Abstract
Compulsory service programmes have been used worldwide as a way to deploy and retain a professional health workforce within countries. Other names for these programmes include ”obligatory”, ”mandatory”, ”required” and ”requisite.” All these different programme names refer to a country’s law or policy that governs the mandatory deployment and retention of a heath worker in the underserved and/or rural areas of the country for a certain period of time. This study identified three different types of compulsory service programmes in 70 countries. These programmes are all governed by some type of regulation, ranging from a parliamentary law to a policy within the ministry of health. Depending on the country, doctors, nurses, midwives and all types of professional allied health workers are required to participate in the programme. Some of the compliance-enforcement measures include withholding full registration until obligations are completed, withholding degree and salary, or imposing large fines. This paper aims to explain these programmes more clearly, to identify countries that have or had such programmes, to develop a typology for the different kinds and to discuss the programmes in the light of important issues that are related to policy concepts and implementation. As governments consider the cost of investment in health professionals’ education, the loss of health professionals to emigration and the lack of health workers in many geographic areas, they are using compulsory service requirements as a way to deploy and retain the health workforce.
ملخص
استُخدِمت برامج الخدمة الإلزامية في كافة بقاع العالم كوسيلة لتوزيع واستبقاء المهنيين الصحيين داخل البلدان. وقد أطلقت أسماء أخرى على هذه البرامج منها البرامج "الإجبارية"، "الواجبة"، "الحتمية"، "الوجوبية". وكل هذه الأسماء المختلفة للبرامج تعود إلى القوانين أو السياسات القطرية التي تحكم التوزيع الإلزامي واستبقاء العاملين الصحيين في المناطق المحرومة من الخدمات أو المناطق الريفية لفترة زمنية محددة. وحددت هذه الدراسة ثلاثة أنماط متباينة من برامج الخدمة الإلزامية في 70 بلداً. وهي برامج تُحكَم جميعها ببعض أنماط التنظيم يمتد من القوانين البرلمانية إلى السياسات الخاصة بوزارة الصحة. ووفقا لنظام البلد، يقتضي على الأطباء، والممرضين، والقابلات، ومختلف العاملين الصحيين والمهنيين المساعدين، المشاركة في هذا البرنامج.
وتشمل بعض الإجراءات الخاصة بتفعيل الامتثال لهذا البرنامج عدم السماح باستكمال التسجيل قبل استيفاء الالتزامات الواجبة، واحتجاز الدرجة والراتب أو فرض غرامات كبيرة. وتهدف هذه الورقة إلى شرح هذه البرامج بوضوح أكثر، وتحديد البلدان التي كانت تستخدمها أو لا تزال تعمل بها وذلك في ضوء القضايا الهامة المتعلقة بمفاهيم السياسات وتنفيذها. ولما كانت الحكومات تنظر بعين الاعتبار في تكلفة استثمار تعليم المهنيين الصحيين، ثم فقدهم بعد ذلك بسبب الهجرة، وما ينجم عن ذلك من نقص في العاملين الصحيين في العديد من المناطق الجغرافية، فإن هذه الحكومات تعمل على فرض اشتراطات الخدمة الإلزامية كوسيلة لتوزيع واستبقاء القوى العاملة الصحية.
Résumé
Les programmes de service obligatoire sont utilisés dans le monde entier comme moyen de déployer et de retenir une main d'œuvre médicale professionnelle dans les pays. On donne à ces programmes des noms divers, qui font référence à une loi ou à une politique du pays considéré qui régit le déploiement et le maintien obligatoires, sur une certaine durée, des agents de santé dans les zones mal desservies et/ou rurales de ce pays. La présente étude identifie trois types différents de programmes de service obligatoire parmi 70 pays. Ces programmes sont régis par certains types de règles, qui vont de la loi parlementaire à la politique ministérielle. Selon le pays, les médecins, le personnel infirmier, les sages-femmes ou tous les types apparentés de professionnels de santé sont obligés de participer à ces programmes. Parmi les mesures pour les faire appliquer, figurent l'absence d'enregistrement complet tant que l'agent ne s'est pas acquitté de ses obligations, la suspension d'avancement ou de salaire ou l'application de lourdes amendes. L'objectif de l'article est de présenter plus clairement ces programmes, d'identifier les pays qui en disposent ou en disposaient, de développer une typologie qui recense leurs différentes formes et de les examiner à la lumière des problèmes importants de conception et de mise en œuvre des politiques. Au vu des investissements consentis dans la formation des professionnels de santé, des pertes de personnel de santé dues à l'émigration et du manque d'agents de santé dans de nombreuses zones géographiques, les gouvernements ont recours au service obligatoire comme moyen de déployer et de retenir la main-d'œuvre médicale.
Resumen
Los programas de servicio obligatorio son una medida utilizada en todo el mundo para distribuir y conservar a los profesionales sanitarios en los países. Bajo distintas denominaciones, todos esos programas hacen referencia a las leyes o políticas de un país que rigen el despliegue y permanencia obligatorios de trabajadores de la salud en zonas subatendidas y/o rurales de su territorio durante un determinado periodo. En este estudio se identificaron tres tipos de programas de servicio obligatorio en 70 países. Todos ellos están sujetos a alguna forma de regulación, desde una ley parlamentaria hasta una política del ministerio de salud. Dependiendo del país, médicos, enfermeras, parteras y todo tipo de auxiliares sanitarios profesionales están obligados a participar en el programa. Como medidas de imposición de esa obligatoriedad cabe citar la suspensión de la colegiación plena hasta haber cumplido el servicio, la retención del título y del sueldo, o el pago de elevadas multas. Este trabajo tiene por objeto explicar más claramente esos programas, determinar qué países los han aplicado o los están aplicando, elaborar una tipología de esos programas, y analizarlos a la luz de algunas cuestiones importantes relacionadas con aspectos normativos y con la aplicación de las políticas. Considerando el costo de las inversiones en formación de los profesionales de la salud, la pérdida de profesionales que emigran y la falta de personal sanitario que sufren muchas zonas geográficas, los gobiernos recurren a formas de servicio obligatorio como alternativa para desplegar y conservar al personal sanitario.
Introduction
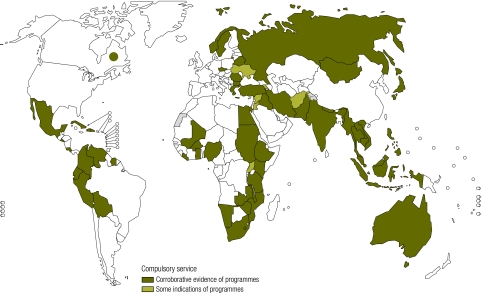
Compulsory service programmes have existed since the early 20th century. Different names have been given to such programmes, including “obligatory”, “mandatory”, “requisite” and “coercive” programmes. In this paper, we will use the term “compulsory service” to describe such programmes. Literature shows evidence of programmes in the Soviet Union in 1920,1–3 in Mexico in 1936,1 and in Norway in 1954. In the 1970s, there was an acceleration of new programmes worldwide. No one reason is evident for this rapid growth, though this decade witnessed an overall increase in attention paid to inequities in health provision (as evidenced by the 1978 adoption of the Declaration of Alma-Ata), as well as increased worldwide interest in socialist ideologies, especially the belief in national service and pride. Over the years different countries created and implemented compulsory service programmes, one of the most recent ones was started in Ghana in 2009. Fig. 1 shows more than 70 countries with current and past compulsory service programmes. The map shows countries where this study found corroborative evidence of compulsory service programmes as well as countries where it found some indications, but no corroborative evidence.
Fig. 1.
Countries with past and current compulsory service programmes
Methods
Robust information on the specifics of compulsory service programmes is not readily available. We did a country-by-country inventory of all Member States of the World Health Organization (WHO). We did a literature search, formal interviews, as well as informal questioning of relevant informants to identify countries with compulsory service programmes and their details in each of the WHO regions.
A literature review was conducted of internet databases (Box 1) using the following terms: bond doctor, bond scheme, bonding, bonding medical, compulsory medical, compulsory medical service, conditional medical, conditional scholarship, mandate doctor, mandate medical, mandate nurse, mandate rural, medicatura rural, obligatory medical, obligatory service, coercive service, rural health service, rurales, social doctor, social medical, social nurse, [COUNTRY NAME] health human resources, [COUNTRY NAME] health human resources rural. A “snowballing” technique was employed, whereby references were culled from each document for review. All searches were conducted in English, though laws published in French, Portuguese or Spanish were reviewed after translation using Google Translator. Documents found included peer-reviewed articles and grey literature, historical and journalistic accounts, policies and laws. Documents were excluded from review if they did not specifically mention one or more compulsory service scheme.
Box 1. Databases used.
PubMed, Academic Search Premier, Scopus, SPORTDiscus, PsycINFO, CINAHL, Global Health, LexisNexis, Google, Google Scholar, Yahoo, NCBI Bookshelf, REHABDATA, AMED, ALADIN, MDConsult, LEXIS-NEXIS Academic Universe, Proquest Research Library Plus, Access Surgery, POPLINE, MEDLINE, images MD, Lexi-Comp, R2 Library, ebrary, First Consult, Cochrane Library, National Guideline Clearinghouse, Psychiatry Online, TOXNET, ABI/Inform Complete Plus, GPO Access, Natural Medicines, Web of Science, CINAHL, PAIS, BMJ Clinical Evidence, Global Health, Himmelfarb (GWU) library’s card catalogue, Wiley Encyclopedia of Clinical Trials, Books @ Ovid, Access Medicine, eMedicine
To better determine the different requirements, interviews with key government officials from nine countries were conducted. A questionnaire was developed after a preliminary review of literature on compulsory service. This questionnaire was pretested in consultations with health workforce experts from five countries that provided feedback. The questionnaire was modified accordingly. Officials completing the instrument either via e-mail or telephone represented Australia, Ghana, Haiti, India (Tamil Nadu, Meghalaya), Mozambique, Nigeria, Norway, Peru and South Africa. Interview topics included: (i) history, (ii) description, (iii) administration and finance, (iv) outcomes, (v) problems/challenges, and (vi) advice to others regarding compulsory service programme implementation.
Classification of programmes
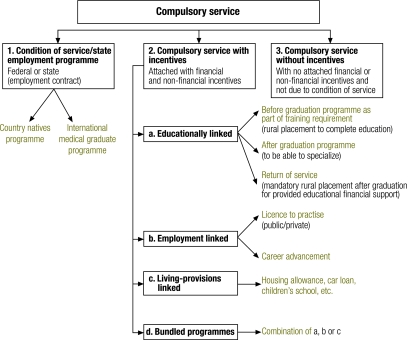
Based on the literature review and key informant interviews, a tripartite classification system for compulsory service programmes was developed (Fig. 2). The types are: (i) condition of service/state employment programme, (ii) compulsory service with incentives, and (iii) compulsory service without incentives.
Fig. 2.
Classification of compulsory service programmes
Condition of service
These programmes require health professionals to work for the government. There is little or no opportunity for private or nongovernmental practice. Government employment contracts give the employer (federal and state ministries of health) the authority to assign health employees in any part of the country, based on need for a specified number of years. The Islamic Republic of Iran’s behvarz, a type of community health worker, work within that country’s health system at rural health clinics as assigned by the government for four years after the completion of their training.4 Cuba’s doctors serve the government both within Cuba and internationally.5 In Myanmar, personnel may choose to spend an entire career in a condition of service system.6 In Australia, all international medical graduates must spend ten years working in a “district of workforce shortage” as assigned by the Rural Workforce Agencies.
Compulsory service with incentives
Compulsory service with incentives does not rely on governmental mandate but, rather, is associated with incentives to serve in designated areas for specified time periods. Governmental regulations govern the implementation and enforcement of these programmes. Four categories of compulsory service with incentives were identified; examples are presented in Table 1.
Table 1. Examples of countries that have compulsory service programmes with incentives.
| Country | Cadre | Years of service | “Buy out” | Incentives to encourage rural posting or retention |
|---|---|---|---|---|
| Australia | Doctor | 6 | No | Scholarship (undergrad), licence to practise (Medicare provider number) |
| Bolivia (Pluri-national State of) | Doctor | 1 | Yes | Graded salary, licence to practise |
| Ecuador | Doctor, dentist, nurse | 1 | Graded salary, licence to practise, preference for PG specialization, career advancement | |
| Ethiopia | Doctor | 2–4 | Yes | Graded salary, preference for PG specialization, degree, textbooks, computer, variable length of service |
| Ghana | Doctor | 1–3 | Yes a | Preference for PG specialization, PG scholarship |
| Nurse | 3 | Preference for PG placement | ||
| Technician | 3 | Preference for PG placement | ||
| India (Meghalaya) | Doctor | 3 | No | Sponsorship to undergraduate training, some undergraduate scholarships, housing |
| India (Orissa) | Doctor | 1 | No | Preference for PG specialization |
| India (Tamil Nadu) | Doctor | 3 | Yesb | Preference for PG specialization, increased preference for every 2 years served in tribal areas. |
| Specialist | 5 | Yesb | Return of service for PG specialization | |
| Indonesia | Doctor | < 1–5 | Graded salary, preference for PG specialization, career advancement | |
| Kenya | Doctor, nurse | 3 | Licence to practise, preference for PG specialization, PG scholarship, career advancement, various according to locality | |
| Lesotho | Doctor | 1/year trained | No | Return of service for training provided overseas, graded salary, housing |
| Malawi | Nurse tutor | 2 | Scholarship (undergraduate/PG), housing, medical assistance | |
| Mozambique | All | 2 | Housing, career advancement | |
| Mongolia | Doctor | 2 | Degree | |
| Myanmar | Doctor, nurse | 3 | No | Graded salary, licence to practise, housing, preference for PG specialization |
| Namibia | Doctor | 2 | Graded salary, preference for PG scholarships | |
| Nepal | Doctor | Licence to practise | ||
| Nigeria | All | 1 | No | Licence to practise, preference for PG specialization, career advancement |
| Norway | Many | 1.5 | No | Licence to practise |
| Pakistan | Doctor | 1 | Preference for PG training after 3 years in rural area | |
| Peru | Doctor | 1 | Yesc | Licence to practise in public sector, preference for PG specialization, PG scholarship, career advancement |
| South Africa | Doctor, dentist, pharmacist | 1 | Yes | Graded salary, licence to practise in private sector |
| Thailand | Doctor | 3 | Yes | Graded salary, preference for PG specialization, housing, career advancement |
| Turkey | 2–4 | Graded salary, variable length of service | ||
| Viet Nam | Doctor | 5 | Degree | |
| Zambia | Doctor | 3 | Graded salary, housing, child education, loans, preference for PG specialization, PG scholarship | |
| Zimbabwe | Doctor | 3 | Licence to practise, preference for PG specialization |
PG, postgraduate
a Ghana’s system of withholding pay cheques from non-compliant personnel means that the equivalent to a “buy out” would be that the health worker accepts no salary.
b Enforced through fine of 1 million rupees (approx. US$ 21 000) which is only affordable to some.
c Health workers may opt to spend their entire career outside Peru’s public sector, such as by emigrating after graduation.
Educational
Three types of education-incentive-linked compulsory service programmes have been identified: In the first type, students are required to complete a rural placement during the course of their training to complete their education. If compulsory service requirement is not met, the diploma/degree will not be given. Pharmacy students in New Zealand are required to perform a rural “externship” during training.7
In the second type, the graduate is required to serve in an underserved region of the country as a prerequisite for entering a postgraduate/specialization programme. Countries requiring this type of service include Mongolia8 and Viet Nam.9
In the third type, there is a return of service programme where rural placement is required after graduation, often for one year for each year that educational financial support was provided. These systems are found in Australia (K Webber, personal communication), Lesotho7 and Japan.10
Employment
Two employment-linked models exist; the first, as a requirement for attaining a licence to practise (publicly or privately) and the second, as a prerequisite for career advancement. For example, Ecuador,1 Myanmar11 and South Africa12 allow medical personnel to practise privately only after they complete a period of compulsory service. Peru has employment-linked compulsory service programmes which are associated with career advancement.
Living provisions-linked
Some countries provide incentives that are family- and resource-linked, such as housing in Kenya13 and Mozambique (J Ferro, Dean Catholic University, Beira, personal communication), and lower car loan rates and children’s scholarships in Zambia,14,15 to encourage the graduates to stay in a remote area after the compulsory service period ends.
Bundled
A few countries like Ecuador and Thailand have programmes that combine incentives for education, employment and living provisions. Ecuador’s Medicatura Rural system requires one year of service before doctors, nurses and dentists gain their licence to practise.1 Rurales are paid variable salaries based upon remoteness of assignments and they receive housing in posted locations. In Thailand, public medical school graduates must perform compulsory service for three years. They may supplement their public salaries by concurrently practising privately, or they can receive US$ 250 per month if they agree only to work in the public system.16 Additional incentives for rural practice include: higher pay for more rural placements, greater access to postgraduate training, logistic and housing support, career enhancement and improved health infrastructure.
Compulsory service without incentives
The third type of compulsory service programme found is one that does not offer any incentives nor relate to condition of service. These programmes require the graduate to work in an underserved setting with no attached incentive, usually for one year. Some examples are found in India in Kerala4 and Assam (T Sundararaman, personal communication), Iraq,17 Malaysia,18 Mexico,1 the former Soviet Union (historic)1 and Venezuela.5
Results
While we found more than 70 countries (and parts of Canada,14 India19 and Japan)10 with some type of compulsory service programme, exact dates of initiation for some programmes were unclear. These programmes were started for several reasons. Most programmes where the designing entity is known were designed by the ministry of health or a legislative body with the involvement of local government agencies (ministry of health: 14; federal body: 6; state bodies: 2; private entity: 2; unknown: 48). Where a method is known, the most common means (64%) of enforcing the requirement is by withholding the certification needed to practise. Some countries enforce graduates to pay back the government money spent on education. For example, in Meghalaya and Tamil Nadu States in India, graduates who do not complete their compulsory service must pay a fine of 1 million Rupees (about US$ 21 000). The cost of the compulsory programme varies due to the size of the service areas, population of the countries and economic status of the country. Costs range from US$ 100 000 in Haiti to US$ 10 million per year in Australia. National taxes are the most common means of financing the programmes.
Outcomes
Numerous programmes indicated that they had not measured outcomes or that they were just starting to measure outcomes and the results were not yet available. The number of health professionals who stay in the rural areas after their compulsory service is over was not clear for most countries (6 of 9).
Norway’s administrators measure a variety of factors related to the types of individuals who stay in rural areas after the requirement is complete. These factors included: rural/urban upbringing, age, family composition and gender. Norway estimated that 20% stay in rural areas, and was in the process of analysing these data at the time of writing this paper. Nigeria anecdotally stated that people do not stay in the rural areas after completing the requirement. In Peru, the health professionals are not allowed to stay in the rural area after the programme has ended. If they do remain, they are often paid less than they received while fulfilling their compulsory service requirement.
Impact
In Puerto Rico before compulsory service, 16 of 78 municipalities had no physician. After implementation, all 78 had at least one doctor.20 Incentive-linked compulsory service in Indonesia increased new doctors’ willingness to work in remote areas.21 Turkey’s programme was effective at mitigating staffing discordance.22 In South Africa, better staffing levels in rural hospitals, shorter patient wait times and more frequent visits to outlying clinics by health workers are reported.23 In Thailand it helped to narrow the disparities in urban/rural health worker density.24
Challenges from professional groups
Many health professionals object to compulsory service programmes.1,6,9,25–27 Reasons given include: cost, utility and sustainability of programmes;25 poor rural facilities;25 lack of transportation; and inadequate clean water, electricity, equipment and medications, making performance of some skills learnt in medical schools impossible.1 In Kerala, India, a strike protesting against a three-year compulsory service requirement influenced the government to reduce the service period to one year.3 Professionals’ opposition can be minimized if programmes are planned in consultation with health professionals.26
Management
Success or failure of these programmes largely depends on supportiveness in the broader health system.23 Governments must clearly state what they expect from compulsory service personnel. While the Ecuadoran government considers participants to be qualified doctors, doctors view compulsory service as part of their education, which results in disillusionment when they perform their service without supervision.1 In South Africa, vague guidelines for compulsory service doctors resulted in uneven utilization by clinics and hospitals.13 Several authors advise that compulsory service should be supplemented by a support system and incentives.2,15,25,27 Programmes that provide reasonable benefits and support may be more costly than compulsory service without incentives, but the likelihood of effective service will be maximized. For instance, in Zambia, before its incentive-based health workforce retention scheme was implemented, many doctors assigned to rural areas resigned from government service to avoid serving in rural posts (T Sundararaman, personal communication).
Turnover of health workers
Doctors’ unwillingness to continue in their assigned posts negatively impacts continuity of care2 and may mean that many workers in underserved areas are inexperienced. Managers in South Africa believe the inexperience of doctors sent to rural areas resulted in slower, poorer care for some patients.2 Thirty-four per cent of compulsory service doctors intended to leave South Africa after completing their obligation, and an additional 13% planned to go into private practice.13 Indonesia offers specialist training as an incentive to serve in remote areas, but this incentive may speed turnover as personnel uninterested in general practice perform their service in rural regions where they are unlikely to return as specialists.28
Community support
Studies regarding community support or disapproval regarding compulsory service programmes are very scant. Community support is a key factor both for making personnel feel welcome in their posts and allowing them to practise their professions. In some parts of Ecuador, compulsory service doctors were interviewed on this subject. One stated: “There were no problems (of adjustment to the post site), because the leaders of the community were organized and helped.”1 In South Africa, “communities valued the services of the compulsory service doctors, as they ‘make a difference’.”29
Human rights
An inherent conundrum of a compulsory service system is the “need to respect the human rights of the professionals [to migrate], at the same time recognizing that the poor countries also have a right to lay claims to the investment they made in training them.”30 It is also argued that freedom of movement, in this case of health workers, is a human right.31
Discussion
The full extent of compulsory service programmes’ prevalence, requirements, effectiveness and long-term impact has never been studied. Two important areas warrant further discussion – policy concepts and policy implementation.
Policy concepts
Compulsory service programmes are an instrument of social justice, an exercise in health equity, in that they enable governments to direct or augment health services to geographical areas that are not well served and in communities that are not favoured by market forces and health worker preferences. The premise that underlies most compulsory service programmes (except condition of service programmes) is that government-sponsored education of a health professional provides that individual with a critical skillset valuable to all members of society. Since it has been given to the individual at little or no cost, the individual therefore has incurred a debt to the country and a period of clinical pay-back is warranted. Most often, this translates into a requirement for service provision in an area of national need, usually defined as “the periphery”, “rural areas” or “underserved populations.”
There are multiple challenges in designing and managing an effective compulsory service programme and high turnover is singled out as a common “weakness.” This criticism bears further examination. The areas to which doctors and other health professionals are sent are typically rural, underdeveloped and deficient in both personal/family amenities and clinical support. These are settings that do not attract doctors or other health professionals under current circumstances. Turnover is very much a given. In the view of many policy-makers and compulsory service programme strategists, service with predictable turnover is far preferable to no service at all. This is hardly a shortcoming of the programmes; rather, it represents a practical adaptation for the provision of health services in the challenging circumstances in rural areas of many countries.
Finding proof of efficacy in clinical outcomes in these programmes is not easily done but, in fairness, evidence of direct physician impact on population health outcomes is not easily proven in health services research in general. The impact of compulsory service is much more easily identified by process measures that track the presence or augmentation of health services. For instance, Mozambique is able to declare this year for the first time that, due to its national service programme, all 148 districts in the country now have at least one physician.20 This is a public health achievement for the country as a whole and for the compulsory service programme in particular.
Some commentators express concerns about compulsory service programmes based on the compulsory nature of the programmes themselves and argue that it is contrary to the rights of the individual health worker. These concerns, however, conflate human rights and the personal preferences of health workers who have received the benefit of state-sponsored education. A compulsory service requirement which is clearly stated at the time of entry into health professions training can hardly be considered an abridgement of human rights. When a country devotes national wealth to establishing health science schools and enrols students in the expectation that they will use their education to better the nation’s health, there is a reasonable presumption that the students will fulfil their commitment by providing service to largely underserved people (which on its own is a strategy that is very much in keeping with basic principles of human rights).
Policy implementation
The spectrum of compulsory service programmes reviewed in this paper suggests several principles that are likely to increase the effectiveness and success of compulsory service programmes.
Good planning
Compulsory service programmes are complex in that they involve the placement of individuals in communities over a period of time. The management of potential problems associated with assignment, placement and fulfilment all depend upon commitments and relationships that can fail. Therefore, prospective and proactive planning are essential predicates of subsequent success. The individuals should be trained in procedures relevant to working in a rural area.
Transparency and clarity
Closely associated with planning is transparency – a clear understanding of the rationale and requirements for any compulsory service programme. Health professionals, who are asked to spend years of service in locations they might not otherwise have chosen, need to have a clear understanding of the rationale for their assignment and a clear set of expectations concerning the many issues that may arise during the compulsory service period. Clarity of intent and consistency of implementation of the assignment process will increase the likelihood of an effective programme. The nature of the assignment process, including the rationale for the assignment, its duration, whether or not the individual has a voice in the assignment, and the role of the host community in the selection process, is critical. Norway’s system is a good example of this clarity. Each graduate is assigned a random number. The numbers are called in order and the graduate has six hours in which to choose a post location from those still available. Except under extreme circumstances (i.e. severe illness in the immediate family), no swapping of assigned locations is permitted (K Straume, personal communication). This system allows each graduate to know his/her chance of gaining a choice post location.
Support
The nature of support provided to compulsory service personnel during assignment plays a major role in the success of the placement. An important aspect is the benefits provided to the health worker, including pay, housing, continuing education and clinical backup or supervision. Programmes that send doctors to remote areas with little support may be delivering on a political promise to place doctors in the periphery, but the absence of assistance is likely to result in a minimally effective programme where clinicians may abandon their site or function ineffectively.
Conclusion
No rigorous study has systematically compared rural and remote workforce disparities in countries with compulsory service to those in countries that don't have such programmes. Compulsory service programmes are a mechanism for staffing and reinforcing the health workforce especially in areas where access to primary and essential heath-care services and systems is weak. Compulsory service may not be able to provide a permanent answer to capacity development, nor guarantee the development of a permanent workforce for underserved communities but, if well planned with incentives, can contribute to a nation’s plan for health workforce capacity development, distribution and retention in rural and underserved areas.
Acknowledgements
We thank Jean-Marc Braichet, Carmen Dolea and Manuel Dayrit from the World Health Organization; Okey Akpala, J Koku Awoonor-Williams, Luis Huicho, Percy Mahlati, Karin Straume, Thiagarajan Sundararaman, Kim Webber and Lambert Wesler.
Funding:
The Health Workforce Migration and Retention, Human Resources for Health, Health Systems and Services at the World Health Organization provided financial support to conduct this study under the work done on “Policy recommendations and guidelines on increasing access to health workers in remote and rural areas through improved retention.”
Competing interests:
None declared.
References
- 1.Cavender A, Albán M. Compulsory medical service in Ecuador: the physician’s perspective. Soc Sci Med. 1998;47:1937–46. doi: 10.1016/S0277-9536(98)00335-9. [DOI] [PubMed] [Google Scholar]
- 2.Omole O, Marincowitz G. Perceptions of hospital managers regarding the impact of doctors’ community service. South African Fam Pract. 2005;47:55–9. [Google Scholar]
- 3.Bärnighausen T, Bloom DE. Designing financial-incentive programmes for return of medical service in underserved areas: seven management functions. Hum Resour Health. 2009;7:52. doi: 10.1186/1478-4491-7-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aghajanian A, Mehryar AH, Ahmadnia S, Kazemipour S. Impact of rural health development programme in the Islamic Republic of Iran on rural-urban disparities in health indicators. East Mediterr Health J. 2007;13:1466–75. doi: 10.26719/2007.13.6.1466. [DOI] [PubMed] [Google Scholar]
- 5.Maybarduk P. A peoples’ health system: Venezuela works to bring healthcare to the excluded. Multinational Monitor 2004. Available from: http://liberationhealth.org/documents/Venezuelaapeopleshealthsystem.pdf [accessed 4 March 2010].
- 6.Myanmar Ministry of Health. Brief country report on HRH development activities. In: 3rd AAAH Conference, Colombo, Sri Lanka, 12-15October2008 [Google Scholar]
- 7.Capstick S, Beresford R, Gray A. Rural pharmacy in New Zealand: effects of a compulsory externship on student perspectives and implications for workforce shortage. Aust J Rural Health. 2008;16:150–5. doi: 10.1111/j.1440-1584.2008.00965.x. [DOI] [PubMed] [Google Scholar]
- 8.Yang D. Annual review of HRH situation in Asia-Pacific Region 2006-07. In: Presentation made to Health Human Resources Development Center, Ministry of Health, 13October2008, Beijing, People’s Republic of China. [Google Scholar]
- 9.Ministry of Health. Viet Nam. Human resources for health activities in Vietnam. In: 3rd AAAH Conference, Colombo, Sri Lanka, 12-15October2008 Available from: http://www.aaahrh.org/3rd_conf_2008/country%20reports/country_report_Vietnam.pdf [accessed 4 March 2010].
- 10.Matsumoto M, Inoue K, Kajii E. Long-term effect of the home prefecture recruiting scheme of Jichi Medical University, Japan. Rural Remote Health. 2008;8:1–15. [PubMed] [Google Scholar]
- 11.Ministry of Health. Myanmar. Brief country report on HRH development activities. In: 3rd AAAH Conference, Colombo, Sri Lanka, 12-15October2008 [Google Scholar]
- 12.Reid SJ. Compulsory community service for doctors in South Africa – an evaluation of the first year. S Afr Med J. 2001;91:329–36. [PubMed] [Google Scholar]
- 13.Ndetei D, Khasakhala L, Omolo J. Incentives for health worker retention in Kenya: an assessment of current practice (discussion paper 62). Harare: University of Limpopo; 2008.
- 14.Simoens S. Experiences of Organization for Economic Cooperation and Development countries with recruiting and retaining physicians in rural areas. Aust J Rural Health. 2004;12:104–11. doi: 10.1111/j.1440-1854.2004.00569.x. [DOI] [PubMed] [Google Scholar]
- 15.Koot J, Martineau T. Mid-term review: Zambian Health Workers Retention Scheme (ZHWRS) 2003-2004. Chapel Hill: HRH Global Resource Center; 2005. Available from: http://www.hrhresourcecenter.org/hosted_docompulsory service/Zambian_Health_Workers_Retention_Scheme.pdf [accessed 4 March 2010].
- 16.Wilbulpolpasert S, Pengpaibon P. Integrated strategies to tackle the inequitable distribution of doctors in Thailand: four decades of experience. London: BioMed Central; 2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Myers W, Behringer B, Olsen M. Rural health in Iraqi Kurdistan [letters]. J Rural Health. 2005;21:1–2. doi: 10.1111/j.1748-0361.2005.tb00055.x. [DOI] [PubMed] [Google Scholar]
- 18.Mohd M. The role of the Malaysian Medical Council in medical education. Med J Malaysia. 2005;60(Supp. D):28–33. [PubMed] [Google Scholar]
- 19.State of Kerala Government Order 263/04. Available from: http://kerala.gov.in/dept_health/health&fly.pdf [accessed 4 March 2010].
- 20.Ramírez de Arellano AB. A health “draft”: compulsory health service in Puerto Rico. J Public Health Policy. 1981;2:70–4. doi: 10.2307/3342100. [DOI] [PubMed] [Google Scholar]
- 21.Lehmann U, Dieleman M, Martineau T. Staffing remote rural areas in middle- and low-income countries: a literature review of attraction and retention. BMC Health Serv Res. 2008;8:19. doi: 10.1186/1472-6963-8-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Erus B, Bilir A. Obligatory service requirement and physician distribution in Turkey. Eur J Public Health. 2007;17(supp. 2):175. [Google Scholar]
- 23.Reid S. Community service for health professionals. South African Health Review 2003. [Google Scholar]
- 24.Wongwatcharapaiboon P, Sirikanokwilai N, Pengpaiboon P. The 1997 massive resignation of contracted new medical graduates from the Thai Ministry of Public Health: what reasons behind? Human Resources for Health Development Journal. 1999;3:147–56. [Google Scholar]
- 25.Liaw ST, McGrath B, Jones G, Russell U, Bourke L, Hsu-Hage B. A compulsory experiential and inter-professional rural health subject for undergraduate students. Rural Remote Health. 2005;5:460. [PubMed] [Google Scholar]
- 26.Homedes N, Ugalde A. Human resources: the Cinderella of health sector reform in Latin America. Hum Resour Health. 2005;3:1. doi: 10.1186/1478-4491-3-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ferrinho P, Van Lergerghe W. Providing health care under adverse conditions: health personnel performance & individual coping strategies. Studies in Health Services Organization & Policy 2000; Issue 16.
- 28.Henderson LN, Tulloch J. Incentives for retaining and motivating health workers in Pacific and Asian countries. Hum Resour Health. 2008;6:18. doi: 10.1186/1478-4491-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reid SJ. Rural health and transformation in South Africa. S Afr Med J. 2006;96:676–7. [PubMed] [Google Scholar]
- 30.Awases M, Gbary A, Nyoni J, Chatora R. Migration of health professionals in six countries: a synthesis report Brazzaville: World Health Organization Regional Office for Africa; 2004. [Google Scholar]
- 31.Stilwell B, Diallo K, Zurn P, Dal Poz MR, Adams O, Buchan J. Developing evidence-based ethical policies on the migration of health workers: conceptual and practical challenges. Hum Resour Health. 2003;1:8. doi: 10.1186/1478-4491-1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]