Abstract
Background
Treatment of partial-thickness articular surface rotator cuff tears varies from simple débridement with or without an acromioplasty to various repair techniques. These repair techniques have included in situ transtendinous methods, as well as completion of the tear and repairing the full-thickness defect. The transtendinous techniques can be associated with stiffness and completing the tear takes down normal intact tissue. Therefore, a technique was developed that repairs the articular-side partial- thickness rotator cuff tears with an all-inside approach that does not violate the intact bursal tissue and does not complete the tear.
Questions/purposes
To compare the preoperative and postoperative Penn shoulder scores (PSS) associated with an in situ all-inside repair technique and the effects of such a repair on postoperative stiffness.
Methods
Twenty patients with partial-thickness articular rotator cuff tears greater than 50% of the width of the tendon repaired with an all-inside repair technique were retrospectively reviewed. Two of the patients were high school athletes and the rest self-described as recreational athletes. The minimum followup was 16 months (average, 29 months; range, 16–41 months). A validated outcome measure (PSS) was used to assess clinical outcome, and postoperative ROM was measured.
Results
The average PSS score improved from 74 (range, 56–84) to 92 (range, 86–99). All but one patient was able to return to the same level of play or higher.
Conclusions
In situ repairs of partial-thickness articular surface tears using an all-inside approach resulted in a substantial increase in PSS with no cases of major postoperative clinical stiffness.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Partial-thickness rotator cuff tears (RCTs) have been classified by Ellman [5] by the depth of the tear. Grade 1 is less than 3 mm, Grade 2 is between 3 and 6 mm, and Grade 3 is greater than 6 mm in depth, and these are further divided into articular (A), bursal (B), or interstitial (I). The management of partial-thickness tears is controversial and is evolving according to new biomechanical and clinical data [3, 6, 11]. Some authors have reported results with simple débridement of small partial-thickness RCTs (Ellman Grades 1 and 2) [3, 14, 20]. A retrospective review of 46 patients with either a Grade I tear (26) or a Grade II tear (20) who were treated with a subacromial decompression reported an increase in ASES scores from 37.4 to 86.6 [14]. However, larger Grade 3 tears treated with débridement have resulted in poorer clinical outcomes when compared to repair, and the literature suggests Grades 3A, 2B, and 3B partial-thickness RCTs are better treated with repair as opposed to débridement [3, 18, 26]. This has prompted many surgeons to repair these larger partial tears with various techniques, including completion of the partial tear and repairing a full-thickness defect and various in situ techniques [1, 10, 11, 16, 22, 24].
Repairing a high-grade articular-sided defect or partial articular supraspinatus tendon avulsion (PASTA) lesion can be technically challenging. The in situ techniques have the advantage of leaving the intact bursal layer of the rotator cuff intact. Although these techniques do not involve completing the tear, they do involve tying suture on the bursal side of the rotator cuff and potentially overtightening the bursal layer of the cuff. Some authors have reported increased stiffness with these transtendinous repair techniques [9, 23, 28]. Therefore, a repair technique that just addresses the abnormality by repairing the articular-side tear only and does not tie down the bursal side of the cuff has been developed. This technique was previously described by the author with preliminary short term data [23].
The purpose of the study was to further describe the in situ all-inside repair technique and the effects of the repair technique on the PSS function score and range of motion (stiffness).
Patients and Methods
Thirty-two patients (22 men, 10 women) with 50% or greater PASTA lesions who had surgical repairs using an all-inside technique were retrospectively reviewed. Fifteen of these patients were previously reported in a 2007 article describing the technique [23]. The data on those patients was short term and included those who had other concomitant procedures performed. Only 8 of those original 15 patients who met our current inclusion criteria were included in this study. Partial tears from 50% to 75% were repaired. The tear size was determined by using a calibrated probe inserted from the subacromial space into the cuff tear through the intact bursal portion of the cuff. The tear size was expressed as a percentage of the amount of exposed tuberosity with respect to the entire cuff thickness or footprint. Surgeries were performed by a single surgeon between February 2006 and January 2009. Patients were included if they had an MRI documented PASTA lesion and had failed at least 6 weeks of nonoperative treatment, including physical therapy with or without subacromial corticosteroid injections. We excluded 12 patients who had additional procedures (eg, distal clavicular resection, labral repair, or biceps tenotomy or tenodesis). These were excluded to minimize other variables so that the effect of the repair could be better isolated. This left 20 patients (16 men, four women) for this study. All patients had unilateral surgery and there was no known pathology in the opposite shoulder. Ages ranged from 18 to 54 years, with an average of 41 years. There were two high school athletes and the rest described themselves as recreational athletes. All patients stated one of their reasons for the surgery was that they were not able to participate in one or more of their sports or recreational activities. The minimum followup was 16 months (average, 29 months; range, 16–41 months). No patients were lost to followup. All patients gave their consent for inclusion in the study and IRB approval was obtained.
The decision to perform an all-inside technique as opposed to completing the tear was made on the basis of the integrity and appearance of the remaining bursal cuff tissue. If the remaining bursal tissue was deemed of poor or questionable quality, the tear was completed and the full-thickness tear was repaired. Subacromial bursoscopy was performed in all, but formal decompressions were performed in only 17 of the 20. The three patients in whom a decompression was not performed were younger (the oldest of the three was 35 years old) and the subacromial space looked pristine.
The all-inside repair technique repairs the torn articular layer of the rotator cuff anatomically to the medial portion of the greater tuberosity. The rotator cuff edge was débrided and the depth was assessed by determining the amount of exposed greater tuberosity. We prepared the greater tuberosity by débriding the adherent tissue as described [23]. A typical articular partial-thickness RCT in a left shoulder as viewed from the posterior portal is shown (Fig. 1). Two portals are used in the rotator cuff interval to facilitate this technique (Fig. 2). The initial portal was made at the lateral apex of the rotator cuff interval and débridement of the tear and tuberosity was performed through this portal. A cannula of sufficient size to accommodate a suture-passing device of choice is required. A second portal was placed just above the subscapularis tendon and was used for retrieving the suture-passing device and suture. An anchor was placed through the intact bursal portion of the rotator cuff into the medial portion of the greater tuberosity (Fig. 3), which was first localized with a spinal needle. This could be facilitated by using a probe to retract the supraspinatus superiorly. The author usually uses a 3-mm polyetheretherketone anchor to minimize the size of the entry site, but any anchor can be used. The sutures were then brought into the joint. A Suture Lasso® (Arthrex, Inc, Naples, FL) or other similar suture-passing device was placed in the lateral cannula (Fig. 4) and was then passed through just the articular layer of the rotator cuff. For a left shoulder, a “right going” lasso was used. The wire from the lasso and a suture limb were then retrieved through the inferior cannula. The suture was placed in the wire and pulled through the tissue. This passed the suture through the articular lamina of the rotator cuff (Fig. 5). The other limb of the suture was then retrieved into the lateral cannula so that both limbs were within the lateral cannula (Fig. 5) and ready to be tied. The articular layer was then tied down, with the knot getting buried between the intact bursal layer and the newly repaired articular layer (Fig. 6). This can be performed multiple times for tears that are larger in the AP dimension starting from posterior and progressing anterior.
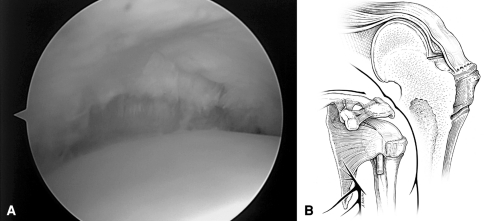
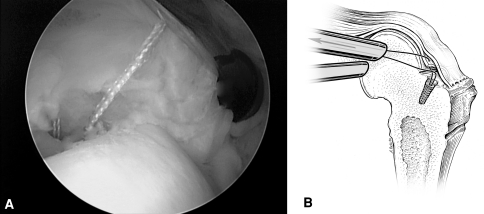
Fig. 1A–B.
(A) An arthroscopic view from the posterior portal shows a partial-thickness articular-surface RCT in a left shoulder. (B) A diagram illustrates a typical partial-thickness RCT. Reprinted with permission and ©2007 Wolters Kluwer Health from Spencer EE Jr. Partial-thickness articular surface rotator cuff tears: an all-inside technique. Tech Shoulder Elbow Surg. 2007;8:180–184.
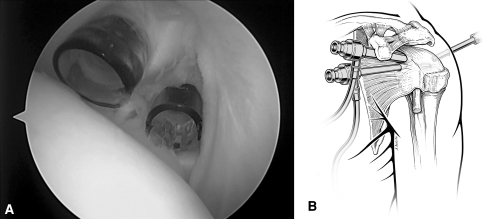
Fig. 2A–B.
(A) An arthroscopic view shows placement of two cannulae, with one at the apex of the rotator cuff interval and a smaller-diameter one inferior and medial just above the subscapularis. (B) A diagram illustrates the two cannulae within the rotator cuff interval. The inferior cannula is above the subscapularis tendon. Reprinted with permission and ©2007 Wolters Kluwer Health from Spencer EE Jr. Partial-thickness articular surface rotator cuff tears: an all-inside technique. Tech Shoulder Elbow Surg. 2007;8:180–184.
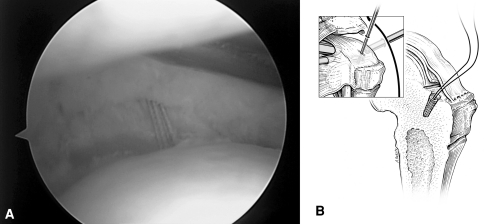
Fig. 3A–B.
(A) An arthroscopic view shows placement of an anchor just lateral to the articular cartilage in the medial portion of the greater tuberosity. (B) A diagram illustrates the anchor placement through the bursal portion of the cuff. Reprinted with permission and ©2007 Wolters Kluwer Health from Spencer EE Jr. Partial-thickness articular surface rotator cuff tears: an all-inside technique. Tech Shoulder Elbow Surg. 2007;8:180–184.
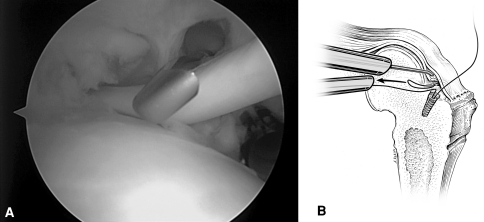
Fig. 4A–B.
(A) An arthroscopic view shows the suture lasso coming in through the lateral or apex cannula. (B) A diagram illustrates the suture lasso passing through the articular lamina and the wire being retrieved through the inferior cannula. Reprinted with permission and ©2007 Wolters Kluwer Health from Spencer EE Jr. Partial-thickness articular surface rotator cuff tears: an all-inside technique. Tech Shoulder Elbow Surg. 2007;8:180–184.
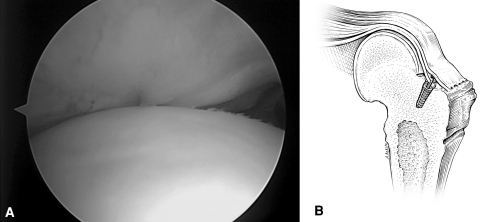
Fig. 5A–B.
(A) An arthroscopic view shows the suture passing through the torn articular lamina of the rotator cuff. The probe is retracting the cuff superiorly. (B) A diagram illustrates both suture limbs retrieved into the lateral cannula and ready to be tied. Reprinted with permission and ©2007 Wolters Kluwer Health from Spencer EE Jr. Partial-thickness articular surface rotator cuff tears: an all-inside technique. Tech Shoulder Elbow Surg. 2007;8:180–184.
Fig. 6A–B.
(A) An arthroscopic view shows the appearance of the repaired rotator cuff. The knot is buried between the two layers of the rotator cuff just behind the long head of the biceps. (B) A diagram illustrates the completed repair. Reprinted with permission and ©2007 Wolters Kluwer Health from Spencer EE Jr. Partial-thickness articular surface rotator cuff tears: an all-inside technique. Tech Shoulder Elbow Surg. 2007;8:180–184.
Formal physical therapy was initiated at 2 weeks postoperatively and included supine active assisted forward elevation and external rotation only for 4 weeks. At 6 weeks postoperatively, supine active forward elevation was started, as well as internal rotation stretching. At 8 weeks postoperatively, upright forward elevation was started with gentle isometric strengthening. ROM exercises and stretching continued until 12 weeks postoperatively when resistive band strengthening was started. Return to full unrestricted activity was allowed at 6 months postoperatively.
We saw patients at 2 weeks, 6 weeks, 12 weeks, 6 months and 12 months. True anteroposterior (Grashey) and supraspinatus outlet view (SOV) plain radiographs were obtained at the 2-week postoperative visit. At each visit the clinical exam included measurement of ROM initially in the supine position (in the early postoperative period) and subsequently in the upright position. All patients completed a validated outcome measure (Penn shoulder score or PSS [13]) preoperatively and at final followup. Postoperative ROM was measured by a therapist at the time of discharge and return to unrestricted activity. ROM measurements represented combined glenohumeral and scapulothoracic motion to give a total arc of motion measured in the upright position with a handheld goniometer. The opposite side was also measured to provide a comparison. Followup MRI was not performed.
Results
The average PSS score improved from 74 (range, 56–84) to 92 (range, 86–99). All but one patient were able to return to the same level of play or higher. One patient fell within the first 6 weeks of surgery and imaging revealed a probable retear, but the patient elected not to undergo surgical repair again.
No patient experienced postoperative stiffness; specifically, there was no difference between the operative and nonoperative shoulder ROM. The average ROM in the operative arm was 169° (range, 159°–176°) for forward elevation, 61° (range, 52°–69°) for external rotation with the arm at the side, 89° (range, 82°–94°) for external rotation in the 90° abducted position, and 48° (range, 36°–60°) for internal rotation in the 90° abducted position. The average ROM in the nonoperative arm was 168° (range, 160°–178°) for forward elevation, 65° (range, 55°–72°) for external rotation with the arm at the side, 90° (range, 86°–100°) for external rotation in the 90° abducted position, and 50° (range, 38°–60°) for internal rotation in the 90° abducted position.
Despite delaying formal physical therapy for 2 weeks, there was no postoperative stiffness.
Discussion
It has been suggested PASTA lesions greater than 50% of the width of the tendon are best managed with surgical repair, especially in younger patients [3, 18, 26]. To date those repairs have involved either converting the PASTA to a full-thickness tear and repairing the full-thickness defect or using a transbursal technique that keeps the bursal layer of the rotator cuff intact, but it also involves tying this layer down [1, 10, 11, 16, 22, 24]. Nonhealing events of the full-thickness tears that were created have been reported with followup ultrasound [11]. Those patients are potentially worse as they now have a full-thickness tear. The various transbursal or transtendinous techniques involve placing anchors in the medial footprint of the tuberosity. In an effort to get the torn articular layer to come back down to the medial footprint of the greater tuberosity, the sutures are passed through both layers of the rotator cuff medial enough to capture the articular layer. Once passed, these sutures are tied down on top of the bursal portion of the rotator cuff in the subacromial space. Such a technique will secure the articular layer to the medial footprint but will potentially overtighten the bursal portion of the cuff. This overtightening is a function of the degree of medial retraction of the torn articular layer. As such, the more medially retracted the articular layer is, the more medial the sutures must be passed. When tied down, the bursal portion of the cuff will be overtightened by an amount equal to the degree of retraction of the articular layer. This overtightening might be the cause of the stiffness that has been reported after these repairs [9, 28]. Therefore a technique was developed that attempts to repair just the PASTA lesion without passing suture through the bursal layer of the cuff, thereby performing the repair all inside the glenohumeral joint [23]. The purpose of the study was to describe an in situ all-inside repair technique and the effects of the repair technique on the PSS function score and range of motion (stiffness).
Readers should be aware of some limitations. First, the patients were carefully selected according to the indications. Further, patients with concomitant pathology were excluded to eliminate other variables in patient outcomes. Second, we had no imaging followup. Further research that includes MRI or ultrasound followup evaluating the all-inside technique is warranted. Also, the results presented here may not be applicable to the high-level overhead professional athlete as the patients in this study were self-described as recreational athletes.
Previous authors have reported substantial increases in American Shoulder and Elbow Surgeons scores by converting the PASTA lesion to a full-thickness tear and then repairing the full-thickness tear [4, 11]. Kamath et al. [11] did however report five nonhealing events in 42 patients treated in this fashion. A transtendinous technique was used by Ide et al. [10] in 17 patients. At an average of 39 months’ followup, they reported 14 excellent, two good, and one fair result. The results of the 20 patients in this study using the all-inside technique also demonstrate a substantial improvement in their PSS scores at an average followup of 29 months.
Stiffness was reported by Huberty et al. [9] as being more common in patients who had undergone transtendinous repair of a PASTA lesion. In contrast, no postoperative stiffness was seen in the patients in this study treated with the all-inside repair. There was no difference in forward elevation, external rotation with the arm at the side, or external and internal rotation in the 90° abducted position between the operative and nonoperative shoulders.
The incidence of partial-thickness RCTs increases with increasing age [21]. The majority of partial-thickness RCTs involve the articular side [7, 15]. This might be secondary to hypovascularity and reduced biomechanical strength [15, 19]. Nakajima et al. [19] found the bursal portion of the rotator cuff was able to undergo greater deformation and had increased tensile strength when compared to the articular portion. This lends support for Codman’s original hypothesis that most RCTs occur through a primary degenerative process [2].
The natural history of these partial-thickness tears is a gradual increase in size with time. Yamanaka and Matsumoto [29] followed 40 partial-thickness articular-surface RCTs with arthrography and found, at an average of 13 months, 53% were larger, 28% had progressed to full-thickness tears, while only 20% were the same or smaller. This clinical observation is supported by a cadaveric biomechanical study that evaluated the strain on the remaining intact portion of a PASTA lesion with respect to tear size [17]. The authors suggested that when the articular defect reaches 50% of the width of the tendon, the strain on the remaining intact fibers increases substantially. They also reported an in situ transbursal repair returned the strain to normal. Another cadaveric study evaluating PASTA lesions compared an in situ suture bridge technique to completing the tear and repairing the full-thickness defect; the gap formation was less and the ultimate tensile load was higher for the in situ technique [8].
The treatment of these partial-thickness tears should consist of nonoperative measures first [28]. Some of these tears become symptomatic secondary to altered kinematics of the glenohumeral joint such as a tight posterior capsule leading to a dynamic anterosuperior translation with forward elevation and subsequent impingement. Nonoperative measures should therefore include stretching (especially the posterior capsule) and rotator cuff strengthening focusing on external rotation strengthening [27].
If nonoperative measures fail, then operative management can be considered. Weber [26] reported on the results of 65 patients with either Grade 3A or 3B partial-thickness RCTs with a minimum 2-year followup. Patients had an arthroscopic decompression with either a mini-open repair or an arthroscopic débridement of the tear. The repair group had higher UCLA scores. With regard to smaller partial-thickness tears, Park et al. [20] reported 86% satisfactory results with tears of less than 50% thickness treated with arthroscopic débridement and decompression. Another study also reported smaller partial-thickness tears (less than 50% thickness) with débridement had L’Insalata scores averaging 89 postoperatively [3]. In addition, Miller et al. [18] reported an age-related difference in results when treating partial-thickness tears, with younger patients (younger than 50 years) not doing as well with débridement. Therefore the literature suggests repair of these larger tears, especially in younger patients, is warranted.
Based on this information, many surgeons choose to repair these larger partial tears. One option is to complete the tear and repair a full-thickness defect. Although Weber [26] reported good clinical results with tear completion, a recent study with ultrasound followup reported five of 42 tears treated in this fashion did not heal with a recurrent full-thickness defect [11]. These patients are potentially worse as they now have full-thickness defects. The repair techniques thus evolved with the creation of several methods of an in situ transtendinous repair [10, 12, 22, 24, 25]. Further evolution of the in situ repair was the development of an all-inside technique to address the issue of stiffness. The present study demonstrates good clinical results can be achieved with this all-inside technique without postoperative stiffness. By eliminating suture passing through the bursal portion of the cuff, this technique strives to limit the overtightening of the bursal portion of the cuff that can occur with previously described techniques.
In summary, the treatment of PASTA lesions remains controversial, but the literature suggests repair of lesions of greater than 50% of the width of the tendon yields better results. In situ repairs have the advantage of leaving the intact bursal cuff tissue intact, and biomechanically and clinically perform well. The all-inside in situ technique repairs the PASTA lesion without tying down the intact bursal portion of the rotator cuff. This allows the surgeon to just address the pathology while minimizing the effect on the surrounding structures, which might reduce postoperative stiffness. It should be noted this is an advanced arthroscopic technique and should be considered by those with an appropriate skill level.
Acknowledgments
I thank Andrea Parton, Jeff Jarnagin, and Lori Sharp for their help in collecting and assimilating the data.
Footnotes
The author certifies that he no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
The author certifies that his institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Brockmeier SF, Dodson CC, Gamradt SC, Coleman SH, Altchek DW. Arthroscopic intratendinous repair of the delaminated partial-thickness rotator cuff tear in overhead athletes. Arthroscopy. 2008;24:961–965. doi: 10.1016/j.arthro.2007.08.016. [DOI] [PubMed] [Google Scholar]
- 2.Codman EA. The Shoulder: Rupture of the Supraspinatus Tendon and Other Lesions in or about the Subacromial Bursa. Malabar, FL: Krieger Publishing Company; 1934. [Google Scholar]
- 3.Cordasco FA, Backer M, Craig EV, Klein D, Warren RF. The partial-thickness rotator cuff tear: is acromioplasty without repair sufficient? Am J Sports Med. 2002;30:257–260. doi: 10.1177/03635465020300021801. [DOI] [PubMed] [Google Scholar]
- 4.Deutsch A. Arthroscopic repair of partial-thickness tears of the rotator cuff. J Shoulder Elbow Surg. 2007;16:193–201. doi: 10.1016/j.jse.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 5.Ellman H. Diagnosis and treatment of incomplete rotator cuff tears. Clin Orthop Relat Res. 1990;254:64–74. [PubMed] [Google Scholar]
- 6.Freedman KB. The partial-thickness rotator cuff tear: is acromioplasty without repair sufficient? Am J Sports Med. 2003;31:325. doi: 10.1177/03635465030310022801. [DOI] [PubMed] [Google Scholar]
- 7.Fukuda H, Hamada K, Nakajima T, Yamada N, Tomonaga A, Goto M. Partial-thickness tears of the rotator cuff. A clinicopathological review based on 66 surgically verified cases. Int Orthop. 1996;20:257–265. doi: 10.1007/s002640050075. [DOI] [PubMed] [Google Scholar]
- 8.Gonzalez-Lomas G, Kippe MA, Brown GD, Gardner TR, Ding A, Levine WN, Ahmad CS. In situ transtendon repair outperforms tear completion and repair for partial articular-sided supraspinatus tendon tears. J Shoulder Elbow Surg. 2008;17:722–728. doi: 10.1016/j.jse.2008.01.148. [DOI] [PubMed] [Google Scholar]
- 9.Huberty DP, Schoolfield JD, Brady PC, Vadala AP, Arrigoni P, Burkhart SS. Incidence and treatment of postoperative stiffness following arthroscopic rotator cuff repair. Arthroscopy. 2009;25:880–890. doi: 10.1016/j.arthro.2009.01.018. [DOI] [PubMed] [Google Scholar]
- 10.Ide J, Maeda S, Takagi K. Arthroscopic transtendon repair of partial-thickness articular-sided tears of the rotator cuff. Am J Sports Med. 2005;33:1672–1679. doi: 10.1177/0363546505277141. [DOI] [PubMed] [Google Scholar]
- 11.Kamath G, Galatz LM, Keener JD, Teefey S, Middleton W, Yamaguchi K. Tendon integrity and functional outcome after arthroscopic repair of high-grade partial-thickness supraspinatus tears. J Bone Joint Surg Am. 2009;91:1055–1062. doi: 10.2106/JBJS.G.00118. [DOI] [PubMed] [Google Scholar]
- 12.Kim KC, Rhee KJ, Shin HD, Kim DK. Arthroscopic transtendon suture-bridge technique for concurrent articular- and bursal-side partial-thickness rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. 2009 June 16. [Epub ahead of print]. [DOI] [PubMed]
- 13.Leggin BG, Michener LA, Shaffer MA, Brenneman SK, Iannotti JP, Williams GR., Jr The Penn shoulder score: reliability and validity. J Orthop Sports Phys Ther. 2006;36:138–151. doi: 10.2519/jospt.2006.36.3.138. [DOI] [PubMed] [Google Scholar]
- 14.Liem D, Alci S, Dedy N, Steinbeck J, Marquardt B, Mollenhoff G. Clinical and structural results of partial supraspinatus tears treated by subacromial decompression without repair. Knee Surg Sports Traumatol Arthrosc. 2008;16:967–972. doi: 10.1007/s00167-008-0580-4. [DOI] [PubMed] [Google Scholar]
- 15.Lohr JF, Uhthoff HK. The microvascular pattern of the supraspinatus tendon. Clin Orthop Relat Res. 1990;254:35–38. [PubMed] [Google Scholar]
- 16.Lyons TR, Savoie FH, 3rd, Field LD. Arthroscopic repair of partial-thickness tears of the rotator cuff. Arthroscopy. 2001;17:219–223. doi: 10.1053/jars.2001.8017. [DOI] [PubMed] [Google Scholar]
- 17.Mazzocca AD, Rincon LM, O’Connor RW, Obopilwe E, Andersen M, Geaney L, Arciero RA. Intra-articular partial-thickness rotator cuff tears: analysis of injured and repaired strain behavior. Am J Sports Med. 2008;36:110–116. doi: 10.1177/0363546507307502. [DOI] [PubMed] [Google Scholar]
- 18.Miller SL, Hazrati Y, Cornwall R, Hayes P, Gothef T, Gladstone JL, Flatow EL. Failed surgical management of partial thickness rotator cuff tears. Orthopedics. 2002;25:1255–1257. doi: 10.3928/0147-7447-20021101-16. [DOI] [PubMed] [Google Scholar]
- 19.Nakajima T, Rokumma N, Hamada K, Tomatsu T, Fakuda H. Histologic and biomechanical characteristics of the supraspinatus tendon: Reference to rotator cuff healing. J Shoulder Elbow Surg. 1994;3:79–87. doi: 10.1016/S1058-2746(09)80114-6. [DOI] [PubMed] [Google Scholar]
- 20.Park JY, Yoo MJ, Kim MH. Comparison of surgical outcome between bursal and articular partial thickness rotator cuff tears. Orthopedics. 2003;26:387–390. doi: 10.3928/0147-7447-20030401-16. [DOI] [PubMed] [Google Scholar]
- 21.Sher JS, Uribe JW, Posada A, Murphy BJ, Zlatkin MB. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am. 1995;77:10–15. doi: 10.2106/00004623-199501000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Snyder SJ, Pachelli AF, Del Pizzo W, Friedman MJ, Ferkel RD, Pattee G. Partial thickness rotator cuff tears: results of arthroscopic treatment. Arthroscopy. 1991;7:1–7. doi: 10.1016/0749-8063(91)90070-E. [DOI] [PubMed] [Google Scholar]
- 23.Spencer E. Partial thickness articular surface rotator cuff tears: An all-inside technique. Tech Shoulder Elbow Surg. 2007;8:180–184. doi: 10.1097/BTE.0b013e3181593e51. [DOI] [Google Scholar]
- 24.Tauber M, Koller H, Resch H. Transosseous arthroscopic repair of partial articular-surface supraspinatus tendon tears. Knee Surg Sports Traumatol Arthrosc. 2008;16:608–613. doi: 10.1007/s00167-008-0532-z. [DOI] [PubMed] [Google Scholar]
- 25.Waibl B, Buess E. Partial-thickness articular surface supraspinatus tears: a new transtendon suture technique. Arthroscopy. 2005;21:376–381. doi: 10.1016/j.arthro.2004.11.008. [DOI] [PubMed] [Google Scholar]
- 26.Weber SC. Arthroscopic debridement and acromioplasty versus mini-open repair in the treatment of significant partial-thickness rotator cuff tears. Arthroscopy. 1999;15:126–131. doi: 10.1053/ar.1999.v15.0150121. [DOI] [PubMed] [Google Scholar]
- 27.Werner CM, Blumenthal S, Curt A, Gerber C. Subacromial pressures in vivo and effects of selective experimental suprascapular nerve block. J Shoulder Elbow Surg. 2006;15:319–323. doi: 10.1016/j.jse.2005.08.017. [DOI] [PubMed] [Google Scholar]
- 28.Wolff AB, Sethi P, Sutton KM, Covey AS, Magit DP, Medvecky M. Partial-thickness rotator cuff tears. J Am Acad Orthop Surg. 2006;14:715–725. doi: 10.5435/00124635-200612000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Yamanaka K, Matsumoto T. The joint side tear of the rotator cuff: A followup study by arthrography. Clin Orthop Relat Res. 1994;304:68–73. [PubMed] [Google Scholar]