Abstract
Reports using the Constant-Murley score often lack details regarding how strength measurement was performed, which may have an important impact on the results obtained. A description of the measurement is especially important when patients are unable to adopt the prescribed position of 90° shoulder abduction, leading to invalid or highly discrepant scores. We investigated the influence of shoulder abduction and torso position on strength measurement with special emphasis on intraobserver reliability. Thirty-three healthy volunteers were examined using a handheld dynamometer (Isobex®) in 30°, 60°, and 90° abduction with or without stabilization of the torso. A linear correlation between strength measurements in different degrees of abduction was observed, with values at 90° abduction on average 15% lower than at 60° and 45% lower than at 30°. In multivariate analysis, gender and weight had a substantial impact on the strength of individual measurement positions. Intraobserver reliability was related to arm and torso position (intraclass correlation coefficients, 0.71–0.93) and was highest for 90° abduction without torso stabilization. These findings emphasize the importance of standardized torso and arm positions ensuring high reliability when performing the strength measurement of the Constant-Murley score.
Introduction
The Constant-Murley score (CMS) was introduced [6, 10] to determine functional outcome after treatment of shoulder injury. This score, used worldwide, is divided into four subscales, including pain (15 points maximum), activities of daily living (20 points maximum), range of motion (40 points maximum), and strength (25 points maximum). The higher the score, the higher is the quality of function (minimum 0, maximum 100). Various studies have affirmed good reproducibility, responsiveness, and construct validity [1–3, 5, 8, 9, 17, 25, 30, 31] of the score, but they did not assess content validity and internal consistency. Rocourt et al. [28] reported how internationally used Constant-Murley shoulder assessment protocols varied widely regarding several procedural details, and therefore they decided to use the original description as published by Constant and Murley in 1987 [10]. Strength measurement represents ¼ of the CMS. The importance of the strength subscale has been debated, especially for the elderly, but in younger persons, strength has an important impact on daily work or recreation [4, 17, 33]. Even so, numerous studies using the CMS do not provide detailed descriptions of arm, sitting, or standing positions when performing strength measurements [11, 15, 22, 23, 25, 27]. However, different positions during measurement are likely to influence the results and therefore any comparison of the clinical data from different studies. Furthermore, only scarce data exist regarding the intraobserver reliability of the strength measurement part of the CMS [5, 17, 19].
The original description of the score defined a measurement position of 90° abduction of the affected shoulder [6, 10]. In clinical reality, a large number of patients may not be able to adopt this position owing to pain or other limitations. In a recent review, Constant et al. [9] recommended strength be scored as zero in patients who are unable to achieve the aforementioned test position. Such a simplification is debatable, as the overall score becomes biased in a disproportionate way; they also do not provide any scientific justification for this approach. Others have measured shoulder strength in the maximum possible position of abduction, which may be less than 90° [3, 21, 32]. This imprecision in the use of the CMS and the absence of data regarding the possible impact of the length of the lever arm [9] (ie, differing arm and torso positions on the force generated) motivated us to evaluate the reliability of the CMS strength measurement in more detail.
We therefore raised three questions. First, we asked whether varying degrees of shoulder abduction and stabilization or nonstabilization of the torso at the time of measurement had an impact on the strength values obtained; if the answer was in the affirmative, we planned additional analysis to quantify the relationships of these measurements. Second, we asked whether different abduction and torso positions also might influence the test-retest reliability of strength measurement. Third, we determined whether age, gender, arm length, or body mass index (BMI) had an effect on the strength measurements.
Materials and Methods
We recruited 33 healthy volunteers with a negative shoulder history from our institution’s staff: 14 males and 19 females with a median age of 31 years (range, 16–50 years). There were no additional exclusion criteria. Owing to missing data in the literature regarding the reliability of strength measurements at varying degrees of shoulder abduction, we could not perform a realistic power analysis. We based our decision to include a minimum number of 30 subjects on existing data showing high intraobserver and interobserver reliability for 90° abduction only as reported by Johansson and Adolfsson [17] and obtained using different strength measurement devices. All volunteers were informed routinely about the study and agreed to participate in accordance with the study approval given by the local ethics committee (EK327/07). Participants did not start any weight-lifting training during the 2-week study interval and did not report any relevant accidents or problems during the study period between single measurements. Volunteers were examined in a standardized manner for shoulder strength. We decided to use a well-established handheld dynamometer (Isobex®; Cursor AG, Berne, Switzerland) [1, 12, 13, 18] to analyze the effect of arm and torso positions on strength measurement. To test for other possible influences on strength, we examined the influence of additional factors, including age, gender, arm length, body weight, height, and BMI. The median length of the right and left arms measured from the acromion to the distal radius at the joint line (lever arm) was 54 cm (range, 42–64 cm). The median body weight and height were 72 kg (range, 45–125 kg) and 173 cm (range, 158–203 cm), respectively, with a median BMI of 23 (range, 17–35). An abbreviated self-assessment CMS test [3, 26] was completed by the volunteers, which indicated no shoulder complaints, with every volunteer scoring the maximum of 75 points on a scale from 0 to 75. The performance of all tests was monitored by an orthopaedic shoulder registrar (BW) not involved in the analysis. The intraobserver reliability of strength measurement was determined by having the same observer assess the shoulder strength of every volunteer on two occasions during a 2-week period. At the second assessment, the observer did not have access to the data from the first assessment. As 12 measurements were made on each volunteer each time, the observer was unlikely to remember the results of the first assessment by the time it came to the second assessment. Data were recorded by a second person. The sequence of single measurements was determined in a randomized manner by drawing lots. Measurements of the isometric strength of the shoulder muscles (in kilograms) were obtained at 30°, 60°, and 90° abduction in the scapular plane with the volunteer sitting on a chair with and without stabilization of the torso. Stabilization of the torso was achieved by direct contact of the contralateral shoulder and trunk with a wall. This position prevents leaning toward the contralateral side and the additional use of the trunk muscles (Fig. 1). The elbow was fully extended and the wrist pronated with the hand facing the floor. The sling of the dynamometer was fixed around the wrist and the mean of the two strength measurements was used for further statistical analysis. Each Isobex® measurement represents the maximum contraction of every volunteer, whereby the dynamometer calculates the mean of 30 readings over a 3-second period after which a sound signals the end of testing. Scapular rotation was restricted by the examiner’s hand as scapular rotation accounts for 1/3 of arm abduction [22]. Functional evaluation was assessed using the CMS as a raw score and abduction of the arm was measured using a goniometer.
Fig. 1A–B.
The photographs illustrate strength measurement with the arm in 60° abduction with (A) a stabilized torso (by the wall) versus (B) a nonstabilized position.
Data were entered in an Excel® sheet (Microsoft Corp, Redmond, WA). Continuous variables were described using means, medians, standard deviations, and ranges. Categorical variables were tabulated with absolute and relative frequencies. We used T tests to compare mean values of different variables, eg, for the comparison of strength measurements in different positions. Pearson correlations were used to test the relation of strength of different measurement conditions. Linear regression analysis was done to calculate the correction factors (single multiplier B each) for the relation between the measurements in 90° abduction and those in 60° and 30° abduction with and without stabilization of the torso. To test our assumption that the law of lever would be operative in strength measurements at differing degrees of abduction, we compared the computed correction factors with the theoretical correction factors for the law of lever: theoretical correction factor = sin (abduction [degrees]). To test the intraobserver reliability, two-way random single-measure intraclass correlation coefficients [ICC (2, 1)] with 95% confidence intervals were calculated to take into account systematic differences (ie, higher values in the second measurement). The impact of possible cofactors of influence such as age, gender, height, weight, or BMI was examined by univariate and multivariate regression analyses. The latter included only those variables significant in the univariate model. BMI is calculated from height and weight; therefore, in the case of significance for all these factors, the BMI or height and weight (but not all three) were included in the model depending on major statistical impact. We used SPSS® 13.0 (SPSS Inc, Chicago, IL) for all analyses.
Results
Varying degrees of shoulder abduction and stabilization or nonstabilization of the torso at the time of measurement influenced the strength values obtained (Tables 1 and 2). The observed absolute strength values differed for the dominant and nondominant arms and also for a stabilized or nonstabilized torso, depending on the evaluated abduction position (Table 1). However, we found high correlations between the relevant measurements (Table 2). Additional examination by linear regression analysis of the observed relations revealed single correction factors for calculation of the mean strength value for one measurement position or another. For example, the mean multiplier (B) between 90° and 60° was 0.854, resulting in a correction factor of 0.854 to transform a measured strength value for 60° abduction into a value for 90° abduction (Table 3). The corresponding correction factors were assumed to follow the law of the lever, resulting in a multiplier of 0.87 to transform a measured strength value for 60° abduction into a value for 90° abduction and a multiplier of 0.50 for 30° into 90° abduction. Comparison of the absolute mean strength value in 90° abduction for the dominant and nondominant arms yielded a correction factor of 1.036 to transform a measured strength value for the nondominant arm into a value for the dominant arm. The correction factor was 1.091 to transform a measured strength value with a stabilized torso into a value with a nonstabilized torso.
Table 1.
Strength measurements*
| Side | Stabilization | Abduction | Strength (kg) | ||||
|---|---|---|---|---|---|---|---|
| Mean | Standard deviation | Median | Minimum | Maximum | |||
| Dominant | Without | 90° | 6.36 | 2.70 | 6.00 | 1.75 | 10.90 |
| Without | 60° | 7.25 | 2.92 | 6.60 | 2.40 | 12.10 | |
| Without | 30° | 11.63 | 5.38 | 10.60 | 4.10 | 23.30 | |
| With | 90° | 5.90 | 2.39 | 5.55 | 1.60 | 9.85 | |
| With | 60° | 6.85 | 2.78 | 6.40 | 1.55 | 12.20 | |
| With | 30° | 10.49 | 4.90 | 8.75 | 3.40 | 24.50 | |
| Nondominant | Without | 90° | 5.80 | 2.77 | 5.75 | 1.55 | 10.70 |
| Without | 60° | 6.98 | 3.18 | 6.70 | 1.95 | 14.25 | |
| Without | 30° | 10.95 | 5.32 | 9.10 | 4.20 | 28.25 | |
| With | 90° | 5.72 | 2.58 | 5.60 | 1.40 | 10.95 | |
| With | 60° | 6.67 | 3.08 | 6.35 | 2.00 | 16.20 | |
| With | 30° | 9.48 | 4.15 | 8.55 | 2.75 | 23.45 | |
* T tests for the same side and stabilization type were significant for all differences between 90° and 60° (5.12 < t < 7.64; p < 0.0001), 60° and 30° (7.94 < t < 9.45; p < 0.0001), and 90° and 30° (9.29 < t < 9.82; p < 0.0001).
Table 2.
Pearson’s correlation (r) for strength under different measurement conditions
| Measurement condition | Dominant side without stabilization | ||
|---|---|---|---|
| 90° | 60° | 30° | |
| Dominant side with stabilization | 0.969 | 0.968 | 0.912 |
| Nondominant side without stabilization | 0.963 | 0.956 | 0.876 |
| Dominant side with stabilization in 90° abduction | 0.975 | 0.890 | |
Table 3.
Linear regression analysis
| Side | Stabilization | 60° abduction | 30° abduction | ||||
|---|---|---|---|---|---|---|---|
| B | Standard error | Corrected R2 | B | Standard error | Corrected R2 | ||
| Dominant | Without | 0.881 | 0.013 | 0.99 | 0.530 | 0.018 | 0.96 |
| With | 0.856 | 0.017 | 0.99 | 0.543 | 0.016 | 0.97 | |
| Nondominant | Without | 0.832 | 0.018 | 0.98 | 0.519 | 0.017 | 0.97 |
| With | 0.846 | 0.021 | 0.98 | 0.595 | 0.021 | 0.98 | |
| Mean | 0.854 | 0.547 | |||||
| Theoretical value (law of lever) | 0.866 | 0.500 | |||||
B = multiplier (correction factor).
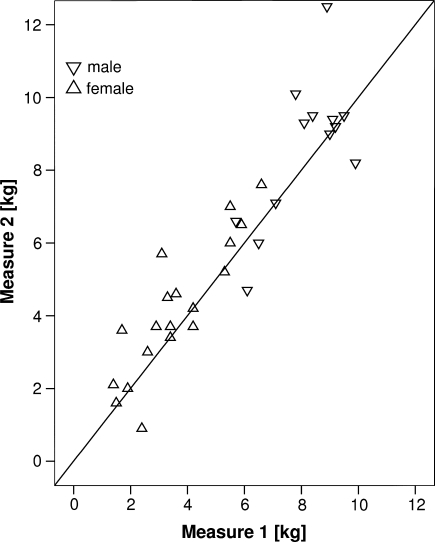
Different abduction and torso positions influenced the test-retest-reliability of the procedure. The highest intraobserver reliability was observed for volunteers sitting without torso stabilization and with the arm in 90° abduction (Fig. 2). Nevertheless, the retest reliability of single shoulder strength measurements was high with a range of ICC values between 0.71 and 0.93 (p < 0.001 for all) (Table 4).
Fig. 2.
A comparison of first and second strength measurements (intraobserver reliability) with the arm in 90° abduction and a nonstabilized torso is shown.
Table 4.
Intraobserver (test-retest) reliability of varying strength measurement positions*
| Side | Stabilization | Abduction | ICC (2, 1) | Lower limit | Upper limit |
|---|---|---|---|---|---|
| Dominant | Without | 90° | 0.93 | 0.86 | 0.96 |
| Without | 60° | 0.76 | 0.56 | 0.88 | |
| Without | 30° | 0.81 | 0.64 | 0.90 | |
| With | 90° | 0.84 | 0.70 | 0.92 | |
| With | 60° | 0.71 | 0.48 | 0.85 | |
| With | 30° | 0.76 | 0.56 | 0.87 | |
| Nondominant | Without | 90° | 0.92 | 0.84 | 0.96 |
| Without | 60° | 0.88 | 0.77 | 0.94 | |
| Without | 30° | 0.84 | 0.70 | 0.92 | |
| With | 90° | 0.88 | 0.78 | 0.94 | |
| With | 60° | 0.91 | 0.82 | 0.95 | |
| With | 30° | 0.81 | 0.64 | 0.90 |
* All single intraclass correlation coefficients (ICCs) were significant (p < 0.0001).
In the univariate analysis, gender, arm length, height, weight, and BMI but not age influenced the strength measurement of single measurement positions but to varying degrees (Table 5). Multivariate regression analysis confirmed this influence only for gender (p < 0.001) and weight (p < 0.017), but not for height (p < 0.246) or arm length (p < 0.137).
Table 5.
Univariate analysis of influencing factors on strength measurement (Pearson’s r)
| Side | Stabilization | Abduction | Male | Arm length | Height | Weight | BMI | Age |
|---|---|---|---|---|---|---|---|---|
| Dominant | Without | 90° | 0.83‡ | 0.57‡ | 0.70‡ | 0.72‡ | 0.58‡ | 0.06 |
| Without | 60° | 0.83‡ | 0.54† | 0.65‡ | 0.67‡ | 0.55‡ | 0.07 | |
| Without | 30° | 0.75‡ | 0.53† | 0.67‡ | 0.69‡ | 0.54† | 0.02 | |
| With | 90° | 0.83‡ | 0.55‡ | 0.67‡ | 0.74‡ | 0.63‡ | −0.02 | |
| With | 60° | 0.80‡ | 0.47† | 0.58‡ | 0.66‡ | 0.58‡ | 0.06 | |
| With | 30° | 0.78‡ | 0.48† | 0.59‡ | 0.67‡ | 0.57‡ | 0.05 | |
| Nondominant | Without | 90° | 0.82‡ | 0.57‡ | 0.68‡ | 0.72‡ | 0.59‡ | 0.00 |
| Without | 60° | 0.77‡ | 0.52† | 0.64‡ | 0.69‡ | 0.58‡ | 0.06 | |
| Without | 30° | 0.79‡ | 0.49† | 0.60‡ | 0.66‡ | 0.55‡ | 0.05 | |
| With | 90° | 0.82‡ | 0.53† | 0.62‡ | 0.68‡ | 0.57‡ | 0.05 | |
| With | 60° | 0.73‡ | 0.45† | 0.55† | 0.63‡ | 0.56‡ | 0.01 | |
| With | 30° | 0.67‡ | 0.32* | 0.44* | 0.57‡ | 0.52† | −0.07 |
* p < 0.05; †p < 0.01; ‡p < 0.001; BMI = body mass index.
Discussion
The CMS is one of the most frequently used evaluation scores for shoulder disorders [6–10, 17, 30]. Even so, several shortcomings in the development and use of the score have been emphasized only recently, particularly regarding strength measurement and the need for reevaluation using scientific methods to verify its reliability and sensitivity [20]. Although muscle strength forms an important subparameter, no consensus exists regarding how exactly it should be assessed. Measurement positions differ importantly in published studies or are not reported at all [10, 11, 14–16, 21, 25, 30]. The primary purpose of our study was to investigate whether and to what extent the degree of shoulder abduction and torso position influence shoulder strength measurement on the CMS. Second, we examined the intraobserver reliability of the relevant strength measurement positions. Finally, additional patient-dependent factors potentially influencing the evaluated strength measures were included in our analysis.
Several limitations of this investigation should be noted. First, the study was performed on a limited population of healthy volunteers with no history of shoulder abnormality and a maximum age of 50 years based on the assumption that the subparameter “strength” is especially important in younger persons. Additional studies are needed to test additional implications of our results, for example, in the elderly or in patients with shoulder abnormalities.
Second, shoulder strength was performed exclusively with the commercially available Isobex® apparatus, which has proven useful, reliable, and efficient for assessing shoulder strength in routine clinical practice [16–19]. Third, our findings are restricted to the specific positions and details of measurement we describe.
We found the degree of shoulder abduction influenced strength measurement, a finding that may be presumed to be an effect of modifying the force lever arm [9, 29]. In the dominant arm, maximum absolute strength values in 30° abduction and without stabilization of the torso were approximately twice as high as in 90° abduction with a stabilized torso. We found high correlations between the different positions of muscle strength measurement, even though absolute strength values varied importantly, especially depending on the degree of abduction. These consistent results provide strong evidence that our measurements are reliable. To our knowledge, there is no other study investigating the relationship between different arm and torso positions and strength measurement. In the current literature, many authors who report the exact shoulder position used for strength measurement of the CMS preferred the 90° abduction position [5, 7, 16, 24, 31]. Some studies do not report their procedure in cases where a patient could not abduct the arm to 90° [11, 16, 23, 27]. Some authors [5, 21, 32] took the strength value measured in maximal possible abduction. According to our findings, this approach overestimates strength on the CMS [24], making the overall score too high. Only recently, Constant et al. [9] underlined the necessity for the strength measurement to be performed in 90° abduction, and their alternative proposal, ie, to set strength as zero for the score if the patient cannot abduct to the 90° abduction position, causes an important underestimation of shoulder strength and a CMS that is too low. They do not give any scientific basis for this recommendation, which contradicts earlier publications [8, 10]. Furthermore, the results of patients with abduction less than 90° will be distorted twice, as their range of motion also is recorded as reduced.
Clinical experience suggests patients often tend to augment their strength by additional contralateral torso inclination during strength measurement for the CMS. In effect, standardized evaluations normally try to avoid body angulation [16]. Our finding that strength was, in general, 10% lower if the volunteer was stabilized compared with the nonstabilized position confirmed our primary question. Interestingly, the observed high correlation of strength measurements in different arm and torso positions offered us the possibility of adjusting strength values more precisely by using elaborated correction factors, eg, to convert the recorded strength values with the arm in 30° abduction into a value for 90° abduction. The correction factors we found were almost identical to those expected by implementing the law of the lever, which supports our assumption of the importance of the law in this context. If future studies in patients confirm our findings in the clinical setting, the overestimation or underestimation of the strength measurement and its consequences for the absolute CMS could be avoided. A feasible alternative is the use of relative instead of absolute score values, ie, the “in patient-weighted” comparison with the contralateral side, at least in patients with a unilateral problem only.
We observed a high retest reliability for the muscle strength measurements in all evaluated positions. The best intraobserver reliability in our study was recorded for participants sitting with a nonstabilized trunk and an extended arm in 90° abduction. This finding did not confirm our clinical expectation that systematic stabilization of the trunk would lead to a greater retest reliability than nonstabilization of the trunk. However, the differences in raw data between stabilized and nonstabilized measurements were low. Conboy et al. [5] reported low intraobserver reliability of the total CMS. In contrast, Johansson and Adolfsson [17], with a different measurement design, found high intraobserver and interobserver reliability for the strength test in the Constant-Murley assessment, with an ICC ranging from 0.89 to 0.98 in 90° abduction. We recorded the highest ICCs of 0.84 to 0.93 with the patient’s arm in 90° abduction. As Conboy et al. [5] reported an examination with the patient’s arm at or as near as possible to 90° abduction, it may be a lower degree of abduction in their study explains the observed discrepancy.
Finally, the assessment of patient-dependent factors potentially affecting the evaluation of strength measurements by multivariate regression analysis revealed an impact of gender and weight but not arm length or height on the observed results. The generally expected effect of gender on strength measurement is consistent with the findings of Brinker et al. [4], who reported higher strength values for men. They assumed this gender effect to be explained partially by differences in the body mass. In contrast, our multivariate analysis suggested gender and weight independently influenced shoulder muscle strength. Our findings imply, without adequate gender and weight modification of the CMS, published results may be biased, which must affect comparison between different study populations. As we report on a group of younger healthy volunteers only, we cannot comment on the overall impact of age in this context. Additional investigations need to specifically address the influence of parameters such as age, body weight, or well-defined muscle activity in more detail.
Our findings emphasize the importance of standardized torso and arm positions ensuring high reliability when performing the strength measurement of the CMS. We found the degree of shoulder abduction influenced strength values. Intraobserver reliability was most reliable at 90° abduction without stabilization of the torso. Our data from healthy volunteers suggest 90° abduction strength may be adequately predicted from measurements in a lower abduction position by the use of specific correction factors. Studies in patients and in the elderly are needed to confirm our findings with the aim of increasing the precision of clinical shoulder evaluation and enabling comparison with international data.
Acknowledgments
We thank J. Buchanan for editorial assistance with the manuscript.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Department of Orthopaedic Surgery and Traumatology, Kantonsspital Bruderholz.
References
- 1.Bankes MJ, Crossman JE, Emery RJ. A standard method of shoulder strength measurement for the Constant score with a spring balance. J Shoulder Elbow Surg. 1998;7:116–121. doi: 10.1016/S1058-2746(98)90220-8. [DOI] [PubMed] [Google Scholar]
- 2.Beaton D, Richards RR. Assessing the reliability and responsiveness of 5 shoulder questionnaires. J Shoulder Elbow Surg. 1998;7:565–572. doi: 10.1016/S1058-2746(98)90002-7. [DOI] [PubMed] [Google Scholar]
- 3.Boehm D, Wollmerstedt N, Doesch M, Handwerker M, Mehling E, Gohlke F. [Development of a questionnaire based on the Constant-Murley Score for self-evaluation of shoulder function by patients] [in German] Unfallchirurg. 2004;107:397–402. doi: 10.1007/s00113-004-0757-3. [DOI] [PubMed] [Google Scholar]
- 4.Brinker MR, Cuomo JS, Popham GJ, O’Connor DP, Barrack RL. An examination of bias in shoulder scoring instruments among healthy collegiate and recreational athletes. J Shoulder Elbow Surg. 2002;11:463–469. doi: 10.1067/mse.2002.126209. [DOI] [PubMed] [Google Scholar]
- 5.Conboy VB, Morris RW, Kiss J, Carr AJ. An evaluation of the Constant-Murley shoulder assessment. J Bone Joint Surg Br. 1996;78:229–232. [PubMed] [Google Scholar]
- 6.Constant CR. Age Related Recovery of Shoulder Function After Injury [master thesis, Mch]. Cork, Ireland: University College; 1986.
- 7.Constant CR. [Assessment of shoulder function] [in German] Orthopade. 1991;20:289–294. [PubMed] [Google Scholar]
- 8.Constant CR. An evaluation of the Constant-Murley shoulder assessment. J Bone Joint Surg Br. 1997;79:695–696. [PubMed] [Google Scholar]
- 9.Constant CR, Gerber C, Emery RJ, Søjbjerg JO, Gohlke F, Boileau P. A review of the Constant score: modifications and guidelines for its use. J Shoulder Elbow Surg. 2008;17:355–361. doi: 10.1016/j.jse.2007.06.022. [DOI] [PubMed] [Google Scholar]
- 10.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 11.Dimakopoulos P, Kasimatis G, Panagopoulos A. Transosseous suture fixation of proximal humeral fractures. J Bone Joint Surg Am. 2007;89:1700–1709. doi: 10.2106/JBJS.F.00765. [DOI] [PubMed] [Google Scholar]
- 12.Gerber C, Arneberg O. Measurement of abductor strength using an electronic device (Isobex) J Shoulder Elbow Surg. 1993;2:56. [Google Scholar]
- 13.Gerber C, Hersche O, Farron A. Isolated rupture of the subscapularis tendon. J Bone Joint Surg Am. 1996;78:1015–1023. doi: 10.2106/00004623-199607000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Gore DR, Murray MP, Sepic SB, Gardner GM. Shoulder-muscle strength and range of motion following surgical repair of full-thickness rotator-cuff tears. J Bone Joint Surg Am. 1986;68:266–272. [PubMed] [Google Scholar]
- 15.Hintermann B, Trouillier HH, Schäfer D. Rigid internal fixation of fractures of the proximal humerus in older patients. J Bone Joint Surg Br. 2000;82:1107–1112. doi: 10.1302/0301-620X.82B8.10330. [DOI] [PubMed] [Google Scholar]
- 16.Hirschmann M, Quarz V, Audige L, Ludin D, Messmer P, Regazzoni P, Gross T. Internal fixation of unstable proximal humerus fractures with an anatomically preshaped interlocking plate: a clinical and radiologic evaluation. J Trauma. 2007;63:1314–1323. doi: 10.1097/01.ta.0000240457.64628.38. [DOI] [PubMed] [Google Scholar]
- 17.Johansson KM, Adolfsson LE. Intraobserver and interobserver reliability for the strength test in the Constant-Murley shoulder assessment. J Shoulder Elbow Surg. 2005;14:273–278. doi: 10.1016/j.jse.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 18.Katolik LI, Romeo AA, Cole BJ, Verma NN, Hayden JK, Bach BR. Normalization of the Constant score. J Shoulder Elbow Surg. 2005;14:279–285. doi: 10.1016/j.jse.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 19.Leggin BG, Neuman RM, Iannotti JP, Williams GR, Thompson EC. Intrarater and interrater reliability of three isometric dynamometers in assessing shoulder strength. J Shoulder Elbow Surg. 1996;5:18–24. doi: 10.1016/S1058-2746(96)80026-7. [DOI] [PubMed] [Google Scholar]
- 20.Lillkrona U. How should we use the Constant Score? A commentary. J Shoulder Elbow Surg. 2008;17:362–363. doi: 10.1016/j.jse.2007.06.013. [DOI] [PubMed] [Google Scholar]
- 21.Meier R, Messmer P, Regazzoni P, Rothfischer W, Gross T. Unexpected high complication rate following internal fixation of unstable proximal humerus fractures with an angled blade plate. J Orthop Trauma. 2006;20:253–260. doi: 10.1097/00005131-200604000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Michiels I, Grevenstein J. Kinematics of shoulder abduction in the scapular plane: on the influence of abduction velocity and external load. Clin Biomech (Bristol, Avon). 1995;10:137–143. doi: 10.1016/0268-0033(95)93703-V. [DOI] [PubMed] [Google Scholar]
- 23.Moonot P, Ashwood N, Hamlet M. Early results for treatment of three- and four-part fractures of the proximal humerus using the PHILOS plate system. J Bone Joint Surg Br. 2007;89:1206–1209. doi: 10.1302/0301-620X.89B9.18528. [DOI] [PubMed] [Google Scholar]
- 24.Moseley H. Examination of the Shoulder. New York, NY: Paul B. Hober; 1972. [Google Scholar]
- 25.Othman A, Taylor G. Is the Constant score reliable in assessing patients with frozen shoulder? 60 shoulders scored 3 years after manipulation under anaesthesia. Acta Orthop Scand. 2004;75:114–116. doi: 10.1080/00016470410001708230. [DOI] [PubMed] [Google Scholar]
- 26.Patel VR, Singh D, Calvert PT, Bayley JI. Arthroscopic subacromial decompression: results and factors affecting outcome. J Shoulder Elbow Surg. 1999;8:231–237. doi: 10.1016/S1058-2746(99)90134-9. [DOI] [PubMed] [Google Scholar]
- 27.Robinson CM, Page RS. Severely impacted valgus proximal humeral fractures: results of operative treatment. J Bone Joint Surg Am. 2003;85:1647–1655. doi: 10.1302/0301-620X.85B7.13959. [DOI] [PubMed] [Google Scholar]
- 28.Rocourt MH, Radlinger L, Kalberer F, Sanavi S, Schmid NS, Leunig M, Hertel R. Evaluation of intratester and intertester reliability of the Constant-Murley shoulder assessment. J Shoulder Elbow Surg. 2008;17:364–369. doi: 10.1016/j.jse.2007.06.024. [DOI] [PubMed] [Google Scholar]
- 29.Sharkey NA, Marder RA, Hanson PB. The entire rotator cuff contributes to elevation of the arm. J Orthop Res. 1994;12:699–708. doi: 10.1002/jor.1100120513. [DOI] [PubMed] [Google Scholar]
- 30.Thomas M, Dieball O, Busse M. [Normal values of the shoulder strength in dependency on age and gender-comparison with the Constant, UCLA, ASES scores and SF36 health survey] [in German] Z Orthop Ihre Grenzgeb. 2003;141:160–170. doi: 10.1055/s-2003-38662. [DOI] [PubMed] [Google Scholar]
- 31.Walton MJ, Walton JC, Honorez LA, Harding VF, Wallace WA. A comparison of methods for shoulder strength assessment and analysis of Constant score change in patients aged over fifty years in the United Kingdom. J Shoulder Elbow Surg. 2007;16:285–289. doi: 10.1016/j.jse.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 32.Wijgman AJ, Roolker W, Patt TW, Raaymakers EL, Marti RK. Open reduction and internal fixation of three and four-part fractures of the proximal part of the humerus. J Bone Joint Surg Am. 2002;84:1919–1925. [PubMed] [Google Scholar]
- 33.Yian EH, Ramappa AJ, Arneberg O, Gerber C. The Constant score in normal shoulders. J Shoulder Elbow Surg. 2005;14:128–133. doi: 10.1016/j.jse.2004.07.003. [DOI] [PubMed] [Google Scholar]