Abstract
Background
Anecdotal evidence suggests an association between glenohumeral internal rotation deficits (GIRD) and scapular dysfunction, an observable alteration in the normal position or motion of the scapula in relation to the thoracic cage.
Questions/purposes
We therefore hypothesized players with GIRD (15° or greater) will have decreased dominant arm scapular upward rotation and increased scapular protraction compared with baseball players with GIRD (14° or less).
Methods
We studied 43 baseball players with no current shoulder or elbow symptoms; 22 had GIRD 15° or greater and 21 had GIRD 14° or less. We measured glenohumeral internal rotation supine with the scapula stabilized. Scapular upward rotation was tested at rest; 60°, 90°, and 120° abduction in the scapular plane; and scapular protraction at 0°, hands on hips, and 90° abduction in the scapular plane.
Results
The GIRD (15° or greater) group had less scapular upward rotation at 60° (3.58), 90° (5.01), and 120° (2.63) in the dominant arm. Scapular protraction at 90° (0.88 cm) also was greater in the dominant arm of the GIRD (15° or greater) group.
Conclusions
Baseball players with more GIRD have alterations to the position and motion of their scapula. A dual goal of minimizing GIRD and strengthening the scapular stabilizers may be warranted in this population.
Level of Evidence
Level II, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Healthy and injured throwers typically have decreased internal and concurrent increased external rotation in the dominant arm [2, 4, 9, 28, 31, 39]. External rotation gain and GIRD occur in healthy overhead-throwing athletes [2, 3, 8, 29], and some authors theorize the deficit places the shoulder at a higher likelihood of having an injury as a result of an altered distribution of stress [6, 22, 38, 39]. The direct cause of these alterations has yet to be determined. Some believe increases in external rotation occur over several years and are associated with the repetitive stretching of the anterior capsule [9, 10, 22, 27, 28]. Based on surgical observations, others have suggested the internal rotation deficits are a result of an acquired hypertrophied posterior capsule [5, 6, 31, 39]. It is thought that a thicker posterior capsule would have increased structural stiffness, thereby limiting internal rotation [5, 6, 31, 39]. Finally, others believe both are caused by an increase of humeral retroversion [8, 32, 33, 35].
Regardless of the direct cause of the internal and external rotation alterations, some studies suggest an association with injury to the rotator cuff and labrum [6, 16, 21, 31]. Abnormalities such as partial undersurface rotator cuff tears, internal impingement, and posterior SLAP lesions are common in these athletes. Some authors have described static (positional) and kinematic (motion pattern) abnormalities (scapular dyskinesis) of the scapula in relation to the thoracic cage [6, 19, 23, 30, 40]. These alterations, commonly identified in baseball throwers, include increased protraction, anterior tilting, and decreased upward rotation [6, 23, 30]. Although position and motion alterations seem prevalent in overhead-throwing athletes, the chronology and mechanism behind these changes remain somewhat controversial.
These changes in motion are believed to place the posterior rotator cuff and labrum at risk and be detrimental to normal function of the shoulder complex. With time, these scapular alterations may place increased stress on the static and dynamic restraints of the shoulder [6, 19, 23, 30, 40].
We therefore hypothesized (1) baseball players with GIRD (15° or greater) would have decreased scapular upward rotation on the dominant arm compared with those with absence of appreciable GIRD (14° or less); (2) baseball players with GIRD (15° or greater) would have no difference in scapular upward rotation on the nondominant arm compared with those with absence of appreciable GIRD (14° or less); (3) baseball players with GIRD (15° or greater) would have increased scapular protraction on the dominant arm compared with those with absence of appreciable GIRD (14° or less); and (4) baseball players with GIRD (15° or greater) would have no difference in scapular protraction on the dominant arm compared with those with absence of appreciable GIRD (14° or less).
Materials and Methods
We used a cross-sectional mixed-model design to assess one independent variable and four dependent variables. The independent variable was the presence of GIRD (15° or greater) or absence of appreciable GIRD (14° or less). These cutoffs were chosen based on humeral retroversion studies, which show an average increase of retroversion of 15° [32, 35]. The dependent variables were dominant and nondominant scapular upward rotation (measured at rest, 60°, 90°, and 120° glenohumeral abduction) and dominant and nondominant scapular protraction (measured at rest, with hands on hips, and 90° glenohumeral abduction). All measurements were taken preseason before any throwing.
From two separate teams we recruited 43 baseball players: 22 were in the GIRD (15° or greater) group (age, 18.86 ± 1.93 years; mass, 88.38 ± 9.88 kg; height, 183.92 ± 5.85 cm) and 21 were in the GIRD (14° or less) group (age, 18.33 ± 2.2 years; mass, 83.81 + 13.68 kg; height, 183.49 ± 7.78 cm). Participants were recruited from high school (19 players) and collegiate (23 players) levels and combined based on the level of GIRD (Table 1). We excluded patients with current shoulder or elbow symptoms. An a priori power analysis was calculated using G*Power v3.0.1 [11]. Parameters for power estimates are as follows: α = 0.05 and 1-β = 0.80; effect size (f) was determined by group means and SDs from preliminary data using a built-in algorithm in the software. Estimates of total sample size for scapular upward rotation and protraction were 50 and 55, respectively. The study was approved by a university Institutional Review Board. Informed consent was obtained from participants and/or the participants’ parents for those younger than 18 years; Health History Questionnaire and Health Insurance Portability and Accountability Act forms were completed before testing.
Table 1.
Group distribution for GIRD
| GIRD | Mean ± SD | 95% confidence interval | |
|---|---|---|---|
| Upper bound | Lower bound | ||
| 15° ≥ group | 20.19 ± 4.79 | 22.31 | 18.07 |
| 14° ≤ group | 8.89 ± 4.59 | 10.98 | 6.8 |
GIRD = glenohumeral internal rotation deficit.
Glenohumeral internal rotation was measured using a Saunders Digital Inclinometer (The Saunders Group Inc, Chaska, MN). A priori test-retest reliability of glenohumeral ROM was assessed by the primary investigator (SJT). Twenty healthy shoulders were measured and then remeasured 3 to 5 days later. The intraclass correlation coefficient (ICC; 2,1) and standard error of measurement values for glenohumeral ROM were 0.989 (1.03°) and 0.943 (2.55°) for internal and external rotation, respectively.
Scapular upward rotation was measured using a Saunders Digital Inclinometer (The Saunders Group Inc) modified to rest evenly on the scapular spine (Fig. 1) using methods described by Johnson et al. [17]. The digital inclinometer was modified by attaching two wooden locator arms that allowed secure and direct contact to the scapular spine. A priori test-retest reliability of the scapular upward rotation measurements were assessed by the primary investigator. We measured the shoulders of 18 healthy subjects (36 shoulders) and then remeasured them 3 to 5 days later. The ICC and standard error of measurement values for scapular upward rotation were 0.967 (0.70°), 0.946 (1.55°), 0.974 (0.86°), and 0.965 (0.89°) at rest and 60°, 90°, and 120° glenohumeral abduction, respectively.
Fig. 1.
Scapular upward rotation was measured using a modified digital inclinometer to rest evenly on the scapular spine as shown.
We measured scapular protraction using Kibler’s Lateral Scapular Slide Test [19] using a Vernier Caliper (Mitutoyo Model 505-633-50; Measurement Technology, Corby, Northants, UK) (Fig. 2) and recorded in centimeters. A priori test-retest reliability of the scapular protraction measurements was assessed by the primary investigator. Thirty-six healthy shoulders were measured and then remeasured 3 to 5 days later. The ICC and standard error of measurement values for scapular protraction were 0.935 (0.328 cm), 0.970 (0.186 cm), and 0.975 (0.231 cm) at rest, hands on hips, and 90° glenohumeral abduction, respectively.
Fig. 2.
Scapular protraction was measured as the distance from the inferior angle of the scapula to the corresponding spinous process using Vernier calipers.
Passive internal rotation measurements were taken with the subject in the supine position with the glenohumeral joint in 90° abduction. The scapula then was stabilized with the tester’s hand by placing a posterior directed force over the anterior acromion and the arm was rotated until scapular motion was detected [1]. The inclinometer then was placed on the dorsal surface of the forearm and the hold button was pressed to record the measurement. This was repeated three times and the average of the three measurements was taken. All measurement techniques were taken bilaterally by the primary investigator. The primary investigator was blinded to the arm dominance of the athlete and the order of testing was alternated. This technique was performed to place subjects in the appropriate GIRD 15° or greater or GIRD 14° or less groups.
Scapular upward rotation measurements were taken with the subject standing with a normal relaxed posture. A guide pole was used to help position the subject’s arm at 60°, 90°, and 120° abduction. When the appropriate amount of abduction was determined, a pin was inserted into the guide pole to help the subject maintain the proper amount of abduction. The subject was asked to abduct their arm until it was positioned against the pin. This position was maintained until the measurement was recorded. The lateral arm of the inclinometer then was placed over the posterior lateral acromion and the medial arm was placed over the root of the scapular spine. The hold button was pressed to record the measurement [17]. This was repeated twice and the average of the two measurements was taken. All measurement techniques were taken bilaterally by the primary investigator. The primary investigator was blinded to arm dominance of the athlete and the order of testing was alternated.
Scapular protraction measurements were taken with the subject standing with a normal relaxed posture. The measurements were performed at three different positions (rest, hands on hips, and 90° glenohumeral abduction with maximum internal rotation) as per the method described by Kibler [19]. The inferior angle of the scapula was palpated and the lateral arm of the calipers was placed at the tip of the inferior angle. The medial arm of the calipers then was positioned at the corresponding spinous process and the measurement was recorded. This was repeated three times and the average of the measurements was used for analysis.
Data analysis consisted of interferential and descriptive statistics. Statistics tests included separate two-way MANOVA for scapular upward rotation and protraction. The SPSS for Windows, Version 13.0, statistical program (SPSS, Inc, Chicago, IL) was used for data analysis.
Results
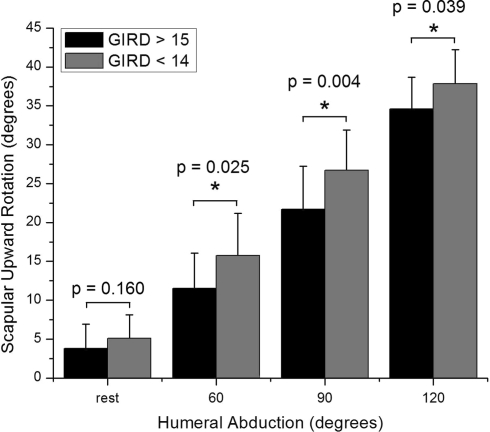
Dominant arm scapular upward rotation at 60°, 90°, and 120° were less for the GIRD (15° or greater) group than for the GIRD (14° or less) group (p = 0.025, p = 0.004, and p = 0.039, respectively) (Fig. 3; Table 2).
Fig. 3.
The bar graph shows dominant arm glenohumeral internal rotation deficits (GIRD) (15° or greater) group versus GIRD (14° or less) group scapular upward rotation means (degrees). GIRD (15° or greater) group had less scapular upward rotation at 60°, 90°, and 120° abduction compared with the GIRD (14° or less) group. The asterisk indicates a difference between the GIRD (15° or greater) group and GIRD (14° or less) group.
Table 2.
GIRD (15° or greater) versus GIRD (14° or less) scapular upward rotation†
| Scapular upward rotation | Position | GIRD ≥ 15° | GIRD ≤ 14° |
|---|---|---|---|
| Dominant arm | 0° | 3.81 ± 3.12 | 5.08 ± 3.03 |
| 60° | 11.44 ± 4.53 | 15.14 ± 5.89* | |
| 90° | 21.69 ± 5.53 | 26.79 ± 5.19* | |
| 120° | 34.43 ± 4.12 | 37.37 ± 4.4* | |
| Nondominant arm | 0° | 3.57 ± 2.22 | 4.05 ± 3.05 |
| 60° | 13.00 ± 5.1 | 14.24 ± 5.81 | |
| 90° | 25.52 ± 5.35 | 26.60 ± 5.67 | |
| 120° | 37.68 ± 4.65 | 37.76 ± 4.29 |
†Mean ± standard deviation; degrees; *significant difference between groups.
Nondominant arm scapular upward rotation was similar at all glenohumeral abduction positions between the GIRD (15° or greater) and the GIRD (14° or less) groups (Table 2).
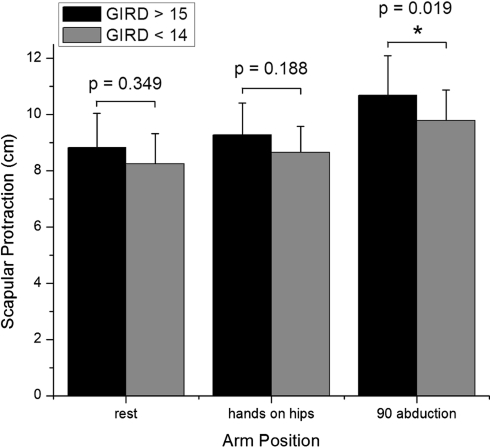
Dominant arm scapular protraction at 90° glenohumeral abduction was greater (p = 0.019) for the GIRD (15° or greater) group than the GIRD (14° or less) group (Fig. 4; Table 3).
Fig. 4.
The bar graph shows dominant arm glenohumeral internal rotation deficits (GIRD) (15° or greater) versus GIRD (14° or less) scapular protraction means (cm). The GIRD (15° or greater) group had more scapular protraction at 90° abduction compared with the GIRD (14° or less) group. The asterisk indicates a difference between the GIRD (15° or greater) group and GIRD (14° or less) group.
Table 3.
GIRD (15° or greater) versus GIRD (14° or less) scapular protraction†
| Kibler’s Lateral Scapular Slide | Position | GIRD ≥ 15° | GIRD ≤ 14° |
|---|---|---|---|
| Dominant arm | 0° | 9.12 ± 1.32 | 8.50 ± 1.55 |
| 45° | 9.41 ± 1.37 | 8.75 ± 1.43 | |
| 90° | 10.70 ± 1.32 | 9.82 ± 1.19* | |
| Nondominant arm | 0° | 8.45 ± 0.915 | 8.31 ± 1.19 |
| 45° | 8.39 ± 0.782 | 8.54 ± 1.08 | |
| 90° | 9.16 ± 1.01 | 9.23 ± 1.11 |
†Mean ± standard deviation; cm; *significance between groups.
Nondominant arm scapular protraction was similar at all glenohumeral abduction positions between the GIRD (15° or greater) group and the GIRD (14° or less) group (Table 3).
Discussion
Healthy and injured throwers typically have decreased internal (glenohumeral internal rotation deficits or GIRD) and concurrent increased external rotation in the dominant arm [2, 4, 9, 28, 31, 39]. Although the cause is unknown, some studies suggest an association of GIRD with injury to the rotator cuff and labrum [6, 16, 21, 31]. It also has been theorized but not confirmed that baseball players with substantial GIRD are more likely to have alterations in the position and motion of the scapula on the dominant arm and that these alterations also may place the posterior rotator cuff and labrum at risk of injury. We therefore hypothesized (1) baseball players with GIRD (15° or greater) would have decreased scapular upward rotation on the dominant arm compared with those with absence of appreciable GIRD (14° or less); (2) baseball players with GIRD (15° or greater) would have no difference in scapular upward rotation on the nondominant arm compared with those with absence of appreciable GIRD (14° or less); (3) baseball players with GIRD (15° or greater) would have increased scapular protraction on the dominant arm compared with those with absence of appreciable GIRD (14° or less); and (4) baseball players with GIRD (15° or greater) would have no difference in scapular protraction on the dominant arm compared with those with absence of appreciable GIRD (14° or less).
There are some limitations to this study that should be acknowledged. First, the power analysis suggested a total sample size of 50 to 55, however we were able to test only 43 subjects for the study. This may be a limitation owing to a slight lack of power; however the study was under-sampled by only seven subjects and we still observed statistically significant differences. Second, pitchers and position players were combined and analyzed together. Pitchers subject their shoulders to additional stress resulting from the high number of repetitions each game and may have more substantial GIRD and scapular alterations. However, pitchers and position players throw on a daily basis and have GIRD and scapular alterations develop. Third, we did not catalog throwing exposures. A basic assumption is that collegiate throwers have subjected their shoulders to more throwing exposures. However, we have no direct data to validate this. Fourth, we measured only two of the possible five degrees of freedom for the scapula. There are other possible alterations in scapular motions such as increased anterior tilting. However, to our knowledge, scapular upward rotation and protraction are the only valid and reliable measurements that can be observed clinically [3, 17, 19]. Although a three-dimensional electromagnetic tracking system can be used to measure all five degrees of scapular motion, this technique does not translate well to clinical practice and there are questions regarding its validity and reliability resulting from skin motion between the sensor and the scapula [26]. For the scapular protraction measurement, the distance from the inferior angle of the scapula to the spinous process is taken. One potential problem with this measurement is that if less scapular upward rotation is present, the inferior angle may be closer to the spinous process attributable solely to a change in upward rotation and not resulting from protraction. This would give a measurement of scapular protraction that is less compared with that of the nondominant arm. This is a limitation to the measurement and future methods should be developed to account for this error.
Our data showed dominant arm scapular upward rotation at 60°, 90°, and 120° glenohumeral abduction was less in the GIRD (15° or greater) group compared with the GIRD (14° or less) group. Previous research showed individuals with impingement syndrome have substantially more GIRD than healthy control subjects [31, 39]. Recently, Laudner et al. [23], although neglecting to measure GIRD, observed alterations in scapular motion in a population with impingement syndrome. The combined results of previous research are similar to results in the current study, which showed there is a decreased amount of scapular upward rotation in a group of baseball players with considerably more GIRD. Less active scapular upward rotation may cause a decrease in subacromial space during glenohumeral abduction, thereby placing the acromion closer to the leading edge of the rotator cuff. This may lead to subacromial impingement and potentially to rotator cuff injury [23–25, 30]. The observed decrease in upward rotation during active shoulder abduction is likely the result of inhibition of the dynamic scapular rotators [34]. The serratus anterior and lower trapezius are especially sensitive to shoulder kinematic perturbations and may be prone to inhibition [19, 34]. Burkhart et al. [6] believe inhibition of the serratus anterior and lower trapezius is chiefly the result of an increased amount of GIRD. The posterior capsule is connected to the humerus and scapula; a loss of internal rotation may force the scapula to get pulled around the thoracic wall, resulting in a more protracted scapula [6, 19]. In time, the static and dynamic restraints of the scapula may be affected with a loss of scapular control. One manifestation for the loss of scapular control is decreased upward rotation. Clinically, these results indicate baseball players with GIRD (15° or greater) have an associated decrease of dominant arm scapular upward rotation, which may be placing them at increased risk for shoulder injuries. This information is potentially valuable to clinicians for early identification of athletes at risk.
We found nondominant arm scapular upward rotation was similar between groups for any of the glenohumeral abduction positions. This is in agreement with clinical findings that suggest the dominant arm develops adaptations to the position and motion of the scapula but the nondominant does not owing to the lack of repetitive throwing stress [6, 19]. Burkhart et al. [6] suggested that clinically the nondominant arm should be used as a control when evaluating the dominant arm. They suggested the nondominant arm is not undergoing repetitive stress and therefore should not acquire adaptive changes. This adds further evidence that the adaptations between groups on the dominant arm are the result of repetitive throwing and not congenital differences.
Our data indicated baseball players with GIRD (15° or greater) had increased dominant arm protraction compared with baseball players with GIRD (14° or less). This excessive scapular protraction is commonly seen during glenohumeral abduction when the scapular stabilizers should be retracting [19, 23, 25, 30]. During the deceleration and/or follow-through phases of the overhead throw, the scapula must protract around the thoracic wall to help dissipate energy [19, 27]. Players with considerable GIRD may force their scapulae into increased protraction around the thoracic cage in an effort to gain humeral internal rotation during the follow-through phase. There are several reasons why excessive scapular protraction is viewed as a potentially harmful alteration [6, 19]. The continual stress on the scapular stabilizers may cause gradual weakness, especially of the serratus anterior muscle. Without a strong serratus anterior, the scapula will not provide a stable base of support for the rotator cuff to function. The scapula now becomes an unstable platform for the rotator cuff, which functions opposite the origin and insertion attachments. Rather than compressing the humeral head into the glenoid fossa, the scapula may be pulled in a lateral direction around the thoracic wall [19, 36]. Additionally, the protracted scapula can increase strain on the anterior capsule and, when combined with GIRD, potentiates the risk for shoulder instability [13, 16] and internal impingement [18, 20] to develop by narrowing the subacromial space and allowing increased translation of the humeral head in relation to the glenoid [14, 19, 24, 29, 31, 36, 37]. Clinically, these results indicate baseball players with GIRD (15° or greater) have an associated increase of dominant arm scapular protraction, which may increase their risk of shoulder injuries.
We observed similar nondominant arm scapula protraction between groups for any of the glenohumeral abduction positions. This is similar to the nondominant arm results for scapular upward rotation. The nondominant arm is not being subjected to the repetitive stress of overhead throwing and therefore does not develop adaptations of the scapula. These results give value to the clinical use of having the nondominant arm serve as the control when evaluating the scapula.
As a result of the association of GIRD and scapular alterations in baseball players, it is paramount to further discuss the potential mechanism by which GIRD develops. During the deceleration phase of the overhead throw, the posterior capsule and posterior rotator cuff decelerate the large internal rotational torques realized at the humerus. The repetitive nature of throwing may cause fatigue of the posterior rotator cuff muscles, which may place more stress on the posterior capsule to maintain joint stability and affect humeral deceleration necessary to complete the follow-through. It is believed that with time, this increased distractive stress will cause repetitive microtrauma to the posterior capsule and a fibroblastic healing response resulting in hypertrophy [6]. This tight and hypertrophied posterior capsule causes a shift in the arthrokinematics of the glenohumeral joint in a posterior-superior direction, thereby placing the shoulder at a higher risk for SLAP lesions and rotator cuff tears [7, 12, 15]. In essence, GIRD may be the physical manifestation of the adaptive thickening response of the posterior capsule [6].
Baseball players with GIRD (15° or greater) have considerably less scapular upward rotation and considerably more scapular protraction compared with baseball players with GIRD (14° or less). Our findings suggest baseball players with considerable GIRD also have major alterations to scapular position and motion similar to those seen in an injured population [6, 19]. Diminished scapular upward rotation and increased protraction may decrease rotator cuff efficiency, increase stress on the static restraints of the glenohumeral joint, and facilitate internal and external impingement. The development of scapular dyskinesis appears concomitant with the level of GIRD present. Early efforts to minimize internal rotation deficits and strengthen the scapular stabilizers in youth baseball players may prevent the development of glenohumeral and scapular adaptations. This may help decrease the likelihood of injury, including those to the rotator cuff and labrum.
Acknowledgments
We thank Fran Murphy and Susan Mills, Archbishop Carroll High School (subject recruitment), and James Sherman, University of Delaware (subject recruitment).
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Archbishop Carroll High School and University of Delaware.
References
- 1.Awan R, Smith J, Boon AJ. Measuring shoulder internal rotation range of motion: a comparison of 3 techniques. Arch Phys Med Rehabil. 2002;83:1229–1234. doi: 10.1053/apmr.2002.34815. [DOI] [PubMed] [Google Scholar]
- 2.Bigliani LU, Codd TP, Connor PM, Levine WN, Littlefield MA, Hershon SJ. Shoulder motion and laxity in the professional baseball player. Am J Sports Med. 1997;25:609–613. doi: 10.1177/036354659702500504. [DOI] [PubMed] [Google Scholar]
- 3.Borsa PA, Timmons MK, Sauers EL. Scapular-positioning patterns during humeral elevation in unimpaired shoulders. J Athl Train. 2003;38:12–17. [PMC free article] [PubMed] [Google Scholar]
- 4.Brown LP, Niehues SL, Harrah A, Yavorsky P, Hirshman HP. Upper extremity range of motion and isokinetic strength of the internal and external shoulder rotators in major league baseball players. Am J Sports Med. 1988;16:577–585. doi: 10.1177/036354658801600604. [DOI] [PubMed] [Google Scholar]
- 5.Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology Part I: pathoanatomy and biomechanics. Arthroscopy. 2003;19:404–420. doi: 10.1053/jars.2003.50128. [DOI] [PubMed] [Google Scholar]
- 6.Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology Part III: the SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy. 2003;19:641–661. doi: 10.1016/S0749-8063(03)00389-X. [DOI] [PubMed] [Google Scholar]
- 7.Clabbers KM, Kelly JD, Bader D, Eager M, Imhauser C, Siegler S, Moyer RA. Effect of posterior capsule tightness on glenohumeral translation in the late-cocking phase of pitching. J Sport Rehabil. 2007;16:41–49. doi: 10.1123/jsr.16.1.41. [DOI] [PubMed] [Google Scholar]
- 8.Crockett HC, Gross LB, Wilk KE, Schwartz ML, Reed J, O’Mara J, Reilly MT, Dugas JR, Meister K, Lyman S, Andrews JR. Osseous adaptation and range of motion at the glenohumeral joint in professional baseball pitchers. Am J Sports Med. 2002;30:20–26. doi: 10.1177/03635465020300011701. [DOI] [PubMed] [Google Scholar]
- 9.Ellenbecker TS, Roetert EP, Bailie DS, Davies GJ, Brown SW. Glenohumeral joint total rotation range of motion in elite tennis players and baseball pitchers. Med Sci Sports Exerc. 2002;34:2052–2056. doi: 10.1097/00005768-200212000-00028. [DOI] [PubMed] [Google Scholar]
- 10.Ellenbecker TS, Roetert EP, Piorkowski PA, Schulz DA. Glenohumeral joint internal and external rotation range of motion in elite junior tennis players. J Orthop Sports Phys Ther. 1996;24:336–341. doi: 10.2519/jospt.1996.24.6.336. [DOI] [PubMed] [Google Scholar]
- 11.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191. doi: 10.3758/BF03193146. [DOI] [PubMed] [Google Scholar]
- 12.Grossman MG, Tibone JE, McGarry MH, Schneider DJ, Veneziani S, Lee TQ. A cadaveric model of the throwing shoulder: a possible etiology of superior labrum anterior-to-posterior lesions. J Bone Joint Surg Am. 2005;87:824–831. doi: 10.2106/JBJS.D.01972. [DOI] [PubMed] [Google Scholar]
- 13.Harryman DT, 2nd, Sidles JA, Clark JM, McQuade KJ, Gibb TD, Matsen FA., III Translation of the humeral head on the glenoid with passive glenohumeral motion. J Bone Joint Surg Am. 1990;72:1334–1343. [PubMed] [Google Scholar]
- 14.Hébert LJ, Moffet H, McFadyen BJ, Dionne CE. Scapular behavior in shoulder impingement syndrome. Arch Phys Med Rehabil. 2002;83:60–69. doi: 10.1053/apmr.2002.27471. [DOI] [PubMed] [Google Scholar]
- 15.Huffman GR, Tibone JE, McGarry MH, Phipps BM, Lee YS, Lee TQ. Path of glenohumeral articulation throughout the rotational range of motion in a thrower’s shoulder model. Am J Sports Med. 2006;34:1662–1669. doi: 10.1177/0363546506287740. [DOI] [PubMed] [Google Scholar]
- 16.Jobe FW, Kvitne RS, Giangarra CE. Shoulder pain in the overhand or throwing athlete: the relationship of anterior instability and rotator cuff impingement. Orthop Rev. 1989;18:963–975. [PubMed] [Google Scholar]
- 17.Johnson MP, McClure PW, Karduna AR. New method to assess scapular upward rotation in subjects with shoulder pathology. J Orthop Sports Phys Ther. 2001;31:81–89. doi: 10.2519/jospt.2001.31.2.81. [DOI] [PubMed] [Google Scholar]
- 18.Kaplan LD, McMahon PJ, Towers J, Irrgang JJ, Rodosky MW. Internal impingement: findings on magnetic resonance imaging and arthroscopic evaluation. Arthroscopy. 2004;20:701–704. doi: 10.1016/j.arthro.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 19.Kibler WB. The role of the scapula in athletic shoulder function. Am J Sports Med. 1998;26:325–337. doi: 10.1177/03635465980260022801. [DOI] [PubMed] [Google Scholar]
- 20.Kibler WB. Scapular involvement in impingement: signs and symptoms. Instr Course Lect. 2006;55:35–43. [PubMed] [Google Scholar]
- 21.Kibler WB, Chandler TJ. Range of motion in junior tennis players participating in an injury risk modification program. J Sci Med Sport. 2003;6:51–62. doi: 10.1016/S1440-2440(03)80008-7. [DOI] [PubMed] [Google Scholar]
- 22.Kibler WB, Chandler JT, Livingston BP, Roetert EP. Shoulder range of motion in elite tennis players: effect of age and years of tournament play. Am J Sports Med. 1996;24:279–285. doi: 10.1177/036354659602400306. [DOI] [PubMed] [Google Scholar]
- 23.Laudner KG, Myers JB, Pasquale MR, Bradley JP, Lephart SM. Scapular dysfunction in throwers with pathologic internal impingement. J Orthop Sports Phys Ther. 2006;36:485–494. doi: 10.2519/jospt.2006.2146. [DOI] [PubMed] [Google Scholar]
- 24.Lukasiewicz AC, McClure P, Michener L, Pratt N, Sennett B. Comparison of 3-dimensional scapular position and orientation between subjects with and without shoulder impingement. J Orthop Sports Phys Ther. 1999;29:574–583; discussion 584–586. [DOI] [PubMed]
- 25.McClure PW, Michener LA, Karduna AR. Shoulder function and 3-dimensional scapular kinematics in people with and without shoulder impingement syndrome. Phys Ther. 2006;86:1075–1090. [PubMed] [Google Scholar]
- 26.McClure PW, Michener LA, Sennett BJ, Karduna AR. Direct 3-dimensional measurement of scapular kinematics during dynamic movements in vivo. J Shoulder Elbow Surg. 2001;10:269–277. doi: 10.1067/mse.2001.112954. [DOI] [PubMed] [Google Scholar]
- 27.Meister K. Injuries to the shoulder in the throwing athlete. Part one: biomechanics/pathophysiology/classification of injury. Am J Sports Med. 2000;28:265–275. doi: 10.1177/03635465000280022301. [DOI] [PubMed] [Google Scholar]
- 28.Meister K, Day T, Horodyski M, Kaminski TW, Wasik MP, Tillman S. Rotational motion changes in the glenohumeral joint of the adolescent/Little League baseball player. Am J Sports Med. 2005;33:693–698. doi: 10.1177/0363546504269936. [DOI] [PubMed] [Google Scholar]
- 29.Michener LA, McClure PW, Karduna AR. Anatomical and biomechanical mechanisms of subacromial impingement syndrome. Clin Biomech (Bristol, Avon) 2003;18:369–379. doi: 10.1016/S0268-0033(03)00047-0. [DOI] [PubMed] [Google Scholar]
- 30.Myers JB, Laudner KG, Pasquale MR, Bradley JP, Lephart SM. Scapular position and orientation in throwing athletes. Am J Sports Med. 2005;33:263–271. doi: 10.1177/0363546504268138. [DOI] [PubMed] [Google Scholar]
- 31.Myers JB, Laudner KG, Pasquale MR, Bradley JP, Lephart SM. Glenohumeral range of motion deficits and posterior shoulder tightness in throwers with pathologic internal impingement. Am J Sports Med. 2006;34:385–391. doi: 10.1177/0363546505281804. [DOI] [PubMed] [Google Scholar]
- 32.Osbahr DC, Cannon DL, Speer KP. Retroversion of the humerus in the throwing shoulder of college baseball pitchers. Am J Sports Med. 2002;30:347–353. doi: 10.1177/03635465020300030801. [DOI] [PubMed] [Google Scholar]
- 33.Pieper HG. Humeral torsion in the throwing arm of handball players. Am J Sports Med. 1998;26:247–253. doi: 10.1177/03635465980260021501. [DOI] [PubMed] [Google Scholar]
- 34.Pink M. Understanding the linkage system of the upper extremity. Sports Med Arthrosc Rev. 2001;9:52–60. doi: 10.1097/00132585-200101000-00006. [DOI] [Google Scholar]
- 35.Reagan KM, Meister K, Horodyski MB, Werner DW, Carruthers C, Wilk K. Humeral retroversion and its relationship to glenohumeral rotation in the shoulder of college baseball players. Am J Sports Med. 2002;30:354–360. doi: 10.1177/03635465020300030901. [DOI] [PubMed] [Google Scholar]
- 36.Smith J, Dietrich CT, Kotajarvi BR, Kaufman KR. The effect of scapular protraction on isometric shoulder rotation strength in normal subjects. J Shoulder Elbow Surg. 2006;15:339–343. doi: 10.1016/j.jse.2005.08.023. [DOI] [PubMed] [Google Scholar]
- 37.Smith J, Kotajarvi BR, Padgett DJ, Eischen JJ. Effect of scapular protraction and retraction on isometric shoulder elevation strength. Arch Phys Med Rehabil. 2002;83:367–370. doi: 10.1053/apmr.2002.29666. [DOI] [PubMed] [Google Scholar]
- 38.Thomas SJ, Swanik KA, Swanik C, Huxel KC. Glenohumeral rotation and scapular position adaptations after a single high school female sports season. J Athl Train. 2009;44:230–237. doi: 10.4085/1062-6050-44.3.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tyler TF, Nicholas SJ, Roy T, Gleim GW. Quantification of posterior capsule tightness and motion loss in patients with shoulder impingement. Am J Sports Med. 2000;28:668–673. doi: 10.1177/03635465000280050801. [DOI] [PubMed] [Google Scholar]
- 40.Warner JJ, Micheli LJ, Arslanian LE, Kennedy J, Kennedy R. Scapulothoracic motion in normal shoulders and shoulders with glenohumeral instability and impingement syndrome: a study using Moire topographic analysis. Clin Orthop Relat Res. 1992;285:191–199. [PubMed] [Google Scholar]