Abstract
Objective
To understand the factors influencing health workers’ choice to work in rural areas as a basis for designing policies to redress geographic imbalances in health worker distribution.
Methods
A cohort survey of 412 nursing and medical students in Rwanda provided unique contingent valuation data. Using these data, we performed a regression analysis to examine the determinants of future health workers’ willingness to work in rural areas as measured by rural reservation wages. These data were also combined with those from an identical survey in Ethiopia to enable a two-country analysis.
Findings
Health workers with higher intrinsic motivation – measured as the importance attached to helping the poor – as well as those who had grown up in a rural area and Adventists who had participated in a local bonding scheme were all significantly more willing to work in a rural area. The main result for intrinsic motivation in Rwanda was strikingly similar to the result obtained for Ethiopia and Rwanda combined.
Conclusion
Intrinsic motivation and rural origin play an important role in health workers’ decisions to work in a rural area, in addition to economic incentives, while faith-based institutions can also influence the decision.
ملخص
الهدف
فهم العوامل التي تؤثـِّر على اختيار العاملين الصحيين للعمل في المناطق الرئيسية باعتباره أساساً لتصميم السياسات لإصلاح التوازن الجغرافي في توزيع العاملين الصحيين.
الطريقة
قدم مسح للأتراب شمل 412 من طلاب التمريض وطلبة الطب في رواندا معطيات فريدة لتقييم الوحدات. وقد استخدم الباحثون تلك المعطيات لإجراء تحليل التحوُّف لدراسة المحدِّدات للقبول المستقبلي لدى العاملين الصحيين للعمل في المناطق الريفية، وقياسه وفق أجور الاستبقاء في الأرياف. كما قارن الباحثون هذه المعطيات مع معطيات أخرى استمدت من مسحٍ مماثل أجري في أثيوبيا للحصول على تحليل للبلدين.
الموجودات
لقد كان العاملون ذوو التحفيز الداخلي الأعلى، والذي يقاس للأهمية المرتبطة بمساعدة الفقراء، إلى جانب العاملين الذين ترعرعوا في المناطق الريفية والسبتيين الذين يساهمون في خطة ارتباط محلية، جميعهم يرحبون بمقدار يعتد به إحصائياً، بالعمل في المناطق الريفية. وقد كانت النتيجة الرئيسية للتحفيز الداخلي في رواندا تشابه إلى درجة مثيرة النتائج التي نتجت عن أثيوبيا ورواندا مجتمعين.
النتيجة
إن للتحفيز الداخلي وللأصل الريفي دوراً هاماً في قرارات العاملين الخاصة بالعمل في المناطق الريفية، وذلك إلى جانب الحوافز الاقتصادية، كما يمكن للمؤسسات العقائدية أن تؤثـِّر على اتِّخاذ القرار حول ذلك.
Résumé
Objectif
Comprendre d'abord les facteurs influant sur le choix des agents de santé de travailler en milieu rural pour pouvoir ensuite concevoir des politiques visant à redresser les déséquilibres géographiques dans la répartition des agents de santé.
Méthodes
Une étude de cohorte portant sur 412 élèves infirmiers et étudiants en médecine rwandais a fourni des données remarquables sur les préférences exprimées. A l'aide de ces dernières, nous avons réalisé une analyse de régression en vue d'étudier les déterminant de la disposition des futurs agents de santé à travailler dans des zones rurales, telle que mesurée par les salaires minimums acceptés en milieu rural. Ces données ont également été combinées à celles d'une étude identique menée en Éthiopie en vue d'une analyse portant sur les deux pays.
Résultats
Les agents de santé disposant d'une bonne motivation propre - mesurée par l'importance attachée à aider les pauvres - et ceux ayant grandi dans une zone rurale, ainsi que les adventistes ayant participé à un programme visant à nouer des liens localement, étaient significativement davantage disposés à travailler en milieu rural. Le principal résultat concernant la motivation propre au Rwanda était remarquablement similaire à celui obtenu pour l'Éthiopie et le Rwanda combinés.
Conclusion
La motivation propre et l'origine rurale jouent un rôle important dans la décision des agents de santé de travailler en milieu rural, en plus des mesures d'incitation économiques, et les institutions confessionnelles peuvent aussi influer sur cette décision.
Resumen
Objetivo
Comprender los factores que determinan la decisión de los trabajadores sanitarios de trabajar en zonas rurales como base para formular políticas de corrección de los desequilibrios de la distribución geográfica de los trabajadores sanitarios.
Métodos
A través de un estudio de cohortes de 412 estudiantes de medicina y enfermería se obtuvieron datos especiales de valoración contingente. A partir de ellos se realizó un análisis de regresión para examinar los determinantes de la disposición de los futuros trabajadores sanitarios a trabajar en las zonas rurales, medida por los salarios de reserva rurales. Estos datos se combinaron además con los de una encuesta idéntica llevada a cabo en Etiopía para hacer un análisis basado en dos países.
Resultados
Los trabajadores sanitarios con más motivación intrínseca -medida como la importancia atribuida a la ayuda a los pobres-, así como los que habían crecido en una zona rural y los adventistas que habían participado en un sistema de vinculación por contrato se mostraron todos ellos significativamente más dispuestos a trabajar en una zona rural. El resultado principal relativo a la motivación intrínseca en Rwanda fue sorprendentemente similar al obtenido para Etiopía y Rwanda combinadas.
Conclusión
Además de los incentivos económicos, la motivación intrínseca y el origen rural influyen mucho en la decisión de trabajar en una zona rural entre los trabajadores de la salud, y las instituciones confesionales también pueden incidir en esa decisión.
Introduction
Health workers form the foundation of health service delivery: their numbers, skill and commitment are critical for the delivery of good quality health care. Geographical imbalances in the health workforce, a problem common to most health systems, raise concerns about equity (i.e. differential access to health care) and efficiency (i.e. the allocation of resources to those areas where they have the greatest impact on health outcomes). Fortunately, renewed attention is being given to this problem, which is particularly relevant for developing countries, where resources are limited and health outcomes are often poor.
Ultimately, success or failure in attracting health staff to rural facilities or retaining them in rural posts depends on health workers' preferences and choices. A growing body of evidence shows that non-wage job attributes, such as training opportunities, career development prospects, and living and working conditions, play a role in what health workers choose.1–4 However, factors on the supply side, such as health workers' preferences, have received little attention, despite the fact that policy-makers seeking to address geographic imbalances need to also take these factors into account. Policies have shifted from compulsory rural service, which is difficult to manage and enforce, to providing economic incentives for such service in the form of rural allowances and bonuses.5,6 But in the absence of rigorous evaluation, just how effective these incentives are in attracting health workers to rural areas or retaining them in rural posts is uncertain. The available evidence suggests that such measures can improve short-term recruitment, but their effect on long-term retention is less clear.7,8 To address these difficulties, countries as diverse as Australia, the United States of America (USA), Indonesia and Thailand have developed recruitment programmes that target health workers who have particular reasons for being committed to rural service.5,6,9–12 Emerging survey evidence suggests that health workers with a rural background are more willing to work in rural posts and are more responsive to incentives to work in rural areas.12–16 Recent theoretical work also suggests that intrinsic motivation, i.e. the desire to do something for its own sake, can have a strong effect on job choice. New evidence confirms this for health workers in developing countries.16–21 However, most human resource policies do not take into account heterogeneity in health worker preferences.
This paper examines the extent to which health workers differ in their willingness to work in rural areas and the reasons for these differences, based on the data collected in Rwanda analysed individually and in combination with data from Ethiopia.
Methods
Study setting and data
Over the last decade, Rwanda has allocated considerable financial resources to the health sector. Nevertheless, key indicators of health service utilization and health outcomes remain well below the average for sub-Saharan Africa.22,23 Policy-makers in Rwanda agree that an overall shortage of human resources and geographic imbalances in health worker allocation are the main constraints to improving health care. Specifically, almost 88% of physicians and 58% of nurses in the country work in urban areas, despite the fact that 82% of the population resides in rural areas.24,25
In 2008 we conducted a cohort survey of 288 nursing students and 124 medical students in Rwanda. This was equivalent to 53% and 76% of all nursing and medical students in the country, respectively, during the selected period. The sample used for the regression analysis in this study only contained second- and third -year nursing students and medical students in their final year, so that the total number of observations was reduced to 222. A similar cohort survey was conducted in Ethiopia in 2005 and the results of a combined analysis for Ethiopia and Rwanda are presented later in the paper.
The medical students in Rwanda were from the only medical school in the country. We surveyed 83% of all medical students in their final year, and we used a two-step strategy to sample nursing students. We began by selecting three schools among the seven nursing schools in Rwanda. Two of them were government-run (one was in Kigali, the capital, and the other outside Kigali) and the third belonged to a nongovernmental organization (NGO). The only private for-profit school in the country was excluded because it was not accredited. The remaining three schools, two of which were run by the government and one by an NGO, were used for piloting and excluded from the survey to avoid contamination. Next we selected different classes of students. A total of 84%, 78% and 77% of all second- and third-year nursing students in the three schools participated in the survey.
The survey instrument was a self-administered (supervised) questionnaire with questions on job preferences, economic status and demographic characteristics, as well as on health worker motivation. A separate medical knowledge test in two parts, one on evidence-based medicine and the other on the delivery of medical interventions, was also completed by the respondents at the same sitting. The test was developed for the cohort survey conducted in Ethiopia and subsequently tested and adapted for Rwanda under the supervision of the medical faculty of the National University of Rwanda. The test scores were included in the regression analysis to determine if students who scored higher were less willing to work in rural areas than students with lower scores.
The Rwandan government plays an important role in assigning public sector health workers and in determining their wages, which therefore exhibit little variation. Thus, actual salaries do not reflect health workers’ personal valuations of the wages for which they are willing to work in a particular setting. We therefore used contingent valuation questions to assess respondents' willingness to work in rural areas.26 The use of contingent valuation had a further advantage. The students in our sample had not yet entered the labour market and therefore had no observable wages; and even if they had entered the labour market already, for any given health worker only an urban or a rural wage would have been observable. Contingent valuation provided us with counterfactual choices. The use of contingent valuation in the area of human resources for health is rare, and we know of only two examples. One is a study in Indonesia, which showed that under certain circumstances physicians can be attracted to more remote areas using relatively small cash incentives. Another is a study in Ethiopia, discussed elsewhere in this paper, in which contingent valuation was used to elicit rural reservation wages, i.e. the lowest remuneration for which a given health worker is willing to work in a rural area.12,27
In brief, the contingent valuation method is used to elicit the valuation of goods or services for which there is no market. For example, the value of preserving a national park can be elicited through contingent valuation questions for different groups of people to inform a cost–benefit analysis of policies to protect it. Thus, contingent valuation provides a method for gauging the otherwise unobserved demand curve.
We followed best practice for contingent valuations. First, we administered the questionnaires in the schools, under team member supervision, to students who had had practical work experience.28,29 We then used actual starting wages for nurses and physicians as reference wages and offered students a concrete choice between a post in Kigali and a post 100 km from Kigali. Finally, by using a payment-card question, we provided respondents with a range of well defined wage offers.26
After careful piloting, we adapted the contingent valuation question in the Ethiopian study to the Rwandan context:
“Imagine that when you finish your studies you are offered two jobs as a health worker in the public sector, one in Kigali and one in a rural area 100 km from Kigali. Both contracts are for at least 3 years and the jobs are otherwise identical. Your monthly salary for the job in Kigali would be [reference wage] Rwandan francs. Which job would you choose if your monthly salary for the rural job were [amount] Rwandan francs?”
The question was repeated for seven different salaries, starting at 165 000 Rwandan francs (RWF) and gradually increasing up to 515 000 for nursing students, and beginning at 310 000 RWF and going up to 710 000 for medical students. For students with a rural reservation wage greater than the highest wage offered, an open-ended question was added to limit censoring from above.
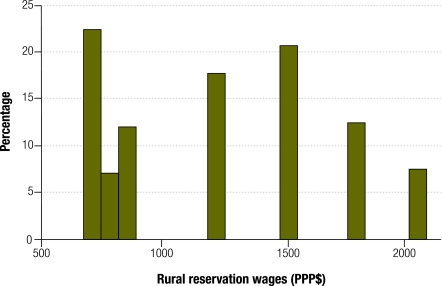
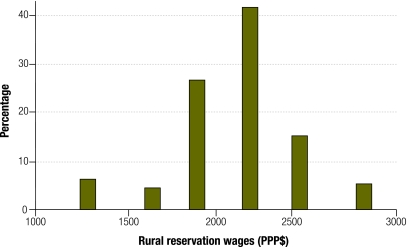
Fig. 1 and Fig. 2 plot the histograms of rural reservation wages (expressed in 2008 United States dollars adjusted for purchasing power parity, henceforth PPP$)30 and indicate that while the distribution for nursing students tends to be bimodal, with one group of nursing students having relatively low reservation wages and a second group distributed around a higher mean, the distribution for medical students is unimodal.
Fig. 1.
Histograms of rural reservation wages among nursing students in Rwanda, 2008
PPP$, purchasing power parity dollar.
Fig. 2.
Histograms of rural reservation wages among medical students in Rwanda, 2008
PPP$, purchasing power parity dollar.
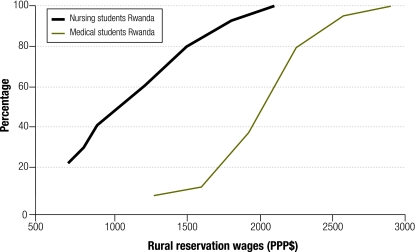
Fig. 3 plots the cumulative distribution functions (CDFs). The line to the left reflects the CDF for nursing students and indicates that close to 40% of nursing students are willing to work in a rural area at the current starting wage (875 PPP$), and that more nursing students are willing to work in a rural post as wage offers increase. A crude reading of the CDF suggests that to get 80% of new nurses to take up a rural post (under the assumption that wages are the sole determinant of location decisions) would require an average premium of 71% on top of the current starting wage. For medical students, only 7% are willing to work in a rural area for the current wage (1430 PPP$), and the concave shape of the CDF indicates that at higher wage levels, additional wage increases attract fewer extra physicians to rural areas. To get 80% of physicians to take up a rural post would require a wage premium of 57%.
Fig. 3.
Cumulative distributions of rural reservation wages among nursing and medical students in Rwanda, 2008
PPP$, purchasing power parity dollar.
Estimation method
To analyse the contingent valuation data for Rwanda we estimate the following equation:
| RWi = β0 + β1HELPPOORi + β2HHEXPi + β3TSCOREi + β4FEMALEi + β5AGEi + β6DISTANCEi + β7KIGALIi + β8RELIGIOUSAFFILi + β9DOCTORi + β10STUDYYRi + β11OPENVALi + εi |
where RW, the dependent variable, is the natural log of the reservation wage at which a rural post would be accepted. On the right-hand side, HELPPOOR is our measure for intrinsic motivation and it takes the value 1 if “opportunity to help the poor” is ranked as the most important job characteristic by the respondent relative to other job attributes related to extrinsic motivation. The variable HHEXP reflects the economic status of the parental household, since most students do not have their own household yet. By including questions on asset ownership identical to the ones used in the national Integrated Household Living Conditions Survey conducted by the National Institute of Statistics of Rwanda, we can predict household expenditures.31,32 The medical knowledge test score, TSCORE, allows us to test the assumption that students who perform better in school are less likely to work in rural areas. Other variables we include on the right-hand side of the equation are FEMALE and AGE. We also include two variables reflecting a rural or urban background: DISTANCE, the time it took to walk to school at age 6, and KIGALI, which takes the value 1 if the respondent was born in Kigali. In line with previous findings, we expect health workers from rural areas to be more willing to work in a rural setting. A variable reflecting religious affiliation, RELIGIOUSAFFIL, is used to test whether this is associated with the provision of rural (and pro-poor) services, as suggested by emerging research.27,33
We estimate the equation by the ordinary least-squares method to provide a point of reference for the subsequent interval regressions. The latter is the preferred method because reservation wages are reported in ranges rather than exact values, and interval regression analysis explicitly takes the censoring of the reported reservation wages into account. Summary statistics are shown in Table 1.
Table 1. Variable descriptions and summary statistics for Ethiopiaa (2005) and Rwandaa (2008) regression samples.
| Variable | Description | Rwanda |
Ethiopia |
|||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| RW | Rural reservation wage (2008 PPP$) | 1 711 | 786 | 620 | 279 | |
| HELPPOOR | Dummy variable. Indicates opportunity to help poor is most important job attribute | 0.05 | 0.23 | 0.24 | 0.43 | |
| HHEXP | Predicted parental household expenditure (2008 PPP$) | 14 158 | 14 051 | 4 985 | 1 750 | |
| TSCORE | Score on medical knowledge test | 0.33 | 0.12 | 0.49 | 0.12 | |
| FEMALE | Dummy variable. Indicates respondent is female | 0.59 | 0.49 | 0.36 | 0.48 | |
| AGE | Age of respondent (years) | 27 | 5 | 23 | 3 | |
| DISTANCE | Time (in minutes) to walk to school at age 6 | 36 | 29 | 30 | 26 | |
| ADVENTIST | Dummy variable. Indicates respondent is Adventist | 0.11 | 0.31 | NA | NA | |
| CATHOLIC | Dummy variable. Indicates respondent is Catholic | NA | NA | 0.09 | 0.28 | |
| PROTESTANT | Dummy variable. Indicates respondent is Protestant | NA | NA | 0.23 | 0.42 | |
| KIGALI | Dummy variable. Indicates respondent born in Kigali | 0.25 | 0.43 | NA | NA | |
| ADDIS | Dummy variable. Indicates respondent born in Addis Ababa | NA | NA | 0.25 | 0.44 | |
| OBLIGATION | Dummy variable. Indicates respondent's obligation to work or repay funding received | 0.62 | 0.49 | NA | NA | |
| RURWEXP | Dummy variable. Indicates respondent had rural work experience during training | 0.42 | 0.49 | NA | NA | |
| DOCTOR | Dummy variable. Indicates respondent is a medical student | 0.31 | 0.46 | 0.31 | 0.47 | |
| No. of observations | 222 | 270 | ||||
NA, not applicable; PPP$, purchasing power parity dollar; SD, standard deviation.
a The respective samples for Ethiopia and Rwanda consist of second- and third-year nursing students and medical students in their final year.
Because of the relatively small number of observations, in the next section we combine the results for nursing and medical students (while including a dummy variable, DOCTOR, for medical students). All the main results are similar for the subsample of nursing students only, and the results for medical students are largely the same but less pronounced due to the small sample size.
Results
Table 2 contains the results of the ordinary least-squares and interval regression analyses for the sample of 222 second- and third-year nursing students and medical students in their final year in Rwanda. The results, which are consistent across specifications and estimation methods, show that students with higher intrinsic motivation – those who rank “helping the poor” as the most important job attribute – had lower rural reservation wages, with a regression coefficient statistically significant at the 5% level. Students from a more prosperous background tended to have higher reservation wages, arguably because they could afford to be more selective about their work location, although the regression coefficient was not significant in the second, third, fifth and sixth specifications, when the proxies for rural background and being born in an urban area were included in the model. We found no evidence that students with a higher score on the medical knowledge test were less willing to work in rural areas. However, students who grew up in more remote areas, as proxied by the time it took to walk from home to school at age 6, had lower rural reservation wages, in line with findings from previous studies.12,34,35 In our sample, the Adventist religious affiliation was the only one that yielded statistically significant results, and our estimations therefore focused on this particular affiliation.
Table 2. Results from ordinary least-squares and interval regression analysis of determinants of rural reservation wagesa among nursing and medical students in Rwanda, 2008.
| Variable | Ordinary least-squares analysisb |
Interval regressionsb |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 |
2 |
3 |
4 |
5 |
6 |
||||||||||||
| RC | SE | RC | SE | RC | SE | RC | SE | RC | SE | RC | SE | ||||||
| HELPPOOR | −0.230** | 0.104 | −0.236** | 0.101 | −0.240** | 0.106 | −0.302** | 0.141 | −0.309** | 0.139 | −0.306** | 0.140 | |||||
| HHEXP | 0.042* | 0.024 | 0.020 | 0.028 | 0.023 | 0.026 | 0.049* | 0.026 | 0.026 | 0.031 | 0.027 | 0.029 | |||||
| TSCORE | 0.003 | 0.002 | 0.003 | 0.002 | 0.003 | 0.002 | 0.003 | 0.003 | 0.003 | 0.002 | 0.003 | 0.003 | |||||
| AGE | 0.007 | 0.004 | 0.006 | 0.004 | 0.010** | 0.004 | 0.007 | 0.005 | 0.006 | 0.005 | 0.010** | 0.005 | |||||
| FEMALE | 0.001 | 0.050 | −0.036 | 0.047 | −0.050 | 0.046 | −0.011 | 0.057 | −0.055 | 0.053 | −0.072 | 0.052 | |||||
| DISTANCE | – | – | −0.001* | 0.001 | −0.002** | 0.001 | – | – | −0.002** | 0.001 | −0.002** | 0.001 | |||||
| KIGALI | – | – | 0.027 | 0.051 | 0.027 | 0.049 | – | – | 0.000 | 0.055 | 0.004 | 0.053 | |||||
| ADVENTIST | – | – | −0.228*** | 0.074 | −0.094 | 0.088 | – | – | −0.323*** | 0.091 | −0.135 | 0.103 | |||||
| RURWEXP | – | – | – | – | −0.132*** | 0.046 | – | – | – | – | −0.150*** | 0.051 | |||||
| OBLIGATION | – | – | – | – | 0.058 | 0.045 | – | – | – | – | 0.073 | 0.049 | |||||
| ADV × RURWEXP × OBLIGc | – | – | – | – | −0.268** | 0.109 | – | – | – | – | −0.403** | 0.161 | |||||
| DOCTOR | 0.281** | 0.120 | 0.278** | 0.113 | 0.211* | 0.118 | 0.310** | 0.145 | 0.310** | 0.134 | 0.242* | 0.138 | |||||
| R2 | 0.59 | – | 0.62 | – | 0.65 | – | – | – | – | – | – | – | |||||
*P < 0.1; **P < 0.05; ***P < 0.01.
RC, regression coefficient; SE, robust standard error.
a The dependent variable is the natural log of the reported rural reservation wage.
b All regressions include a constant term and controls for year of study and for respondents with rural reservation wages greater than the highest wage offer.
c ADV × RURWEXP × OBLIG indicates that a respondent has rural work experience, an obligation to work or repay funding received, and is Adventist.
The results from the second and fifth specifications in Table 2 imply that Adventist students had lower rural reservation wages on average. Anecdotal evidence suggests that this reflects a local bonding scheme operated by Adventist communities in Rwanda, whereby students must repay funding either by working for the community or in cash, and they are encouraged to intern in a rural facility where they can later work. To unravel the effect of being an Adventist, we included an indicator variable, RURWEXP, for having rural work experience and another indicator variable, OBLIGATION, to reflect if the health worker was under obligation to pay back educational expenses. Because not all Adventists participated in a bonding scheme, we included an interaction term between ADVENTIST and these two variables, to reflect participation in such a scheme. When the interaction term was included in the model, the coefficient for the ADVENTIST variable lost statistical significance (third and sixth specifications). This confirms that the statistically significant regression coefficient for the variable ADVENTIST in the second and fifth specifications reflected participation in the bonding scheme. Finally, medical students had significantly higher reservation wages than nursing students, as expected.
Thus, using unique data based on contingent valuation questions, we found that intrinsic motivation, rural background, and Adventists’ participation in a local bonding scheme were strongly related to health workers’ willingness to work in a rural area in Rwanda. These results, especially those related to intrinsic motivation, are highly consistent with the results of a joint analysis including data from a similar cohort survey conducted in Ethiopia, presented in the following section.
Combined analysis
Because the survey instrument we used in Rwanda was identical to the one used in the Ethiopian survey, we were able to compare findings for the two countries and conduct a joint analysis using data from both countries. The regression results for Ethiopia, which also showed a statistically significant positive association between intrinsic motivation and willingness to work in a rural area, are described in the original publication.27 As in Rwanda, in Ethiopia, students from a more prosperous background had higher reservation wages, and those who grew up in more remote areas or who were Catholic had lower reservation wages. The last mentioned is explained by the fact that most Catholic students attend an NGO school that strongly encourages commitment to rural service in its education.
Because of the relatively small number of observations in each country sample, we pooled the observations for the two countries to estimate the regression coefficients more precisely. Table 3 shows the results of the ordinary least-squares and interval regression analysis for the joint Ethiopian and Rwandan sample. The regression coefficient on intrinsic motivation remained highly significant in the joint sample, indicating that more motivated future health workers had lower rural reservation wages. Being Adventist also remained highly significant, and being Catholic was weakly significant. The coefficient on the Protestant variable was also statistically significant in the pooled data but not in the separate analyses. Further analysis is needed to understand what this effect is capturing. A rural background, as proxied by the distance to school at age 6, was no longer significant, whereas being from Addis Ababa (the Ethiopian capital) was significant in the ordinary least-squares analysis (second specification in Table 3), but not in the interval regression analysis (fourth specification in Table 3). The reason is that the variables proxying for rural background were different in the two countries: distance to school in Rwanda and having a permanent address in Addis Ababa in Ethiopia.
Table 3. Results from ordinary least-squares and interval regression analysis of determinants of rural reservation wagesa among nursing and medical students in Ethiopia (2005) and Rwanda (2008).
| Variable | Ordinary least-squares analysisb |
Interval regressionb |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 |
2 |
3 |
4 |
||||||||
| RC | SE | RC | SE | RC | SE | RC | SE | ||||
| HELPPOOR | −0.153*** | 0.042 | −0.179*** | 0.043 | −0.230*** | 0.065 | −0.236*** | 0.067 | |||
| HHEXP | 0.000 | 0.000 | −0.000 | 0.000 | −0.000 | 0.000 | −0.000 | 0.000 | |||
| TSCORE | −0.001 | 0.002 | −0.001 | 0.002 | −0.001 | 0.003 | −0.001 | 0.003 | |||
| FEMALE | 0.047 | 0.033 | 0.007 | 0.035 | −0.017 | 0.047 | −0.038 | 0.049 | |||
| AGE | 0.000 | 0.004 | −0.000 | 0.004 | −0.003 | 0.005 | −0.003 | 0.005 | |||
| DISTANCE | – | – | −0.001 | 0.001 | – | – | −0.001 | 0.001 | |||
| KIGALI | – | – | −0.012 | 0.067 | – | – | −0.022 | 0.082 | |||
| ADDIS | – | – | 0.086** | 0.041 | – | – | −0.044 | 0.070 | |||
| ADVENTIST | – | – | −0.291*** | 0.100 | – | – | −0.395*** | 0.129 | |||
| CATHOLIC | – | – | −0.074 | 0.050 | – | – | −0.115* | 0.070 | |||
| PROTESTANT | – | – | −0.074* | 0.040 | – | – | −0.123** | 0.054 | |||
| DOCTOR | 0.694*** | 0.029 | 0.640*** | 0.033 | 0.710*** | 0.041 | 0.662*** | 0.045 | |||
| R2 | 0.76 | – | 0.77 | – | – | – | – | – | |||
*P < 0.1; **P < 0.05; ***P < 0.01.
RC, regression coefficient; SE, robust standard error.
a The dependent variable is the natural log of the reported rural reservation wage.
b All regressions include a constant term and a dummy variable for Ethiopia.
Discussion
The results presented in this paper provide clear evidence of substantial heterogeneity in health workers’ willingness to work in a rural area. In Rwanda, future health workers who are more intrinsically motivated, come from a rural background, or participate in an Adventist local bonding scheme were all found to have significantly lower rural reservation wages.
When the data from Rwanda were pooled with those from Ethiopia, two key determinants of rural reservation wages emerged: motivation to help the poor and religious affiliation, with the latter reflecting country-specific activities by faith-based institutions. In Rwanda, the Adventist community operates a local bonding scheme, which our results suggest is effective in getting future health workers to take up rural posts. So far this has only been documented with anecdotal evidence. In Ethiopia, a Catholic NGO offers training that encourages rural service. In all these results, the effect of intrinsic motivation stands out as a particularly strong and robust finding.
These results are very robust despite the notable differences between the two countries: Rwanda is a small country with a high population density and a mixed public–private health system, while Ethiopia is a vast country with a low population density that has only recently made the transition to a combined public–private health system. This suggests that health workers’ willingness to work in a rural area is not as context-specific as is often assumed.
What do these findings imply for policy-making? First, that while economic incentives undoubtedly play an important role in future health workers' choice of rural or urban postings, they are not the only factor. In line with a growing theoretical literature on public service delivery, our results corroborate empirically that health worker motivation is also important.18,20,36,37 As a result, schemes intended to attract and retain staff in rural areas can be made more effective by targeting highly motivated health workers. A simple simulation illustrates how it can also reduce costs. Assume for simplicity that we want 80% of nurses in rural areas because that is where approximately 80% of the population lives. Paying the rural premium of 71% of starting wages to all nurses would require an increase of 30% of the human resource budget or 1.2% of the total annual health budget. If instead highly motivated health workers are targeted with the goal of obtaining 50% motivated workers, the human resource budget would only need to increase by 22.5% or 0.9% of the total health budget. Although these are naïve simulations based on stringent assumptions, they illustrate the potential benefits of integrating motivation into human resource for health policies.
Second, health workers with certain observable characteristics, such as a rural background, tend to be more willing to work in rural areas and should therefore be actively encouraged to choose a rural posting through targeted recruitment programmes like the ones previously discussed.
Third, our findings in connection with religious affiliation underline the important role of faith-based institutions in the health sector in sub-Saharan Africa, and both Ethiopia and Rwanda offer examples to inspire future policy-making.
Of the three factors that influence health workers’ willingness to work in a rural area, rural background is the most tangible. The roles of intrinsic motivation and of context-specific faith-based institutions deserve more attention in future analytical work.
Acknowledgements
We would like to thank Agnes Soucat, Magnus Lindelöw and Chris Herbst for their valuable insights and continuous support. The findings, interpretations and conclusions expressed in this paper are entirely those of the authors. They do not necessarily represent the views of The World Bank.
Funding:
This study was funded by The World Bank. Montalvo acknowledges the support of SEJ2007-64340 and ICREA-Academia.
Competing interests:
None declared.
References
- 1.Hays RB, Veitch PC, Cheers B, Crossland L. Why doctors leave rural practice. Aust J Rural Health. 1997;5:198–203. doi: 10.1111/j.1440-1584.1997.tb00267.x. [DOI] [PubMed] [Google Scholar]
- 2.Kamien M. Staying in or leaving rural practice: 1996 outcomes of rural doctors’ 1986 intentions. Med J Aust. 1998;169:318–21. doi: 10.5694/j.1326-5377.1998.tb140285.x. [DOI] [PubMed] [Google Scholar]
- 3.Peters DH, Yazbeck A, Sharma R, Ramana GNV, Pritchett L, Wagstaff A. Better health systems for India’s poor: findings, analysis and options Washington, DC: The World Bank; 2002. [Google Scholar]
- 4.Shields MA. Addressing nurse shortages: what can policymakers learn from the econometric evidence on nurse labour supply? Econ J. 2004;114:F464–98. doi: 10.1111/j.1468-0297.2004.00255.x. [DOI] [Google Scholar]
- 5.Wibulpolprasert S, Pengpaibon P. Integrated strategies to tackle the inequitable distribution of doctors in Thailand: four decades of experience. Hum Resour Health. 2003;1:12. doi: 10.1186/1478-4491-1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sempowski IP. Effectiveness of financial incentives in exchange for rural and underserviced area return-of-service commitments: systematic review of the literature. Can J Rural Med. 2004;9:82–8. [PubMed] [Google Scholar]
- 7.Anderson M, Rosenberg MW. Ontario’s underserviced area program revisited: an indirect analysis. Soc Sci Med. 1990;30:35–44. doi: 10.1016/0277-9536(90)90327-O. [DOI] [PubMed] [Google Scholar]
- 8.Nigenda G. The regional distribution of doctors in Mexico, 1930–1990: a policy assessment. Health Policy. 1997;39:107–22. doi: 10.1016/S0168-8510(96)00864-0. [DOI] [PubMed] [Google Scholar]
- 9.Rabinowitz HK, Diamond JJ, Markham FW, Hazelwood CE. A program to increase the number of family physicians in rural and underserved areas: impact after 22 years. JAMA. 1999;281:255–60. doi: 10.1001/jama.281.3.255. [DOI] [PubMed] [Google Scholar]
- 10.Easterbrook M, Godwin M, Wilson R, Hodgetts G, Brown G, Pong R, et al. Rural background and clinical rural rotations during medical training: effect on practice location. CMAJ. 1999;160:1159–63. [PMC free article] [PubMed] [Google Scholar]
- 11.Rolfe IE, Pearson SA, O’Connell DL, Dickinson JA. Finding solutions to the rural doctor shortage: the roles of selection versus undergraduate medical education at Newcastle. Aust N Z J Med. 1995;25:512–7. doi: 10.1111/j.1445-5994.1995.tb01497.x. [DOI] [PubMed] [Google Scholar]
- 12.Chomitz KM, Setiadi G, Azwar A, Ismail N, Widiyarti N. What do doctors want? Developing incentives for doctors to serve in Indonesia’s rural and remote areas (World Bank Policy Research Working Paper No. 1888). Washington, DC: The World Bank; 1998.
- 13.Kristiansen IS, Førde OH. Medical specialists’ choice of location: the role of geographical attachment in Norway. Soc Sci Med. 1992;34:57–62. doi: 10.1016/0277-9536(92)90067-Z. [DOI] [PubMed] [Google Scholar]
- 14.Laven G, Wilkinson D. Rural doctors and rural backgrounds: how strong is the evidence? A systematic review. Aust J Rural Health. 2003;11:277–84. doi: 10.1111/j.1440-1584.2003.00534.x. [DOI] [PubMed] [Google Scholar]
- 15.Lievens T, Serneels P, Butera JD. Where, why and for how much. Diversity in career preferences of future health workers in Rwanda Washington, DC: The World Bank; 2010. [Google Scholar]
- 16.Lindelow M, Serneels P. The performance of health workers in Ethiopia: results from qualitative research. Soc Sci Med. 2006;62:2225–35. doi: 10.1016/j.socscimed.2005.10.015. [DOI] [PubMed] [Google Scholar]
- 17.Besley T, Ghatak M. Competition and incentives with motivated agents. Am Econ Rev. 2005;95:616–36. doi: 10.1257/0002828054201413. [DOI] [Google Scholar]
- 18.Dixit A. Incentives and organizations in the public sector: an interpretative review. J Hum Resour. 2002;37:696–727. doi: 10.2307/3069614. [DOI] [Google Scholar]
- 19.Franco LM, Bennett S, Kanfer R. Health sector reform and public sector health worker motivation: a conceptual framework. Soc Sci Med. 2002;54:1255–66. doi: 10.1016/S0277-9536(01)00094-6. [DOI] [PubMed] [Google Scholar]
- 20.Francois P, Vlassopoulos M. Pro-social motivation and the delivery of social services. CESifo Econ Stud. 2008;54:22–54. doi: 10.1093/cesifo/ifn002. [DOI] [Google Scholar]
- 21.Prendergast C. Intrinsic motivation and incentives. Am Econ Rev. 2008;98:201–5. doi: 10.1257/aer.98.2.201. [DOI] [Google Scholar]
- 22.World Health Organization. World health report 2006: statistical annex. Geneva: WHO; 2006. [Google Scholar]
- 23.Rwanda, Ministry of Health. Rwanda health sector policy Kigali: MOH; 2005. Available from: http://www.moh.gov.rw/index.php?option=com_content&view=article&id=53&Itemid=28 [accessed 19 February 2010].
- 24.World Health Organization. Global health atlas Washington, DC: WHO; 2009. Available from: http://apps.who.int/globalatlas/DataQuery/default.asp [accessed 19 February 2010]. [Google Scholar]
- 25.The World Bank. World development indicators Washington, DC: WB; 2009. [Google Scholar]
- 26.Portney PR.The contingent valuation debate: why economists should care. J Econ Perspect 199483–17.[REMOVED HYPERLINK FIELD]10136763 [Google Scholar]
- 27.Serneels P, Lindelöw M, Montalvo JG, Barr A. For public service or money: understanding geographical imbalances in the health workforce. Health Policy Plan. 2007;22:128–38. doi: 10.1093/heapol/czm005. [DOI] [PubMed] [Google Scholar]
- 28.Diamond PA, Hausman JA.Contingent valuation: is some numbers better than no numbers? J Econ Perspect 1994845–64.10136765 [Google Scholar]
- 29.Hanemann WM. Valuing the environment through contingent valuation. J Econ Perspect. 1994;8:19–43. [Google Scholar]
- 30.International Monetary Fund. World economic outlook database Washington, DC: IMF; 2008. [Google Scholar]
- 31.Grosh M, Baker J. Proxy means test for targeting social programs: simulations and speculation (LSMS Working Paper 118). Washington, DC: The World Bank; 1995.
- 32.Ahmed A, Bouis H. Weighing what’s practical: proxy means tests for targeting food subsidies in Egypt. Food Policy. 2002;27:519–40. doi: 10.1016/S0306-9192(02)00064-7. [DOI] [Google Scholar]
- 33.Reinikka R, Svensson J. Working for God? Evaluating service delivery of religious not-for-profit health care providers in Uganda (World Bank Policy Research Working Paper No. 3058). Washington, DC: The World Bank; 2003.
- 34.Dunbabin J, Levitt L.Rural origin and rural medical exposure: their impact on the rural and remote medical workforce in Australia. Rural Remote Health 20033.Available from: http://www.rrh.org.au/publishedarticles/article_print_212.pdf[accessed 19 February 2010] [PubMed] [Google Scholar]
- 35.de Vries E, Reid S. Do South African medical students of rural origin return to rural practice? S Afr Med J. 2003;93:789–93. [PubMed] [Google Scholar]
- 36.Dixit A. Power of incentives in private versus public organisations. Am Econ Rev. 1997;87:378–82. [Google Scholar]
- 37.Wilson JQ. Bureaucracy: what government agencies do and why they do it New York: Basic Books; 1989. [Google Scholar]