaching methods, such as the use of case studies, group discussions, and simulated or actual patients, that produce competent pharmacists and foster the development of critical-thinking and problem-based learning skills.16 The elective course, Patient-Centered Approach to Medication Therapy Management, was developed to offer students an opportunity to learn more about MTM and to prepare them for patient interaction by incorporating many of the active-learning strategies suggested by ACPE.
No previous studies have been performed to identify whether student pharmacists have been prepared or feel prepared to offer MTM based on current pharmacy curriculum. This study was designed to: (1) evaluate the fulfillment of the course objectives; (2) determine whether face-to-face comprehensive medication reviews provided by student pharmacists would improve the students' class experience; (3) determine whether the students felt the elective course prepared them to participate in real-life MTM counseling sessions; and (4) determine whether participation in the course influenced the student's decision to participate in MTM in the future.
DESIGN
In 2009, the Patient-Centered Approach to Medication Therapy Management elective course was offered for the first time to doctor of pharmacy (PharmD) students at the South Carolina College of Pharmacy (SCCP), Charleston campus. The 2-credit elective course was designed to prepare students to counsel patients during the delivery of medication therapy management. The course required students to possess pharmacotherapy knowledge, therefore it was offered during the spring semester of their third year. By this point in the curriculum, the students were in their final semester of pharmacotherapy, having already completed 1 semester of self-care therapeutics, 5 semesters of a case-based course entitled Clinical Applications, and 2 semesters of pharmacotherapy.
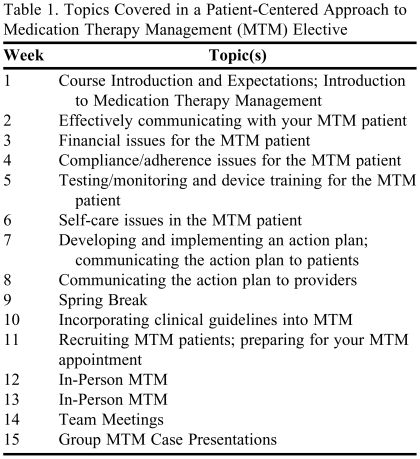
Eighteen students were enrolled in the first offering of the course. The first 11 weeks of the course were held in the classroom setting and consisted of interactive lectures, group discussions, and in-class activities about various MTM topics (Table 1). The course objectives were designed around the highest levels of Bloom's Taxonomy of Learning to develop the students' problem-solving skills.18 The primary objective for each class session was to provide background about medication therapy management to prepare the students to perform real-life comprehensive medication reviews. Various active-learning techniques were used throughout the semester and counted as part of the students' in-class activity grade. Some of the techniques used to develop the students' critical-thinking skills included patient cases, group discussions, and role playing. (Examples of in-class activities are available upon request from the authors.) The last half-hour to hour of the class generally was used for in-class activities. No course textbook was required; instead, handouts developed by course instructors were used. Four instructors, with experience in clinical community pharmacy practice and medication therapy management, taught the course.
Table 1.
Topics Covered in a Patient-Centered Approach to Medication Therapy Management (MTM) Elective
While role-playing activities were incorporated throughout the semester to simulate pharmacist-patient interactions, the course also expected the students to have face-to-face interactions with patients. Face-to-face interactions are beneficial because they “optimize the pharmacist's ability to observe signs and visual cues to the patient's health problems and can enhance the patient-pharmacist relationship.”13 At the end of the semester, on 2 separate occasions, the students visited a local senior center that hosted low-income and homeless patients. Students worked in teams of 3 to deliver MTM to 2 to 3 patients over the 2 weeks in which the class sessions were scheduled. During the patient visits, the students practiced the skills learned during class. Students performed a comprehensive medication review (CMR), developed a personal medication record (PMR) for the patient, and developed a medication action plan (MAP). The patients were encouraged to discuss the students' referrals or recommendations with their primary care provider. The students then prepared and presented their group MTM cases based on the patients seen at the senior center. Students completed peer evaluations of their team members and a take-home final examination to earn the remaining points toward their grade for the course.
Students' performance and knowledge were evaluated over the course of the semester by completion of in-class activities, in-person CMRs, group MTM case presentations, and take-home final examinations. In-class activities were evaluated weekly for completeness and quality. Two community pharmacy faculty members supervised students performing CMRs at the senior center and provided feedback during and following the visits. For the group MTM case presentations, each student group presented a 12- to 15-minute PowerPoint presentation on one of the patients seen at the senior center. The presentation included the following items: subjective, objective, assessment, and plan (SOAP) for the patient's medication-related problems; evidence behind recommendations made; and general reflections of counseling experiences at the senior center. Two course faculty members evaluated the final presentations using a customized evaluation tool. Students were also required to evaluate their peers' performances and participation during the project. (Both the presentation and peer evaluation tools are available from the author upon request.) Last, students were required to complete a take-home examination, which consisted of 2 to 3 questions per lecture topic, and included mostly short-answer and case-based short-answer questions, but also some multiple-choice and true/false questions.
EVALUATION AND ASSESSMENT
A 23-item survey instrument was constructed to evaluate the fulfillment of course objectives, students' perceived value of face-to-face CMRs, students' preparedness to participate in real-life MTM counseling sessions, and students' decision to participate in MTM in the future. A 5-point Likert scale (1 = strongly disagree; 2 = disagree; 3 = neutral; 4 = agree; 5 = strongly agree) was used for students to indicate their level of agreement or disagreement with each statement. The instrument was reviewed by 4 community-based faculty members for appropriateness and by 2 student volunteers for content interpretation. The survey was approved as an exempt study by the institutional review board of the Medical University of South Carolina.
The paper survey instrument, which took 5 to 10 minutes to complete, was distributed to all students at the end of class during week 11 (pre-CMR survey) and again during week 15 (post-CMR survey) of the course. The survey was anonymous, no incentives were provided, and participation was voluntary. Demographic information was collected to determine the students' past and current experiences and interest in community pharmacy and MTM. General comments on the course were not solicited. The completed survey instruments were analyzed using SPSS, version 11.0.4 (SPSS, Chicago, IL). Descriptive statistics were used to evaluate Likert scales and the Wilcoxon signed-rank test was used to analyze ordinal data with alpha set at 0.05.
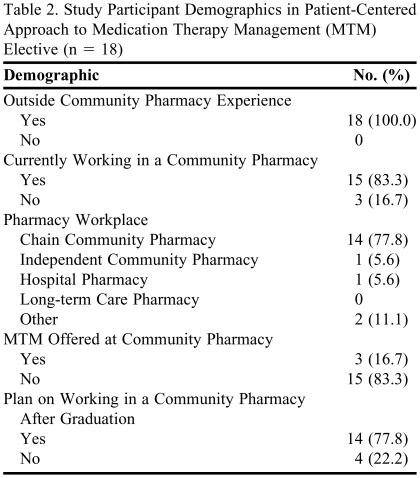
All 18 students enrolled in the elective provided usable responses on both the pre-CMR and post-CMR surveys. Most respondents had community pharmacy experience outside of the pharmacy curriculum, worked at a chain community pharmacy that did not offer MTM at the time of survey completion, and planned to work in a community pharmacy upon graduation (Table 2).
Table 2.
Study Participant Demographics in Patient-Centered Approach to Medication Therapy Management (MTM) Elective (n = 18)
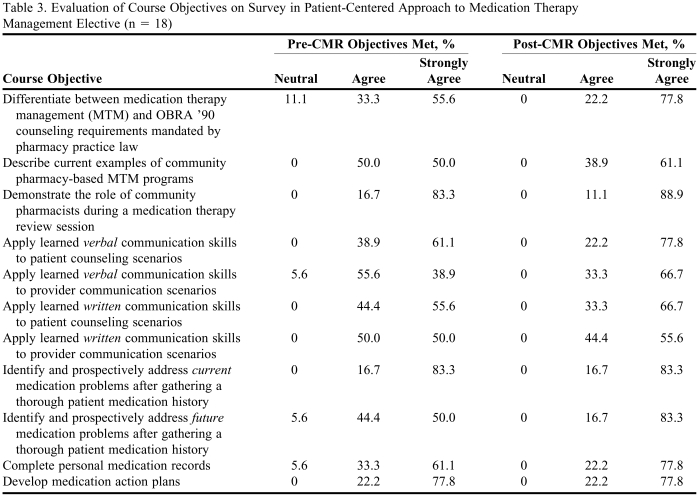
Table 3 lists the percentage of students answering each item on the Likert scale based on course objectives. Results were divided into both week 11 (pre-CMR) and week 15 (post CMR). None of the students answered strongly disagree or disagree when evaluating the course objectives and expectations pre- and post-CMR. Responses to statements assessing course objectives were positive, with only a few neutral responses on the pre-CMR survey instruments. Although not significant, post-CMR results were more positive than pre-CMR results. None of the students answered neutral on the post-CMR survey and there were greater trends in answers toward strongly agree on all objectives post-CMR. Of note, the percent of students answering strongly agree increased on 9 of the 11 course objectives from pre- to post-CMR survey. In one particular objective assessment, “identify and prospectively address future medication problems after gathering a thorough patient medication history,” 15 students selected strongly agree on the post-CMR survey compared to only 9 students on the pre-CMR survey.
Table 3.
Evaluation of Course Objectives on Survey in Patient-Centered Approach to Medication Therapy Management Elective (n = 18)
Abbreviations: OBRA '90 = Omnibus Budget Reconciliation Act of 1990
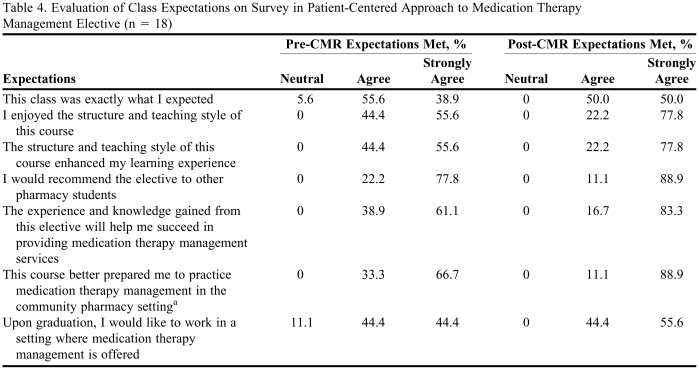
Survey results based on course expectations were similarly positive pre-CMR with a trend to even more positive answers post-CMR. More students selected strongly agree for each expectation statement post-CMR compared to pre-CMR. There was a significant improvement in one particular course expectation, “This course better prepared me to practice medication therapy management in the community pharmacy setting” (p = 0.046; Table 4).
Table 4.
Evaluation of Class Expectations on Survey in Patient-Centered Approach to Medication Therapy Management Elective (n = 18)
a Wilcoxon signed-rank test significant difference between Pre-CMR and Post-CMR responses (p = 0.046)
DISCUSSION
A Patient-Centered Approach to MTM was an elective course offered to third-year pharmacy students enrolled on the Charleston campus of the SCCP. The course was designed to provide students with the knowledge and skills necessary for participating in MTM services. This study evaluated the effect the course had on pharmacy students' preparedness for providing MTM in the community setting.
One objective of the study was to evaluate the effect of a face-to-face CMR on students' perceptions of the course. After the face-to-face CMR, all 18 students either agreed or strongly agreed that taking the course allowed them to meet all course objectives. Some objectives had more positive results than others. More students felt strongly about being able to distinguish between MTM and the guidelines provided in the Omnibus Budget Reconciliation Act of 1990 (OBRA '90), apply verbal communication skills to counseling sessions, identify and address future medication problems, and complete a personal medication review post-CMR than pre-CMR. There was no significant difference in students' ability to meet course objectives pre- and post-CMR, suggesting that the course was effective in meeting all objectives before the face-to-face CMR took place.
During the in-class activities, a faculty member observed the students' work and provided verbal feedback. After the activity was completed in groups, 1 to 2 student groups were asked to share their work and/or perform the role-playing exercise for the entire class to stimulate class discussion and reinforce the learning objectives for that lecture. The in-class activities, such as role-playing, were designed specifically to develop students' communication and problem-solving skills, and may have been sufficient in meeting course objectives. This finding is important because some pharmacy schools may not have the resources available to provide real patients for student-provided MTM sessions.
Similar to the course objective responses, the majority of students either agreed or strongly agreed with the survey statements regarding their expectations of the course. The majority of the pre-CMR responses were not significant compared to the post-CMR responses, suggesting the in-class activities increased the students' satisfaction with the course. Interestingly, the face-to-face CMR did not increase the students' desire to work in a setting where MTM is offered. The lack of significant difference between pre- and post-CMR responses for this statement may have been due to the population surveyed. Third-year pharmacy students at the college had several different electives from which to choose, and that the students chose to enroll in this course suggested they had a desire to conduct MTM sessions prior to taking the course.
Before the face-to-face CMR, only 8 students strongly agreed with the statement that the course better prepared them to practice MTM in the community pharmacy setting. This was significant compared to 16 students who strongly agreed with that statement post-CMR, suggesting experience providing real-life MTM services improved students' confidence in providing MTM in the community setting. These results were consistent with research findings that pharmacists with MTM experience were significantly less likely to report barriers to MTM than pharmacists without MTM experience.15 Pharmacists contracted with a Medicare Part D company to provide MTM also were significantly more comfortable with providing MTM services than pharmacists without a contract to provide MTM.19 Pharmacists with direct patient care experience were better able to conduct medication therapy reviews, develop medication action plans, and intervene and/or refer on the patient's behalf than pharmacists without direct patient care experience.20
A strength in the design of the course was the incorporation of lecture, in-class active learning assignments, and interaction with real patients. Evidence suggests that patient simulation in pharmacy courses improves the learning experience for students.21 Additional evidence suggests that pharmacy students prefer real-life patients over standardized patients.22 The ACPE recommends using real patients whenever possible.16 Even though there was no significant difference between students' pre- and post-CMR responses regarding meeting course objectives, the results supported the incorporation of real-life MTM sessions in pharmacy courses.
There are limitations to this study that should be considered when interpreting the results. The course was offered only once, thus only 1 year of student responses is reported here. Also, only 18 students were enrolled the first year and some of the nonsignificant results may have been due to the limited number of students. After multiple offerings of the course, additional differences between pre- and post-CMR responses may become evident. The study investigators decided to publish results after only 1 course offering due to the lack of available literature on MTM in the pharmacy curriculum. Future evaluations of the course will need to address areas of improvement for the course to continue to be effective in preparing pharmacy students for MTMs. Also, research will need to be conducted post-course to determine if students continue to apply their MTM skills.
The objective of this study was not to evaluate students' preparedness to develop and implement MTM services. The college also offers another MTM elective, Medication Therapy Management, that is designed to prepare students to create and implement an MTM service, and covers topics such as barriers to implementation, reimbursement, and quality assurance. In addition, students enrolled in the course are required to write and present a business plan for an MTM service they develop. Future research will determine what effect the alternate course has on students' preparedness to develop and implement MTM services and evaluate the benefit of taking both MTM courses versus only 1 course, or none at all.
Since the survey instruments were administered near the end of the semester, the course's ability to meet objectives may not have been adequately evaluated. A significant difference may have been found if the survey instruments had been administered at the beginning and end of the course instead of before and after the face-to-face CMR. The survey responses, however, suggest that the design of the course prior to the face-to-face CMR was sufficient to meet the course objectives. In fact, the face-to-face CMR may have enhanced several learning objectives. A larger study population may have identified differences not found with this study. Also, more significant results may have been found if student preparedness to conduct MTM was compared among students who took the elective and students who did not. Study investigators chose to survey only students enrolled to evaluate the effectiveness of the active-learning strategies.
Another limitation was the inability to offer this course to all pharmacy students at the South Carolina College of Pharmacy. SCCP has 2 campuses, one in Charleston, SC, and the other in Columbia, SC. During the study, the majority of courses were offered via video conferencing. For the first year, this elective was offered only on the Charleston campus. Offering the course via distance education technology may present several problems. In-class activities will have to be modified to accommodate the distance education platform, and a coordinator on the Columbia campus will have to find patients for the face-to-face CMR.
SUMMARY
A medication therapy management elective, Patient-Centered Approach to MTM, provided students with the skills necessary to participate in MTM counseling sessions. Pharmacy students who completed the course expressed positive attitudes toward the elective. Overall, the students believed the course fulfilled its objectives prior to the face-to-face comprehensive medication review; however, conducting the real-life MTM session increased the students' preparedness to provide MTM services. Pharmacy faculty members should incorporate an MTM elective similar to this course into their curriculum to prepare their students for MTM in the community setting. If possible, actual patients should be used to provide students with experience conducting MTM counseling sessions.
ACKNOWLEDGMENTS
We would like to thank Kristy Brittain, PharmD, for co-teaching the Patient-Centered Approach to MTM elective course in spring 2009, during the time this study was conducted.
REFERENCES
- 1.Ernst FR, Grizzle AJ. Drug-related morbidity and mortality: updating the cost-of-illness model. J Am Pharm Assoc. 2001;41(2):192–199. doi: 10.1016/s1086-5802(16)31229-3. [DOI] [PubMed] [Google Scholar]
- 2.Bunting BA, Cranor CW. The Asheville Project: long-term clinical, humanistic, and economic outcomes of a community-based medication therapy management program for asthma. J Am Pharm Assoc. 2006;46(2):133–147. doi: 10.1331/154434506776180658. [DOI] [PubMed] [Google Scholar]
- 3.Bunting BA, Smith BH, Sutherland SE. The Asheville Project; clinical and economic outcomes of a community-based long-term medication therapy management program for hypertension and dyslipidemia. J Am Pharm Assoc. 2008;48(1):23–31. doi: 10.1331/JAPhA.2008.07140. [DOI] [PubMed] [Google Scholar]
- 4.Cranor CW, Bunting BA, Christensen DB. The Asheville Project: long-term clinical and economic outcomes of a community pharmacy diabetes care program. J Am Pharm Assoc. 2003;43(2):173–184. doi: 10.1331/108658003321480713. [DOI] [PubMed] [Google Scholar]
- 5.DaVanzo J, Dobson A, Koenig L. Medication therapy management services: a critical review. J Am Pharm Assoc. 2005;45(5):580–587. doi: 10.1331/1544345055001328. [DOI] [PubMed] [Google Scholar]
- 6.Fera T, Bluml BM, Ellis WM, Schaller CW, Garrett DG. The Diabetes Ten City Challenge: interim clinical and humanistic outcomes of a multistate community pharmacy diabetes care program. J Am Pharm Assoc. 2008;48(2):181–190. doi: 10.1331/JAPhA.2008.07166. [DOI] [PubMed] [Google Scholar]
- 7.Touchette DR, Burns AL, Bough MA, Blackburn JC. Survey of medication therapy management programs under Medicare Part D. J Am Pharm Assoc. 2006;46(6):683–691. doi: 10.1331/1544-3191.46.6.683.touchette. [DOI] [PubMed] [Google Scholar]
- 8. Public Law 108-13. The Medicare Prescription Drug, Improvement, and Modernization Act of 2003. HR 1. December 8, 2003. http://www.cms.hhs.gov/MMAUpdate/downloads/PL108-173summary.pdf. Accessed February 17, 2010.
- 9.Christensen DB, Farris KB. Pharmaceutical care in community pharmacies: practice and research in the US. Ann Pharmacother. 2006;40(7):1400–1406. doi: 10.1345/aph.1G545. [DOI] [PubMed] [Google Scholar]
- 10.Doucette WR, Kreling DH, Schommer JC, Gaither CA, Mott DA, Pedersen CA. Evaluation of community pharmacy service mix: evidence from the 2004 National Pharmacist Workforce Study. J Am Pharm Assoc. 2006;46(3):348–355. doi: 10.1331/154434506777069471. [DOI] [PubMed] [Google Scholar]
- 11.American Pharmacists Association and National Association of Chain Drug Stores Foundation. Medication therapy management in community pharmacy practice: core elements of an MTM service (version 1.0) J Am Pharm Assoc. 2005;45(5):573–579. doi: 10.1331/1544345055001256. [DOI] [PubMed] [Google Scholar]
- 12.American Pharmacists Association and National Association of Chain Drug Stores Foundation. Medication therapy management in community pharmacy practice: core elements of an MTM service (version 2.0) J Am Pharm Assoc. 2008;48(3):341–353. doi: 10.1331/JAPhA.2008.08514. [DOI] [PubMed] [Google Scholar]
- 13.Bluml BM. Definition of medication therapy management: development of professionwide consensus. J Am Pharm Assoc. 2005;45(5):566–572. doi: 10.1331/1544345055001274. [DOI] [PubMed] [Google Scholar]
- 14.Touchette DR, Burns AL, Bough MA, Blackburn JC. Survey of medication therapy management programs under Medicare Part D. J Am Pharm Assoc. 2006;46(6):683–691. doi: 10.1331/1544-3191.46.6.683.touchette. [DOI] [PubMed] [Google Scholar]
- 15.Lounsbery JL, Green CG, Bennett MS, Pedersen CA. Evaluation of pharmacists' barriers to the implementation of medication therapy management services. J Am Pharm Assoc. 2009;49(1):51–58. doi: 10.1331/JAPhA.2009.017158. [DOI] [PubMed] [Google Scholar]
- 16. Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. http://www.acpe-accredit.org/standards/default.asp. Accessed February 17, 2010.
- 17. American Association of Colleges of Pharmacy, Center for the Advancement of Pharmaceutical Education (CAPE) Advisory Panel on Educational Outcomes. Educational Outcomes, revised version 2004.
- 18.Bloom BS, editor. Taxonomy of Educational Objectives. The Classification of Educational Goals. Handbook I: Cognitivie Domain. New York, NY: McKay; 1956. [Google Scholar]
- 19.McIntosh C, Weiser C, Wassimi A, Reddick J, Scovis N, Guy M, Boesen K. Attitudes toward and factors affecting implementation of medication therapy management services by community pharmacists. J Am Pharm Assoc. 2009;49(1):26–30. doi: 10.1331/JAPhA.2009.07122. [DOI] [PubMed] [Google Scholar]
- 20.Moczygemba LR, Barner JC, Roberson K. Texas pharmacists' opinions about and plans for provision of medication therapy management services. J Am Pharm Assoc. 2008;48:38–45. doi: 10.1331/JAPhA.2008.07015. [DOI] [PubMed] [Google Scholar]
- 21.Seybert AL, Kobulinsky LR, McKaveney TP. Human patient simulation in a pharmacotherapy course. Am J Pharm Educ. 2008;72(2) doi: 10.5688/aj720237. Article 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gallimore C, George AK, Brown MC. Pharmacy students' preferences for various types of simulated patients. Am J Pharm Educ. 2008;72(1) doi: 10.5688/aj720104. Article 4. [DOI] [PMC free article] [PubMed] [Google Scholar]