Abstract
Background
In some patients nonoperative treatment of a rotator cuff tear is sufficient, while in others it is only the first stage of treatment prior to surgery. Fatty infiltration progresses throughout the nonoperative treatment although it is not known at what point fatty infiltration contributes to poor functional outcomes, absence of healing, or increased rerupture rates.
Questions/purposes
We therefore identified factors related to the appearance of supraspinatus muscle fatty infiltration, determined the speed of appearance and progression of this phenomenon, and correlated fatty infiltration with muscular atrophy.
Methods
We retrospectively reviewed 1688 patients with rotator cuff tears and recorded the following: number of tendons torn, etiology of the tear, time between onset of shoulder symptoms and diagnosis of rotator cuff tear. Fatty infiltration of the supraspinatus was graded using either CT or MRI classification. Muscular atrophy was measured indirectly using the tangent sign.
Results
Moderate supraspinatus fatty infiltration appeared an average of 3 years after onset of symptoms and severe fatty infiltration at an average of 5 years after the onset of symptoms. A positive tangent sign appeared at an average of 4.5 years after the onset of symptoms.
Conclusions
Our results suggest that rotator cuff repair should be performed before the appearance of fatty infiltration (Stage 2) and atrophy (positive tangent sign)—especially when the tear involves multiple tendons.
Level of Evidence
Level IV, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Pathology of the rotator cuff influences both the tendon and corresponding muscle. More specifically, a full-thickness tear of a rotator cuff tendon can result in retraction of the muscle belly and its tendon. Retraction of the muscle belly may lead to a change in the pennation angle between the muscle fibers and the subsequent development of fatty infiltration [9]. Goutallier et al. [11] first reported a classification system to define the severity of fatty infiltration using CT images of the rotator cuff muscle. Subsequently, the amount of fatty infiltration has been considered an important prognostic factor for healing of a rotator cuff repair, as well as for functional outcome, as this chronic change may signal poor biologic capacity to heal the tendon as well as the muscle and may suggest tissue with poor mechanical properties that can be difficult to mobilize or hold suture [1, 8, 10, 13, 14, 18, 19]. Atrophy of the rotator cuff muscle is also an important factor for assessing the treatment of rotator cuff tears [1, 19, 20, 22, 26].
Despite the current literature describing the importance of fatty infiltration and atrophy, these concepts have not been specifically defined for the supraspinatus musculotendinous unit. In certain cases, nonoperative treatment of rotator cuff tears is sufficient, while in others, it is the first stage of treatment prior to surgery. However, the fatty infiltration progresses throughout the nonoperative treatment. Since the degree of fatty infiltration influences outcome, it is critical in individual patients to identify the degree that results in poor functional outcomes, poor healing, or increased rerupture rates.
The goals of our study were therefore to (1) identify factors related to the appearance of supraspinatus muscle fatty infiltration; (2) determine the speed of appearance and progression of this phenomenon; and (3) correlate fatty infiltration with muscular atrophy.
Patients and Methods
We retrospectively reviewed 2500 patients with rotator cuff tears who underwent open or arthroscopic tendon repair, arthroscopic débridement, or a reverse shoulder arthroplasty between 1988 and 2005. We excluded 812 patients with previous surgery on the affected shoulder or incomplete imaging studies. The average age of the remaining 1688 patients at the time of imaging was 57.2 years (range, 18–83 years). Men represented 60% of cases (1005/1688); 72% (1209/1688) involved the dominant side. Of the 1688 patients, 1377 (82%) had a preoperative CT arthrogram and 311 (18%) had a preoperative MRI. Demographic data were obtained for each patient in addition to the details regarding their rotator cuff tear (number of tendons torn, etiology of the tear, time between onset of shoulder symptoms, and diagnosis of rotator cuff tear).
We identified and characterized the rotator cuff tears based upon preoperative CT arthrogram or MRI, ranging from isolated single tendon tears to massive multiple tendon tears [21]. For the supraspinatus tendon we differentiated between partial thickness (articular side, intratendinous, superficial side) and full thickness tears; for the infraspinatus and the subscapularis tendon, we did not distinguish between partial and complete tears because the study focused on the supraspinatus. There were no teres minor tears in this series. Rotator cuff tears were identified on preoperative images and confirmed intraoperatively, but the observers were not blinded as they had evaluated the preoperative imaging and were present at the time of surgery. The rotator cuff tears involved the supraspinatus in 93% of cases (1573/1688), the subscapularis in 38% (633/1688), and the infraspinatus in 24% (411/1688) (Table 1). We did not quantify the size of the tears due to lack of consensus in the literature, no methods to measure tear size and the variability these measurements would introduce into the study.
Table 1.
Type of rotator cuff tears and epidemiology
| Variable | Partial thickness SS tears | Full thickness SS tears | Isolated SScap tears | SS + Sscap tears | SS + IS ± TM tears | SS + IS + Sscap tears | Total |
|---|---|---|---|---|---|---|---|
| n | 232 | 577 | 115 | 353 | 246 | 165 | 1688 |
| % | 13.7% | 34.2% | 6.8% | 20.9% | 14.6% | 9.7% | 100% |
| Age at imaging (years) | 51.7 | 56.8 | 52.1 | 58.5 | 59.9 | 63.1 | 57.2 |
| Male | 62.1% | 52.9% | 80.9% | 62% | 58.9% | 60% | 59.2% |
| Dominant side | 62.1% | 69% | 75.7% | 78.2% | 71.1% | 78.2% | 71.6% |
| Traumatic onset | 33.5% | 35.8% | 46% | 45.1% | 43.6% | 39% | 39.6% |
| Degenerative onset | 62.5% | 56.5% | 49.6% | 48.6% | 44% | 58.5% | 53.5% |
| Mixed onset | 4% | 7.7% | 4.4% | 6.3% | 12.4% | 2.5% | 6.9% |
SS = supraspinatus; Sscap = subscapularis; IS = infraspinatus; TM = teres minor.
The etiology of the rotator cuff tear was classified as traumatic (those patients who recalled a specific event), degenerative (those who did not recall a single incident), or mixed. The mixed type was defined as a patient with chronic shoulder symptoms who experienced an acute traumatic event that exacerbated the chronic symptoms and motivated the patient to seek formal treatment. The etiology of the rotator cuff tear was traumatic in 669 of the 1688 cases (40%), degenerative in 903 (54%), and mixed in 116 (7%).
One of us (BM) graded fatty infiltration of the supraspinatus using either the CT arthrogram (soft-tissue sequences) and the classification of Goutallier et al. [11] or MRI (T1 sequences) and the classification developed by Fuchs et al. [6]. Both classifications systems compare the ratio of fat to muscle on sagittal oblique images: stage 0–1 is considered normal and has no (0) to trace (1) amounts of fat investing the muscle bellies. Stages 2–4 are considered pathologic: more muscle than fat (2); equal muscle to fat (3); more fat than muscle (4). Lesage et al. reported a moderate interobserver agreement in the analysis of the supraspinatus fatty infiltration according to Goutallier classification on the CT scan [17]; Williams et al. reported a good intraobserver and a moderate interobserver agreement in the analysis of the supraspinatus fatty infiltration according to Goutallier classification on the CT scan [24]; Fuchs et al. reported a good interobserver reliability for grading fatty infiltration according to Goutallier classification for the CT-scan and for the MRI [6]. We did not compare or contrast CT scans with MRI; nevertheless, in our series the delay of appearance of different stages of fatty infiltration and the mean age of patients for each stage of fatty infiltration were similar in CT and MRI groups, and we think that the small series of MRI (only 18%) and the small differences in results have minimal influence on the data. Because the distribution of fatty infiltration through a muscle belly is variable and random, the final stage of supraspinatus fatty infiltration was determined by grading the muscle in an entire set of three imaging planes (coronal, axial, and sagittal) and not in one specific window (Figs. 1, 2). The average of these values was defined as the final stage of fatty infiltration for the supraspinatus muscle. Fatty infiltration of the infraspinatus and the subscapularis was graded using only axial images at the superior (tip of coracoid process) and inferior portion (lowest portion at the glenohumeral joint) of the glenoid as described by Goutallier [11]. The average of these two values defined the final stage of fatty infiltration for the infraspinatus and subscapularis muscles. For statistical evaluation we classified fatty infiltration as minimal for Goutallier stages 0 and 1, moderate for Goutallier Stage 2 and severe for Goutallier stages 3 and 4 [24].
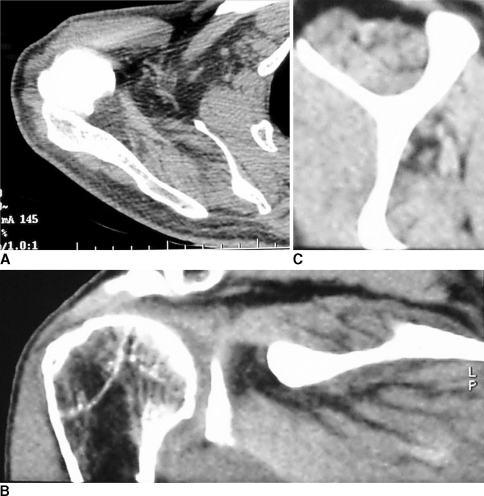
Fig. 1A–C.
Fatty infiltration of the supraspinatus was graded in soft-tissue sequences of the CT scan according to Goutallier classification [11]. The average of values determined in (A) axial, (B) coronal, and (C) sagittal plane was defined as the final stage of fatty infiltration.
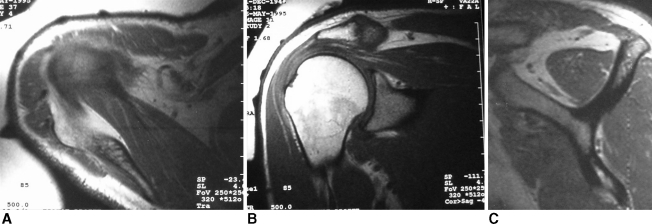
Fig. 2A–C.
Fatty infiltration of the supraspinatus was graded in T1 sequences according to Goutallier classification adapted by Fuchs to MRI [6]. The average of values determined in (A) axial, (B) coronal, and (C) sagittal plane was defined as the final stage of fatty infiltration.
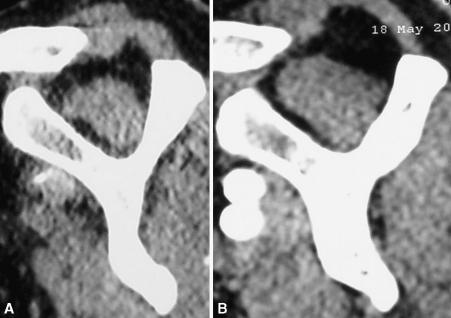
One of us (BM) also measured muscular atrophy indirectly using the tangent sign on the most lateral cut of the sagittal plane where the spine appears in contact with the scapula on the MRI/CT as described by Zanetti [26] (Fig. 3). A healthy supraspinatus should cross a line drawn for the superior border of the coracoid process to the superior border of the scapular spine; this line is called the “tangent.” Failure of the supraspinatus to cross the tangent is considered a “tangent sign” [26]. Only 584 had the appropriate “Y” cut on the most lateral sagittal plane where the spine appears in contact with the scapula (as described by Zanetti [26]) for the atrophy measurement.
Fig. 3A–B.
If the muscle belly of the supraspinatus fails to intersect a line drawn across the supraspinatus fossa, the tangent sign is Positive (A); if, however, the muscle does cross the line, it is a Negative tangent sign (B).
We used multiple regression analysis to determine the influence of several factors on the appearance of supraspinatus muscle fatty infiltration: increasing patient age, delay between onset of symptoms and diagnosis, etiology, and the number of involved tendons. The values of fatty infiltration were then analyzed two by two and multivariate logistic regression was used to determine the influence of the same factors on the speed of appearance and progression of this phenomenon. To evaluate the speed and progression at discrete time periods, the analysis of variance (ANOVA) with post hoc testing using the Bonferroni method was used or nonparametric test (Kruskal-Wallis, Wilcoxon) when the variance was not equal when analyzing trends with tear size. Fatty infiltration was analyzed by comparing muscle with minimal fatty infiltration to muscle with moderate and severe amount of fatty infiltration, respectively, with chi square of the maximum likelihood test for qualitative variables. Moderate and severe amounts of fatty muscle infiltration were also compared to each other. Finally, regression analysis was used to correlate fatty infiltration and atrophy.
Results
The appearance of fatty infiltration of the supraspinatus was related to increasing patient age, delay between onset of symptoms and diagnosis, and the number of involved tendons (p < 0.001 for all three variables). Variations were observed in the frequency and severity of supraspinatus fatty infiltration according to the number of tendons torn (Table 2); that is, fatty infiltration increases (p < 0.001) from minimal in partial ruptures of the supraspinatus to severe in massive rotator cuff tears involving the supraspinatus, infraspinatus, and subscapularis. We observed a relationship (p < 0.001) between increasing patient age and both the severity and frequency of supraspinatus fatty infiltration (Table 3). Age was a more likely predictor than time between onset of symptoms and diagnosis in terms of the development of fatty infiltration.
Table 2.
Supraspinatus fatty infiltration (FI) according to tendons tears (p < 0.0005)
| Supraspinatus fatty infiltration | Isolated Sscap tears n = 114 | Partial thickness SS tears n = 231 | Full thickness SS tears n = 571 | SS + Sscap tears n = 352 | SS + IS ± TM tears n = 244 | SS + IS + Sscap tears n = 165 | Total n = 1677 |
|---|---|---|---|---|---|---|---|
| Minimal | 108 (95%) | 215 (93%) | 417 (73%) | 223 (63%) | 101 (41%) | 47 (28%) | 1111 (66%) |
| Moderate | 5 (4%) | 16 (7%) | 142 (25%) | 121 (34%) | 99 (41%) | 85 (52%) | 468 (28%) |
| Severe | 1 (1%) | 0 (0%) | 12 (2%) | 8 (3%) | 44 (18%) | 33 (20%) | 98 (6%) |
SS = supraspinatus; Sscap = subscapularis; IS = infraspinatus; TM = teres minor.
Table 3.
Fatty infiltration (FI) stages according to age class (p < 0.0005)
| Supraspinatus fatty infiltration | Age | ||
|---|---|---|---|
| 50 years or younger | Between 50 and 60 years old | 60 years or older | |
| Minimal | 90% | 73% | 47% |
| Moderate | 9% | 24% | 41% |
| Severe | 1% | 3% | 12% |
Temporally, fatty infiltration and muscular atrophy correlated with the onset of rotator cuff symptoms and the delay of diagnosis in terms of presence and severity. Supraspinatus fatty infiltration increased (p < 0.001) as more time elapsed between the onset of symptoms and diagnosis of rotator cuff tear for both types of ruptures (traumatic and degenerative) (Table 4). On average, moderate (Stage 2) fatty infiltration appeared at a mean of 4 years (45.7 ± 61.8 months) after the onset of symptoms; severe fatty infiltration appeared at an average of 6 years (70.3 ± 74 months) after the onset of symptoms. In traumatic tears, where the delay can be precisely determined, moderate (Stage 2) fatty infiltration appeared at an average of 3 years (34.8 ± 55.7 months) and severe (stages 3 and 4) fatty infiltration at an average of 5 years (57.7 ± 66.7 months) after the onset of injury. Fatty infiltration appeared earlier and progressed faster in tear patterns involving more tendons (Table 5).
Table 4.
Delay between the symptoms onset and the imaging studies for the different fatty infiltration stages (variation observed according to the onset.)
| Supraspinatus fatty infiltration | Delay onset – imaging studies (months) | ||
|---|---|---|---|
| Total | Traumatic onset | Progressive onset | |
| Minimal | 23.6 ± 36.8 | 19.4 ± 37.3 | 29.5 ± 37.5 |
| Moderate | 45.7 ± 61.8 | 34.8 ± 55.7 | 54.1 ± 66.7 |
| Severe | 70.3 ± 74.2 | 57.7 ± 66.7 | 83.9 ± 80.2 |
Between minimal and moderate and between minimal and severe: P < 0.0005.
Between moderate and severe: P = 0.001 for total; P = 0.04 for traumatic onset; P = 0.003 for progressive onset.
Table 5.
Time elapsed (months) since the beginning of symptoms for the different type of tendinous rupture
| Supraspinatus fatty infiltration | SS tears | SS + IS ± TM tears | SS + IS + SScap tears | SS + SScap tears | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Full series | Traumatic onset | Progressive onset | Full series | Traumatic onset | Progressive onset | Full series | Traumatic onset | Progressive onset | Full series | Traumatic onset | Progressive onset | |
| Minimal | 24 | 17 | 31 | 16 | 14 | 24 | 23 | 13 | 34 | 26 | 26 | 27 |
| Moderate | 52 | 48 | 57 | 46 | 21 | 75 | 50 | 39 | 55 | 36 | 34 | 35 |
| Severe | 51 | 73 | 48 | 68 | 51 | 88 | 84 | 72 | 92 | 58 | 7 | 90 |
Between minimal and moderate and between minimal and severe: P < 0.0005.
Between moderate and severe: P = 0.001 for total; P = 0.04 for traumatic onset; P = 0.003 for progressive onset.
SS = supraspinatus; Sscap = subscapularis; IS = infraspinatus; TM = teres minor.
Muscle atrophy (positive tangent sign) was influenced by the degree of fatty infiltration, number of tendons involved, time after diagnosis, and age of the patient. The degree of fatty infiltration of the supraspinatus was described as minimal in 1111 of 1677 (66%), moderate in 68 (28% 4), and severe in 98 (6%). The tangent sign was positive in 14% (81/584) of the cases, and we observed a correlation between muscle atrophy (positive tangent sign) and the degree of supraspinatus fatty infiltration (p < 0.001). A positive tangent sign correlated with the degree of fatty infiltration of the supraspinatus (p < 0.001) and of the infraspinatus (p < 0.001) in the isolated supraspinatus tendon tears and in the tears involving both the supraspinatus and infraspinatus tendons: positive in 10% of isolated tears of the supraspinatus and in 28% of combined supraspinatus and infraspinatus. The prevalence of muscle atrophy increased with the number of torn tendons; in other words, we observed a positive tangent sign less frequently in partial tears of the supraspinatus and more commonly in massive rotator cuff tears involving supraspinatus, infraspinatus, and subscapularis (Table 6). We observed no correlation between muscular atrophy (positive tangent sign) and subscapularis fatty infiltration. For the entire series, the tangent sign was negative at an average of 2.5 years (30.2 ± 47.1 months) and positive at an average of 4.5 years (55 ± 63.5 months) after the onset of symptoms (p = 0.001). The average age of patients with a positive tangent sign, 62.8 years (range, 35–82 years), was higher (p < 0.001) than in patients with a negative tangent sign, 56.6 years (range, 18–82 years).
Table 6.
Relationship between tangent sign (TS) and tendon tears
| TS | Partial thickness SS tears | Isolated Sscap tears | Full thickness SS tears | SS + Sscap tears | SS + IS ± TM tears | SS + IS + Sscap tears | Total |
|---|---|---|---|---|---|---|---|
| Negative | 79 (97.5%) | 31 (96.9%) | 188 (90.4%) | 101 (88.6%) | 63 (72.4%) | 41 (66.1%) | 503 (86.1%) |
| Positive | 2 (2.5%) | 1 (3.1%) | 20 (9.6%) | 13 (11.4%) | 24 (27.6%) | 21 (33.9%) | 81 (13.9%) |
SS = supraspinatus; Sscap = subscapularis; IS = infraspinatus; TM = teres minor.
Discussion
Understanding the relationship of fatty infiltration and rotator cuff muscle atrophy and the clinical and temporal factors that influence this process may help physicians improve outcomes or provide patients with better prognostic information. The goals of our study were, therefore, to identify factors related to the appearance of supraspinatus muscle fatty infiltration, to determine the speed of appearance and progression of this phenomenon, and to correlate fatty infiltration with muscular atrophy.
We were first limited by a lack of a uniform imaging protocol for all tendon tears; however, we do not believe that this factor compromised our ability to analyze the fatty infiltration or muscle atrophy. Second, we did not measure rotator cuff tear size or tendon retraction as there is not a reliable rubric to this purpose. Our choice of symptoms onset corresponding with the onset of degenerative muscle change may limit the study because some tears are asymptomatic and the appearance of fatty infiltration may precede the symptom onset. However, as demonstrated by Yamaguchi et al., asymptomatic tears are usually small, becoming symptomatic as their size increases [25]. Third, we analyzed several tear patterns; application of the currently available systems oversimplifies the factors of tear morphology and retraction; their use in this study would not have generated meaningful data. The groups were too small and the data points insufficient to define the exact onset or describe a difference among the tear types (Table 6). Instead, the entire group of tears had to be analyzed together to report general conclusions. Retraction of the torn rotator cuff tendon may be a factor in the development of supraspinatus fatty infiltration [9].
Degenerative muscular changes associated with rotator cuff tears include fatty infiltration and atrophy [9, 11]. Both of these changes influence healing and clinical outcome of rotator cuff repairs [4, 7, 8, 10, 12, 14, 15, 19, 20, 22, 26]. Several studies have associated these changes with poor clinical outcome [2–4, 7, 8, 10–12, 15, 16, 19, 20, 23]. The natural history of fatty infiltration is described as irreversible and, usually, progressive [3, 8, 10, 14, 20]. Indeed, fatty infiltration graded as Stage 2 or higher is associated with a definitive loss of muscular function and, as a result, increases the rate of repair failure and limits the achievable outcome during the postoperative period [18, 22]. Although the changes may be irreversible, repair seems to halt atrophy because in patients with a retear there was more atrophy compared to patients with a healed supraspinatus repair [5, 8]. In general, most patients (66%) in this study had a minimal amount of supraspinatus fatty infiltration; the remaining patients had a moderate (28%) or a severe (6%) amount of fatty infiltration. Increasing patient age correlated with the presence and severity of supraspinatus fatty infiltration. Fatty infiltration increased with the severity of the rotator cuff tear (partial thickness tear to massive rotator cuff tear) (Table 1).
Recent reports have focused on defining the influence of fatty infiltration and atrophy on healing and postoperative outcome [10, 16, 18]. We did not evaluate postoperative integrity of repaired rotator cuffs or clinical outcome. Instead, the goal was to better define the relationship between the symptomatic time period before diagnosis of rotator cuff tear and the development of fatty infiltration and atrophy among various tear patterns. Overall, the onset of fatty infiltration is earlier, and its progression is faster in patients with more than one tear. The time between the onset of rotator cuff symptoms and diagnosis of rotator cuff tear plays a major role in the development of muscular changes. For traumatic tears, the time of onset of symptoms is easier to determine than in others types (degenerative or mixed). We observed that the fatty infiltration was minimal (stage 0 or 1) in small tears: if fatty infiltration is minimal in small symptomatic tears, we can presume that it is minimal or absent in asymptomatic small tears. Greater supraspinatus fatty infiltration was observed with longer delay between symptom onset and the diagnosis of rotator cuff tear on imaging studies. With all rotator cuff tear types in this study, moderate (Stage 2) fatty infiltration developed at an average of 4 years (45.7 months ± 61.8 months) after the onset of symptoms. Severe fatty infiltration appeared at an average of 6 years (70.3 months ± 74 months) after the onset of symptoms. Nevertheless for patients who experienced traumatic rotator cuff tears, moderate (Stage 2) fatty infiltration appeared at an average of 3 years (34.8 ± 55.7 months) after the initial incident/onset of symptoms. Severe fatty infiltration (stage 3 or 4) developed at an average of 5 years (57.7 ± 66.7 months) after the initial incident/onset of symptoms.
We used the tangent sign as an indirect measure of muscle atrophy, observing a positive tangent sign more frequently in cases where more rotator cuff tendons were torn. Atrophy in the supraspinatus was associated with a concomitant infraspinatus tear, but not a subscapularis tear. The development of a tangent sign also correlated with the time interval between onset of symptoms and diagnosis of rotator cuff tear. With all tear types under consideration in this study, a negative tangent sign occurred at a mean of 2.5 years (30.2 months ± 47.1 months) and a positive tangent sign at 4.5 years (55 months ± 63.5 months) after the onset of symptoms (Table 6). The data suggest the tangent sign is negative when there is minimal fatty infiltration. Our findings differ from those of Nakagaki et al. who reported no correlation between the period of preoperative symptoms and the degree of supraspinatus atrophy [20].
Overall, the findings in this study were consistent with previous studies that reported the importance of muscular atrophy in the evaluation of rotator cuff tears [6, 22]. The development of fatty infiltration and its severity increases with age. The progression of fatty infiltration is faster in rotator cuff tears that are traumatic and/or involve more than one tendon with moderate (Stage 2) fatty infiltration appearing at an average of 3 years after onset of symptoms. Based on the findings in this study, rotator cuff repair should be performed before the appearance of fatty infiltration (Stage 2) and atrophy (positive tangent sign) and as soon as possible in older patients when the tear involves multiple tendons. Understanding the influence of age and number of tendons torn as well as the time interval between the onset of rotator cuff symptoms and diagnosis of rotator cuff tear with fatty infiltration and atrophy should guide the length of nonoperative management, determine the urgency for surgical intervention, and define patient expectations. Future studies will help to confirm the findings of this study and their usefulness in clinical practice.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Department of Shoulder Surgery, Centre Orthopédique Santy, Lyon, France.
References
- 1.Bernageau J, Goutallier D, Postel JM. Density study of the muscles of the rotator cuff [in French]. In: Laredo JD, Bard H eds. Monographies du GETROA. Montpellier, France: Sauramps Medical; 1993:277–281.
- 2.Bigliani LU, Cordasco FA, McIlveen SJ, Musso ES. Operative treatment of failed repairs of the rotator cuff. J Bone Joint Surg Am. 1992;74:1505–1515. [PubMed] [Google Scholar]
- 3.Bjoerkenheim J. Structure and function of the rabbit’s supraspinatus muscle after resection of its tendon. Acta Orthop Scand. 1989;60:461–463. doi: 10.3109/17453678909149320. [DOI] [PubMed] [Google Scholar]
- 4.Franco MJ, Bershadsky B, Ciccone J, Yum JK, Iannotti JP. Functional outcome of arthroscopic rotator cuff repairs: a correlation of anatomic and clinical results. J Shoulder Elbow Surg. 2007;16:759–765. doi: 10.1016/j.jse.2007.03.020. [DOI] [PubMed] [Google Scholar]
- 5.Fuchs B, Gilbart M, Hodler J, Gerber CH. Clinical and structural results of open repair of an isolated one-tendon tear of the rotator cuff. J Bone Joint Surg Am. 2006;88:309–316. doi: 10.2106/JBJS.E.00117. [DOI] [PubMed] [Google Scholar]
- 6.Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: Assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. 1999;8:599–605. doi: 10.1016/S1058-2746(99)90097-6. [DOI] [PubMed] [Google Scholar]
- 7.Gazielly DF, Gleyze P, Montagnon C. Functional and anatomical results after rotator cuff repair. Clin Orthop Relat Res. 1994;304:43–53. [PubMed] [Google Scholar]
- 8.Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82:505–515. doi: 10.2106/00004623-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Ch Gerber, Meyer D, Frey E, Rechenberg B, Hoppeler H, Frigg R, Jost B, Zumstein M. Reversion of structural muscle changes caused by chronic rotator cuff tears using continous musculotendinous traction: An experimental study in sheep. J Shoulder Elbow Surg. 2009;18:163–171. doi: 10.1016/j.jse.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 10.Gladstone JN, Bishop JY, Lo IKY, Flatow EL. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med. 2007;35:719–728. doi: 10.1177/0363546506297539. [DOI] [PubMed] [Google Scholar]
- 11.Goutallier D, Bernageau J, Patte D. Assessment of the trophicity of the muscles of the ruptured rotator cuff by CT scan. In: Post M, Morrey BF, Hawkins RJ, eds. Surgery of the Shoulder. St. Louis, MO: Mosby; 1990:11–13.
- 12.Goutallier D, Le Guilloux P, Postel JM, Gleyze P. Fatty muscular degeneration [in French] Rev Chir Orthop Reparatrice Appar Mot. 1999;85(Supp II):132–136. [Google Scholar]
- 13.Goutallier D, Postel JM, Lavau L, Bernageau J. Influence of muscular degeneration of the supra and infraspinatus on the prognosis of surgical repair of the rotator cuff [in French] Acta Orthop Belg. 1998;64:41–45. [PubMed] [Google Scholar]
- 14.Goutallier D, Postel JM, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78–83. [PubMed] [Google Scholar]
- 15.Harryman DT, II, Mack LA, Wang KY, Jackins SE, Richardson ML, Masten FA. Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. J Bone Joint Surg Am. 1991;73:982–989. [PubMed] [Google Scholar]
- 16.Jost B, Zumstein M, Pfirrmann Ch, Gerber Ch. Long-term outcome after structural failure of rotator cuff repairs. J Bone Joint Surg Am. 2006;88:472–479. [DOI] [PubMed]
- 17.Lesage P, Maynou C, Elhage R, Boutry N, Herent S, Mestdagh H. Reproducibility of the tomographic evaluation of muscular fatty degeneration [in French] Rev Chir Orthop Reparatrice Appar Mot. 2002;88:359–364. [PubMed] [Google Scholar]
- 18.Liem D, Lichtenberg S, Magosch P, Habermeyer P. Magnetic resonance imaging of arthroscopic supraspinatus tendon repair. J Bone Joint Surg Am. 2007;89:1770–1776. doi: 10.2106/JBJS.F.00749. [DOI] [PubMed] [Google Scholar]
- 19.Mellado JM, Calmet J, Olona M, Esteve C, Camins A, Perez Del Palomar L, Gine J, Sauri A. Surgically repaired massive rotator cuff tears: MRI of tendon integrity, muscle fatty degeneration, and muscle atrophy correlated with intraoperative and clinical findings. Am J Roentgenol. 2005;184:1456–1463. doi: 10.2214/ajr.184.5.01841456. [DOI] [PubMed] [Google Scholar]
- 20.Nakagaki K, Ozaki J, Tomita Y, Tamai S. Alterations in the supraspinatus muscle belly with rotator cuff tearing: Evaluation with magnetic resonance imaging. J Shoulder Elbow Surg. 1994;3:88–93. doi: 10.1016/S1058-2746(09)80115-8. [DOI] [PubMed] [Google Scholar]
- 21.Patte D. Classification of rotator cuff lesions. Clin Orthop Relat Res. 1990;254:81–86. [PubMed] [Google Scholar]
- 22.Thomazeau H, Rolland Y, Lucas C, Duval JM, Langlais F. Atrophy of the supraspinatus belly: assessment by MRI in 55 patients with rotator cuff pathology. Acta Orthop Scand. 1996;67:264–268. doi: 10.3109/17453679608994685. [DOI] [PubMed] [Google Scholar]
- 23.Warner JJP, Higgins L, Parson IM, IV, Dowdy P. Diagnosis and treatment of anterosuperior rotator cuff tears. J Shoulder Elbow Surg. 2001;10:37–46. doi: 10.1067/mse.2001.112022. [DOI] [PubMed] [Google Scholar]
- 24.Williams MD, Lädermann A, Melis B, Barthelemy R, Walch G. Fatty infiltration of the supraspinatus: a reliability study. J Shoulder Elbow Surg. 2009;18:581–587. doi: 10.1016/j.jse.2008.12.014. [DOI] [PubMed] [Google Scholar]
- 25.Yamaguchi K, Ditsios K, Middleton WD, Hildebolt CF, Galatz LM, Teefey SA. The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic ansd symptomatic shoulders. J Bone Joint Surg Am. 2006;88:1699–1704. doi: 10.2106/JBJS.E.00835. [DOI] [PubMed] [Google Scholar]
- 26.Zanetti M, Gerber C, Hodler J. Quantitative assessment of the muscles of the rotator cuff with magnetic resonance imaging. Invest Radiol. 1998;33:163–170. doi: 10.1097/00004424-199803000-00006. [DOI] [PubMed] [Google Scholar]