The description of coronal alignment in the perioperative assessment of knee disorders is important for accurately reporting diagnoses and outcomes. Most orthopaedic subspecialties—pediatrics, osteotomy/deformity correction, sports medicine, and tumor reconstruction—rely on coronal alignment to ensure satisfactory, reproducible, and reliable outcomes. After TKA, proper coronal alignment is important, as malalignment may lead to component failure [2, 5, 9, 12, 16]. All areas of lower extremity surgery thus use some form of alignment descriptors and measurement tools.
Despite the importance of alignment, the manner in which lower extremity coronal alignment in knee radiographs is presented is highly variable and often confusing. The terms varus and valgus are used frequently, but they are imprecise. For example, when authors state that a total knee component is positioned in 3° varus (eg, Hsu et al. [7]), the reader wonders whether this means 3° more than the normal limits of varus (ie, 6° of total varus), or, alternatively, whether it is 4° of absolute varus. Such ambiguity is not particular to knee arthroplasty [1, 17].
The terms ‘varus’ (from the Latin for ‘crooked’) and ‘valgus’ (Latin for twisted or bent) historically have had confusing and etymologic conflicting meanings [6]. (The use of varus and valgus to confer ‘bowlegged’ and ‘knock-kneed’ limb deformities, respectively, is the opposite of meanings in antiquity.) With these discrepancies in terminology, we must ask if all authors use the same 5° variation from the 180° femorotibial alignment to describe ‘normal’ alignment, namely 175°. Although our intent is not to replace the commonly used terms varus and valgus, we believe it is important to state the alignment precisely in terms of absolute degrees.
Based on the perceived inadequacies with the current language of knee angle descriptors, we asked if disparities in reporting existed; and, if a more uniform reporting system and change of language could be considered to improve the consistency and clarity of reporting lower extremity angular alignment. We suggest that measuring number of degrees (in an 180°-system) from the center of the femoral shaft would be accurate and lead to more consistent reporting.
To examine potential variability in the literature, we reviewed all articles published in Clinical Orthopaedics and Related Research, The Journal of Arthroplasty, and The Journal of Bone and Joint Surgery (American edition) from January 2008 to December 2009. Ninety-six papers were selected based on their inclusion of a coronal plane radiographic measurement tool and results directly made from this system.
Ninety percent of the papers (90 articles) used a variation on the varus/valgus system without a strict definition (eg, Meneghini et al. [13]) often using terms like “X degrees from/of varus” or “Y degrees from/of valgus.” Only 2% of papers involved a 180°-degree coronal system [3, 14] to describe the coronal angular alignment in the lower extremity. In addition, there was marked variation in language used to describe other angular measurements (eg, hip-knee-ankle, component angles), and reference points (eg, differing points at either the distal femoral surface or proximal tibial surface for the “center” of the knee). Four percent of papers were classified as using either a combination of systems or a distinct system [4, 11]. Moreover, there was no consistent notation whether radiographs were taken with weightbearing.
Clearly, no standard system exists for reporting lower extremity coronal alignment, and this proves problematic when interpreting radiographic outcomes. This is compounded by the variation in imaging modalities, language, and reference points (eg, native landmarks versus angles measured in relation to implanted components). Although originally devised for plain radiographs, coronal alignment descriptors now must be applied to three-dimensional imaging modalities, such as MRI and CT. The advent of computer-assisted surgery further challenges our varying systems, as new software may present data according to internal or intraoperative reference points, rather than pure 180°-coronal alignment.
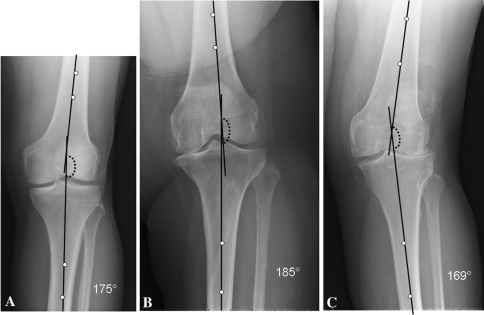
The use of a 180°-system is familiar to all orthopaedic surgeons. It is the standard nomenclature for defining fractures, upper extremity malalignment, deformity correction [10], and neck-shaft angles. It is precise and familiar. The center of the femur is defined by a line connecting two points each equidistant from the medial and lateral cortices along the femoral diaphysis on an AP radiograph. Likewise, the center of the tibia is similarly defined by a line connecting two diaphyseal points. If we start with the line formed along the center of the femur as the reference, all angles (0° to 360°, moving in clockwise fashion) can be determined (Fig. 1). For example, the anatomic lower extremity axis (using the central axes of the femur and tibia as defined above) may average 175°, and the mechanical axis (described in relation to a plumb line from the center of the femoral head) may average −5° (or 355°). Depending on the particular study, the anatomic axis may be the preferred angular system about the knee, although the mechanical axis may be used for describing entire-limb measurements.
Fig. 1A–C.
Standing AP knee radiographs show (A) normal, (B) varus, and (C) valgus femorotibial alignment as defined by a standardized 360° classification system.
Although an 180°-system may be imperfect (eg, limited by properly identifying the central axes of the femur and tibia) and must be defined carefully, the current use of varus/valgus is imprecise. Distinctions also could be made between other angular descriptors, such as mechanical, tibiofemoral alignment, and hip-knee-ankle limb alignments. Variation exists in the choice of the central axis of the knee [15] for mechanical axis measurements, and inaccuracies exist in identifying the true center of the intramedullary canal in anatomic axis measurements [8, 15]. However, these variables will exist in any measuring system and possibly may be reduced by recording true angular measurements.
Coronal alignment remains critical to long-term functional and clinical outcomes. Therefore, we need a more uniform and precise system of measurement and description. A useful, clear system would be based on a 180° radiographic model, in which magnitude of varus/valgus alignment is presented as a deviation (+/− X degrees) from a 180°-normal. Without a standardized system of coronal plane measurement, the literature is plagued by ambiguity and difficulties with data interpretation.
Footnotes
One the authors (PAL) receives royalties from Innomed and Lippincott Publishers, is a paid consultant to DePuy, Bayer, and Stryker, and is on the speakers’ bureau for DePuy and Bayer. One the authors (CLI) is a paid consultant and participant of the speakers’ bureau for Zimmer, Inc.
This study was performed at the University of Pennsylvania.
References
- 1.Billings A, Scott DF, Camargo MP, Hofmann AA. High tibial osteotomy with a calibrated osteotomy guide, rigid internal fixation, and early motion: long-term follow-up. J Bone Joint Surg Am. 2000;82:70–79. doi: 10.2106/00004623-200001000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Cameron HU, Hunter GA. Failure in total knee arthroplasty: mechanisms, revisions, and results. Clin Orthop Relat Res. 1982;170:141–146. [PubMed] [Google Scholar]
- 3.Chouteau J, Lerat JL, Testa R, Moyen B, Scott BA. Sagittal laxity after posterior cruciate ligament-retaining mobile-bearing total knee arthroplasty. J Arthroplasty. 2009;24:710–715. doi: 10.1016/j.arth.2008.05.028. [DOI] [PubMed] [Google Scholar]
- 4.Dewan A, Bertolusso R, Karastinos A, Conditt M, Noble PC, Parsley BS. Implant durability and knee function after total knee arthroplasty in the morbidly obese patient. J Arthroplasty. 2009;24(6 suppl):89–94. doi: 10.1016/j.arth.2009.04.024. [DOI] [PubMed] [Google Scholar]
- 5.Dorr LD, Boiardo RA. Technical considerations in total knee arthroplasty. Clin Orthop Relat Res. 1986;205:5–11. [PubMed] [Google Scholar]
- 6.Houston CS, Swischuk LE. Occasional notes. Varus and valgus: no wonder they are confused. New Engl J Med. 1980;302:471–472. doi: 10.1056/NEJM198002213020822. [DOI] [PubMed] [Google Scholar]
- 7.Hsu RW, Fan GF, Ho WP. A follow-up study of porous-coated anatomic knee arthroplasty. J Arthroplasty. 1995;10:29–36. doi: 10.1016/s0883-5403(05)80097-x. [DOI] [PubMed] [Google Scholar]
- 8.Ishii Y, Ohmori G, Bechtold JE, Gustilo RB. Extramedullary versus intramedullary alignment guides in total knee arthroplasty. Clin Orthop Relat Res. 1995;318:167–175. [PubMed] [Google Scholar]
- 9.Kagen A., 2nd Mechanical causes of loosening in knee joint replacements. J Biomech. 1977;10:387–391. doi: 10.1016/0021-9290(77)90014-8. [DOI] [PubMed] [Google Scholar]
- 10.Koshino T, Murase T, Saito T. Medial opening-wedge high tibial osteotomy with use of porous hydroxyapatite to treat medial compartment osteoarthritis of the knee. J Bone Joint Surg Am. 2003;85:78–85. doi: 10.1302/0301-620X.85B1.12468. [DOI] [PubMed] [Google Scholar]
- 11.Lionberger DR, Weise J, Ho DM, Haddad JL. How does electromagnetic navigation stack up against infrared navigation in minimally invasive total knee arthroplasties? J Arthroplasty. 2008;23:573–580. doi: 10.1016/j.arth.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 12.Lotke PA, Ecker ML. Influence of positioning of prosthesis in total knee replacement. J Bone Joint Surg Am. 1977;59:77–79. [PubMed] [Google Scholar]
- 13.Meneghini RM, Lewallen DG, Hanssen AD. Use of porous tantalum metaphyseal cones for severe tibial bone loss during revision total knee replacement. J Bone Joint Surg Am. 2008;90:78–84. doi: 10.2106/JBJS.F.01495. [DOI] [PubMed] [Google Scholar]
- 14.Mizu-Uchi H, Matsuda S, Miura H, Higaki H, Okazaki K, Iwamoto Y. Three-dimensional analysis of computed tomography-based navigation system for total knee arthroplasty: the accuracy of computed tomography-based navigation system. J Arthroplasty. 2009;24:1103–1110. doi: 10.1016/j.arth.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 15.Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. 1987;69:745–749. [PubMed] [Google Scholar]
- 16.Tew M, Waugh W. Tibiofemoral alignment and the results of knee replacement. J Bone Joint Surg Br. 1985;67:551–556. doi: 10.1302/0301-620X.67B4.4030849. [DOI] [PubMed] [Google Scholar]
- 17.Zagorski JB, Latta LL, Zych GA, Finnieston AR. Diaphyseal fractures of the humerus: treatment with prefabricated braces. J Bone Joint Surg Am. 1988;70:607–610. [PubMed] [Google Scholar]