Abstract
Objectives
To determine whether students' previous pharmacy-related work experience was associated with their pharmacy school performance (academic and clinical).
Methods
The following measures of student academic performance were examined: pharmacy grade point average (GPA), scores on cumulative high-stakes examinations, and advanced pharmacy practice experience (APPE) grades. The quantity and type of pharmacy-related work experience each student performed prior to matriculation was solicited through a student survey instrument. Survey responses were correlated with academic measures, and demographic-based stratified analyses were conducted.
Results
No significant difference in academic or clinical performance between those students with prior pharmacy experience and those without was identified. Subanalyses by work setting, position type, and substantial pharmacy work experience did not reveal any association with student performance. A relationship was found, however, between age and work experience, ie, older students tended to have more work experience than younger students.
Conclusions
Prior pharmacy work experience did not affect students' overall academic or clinical performance in pharmacy school. The lack of significant findings may have been due to the inherent practice limitations of nonpharmacist positions, changes in pharmacy education, and the limitations of survey responses.
Keywords: work experience, performance admissions, academic performance, high-stakes testing
INTRODUCTION
In spite of the increase in the number of colleges and schools of pharmacy during the last decade, the number of admission applications to doctor of pharmacy (PharmD) programs still exceeds the number of slots available. In fact, there was a 7% increase in the number of applicants in 2007-2008, preceded by a 3.5% increase in 2006-2007.1 With multiple qualified candidates vying for each position within a class, colleges of pharmacy are faced with many challenges in evaluating applicants for admission. The profession of pharmacy has shifted from a science-based mode of practice to a clinically based patient-centered practice; thus, colleges of pharmacy are faced with the added burden of identifying student characteristics that predict clinical success as well as academic success. As the responsibilities of pharmacy practice expand from filling prescriptions to providing pharmaceutical care, colleges and schools have a responsibility to identify preadmission factors associated with applicants' ability to provide patient-care services in a multidisciplinary setting. A clear understanding of these factors will ensure that students with the greatest potential to maximize patient outcomes and provide optimal quality of care will be matriculated.
Academic performance or success has been defined as early classroom grade point average (GPA for first 3 years).2-8 Clinical success generally has been measured by experiential performance, namely grades in introductory pharmacy practice experiences (IPPEs) or advanced pharmacy practice experiences (APPEs). Other measures of pharmacy student clinical performance have included low-stakes progress examinations, high-stakes progress examinations, and case-based objective structured clinical examinations (OSCEs). These measures tend to be more qualitative or subjective than classroom grades and generally have been less accurate in predicting students' clinical success after graduation.9-12 A detailed description of the various progress examinations in use has recently been presented.13
Little has been done to identify factors that can predict clinical performance accurately, or to predict clinical success in a multidisciplinary patient-care setting. At Touro University-California College of Pharmacy (TU-COP), a cumulative high-stakes examination called the Triple Jump Examination (TJE), given at the end of each of the 4 didactic semesters, is being used to determine the progression of students into clinical APPEs.14 TU-COP is unique in its use of a 2 + 2 medical school-type curriculum format (ie, 2 years of classroom training followed by 2 years of experiential training). The correlation between TJE scores and grades in APPEs has been moderately high (r = 0.59), suggesting that the TJE may be a valid tool to predict success in clinical APPEs.14 However, there is still a significant need to look at both quantitative and qualitative measures of applicants' abilities during the admissions process as such measures may be useful in predicting success in a program.2 Nontraditional factors such as emotional intelligence, motivation, empathy, and leadership can be evaluated with questionnaires and interviews, but are rarely used.15 Other factors that can predict academic success in a PharmD curriculum and clinical success during clerkships have not been determined.
Previous pharmacy work experience likely plays a role in the admission decision process as the assumption is that applicants with prior exposure to the workplace have a more complete understanding of the role of pharmacists in a practice setting.16 The actual impact that previous exposure to the pharmacy workplace has on the clinical success of the student pharmacist is unclear. We hypothesized that experience obtained in the pharmacy workplace prior to matriculation into pharmacy school may have resulted in the accumulation of skills that could be useful during the students' pharmacy school education. However, it is unclear whether specific types of pharmacy experiences vary in their value towards successful completion of either classroom education, experiential (APPE) education, or both. This study attempts to determine the association between a students' previous pharmacy work experience and their pharmacy school academic performance.
METHODS
All students enrolled in the PharmD program at the time the study was conducted were invited to participate in a survey. Any survey instruments that were not returned by the end of the data collection phase or that were incomplete were excluded from analysis. The specific measures of student academic and clinical performance used in the study were: (1) 2 years of didactic training as measured by cumulative pharmacy GPA; (2) cumulative TJE scores; (3) Standardized Pharmacy Curriculum Outcomes Assessment (PCOA) scores; and (4) APPE evaluations.
Prepharmacy GPA, pharmacy GPA, and TJE scores were collected for the sample population of first- through fourth-year (P1-P4) pharmacy students (classes of 2009 through 2012, respectively) This cohort represented the first full complement of students in the TU-COP program. Pharmacy GPA was reported as an average (65% to 100%) across the 4 course tracks: (1) biological sciences, (2) pharmaceutical sciences, (3) social/behavioral/administrative sciences, and (4) clinical sciences. During their P1 and P2 years, students completed 4 courses each semester (16 didactic courses). TJE scores were weighted averages of 3 comprehensive test components: (1) case-based closed-book examination; (2) case-based open-book examination; and (3) an OSCE. The closed-book and open-book examination components of the TJE were designed to assess critical-thinking skills and resource-utilization ability, while the OSCEs were designed to gauge professionalism and knowledge during a simulated patient/provider interaction. The TJEs were given at the end of each semester during the P1 and P2 years (ie, each semester prior to the beginning of experiential training). The PCOA, a standardized examination made available nationwide to pharmacy students beginning in spring 2007, assists in the development of the pharmacy curriculum and measures student academic performance in 4 major content areas: basic biomedical sciences, pharmaceutical sciences, social/behavioral/administrative pharmacy sciences, and clinical sciences.17 The PCOA was administered to TU-COP students in spring 2008 (ie, class of 2009 through class of 2011). APPE scores for P3 and P4 students (65% to 100%) were determined by preceptors. At the time of this survey, first semester APPE scores were available only for the inaugural class of 2009 and the class of 2010 (ie, P3 year experiential training for surveyed P4s).
Prior to dissemination of the survey instrument, a focus group met to determine the appropriateness of the questions, their length, and their understandability. All pharmacy students were invited to participate in the focus group via 2 separate mass e-mails sent to each class. Lunch was provided for the focus group as an incentive.
Guided by feedback from the focus group, an electronic survey instrument was developed to collect demographic information (5 items: student identification number, age, ethnicity, gender, class year), preadmission pharmacy school work experience (2 items: position, setting), whether the experience was paid or unpaid (1 item), and number of hours of work experience prior to entering the TU-COP program (4 items: hours per week, weeks per year, number of years, estimated total hours).
The survey instrument was available via the Blackboard Academic Suite (Blackboard, Inc., Washington, DC). All TU-COP students (classes 2009 through 2012) were asked to complete the survey instrument during a 3-week time period (from February to March 2009), during which the survey was continuously available. Informed consent was obtained from each participant prior to beginning the survey. Students were required to answer questions in sequential order, but were not required to complete the survey instrument during 1 sitting. Also, students could choose to exit the survey instrument at any time prior to submitting their answer to the final question. As an incentive for their participation, students were given an informal, student-compiled study packet with study guides, review tables, and comprehensive presentations. Study protocol was reviewed by the Touro University – California Institutional Review Board (IRB) and the study was determined to be exempt.
Student survey information was linked with pharmacy GPA, TJE scores, PCOA scores, and APPE scores using each student's unique college identification number. Student confidentiality was maintained by limiting investigator access to the registrar's roster linking student name with identification number. A database of all variables was created using SAS, version 9.1.3 (SAS, Cary, NC). Differences in study variables between students with and without work experience prior to matriculation where tabulated. Student t tests were used to compare students' ages, pharmacy GPAs, TJE scores, APPE evaluations, and PCOA scores, while chi-square tests were used to compare students' gender, ethnicity, and graduation year. The relationship between previous work experience and 11 different dependent measures of academic performance were explored, including overall GPA (composite or average (track I-IV) first semester didactic grades) and individual-track first-semester grades, overall and individual component performance on the TJE, PCOA, and first semester APPE grades. A multivariate model accounting for age, gender, and prepharmacy GPA was also assembled. The amount of variance explained by the overall model (r2) was determined and the beta coefficient associated with the dichotomous work experience (yes/no) variable for each multivariate model was reported. Subanalyses were conducted on the work experience only cohort, including impact of type of work setting and position on academic performance. In addition, further analyses were conducted on individuals with substantial work experience, ie, more than 2,000 hours (or roughly 1 year) of previous pharmacy work experience. The a priori level of significance was set at a p value of less than 0.05 (α < 0.05).
RESULTS
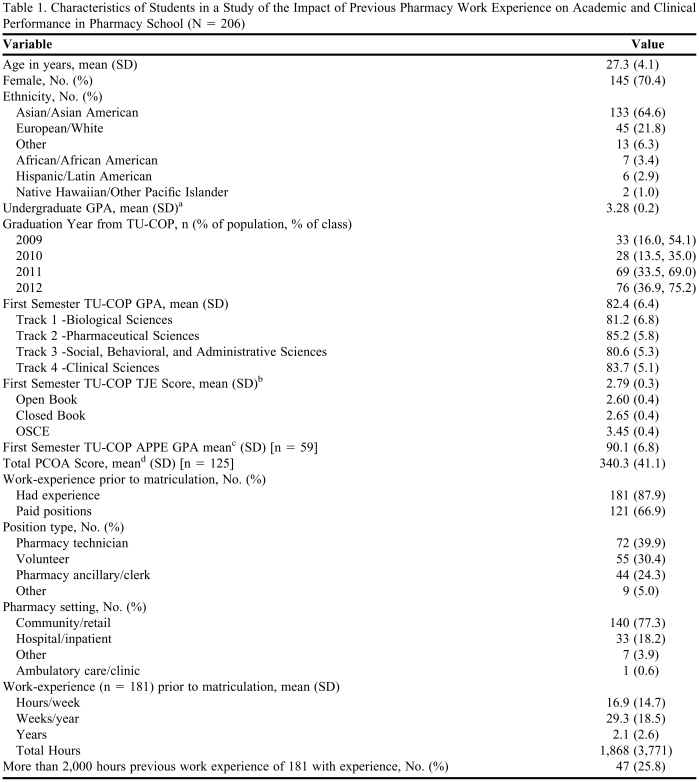
Of 338 eligible students, 239 submitted a survey instrument, for an initial response rate of 70.1%. Of submitted survey instruments, only 206 were fully completed and therefore included in the final analytical cohort, for an overall study inclusion rate of 60.1%. Class of 2009, 2011, and 2012 students were more likely to complete the entire survey instrument (54.1%, 69.0%, and 54.1%, respectively) compared to class of 2010 students (35.0% Table 1).
Table 1.
Characteristics of Students in a Study of the Impact of Previous Pharmacy Work Experience on Academic and Clinical Performance in Pharmacy School (N = 206)
Abbreviations: TU-COP: Touro University – California College of Pharmacy; OSCE: Objective Structured Clinical Examination
a Undergraduate GPA based on a 4-point scale.
b TJE score based on a 4-point scale, scores are meant to be progressive throughout the 2 didactic years.
c TU-COP GPA based on a percent score.
d PCOA score based on 600 point total; national average: 342.
The mean age of respondents was 27.3 years, and 70.4% were female. The majority of respondents (64.6%) were Asian/Asian American; 21.8% were American/European American, and the remaining 13.6% were African/African American, Hispanic/Latin American, Native Hawaiian/Pacific Islander or other. The age, gender, and ethnic breakdown of the study sample closely reflected and were not significantly different from the demographics of the TU-COP student body (p > 0.05). The mean prepharmacy GPA for the study population was 3.3, which did not differ significantly (p > 0.05) from the mean prepharmacy GPA of the entire TU-COP student body. The mean pharmacy GPA of the study group was 82.4%; mean TJE score, 2.79; mean PCOA score, 340.3; and mean APPE score, 90.1%. None of these measures were significantly different from the means for the overall TU-COP student body, suggesting that the study population analyzed was representative of the overall student population.
Of the 206 students responding, 87.9% had some form of pharmacy experience prior to matriculation; the majority (66.9%) had a paid position. The work experience primarily was performed at a community/retail setting (77.3%), with 18.2% having pharmacy experience in a hospital/inpatient setting, and the remaining 4.5% in an ambulatory care or other setting (Table 1). Common positions held were pharmacy technician (39.9%) and volunteer (30.4%), followed closely by pharmacy ancillary/clerk (24.3%) and other (5.0%) (Table 1). The 189 students who had pharmacy work experience averaged 16.9 hours of work per week, 29.3 weeks per year, and 2.1 years, for an average of 1,869 hours of experience per student prior to beginning the PharmD program.
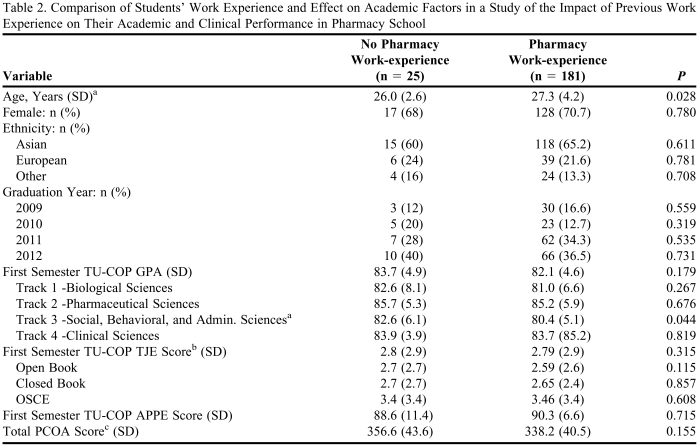
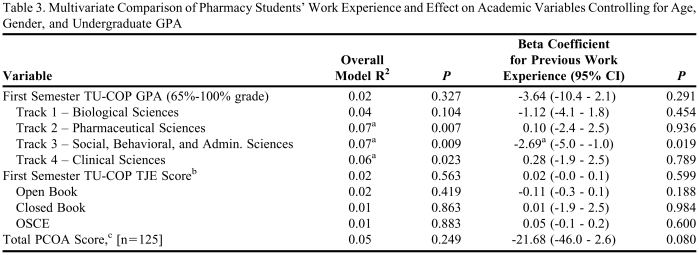
Bivariate analysis (Table 2) revealed no significant differences between the 2 groups (prior pharmacy work experience vs. no prior pharmacy work experience), except for age and track 3 (social/behavioral/administrative sciences) first semester grade (track 3 pharmacy GPA). Multivariate analyses (Table 3) controlling for age, gender, and prepharmacy GPA revealed no significant differences between the 2 groups for any measure of pharmacy school performance, with the exception of first semester track 3 (social/behavioral/administrative sciences) grades. A set of stratified-analyses examining the potential effect of previous work setting (ie, community/retail, hospital/inpatient, ambulatory care/clinic, other) and specific position type (pharmacy technician, volunteer, pharmacy ancillary/clerk, other) on the dependent academic measures examined found no significant differences. Finally, a subanalysis was performed to determine the potential impact of substantial work experience (more than 2,000 hours, n = 47) among those with work experience (n = 181). No differences among the 11 measures of academic performance were observed between the cohort with substantial work experience and the cohort with some work experience.
Table 2.
Comparison of Students' Work Experience and Effect on Academic Factors in a Study of the Impact of Previous Work Experience on Their Academic and Clinical Performance in Pharmacy School
a p < 0.05
b TJE score based on a 4-point scale. Scores are meant to be progressive throughout the 2 didactic years.
c PCOA score based 600 point total; national average: 342.
Table 3.
Multivariate Comparison of Pharmacy Students' Work Experience and Effect on Academic Variables Controlling for Age, Gender, and Undergraduate GPA
a p < 0.05
b TJE Score based on a 4-point scale. Scores are meant to be progressive throughout the 2 didactic years.
c PCOA Score based 600 point total; national average: 342.
DISCUSSION
Several studies have been conducted to evaluate prepharmacy factors that could be used as predictors of academic performance, clerkship success, and success in passing the NAPLEX.4-10;18,19 Many preadmission factors considered singly or collectively seem to offer insight into students' ability to perform academically, but do not explain fully or provide a model for identifying students who will be successful in the clinical setting. In recognizing the limitations of cognitive factors, assessing the impact of noncognitive factors is needed. The current study sought to explore 1 of these factors: preadmission pharmacy work experience. The objective was to determine whether an association exists between prior pharmacy work experience and academic/clinical performance as measured by GPA, TJE scores, PCOA scores, and APPE scores for students enrolled in the TU-COP PharmD program. The analyses detected few overall differences, suggesting little difference between the academic and clinical performance of students with and without work experience.
As pharmacy education continues to evolve from a technical-based to a clinical-based profession, prepharmacy work experience may not be as academically beneficial as initially hypothesized. While scientific knowledge and technical skills are essential to being successful as a pharmacist, contemporary pharmacy practice also requires cognitive, interpersonal, and managerial abilities that often cannot be learned adequately through work experience in a technical role (eg, pharmacy assistant). The kind of positions students are qualified to hold prior to completing pharmacy school may allow them to gain an understanding of the field of pharmacy in general, but would not necessarily teach them the art of pharmacy practice. Specifically, most pharmacy work settings would provide a student with little, if any, formal exposure to pharmacology, cultural competency, or clinical training.
There are inherent limitations to pharmacy practice for those who do not possess a pharmacy degree. For example, nonpharmacist personnel are relegated to positions involving only the noncognitive functions of pharmacy practice including customer service, inventory, dispensing, and third-party processing. Though essential to pharmacy operations, these positions offer little experience performing the actual responsibilities of a pharmacist such as making clinical judgments, conducting consultations, and reviewing patients' medication regimens. Such roles can be learned on the surface perhaps, but not to the degree required to function as a clinically competent pharmacist.
Stratified analysis revealed a significant difference between the 2 groups in the study as to age and early track 3 pharmacy GPA. Students with work experience tended to be older (mean = 27.3 years) compared to those without (mean = 26.0 years), p = 0.028. Possible explanations for this difference include the need to work to be self-sufficient or to support family members, or an event/life experience that steered the student towards a career in pharmacy. The apparent detrimental effect on social/behavioral/administrative science grades of students having previous work experience is puzzling, (no work experience = 82.6% versus experience = 80.4%; p = 0.044). Possibly, practice skills learned in one work setting may not be valid in other settings because of differences in state laws, or previous experience may prejudice a student to a certain style of management or procedure. Alternatively, social/behavioral/administrative material may be thought of as different types of science than pharmacy coursework, covering a different body of knowledge and set of skills. The low impact of previous work experience on academic performance appears robust, as subanalyses of type of work setting, position held, and having more than 1 year of experience (greater than 2,000 hours), failed to reveal any significant differences.
Several study limitations should be considered when evaluating the results, including incomplete sampling, failure to survey the underlying reason for working, and the inability to quantify finer types of work experiences on academic and clinical performance using the survey. As mentioned previously, the majority of students who responded were in the didactic portion of the program, making it difficult to assess the full impact of previous pharmacy work experience on clinical clerkships. In addition, students' work experience was limited predominantly to community or retail experience. The study population was also restricted to 1 college's pharmacy program, and the unique curriculum format at TU-COP may make generalizing findings to other pharmacy schools' applicants difficult. Furthermore, the relatively small number of respondents without pharmacy work experience (< 10% of total sample) may have made detecting differences more difficult, although absolute differences among the examined dependent measures appeared small. Lastly, only a limited number of students (n=6) participated in the survey development focus group.
The survey instrument itself also may have limited the study, because it did not include items asking students' the reasons for pursuing pharmacy work experience; therefore, the complete impact of work experience on student performance may not have been assessed. Reasons for work experience may have provided insight into underlying motivations for choosing pharmacy as a career, and potentially point to future research. The survey also relied upon students self-reporting their work experience, and may have inadvertently introduced bias if those without work experience chose not to participate in the study. Furthermore, the high percentage of pharmacy students with prior work experience suggests that this characteristic may have been a factor in their acceptance into the program.
CONCLUSION
Prior pharmacy-related work experience had little impact on academic/clinical performance of the students in this study. While these results were unexpected, they provide insight into an area of pharmacy education research for which few studies exist, and set the stage for further studies to evaluate the effect of work experience on the academic and clinical performance of pharmacy students. Future studies may include determining the impact that intern hours during classroom years (early intern hours including IPPE hours) have on pharmacy school GPA, clinical clerkships, and NAPLEX passage rates, or assessing the value of intern hours on clinical success after graduation from pharmacy school. Moreover, this study suggests that factors impacting pharmacy student performance during the didactic and experiential portion of training are yet to be identified.
ACKNOWLEDGMENTS
The authors would like to acknowledge Mr. Richard Hornstein, curriculum support specialist for the Touro University – California College of Pharmacy, for invaluable assistance with Blackboard. The authors would also like to gratefully acknowledge Dr. Karl Meszaros, professor of biological sciences at Touro University – California College of Pharmacy, for several lively discussions regarding the TJE; and Dr. Gordon McCarter, Assistant Dean for Pharmacy Student Services at Touro University – California College of Pharmacy, for noteworthy assistance in interpretation of student academic measures.
REFERENCES
- 1. AACP-Annual Report. American Association of Colleges of Pharmacy. http://tinyurl.com/aacp2008. Accessed March 3, 2010.
- 2.Hardigan PC, Lai LL, Arneson D, Robeson A. Significance of academic merit, test scores, interviews and the admissions process: a case study. Am J Pharm Educ. 2001;65(1):40–44. [Google Scholar]
- 3.Kelley KA, Secnik K, Boye ME. An evaluation of the Pharmacy College Admissions Test as a tool for the pharmacy college admissions committees. Am J Pharm Educ. 2001;65(3):225–230. [Google Scholar]
- 4.McCall KL, Allen DD, Fike DS. Predictors of academic success in a doctor of pharmacy program. Am J Pharm Educ. 2006;70(5):106. doi: 10.5688/aj7005106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thomas MC, Draugalis JR. Utility of Pharmacy College Admission Test (PCAT): implications for admission committees. Am J Pharm Educ. 2002;66(1):47–51. [Google Scholar]
- 6.Chisholm MA, Cobb HH, Kotzan JA. Significant factors for predicting academic success of first-year pharmacy students. Am J Pharm Educ. 1995;59(4):364–70. [Google Scholar]
- 7.Chisholm MA, Cobb HH, Kotzan JA. Prior four year college degree and academic performance of first year pharmacy students: a three-year study. Am J Pharm Educ. 1997;61:278–281. [Google Scholar]
- 8.Chisholm MA, Cobb HH, DiPiro JT. Development and validation of a model that predicts the academic ranking of first-year pharmacy students. Am J Pharm Educ. 1999;63:388–94. [Google Scholar]
- 9.Allen DD, Bond CA. Prepharmacy predictors of success in pharmacy school: grade point averages, Pharmacy College Admissions Test, communication abilities, and critical thinking skills. Pharmacother. 2001;21(7):842–849. doi: 10.1592/phco.21.9.842.34566. [DOI] [PubMed] [Google Scholar]
- 10.Kidd RS, Latif DA. Traditional and novel predictors of classroom and clerkship success of pharmacy students. Am J Pharm Educ. 2003;67(4):109. [Google Scholar]
- 11.Hill LH, Delafuente JC, Sicat BL, Kirkwood CK. Development of a competency-based assessment process for advanced pharmacy practice experiences. Am J Pharm Educ. 2006;70(1) doi: 10.5688/aj700101. Article 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kassam R, Poole G, Collins JB. Development of an instrument to assess the impact of an enhanced experiential model on pharmacy students' learning opportunities, skills and attitudes: a retrospective comparative-experimentalist study. BMC Med Educ. April 8, 2008;8:17. doi: 10.1186/1472-6920-8-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Plaza CM. Progress examinations in pharmacy education. Am J Pharm Educ. 2007;71(4):66. doi: 10.5688/aj710466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meszaros K, Barnett MJ, McDonald M, Wehring H, Evans DJ, Sasaki-Hill D, Goldsmith PC, Knapp KK. Progress examination for assessing students' readiness for advanced pharmacy practice experiences. Am J Pharm Educ. 2009;73(6):109. doi: 10.5688/aj7306109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Latif DA. Including the assessment of nontraditional factors in pharmacy school admissions. Ann Pharmacother. 2005;39(4):721–726. doi: 10.1345/aph.1E498. [DOI] [PubMed] [Google Scholar]
- 16.DeYoung M, Sorofman BA. Working during the academic year: an examination of pharmacy students. Am J Pharm Educ. 1989;53:20–23. [Google Scholar]
- 17. Pharmacy Curriculum Outcomes Assessment. National Association of Boards of Pharmacy. http://www.nabp.net/pcoa/intro.asp. (PCOA Section) Accessed March 3, 2010.
- 18.McCall KL, MacLaughlin EJ, Fike DS, Ruiz B. Preadmission predictors of PharmD graduates' performance on the NAPLEX. Am J Pharm Educ. 2007;71(1) doi: 10.5688/aj710105. Article 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Houglum JE, Aparasu RR, Delfinis TM. Predictors of academic success and failure in a pharmacy professional program. Am J Pharm Educ. 2005;69(3) Article 43. [Google Scholar]