Abstract
Problem
Significant regional disparities in human resources for health deployment in Senegal weaken the country's health system and compromise population health.
Approach
In recent years, the Ministry of Health adopted measures to improve the posting, recruitment and retention of health workers in rural and remote areas. One was the introduction of a special contracting system to recruit health workers.
Local setting
Health workers in Senegal are concentrated in specific urban centres, particularly Dakar. Whereas the Dakar region has 0.2 physicians per 1000 population, the Fatick, Kaolack, Kolda and Matam regions have fewer than 0.04. The density of midwives and, to a lesser extent, of nurses also varies considerably among different regions in Senegal.
Relevant changes
Between 2006 and 2008, the introduction of the special contracting system contributed to the successful recruitment of health workers in remote and rural regions and the reopening of health outposts.
Lessons learnt
The introduction of a special contracting system for health workers was a successful approach to reopening health posts in regions with low health workforce density in Senegal. However, the long-term sustainability of such an approach, particularly in fiscal terms, must be considered, as a single policy intervention may not be enough to address the diverse and complex challenges in human resources for health facing different regions of Senegal.
ملخص
المشكلة
تتسبب التفاوتات الإقليمية الهائلة في الموارد البشرية الصحية في السنغال في إضعاف النظام الصحي للبلاد وتضر بصحة السكان.
الأسلوب
في السنوات القليلة المنصرمة، اعتمدت وزارة الصحة إجراءات تسعى لتحسين توظيف وتعيين واستبقاء العاملين الصحيين في المناطق الريفية والمناطق النائية. وإحدى هذه الإجراءات هي إدخال نظام خاص للتعاقد من أجل تعيين العاملين الصحيين.
الوضع المحلي
يتركز العاملون الصحيون في السنغال في مراكز حضرية معينة، ولاسيما في داكار. وبينما يتميز إقليم داكار بوجود 0.2 طبيب لكل ألف من السكان، فإن أقاليم مثل فاتيك، وكوالاك، وكولدا، وماتام لا تتعدى نسبة الأطباء فيها عن 0.04. كما أن كثافة القابلات، وبصورة أقل، كثافة الممرضين تتباين تبايناً كبيراً بين مختلف الأقاليم في السنغال.
التغيرات ذات الصلة
في ما بين العامين 2006 و 2008، ساهم إدخال نظام خاص للتعاقد في نجاح تعيين العاملين الصحيين في الأقاليم النائية والأقاليم الريفية، وإعادة تشغيل النقاط الصحية الخارجية.
الدروس المستفادة
كان إدخال نظام التعاقد الخاص للعاملين الصحيين أسلوباً ناجحاً لإعادة فتح النقاط الصحية الخارجية في الأقاليم ذات الكثافة المنخفضة من العاملين الصحيين في السنغال. غير أنه يجب دراسة ضمان استمرارية مثل هذا الأسلوب على الأمد الطويل، ولاسيما من الناحية المالية، حيث أن المداخلة السياسية الواحدة لا تكفي في التصدي للتحديات المتنوعة والمعقدة في الموارد البشرية الصحية التي تواجه مختلف أقاليم السنغال.
Résumé
Problématique
Des disparités régionales notables dans le déploiement des ressources humaines pour la santé affaiblissent le système de santé du Sénégal et compromettent la santé de sa population.
Démarche
Au cours des dernières années, le Ministère de la santé a adopté des mesures pour améliorer l'affectation, le recrutement et le maintien des agents de santé dans les zones rurales ou reculées. L'une de ces mesures résidait dans l'introduction d'un système de contrat spécial pour le recrutement des agents de santé.
Contexte local
Au Sénégal, les agents de santé se concentrent dans certains centres urbains, notamment autour de Dakar. Alors que la région de Dakar bénéficie de 0,2 médecin pour 1000 habitants, les régions de Fatick, de Kaolack, de Kolda et de Matam disposent de moins de 0,04 médecin pour 1000 habitants. La densité de sages-femmes et, dans une moindre mesure de personnel infirmier, varie aussi considérablement entre les différentes régions sénégalaises.
Modifications pertinentes
Entre 2006 et 2008, l'introduction d'un système spécial de contrat a contribué avec succès au recrutement d'agents de santé dans des régions reculées ou rurales et à la réouverture de postes de santé avancés.
Enseignements tirés
Au Sénégal, la démarche consistant à instaurer un système de contrat spécial pour les agents de santé a été couronnée de succès avec la réouverture de postes de santé dans des régions à faible densité de main-d'œuvre médicale. Cependant, la pérennité de cette démarche sur le long terme, notamment sous l'angle de la fiscalité, doit être examinée, tout comme la possibilité qu'une intervention politique simple ne suffise pas pour répondre aux difficultés diverses et complexes auxquelles sont confrontées les différentes régions du Sénégal dans le domaine des ressources humaines pour la santé.
Resumen
Problema
Las importantes disparidades regionales de recursos humanos en el despliegue de la atención sanitaria en el Senegal debilitan el sistema de salud del país y comprometen la salud de la población.
Enfoque
En los últimos años, el Ministerio de Salud ha adoptado diversas medidas para mejorar el traslado, contratación y permanencia de trabajadores sanitarios en zonas rurales y remotas. Una de ellas fue la implantación de un sistema de contratación especial para captar personal sanitario.
Contexto local
Los trabajadores sanitarios del Senegal se concentran en determinados centros urbanos, sobre todo en Dakar. Mientras que en la región de Dakar hay 0,2 médicos por 1000 habitantes, en las regiones de Fatick, Kaolack, Kolda y Matam hay menos de 0,04. La densidad de parteras, y en menor medida de enfermeras, también difiere considerablemente entre las distintas regiones del Senegal.
Cambios destacables
Entre 2006 y 2008, la implantación del sistema especial de contratación permitió atraer exitosamente a trabajadores sanitarios a las regiones remotas y rurales, y reabrir en ellas puestos de salud periféricos.
Enseñanzas extraídas
La implantación de un sistema especial de contratación de trabajadores sanitarios fue una solución eficaz para reabrir puestos de salud en regiones con baja densidad de personal de salud en el Senegal. Sin embargo, debe estudiarse la sostenibilidad a largo plazo de esa medida, sobre todo en términos financieros, dado que una intervención de política por sí sola puede ser insuficiente para hacer frente a los muchos y complejos retos que deben superar las diferentes regiones del Senegal en materia de recursos humanos para la salud.
Introduction
Like most sub-Saharan African countries, Senegal is experiencing a critical health workforce shortage.1 Health worker shortages, which are more marked in remote and rural areas, weaken health systems and compromises the population's access to health services.2 Various policy interventions can improve health workforce recruitment and retention in rural and remote areas.3–6 Over the past few years, the Ministry of Health of Senegal adopted measures to improve the posting process and the recruitment and retention of health workers in rural and remote areas. Among them was the introduction of an innovative special contracting system for recruiting health workers.
As illustrated in Table 1, health workers in Senegal are concentrated in certain urban centres, particularly the capital, Dakar. According to the ministry of health, the Dakar region has 0.2 physicians per 1000 population, the regions of Fatick, Kaolack, Kolda and Matam have fewer than 0.04. In other words, Dakar has more than 60% of all physicians in the entire country, even though its dwellers represent only 23% of Senegal's total population. The Kaolack and Kolda regions, which have an acute shortage of medical personnel, are also among Senegal's poorest regions.7 The density of midwives and nurses also varies widely in Senegal.
Table 1. Number of physicians, nurses and midwives in the regions of Senegal, 2008.
| Region | Population | Physicians |
Nurses |
Midwives |
Total |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | Per 1 000 population | No. | Per 1 000 population | No. | Per 1 000 population | No. | Per 1 000 population | |||||
| Dakar | 2 564 891 | 524 | 0.20 | 956 | 0.37 | 445 | 0.17 | 1925 | 0.75 | |||
| Diourbel | 1 271 742 | 48 | 0.04 | 178 | 0.14 | 59 | 0.05 | 285 | 0.22 | |||
| Fatick | 675 485 | 16 | 0.02 | 157 | 0.23 | 25 | 0.04 | 198 | 0.29 | |||
| Kaolack | 1 171 428 | 32 | 0.03 | 237 | 0.20 | 40 | 0.03 | 309 | 0.26 | |||
| Kolda | 951 839 | 18 | 0.02 | 160 | 0.17 | 33 | 0.03 | 211 | 0.22 | |||
| Louga | 761 005 | 30 | 0.04 | 129 | 0.17 | 32 | 0.04 | 191 | 0.25 | |||
| Matam | 514 469 | 14 | 0.03 | 144 | 0.28 | 14 | 0.03 | 172 | 0.33 | |||
| Saint-Louis | 812 412 | 33 | 0.04 | 215 | 0.26 | 39 | 0.05 | 287 | 0.35 | |||
| Tambacounda | 708 822 | 31 | 0.04 | 179 | 0.25 | 38 | 0.05 | 248 | 0.35 | |||
| Thies | 1 442 338 | 61 | 0.04 | 303 | 0.21 | 97 | 0.07 | 461 | 0.32 | |||
| Ziguinchor | 468 897 | 25 | 0.05 | 197 | 0.42 | 52 | 0.11 | 274 | 0.58 | |||
| Total | 11 343 328 | 832 | 0.07 | 2855 | 0.25 | 874 | 0.08 | 4561 | 0.40 | |||
Data obtained from Senegal’s Ministry of Health and Medical Prevention, 2008.
Approach
In recent years, the Ministry of Health has spearheaded various measures to improve the posting process and the recruitment and retention of health workers in underserved areas. In collaboration with the World Health Organization, in July 2008 it reviewed the measures adopted to improve health worker deployment in Senegal, particularly the contracting system, as well as other potential measures.
In 2006, the Ministry of Health introduced a special contracting system8 in the context of “Plan Cobra.” This plan was developed to facilitate recruitment to remote and rural areas of Senegal, with a particular focus on the country's border regions. This recruitment process differs from the main, traditional approach whereby the Ministry of Health recruits health workers as civil servants and makes them available for deployment. Under such a scheme, the Ministry of Public Services, in collaboration with the Ministry of Health, establishes a yearly quota of health worker positions for which candidates then apply, but without knowing where they will be deployed if they are selected. While this system is well established for health workers in Senegal, it remains rather inflexible and is often limited in its ability to respond effectively to specific and developing health workforce needs in rural and remote areas. In addition, deployment to such areas is often unpopular among health workers because under this system the length of stay in those regions is uncertain.
The temporary employment contracting system that was launched in 2006 in the context of “Plan Cobra” was designed precisely to be more responsive to changing health workforce needs. Under this system, which is unlike the recruitment system of the Ministry of Public Services, the health worker enters into a contractual arrangement with the Ministry of Health for a specific post in a particular location and for a specific length of time. Like health workers in the civil service, health workers who are contracted are entitled to special benefits when working in remote and rural areas. For instance, housing is provided to contracted nurses who head health outposts. Contracted health workers also benefit from motivation and hardship allowances.
While there was clear recognition that such a measure could lead to the reopening of health posts that had been previously left without health workers, it is less clear whether each region, and particularly those with a low health workforce density, benefited to the same degree from this programme.
Results
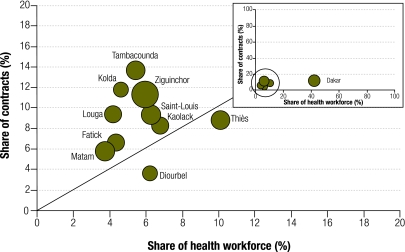
In the context of “Plan Cobra”, 122 health outposts were reopened in Senegal. This contributed substantially to reinforcing health district teams. Overall, 365 contracts were issued between 2006 and 2008, including 59 for physicians, 155 for nurses and 151 for midwives. On average, contracts lasted one year and were renewable. However, the results presented in Fig. 1 show that not all regions benefited from the contracting system to the same degree.
Fig. 1.
Share of contracts compared to share of the health workforce and density, Senegal, 2008
Data obtained from Senegal’s Ministry of Health and Medical Prevention, 2008.
Fig. 1 combines three types of information: (i) the share of the country’s total number of physicians, nurses and midwives working in each region (horizontal axis); (ii) the share of the country’s total number of contracts issued to physicians, nurses and midwives combined in each region between 2006 and 2008 (vertical axis), and (iii) the number of physicians, nurses and midwives combined per 1000 population per region (size of the dots).
Most regions are above the equality line (diagonal line), which indicates that they benefited from the contracting system relatively more than others with a larger share of the national health workforce. This is a positive result, especially for the country's border regions with a low health workforce density, such as Tambacounda and Kolda. These two regions benefited from 14% and 12% of the contracts, respectively, even though each region only had around 5% of the country’s health workforce. Results are also encouraging, albeit to a lesser extent, for border regions such as Ziguinchor, Matam and Saint-Louis.
The situation is quite different, however, for the region of Diourbel, whose health workforce density is also low. Although this region has around 6% of the country’s health workforce, it secured less than 4% of the contracts. It is possible that it was not considered a top priority under “Plan Cobra” because it is not on the border. Finally, the region of Dakar is well below the equality line (Fig. 1), as expected in the light of its health workforce concentration.
Discussion
These results show the positive role that a flexible contracting system can play in improving health workforce recruitment and deployment to rural and remote areas, as well as in redressing the imbalance in health worker distribution between geographical regions. The system was especially effective for drawing workers to remote and rural areas in Senegal’s border regions, which were the main target of “Plan Cobra.” One key factor in facilitating the development of this system was the creation in 2004 of a Human Resources Directorate at the Ministry of Health. This directorate spurred the improvement and strengthening of human resources management coordination in Senegal and spearheaded the campaign for better health worker career management.
Nurses and midwives represented more than 80% of all contracted health professionals between 2006 and 2008, primarily because health outposts in remote and rural areas are usually headed by a nurse or a midwife rather than a physician. Since the region of Dakar has a high concentration of midwives – over 50% of all midwives in Senegal9 – contracting seems to be an interesting and relevant way to strengthen their presence, at least temporarily, in remote and rural regions.
Although these outcomes are encouraging, the contracting system pertains to only a small share of the total health workforce in Senegal and is a source of short-term employment exclusively. Expanding the scheme by increasing the number of contracts and their length would require significant considerations of the fiscal sustainability of such an approach. The case of Diourbel also illustrates the need for a coherent policy at the national level to enable an equitable set of policy interventions across the different regions of Senegal (Box 1).
Box 1. Summary of the main lessons learnt.
• Introducing a special contracting system for health workers can be a successful way to reopen unstaffed health posts in regions with low health workforce density and to redress the uneven distribution of workers in different health professions.
• Since the system offers contracts for short-term employment only, policy-makers must carefully consider the sustainability of this approach, particularly from a financial perspective.
• Including this system in a bundled policy intervention to improve health workforce recruitment and retention in rural and remote areas can be more effective in addressing the challenges facing different regions in terms of human resources for health.
Although its overall impact has been positive, the contracting system is not enough to redress geographical health worker imbalances in Senegal, particularly because contracts are only for short-term employment. Besides, the number of additional physicians, nurses and midwives required to overcome the critical health workforce shortage in Senegal and reach a density of 2.28 physicians, nurses and midwives per 1000 population, as recommended in The world health report 2006, is well beyond the capacity of the current contracting system.1,9
In addition to contracting, other strategies to increase staff salaries were initiated in Senegal, together with measures to increase the number of trained health workers, especially by increasing the number of students from regions other than Dakar. In several countries, similar efforts to train more students from remote and rural areas have met with some success.10 Senegal recently adopted this approach, along with decentralization of public schools for paramedics. Training centres were subsequently opened in Kaolack, Saint-Louis, Tambacounda, Thiès, Kolda and Ziguinchor, and this allowed for more local training and recruitment of health workers in various regions of the country.9 Measures have also been adopted to increase financial support for students in remote and rural areas. For instance, grants are now available for seventh-year medical students wishing to do internships in such areas. Unfortunately, few medical students actually take advantage of this opportunity, despite its potential to raise their awareness of rural health issues, and measures to highlight the benefits of internships in remote and rural areas are under discussion.
Senegal is genuinely capable of increasing the number of health workers in remote and rural areas, thanks to existing measures for health workforce management and to its training capacity. Yet adopting additional measures and strategies would complement and strengthen the effect of those that have already been adopted, such as contracting, and would further improve health worker recruitment and retention in remote and rural areas. Such measures might include the development of a more equitable and transparent health workforce posting system; wider dissemination of information on health workforce management; task shifting; the training of individuals more likely to work in remote and rural areas and, finally, a more intersectoral approach.
Acknowledgements
We thank Laura Stormont and Ben Fouquet for editing and for their valuable comments and suggestions. We would also like to thank Ibrahima Souka Ndella Diouf and Mamadou Coulibaly for their support during the field trip and for data collection.
Competing interests:
None declared.
References
- 1.World Health Organization. The world health report: working together for health. Geneva: WHO; 2006. [Google Scholar]
- 2.Anand S, Bärnighausen T. Human resources and health outcomes: cross-country econometric study. Lancet. 2004;364:1603–9. doi: 10.1016/S0140-6736(04)17313-3. [DOI] [PubMed] [Google Scholar]
- 3.Lehmann U, Dieleman M, Martineau T. Staffing remote rural areas in middle- and low-income countries: a literature review of attraction and retention. BMC Health Serv Res. 2008;8:19. doi: 10.1186/1472-6963-8-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilson NW, Couper ID, De Vries E, Reid S, Fish T, Marais BJ. A critical review of interventions to redress the inequitable distribution of healthcare professionals to rural and remote areas. Rural Remote Health. 2009;9:1060. [PubMed] [Google Scholar]
- 5.Grobler L, Marais BJ, Mabunda SA, Marindi PN, Reuter H, Volmink J. Interventions for increasing the proportion of health professionals practising in rural and other underserved areas. Cochrane Database Syst Rev. 2009;1:CD005314. doi: 10.1002/14651858.CD005314.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Iipinge S, Dambisya YM, Loewenson R, Chimbari M, Ndetei D, Munga M et al. Policies and incentives for health worker retention in east and southern Africa: learning from country research (Discussion paper 78). Harare: University of Namibia, Training and Research Support Centre, University of Limpopo, EQUINET, ECSA-HC; 2009. Available from: www.equinetafrica.org/bibl/docs/Diss78synthesisHRH09.pdf [accessed 13 March 2010].
- 7.Senegal, Ministry of Economy and Finance. Poverty reduction strategic paper 2006-2010. Dakar: MEF; 2006.
- 8.Perrot J, Carrin G, Evans D. Application of contracting in health systems: key messages (Technical Briefs for Policy Makers Number 4). Geneva: World Health Organization; 2005. Available from: www.who.int/contracting/issues/pb_number_05_04.pdf [accessed 13 March 2010].
- 9.Zurn P, Codjia L, Sall FL. La fidélisation des personnels de santé dans les zones difficiles au Sénégal, accroître l'accès aux personnels de santé dans les zones rurales ou reculées: etude de cas No 1 Geneva: World Health Organization; 2010. French. Available from: http://www.who.int/hrh/resources/case_senegal/fr/index.html [accessed 13 March 2010].
- 10.Fournier MA, Contandriopoulos AP, Diene CP, Trottier LH. Mesures d'attraction et de rétention des médecins en région éloignée: politiques adoptées dans les provinces canadiennes et dans certains pays et leçons à tirer pour le Québec. Montreal: Secteur Santé Publique, Faculté de Médecine, Université de Montréal; 2004. French. Available from: www.gris.umontreal.ca/rapportpdf/R04-08.pdf [accessed 13 March 2010].