Abstract
Admission to the hospital on weekends is associated with increased mortality for several acute illnesses. We investigated whether patients admitted on a weekend with acute kidney injury (AKI) were more likely to die than those admitted on a weekday. Using the Nationwide Inpatient Sample, a large database of admissions to acute care, nonfederal hospitals in the United States, we identified 963,730 admissions with a diagnosis of AKI between 2003 and 2006. Of these, 214,962 admissions (22%) designated AKI as the primary reason for admission (45,203 on a weekend and 169,759 on a weekday). We used logistic regression models to examine the adjusted odds of in-hospital mortality associated with weekend versus weekday admission. Compared with admission on a weekday, patients admitted with a primary diagnosis of AKI on a weekend had a higher odds of death [adjusted odds ratio (OR) 1.07, 95% confidence interval (CI) 1.02 to 1.12]. The risk for death with admission on a weekend for AKI was more pronounced in smaller hospitals (adjusted OR 1.17, 95% CI 1.03 to 1.33) compared with larger hospitals (adjusted OR 1.07, 95% CI 1.01 to 1.13). Increased mortality was also associated with weekend admission among patients with AKI as a secondary diagnosis across a spectrum of co-existing medical diagnoses. In conclusion, among patients hospitalized with AKI, weekend admission is associated with a higher risk for death compared with admission on a weekday.
Admission to hospital on weekends has been associated with increased mortality compared with weekday admissions among patients with certain medical conditions.1–7 Although this observation may be due to unmeasured differences in severity of illness among patients who present to the hospital at different times, others have hypothesized that differences in processes of care on weekends may explain these outcomes.1,8 Potential process factors include lower levels of staffing, provider coverage issues, and restricted availability of tests and procedures during weekends.1,9,10
A previous analysis of Canadian data demonstrated that patients with a primary diagnosis of “renal failure” experienced a 34% higher risk of adjusted in-hospital mortality when admitted on a weekend compared with a weekday.1 However, because admissions for acute kidney injury (AKI) were not distinguished from those for chronic kidney disease (CKD), some speculated that this association was in fact driven by admissions of patients with ESRD.11 Whether delayed access to diagnostic or therapeutic procedures in patients with AKI contributes to increased weekend mortality has not been previously studied.
We sought to determine if admission to hospital on the weekend with a diagnosis of AKI was associated with higher in-hospital mortality than admission on a weekday using nationally representative data from U.S. acute care, nonfederal hospitals between 2003 and 2006. We hypothesized that patients admitted with AKI on weekends would experience higher in-hospital mortality independent of demographic and clinical characteristics, including severity of illness. Because the availability of resources for patient assessment, diagnosis, and management are known to vary with hospital characteristics, we also hypothesized that this association would be most pronounced in smaller hospitals, characterized by fewer beds and lower levels of staffing.
Results
Characteristics of Weekend and Weekday Admissions with AKI
During a 4-year period, we identified 963,730 admissions with a diagnosis of AKI within acute care, nonfederal U.S. hospitals. Admission on a weekend occurred in 214,832 (22.3%) of those with AKI. The characteristics of patients with AKI admitted on weekends were for the most part similar to those admitted on weekdays, although statistically significant differences in the distributions of several demographic, clinical, and hospital characteristics were observed (Table 1). The median length of hospital stay of 7 days was similar for weekend and weekday admissions with AKI. The proportions of patients discharged to another short-term hospital (3.6% versus 3.4%, P < 0.001) and to an intermediate care or skilled nursing facility (29.4% versus 28.5%, P < 0.001) were greater for weekend than for weekday admissions. Patients admitted with AKI on a weekend were more likely to receive mechanical ventilation [odds ratio (OR) 1.20, 95% confidence interval (CI) 1.14 to 1.26] irrespective of hospital size (P interaction 0.67). Conversely, patients admitted on a weekend were less likely to receive dialysis (OR 0.94, 95% CI 0.90 to 0.97), regardless of hospital size (P interaction 0.45).
Table 1.
Characteristics of admissions with a diagnosis of AKI according to day of admission on the basis of NIS data from 2003 to 2006
| Weekend | Weekday | P Value | |
|---|---|---|---|
| Number of admissions | 214,832 | 748,898 | |
| Age, mean (SD), years | 69.4 (16.8) | 69.2 (16.5) | <0.001 |
| Women, n (%) | 103,705 (48.3) | 357,701 (47.8) | <0.001 |
| Race, n (%) | <0.001 | ||
| white | 109,110 (50.8) | 387,325 (51.7) | |
| black | 29,272 (13.6) | 97,467 (13.0) | |
| Hispanic | 14,923 (6.9) | 50,099 (6.7) | |
| Asian or Pacific Islander | 3,922 (1.8) | 12,351 (1.6) | |
| Native American | 605 (0.3) | 2,020 (0.3) | |
| other | 3,132 (1.0) | 11,518 (1.5) | |
| missing | 53,868 (25.1) | 188,118 (25.1) | |
| Charlson comorbidity index, mean (SD) | 2.79 (2.18) | 2.84 (2.21) | <0.001 |
| Procedures, n (%) | |||
| mechanical ventilation | 38,231 (17.8) | 114,902 (15.3) | <0.001 |
| dialysis | 18,071 (8.4) | 66,572 (8.9) | <0.001 |
| Primary diagnosis, n (%)a | |||
| AKI | 45,203 (21.0) | 169,759 (22.7) | <0.001 |
| sepsis | 45,409 (21.0) | 137,713 (18.4) | <0.001 |
| pneumonia | 35,882 (16.7) | 107,761 (14.4) | <0.001 |
| acute myocardial infarction | 24,879 (11.6) | 74,466 (9.9) | <0.001 |
| heart failure | 30,358 (14.1) | 113,900 (15.2) | 0.007 |
| gastrointestinal bleed | 8,533 (4.0) | 26,415 (3.5) | <0.001 |
| pancreatitis | 4,411 (2.1) | 13,065 (1.7) | <0.001 |
| liver failure | 3,825 (1.8) | 11,769 (1.6) | <0.001 |
| other | 16,332 (7.6) | 94,050 (12.6) | <0.001 |
| Hospital size, n (%) | <0.001 | ||
| small | 23,553 (11.0) | 82,754 (11.1) | |
| medium | 53,887 (25.1) | 182,942 (24.4) | |
| large | 137,392 (63.9) | 483,202 (64.5) | |
| Hospital teaching status, n (%) | <0.001 | ||
| nonteaching | 118,251 (55.0) | 405,588 (54.2) | |
| teaching | 96,581 (45.0) | 343,310 (45.8) |
aFor admissions where AKI was not the primary diagnosis, AKI was present as a secondary (co-existing) diagnosis.
Weekend Admissions with AKI as a Primary Diagnosis
A total of 214,962 admissions designated AKI as the primary diagnosis (primary reason for admission to hospital); 45,203 on a weekend, 169,759 on a weekday. During hospitalization, 14,686 (6.8%) patients admitted with a primary diagnosis of AKI died; 7.3% of patients admitted on a weekend and 6.7% of patients admitted on a weekday. Compared with weekday admissions for AKI, the unadjusted odds of death associated with weekend admission was increased by 26% by day 3 of admission (OR 1.26, 95% CI 1.19 to 1.34) and by 11% for the total hospital stay (OR 1.11, 95% CI 1.06 to 1.15). After adjustment for age, sex, race, Charlson comorbidity index, and the requirement for mechanical ventilation, weekend admission with AKI remained associated with a 22% increased odds of death by day 3 of admission (OR 1.22, 95% CI 1.15 to 1.30) and a 7% increase for the duration of the hospital stay (OR 1.07, 95% CI 1.02 to 1.12) (Table 2).
Table 2.
Mortality associated with weekend versus weekday admission with a primary diagnosis of AKI on the basis of NIS data from 2003 to 2006
| Mortality, n (%) |
OR (95% CI) |
|||
|---|---|---|---|---|
| Weekend (n = 45,203) | Weekday (n = 169,759) | Unadjusted | Adjusteda | |
| Mortality by third day of admission | 1442 (3.2%) | 4318 (2.5%) | 1.26 (1.19 to 1.34) | 1.22 (1.15 to 1.30) |
| Total in-hospital mortality | 3321 (7.3%) | 11,365 (6.7%) | 1.11 (1.06 to 1.15) | 1.07 (1.02 to 1.12) |
aOR adjusted for age, gender, race, Charlson comorbidity index, and use of mechanical ventilation.
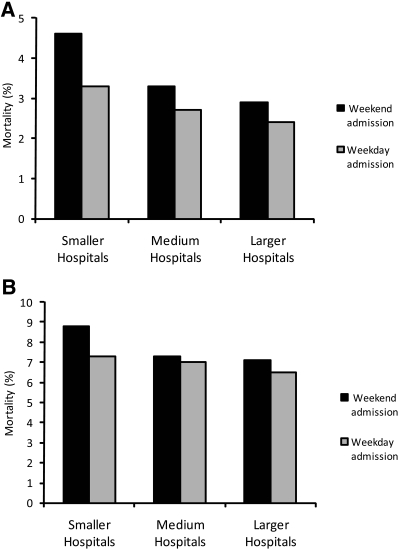
Figure 1 shows mortality rates by weekend versus weekday admission (top panel within 3 days, bottom panel during total hospital stay), stratified by hospital size. A statistically significant interaction was observed between weekend admission and hospital size (P < 0.001) but not between weekend admission and hospital teaching status (P = 0.12). Increases in mortality associated with weekend admission for AKI were most pronounced in smaller hospitals, where a 35% increase in the adjusted odds of death was observed by day 3 (OR 1.35, 95% CI 1.14 to 1.59) and a 17% increase in the adjusted risk of death remained for the total hospital admission (OR 1.17, 95% CI 1.03 to 1.33). For medium-sized and larger hospitals, mortality associated with weekend admission for AKI was increased to a lesser degree. Within the larger hospitals, a 24% increase in the adjusted risk of death was observed by day 3 (OR 1.24, 95% CI 1.10 to 1.39), and a 7% increase in the adjusted risk of death remained for the total hospital admission (OR 1.07, 95% CI 1.01 to 1.13).
Figure 1.
Higher mortality for primary diagnosis of AKI with weekend versus weekday admission by hospital day 3 (A) and during total hospital stay (B), most pronounced in smaller hospitals.
Weekend Admissions with AKI as a Secondary Diagnosis
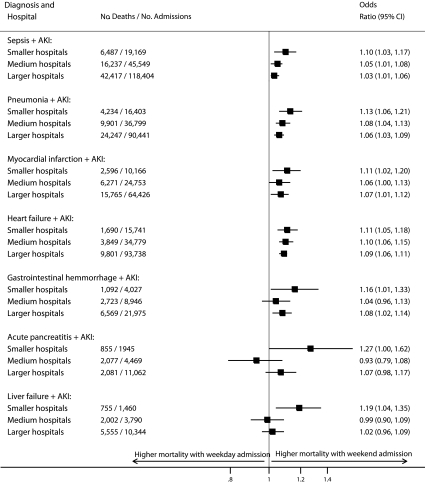
Increased risk of in-hospital mortality associated with weekend admission was consistently observed across seven medical conditions (present as primary diagnoses) that co-existed with AKI (recorded as a secondary diagnosis) (Figure 2).
Figure 2.
Higher mortality for weekend versus weekday admission across multiple primary acute conditions with AKI as secondary diagnosis (OR adjusted for age, sex, race, Charlson comorbidity index, and use of mechanical ventilation).
Discussion
AKI is a relatively common condition that continues to be associated with high mortality.12 Although some studies have suggested a recent trend toward improved outcomes in the setting of AKI, it is unclear whether these observations are due to overall improvements in the quality of health care or if they have resulted from differences over time in the way AKI is recognized and defined.13,14 Hospital admission on a weekend may delay the provision of some elements of care, including diagnostic and therapeutic interventions.8–10 We observed an increased risk of death with weekend admission for patients with AKI that was most evident for admissions to smaller hospitals. Furthermore, weekend admissions were associated with heightened mortality when AKI complicated a wide array of acute medical conditions.
The excess risk of in-hospital death among patients admitted with AKI on a weekend was modest when expressed in relative terms (ranging from 7% to 17% depending on hospital size, compared with admission on a weekday). However, when projected across the U.S. health care system, the high incidence of AKI translates into a large increase in deaths. On the basis of these estimates, we project that approximately 4000 additional deaths per year occur in patients with AKI admitted on the weekend in the United States, representing 1 additional death for every 65 weekend admissions with AKI. Admission on a weekend thus appears to be a clinically relevant risk factor for mortality among patients with AKI.
Little is known about the association between time of admission and outcomes for AKI. For other complex acute medical conditions with high mortality, increased weekend mortality has been felt to be a consequence of reduced levels of staffing.1 In patients admitted with acute myocardial infarction on the weekend, higher mortality appears to be mediated by reduced access to invasive cardiac procedures.8,10 Conversely, weekend admissions to critical care units have not been associated with increased mortality, an observation perhaps attributable to more constant levels of access to staff and availability of medical procedures in these settings.15–17 Few studies have examined how timing of assessment or institution of treatment specific to the management of AKI affects clinical outcomes. Observational studies examining the effects of timing of nephrology consultation and institution of renal replacement therapy on clinical outcomes in patients with AKI have produced conflicting results.18–20 However, delays in appropriate diagnosis and management in several medical conditions (e.g., reperfusion for ST elevation myocardial infarction,10,21 early management of severe sepsis22) have been shown to affect clinical outcomes, suggesting that processes of acute medical care may be influential.
There are several reasons why we may have observed a higher risk of death among patients with AKI admitted on the weekend. On the basis of recorded diagnoses and procedures, patients admitted on a weekend appeared to be more severely ill than those admitted on a weekday. However, higher mortality with weekend admission persisted in analyses adjusted for demographic characteristics, recorded comorbidities, and provision of mechanical ventilation and across most of the acute medical conditions that co-existed with AKI.
The reasons for excess mortality among patients admitted with AKI on a weekend are uncertain, although delays in assessment, diagnosis, and management of other acute medical conditions on weekends have been previously described.9 We found that patients admitted with AKI on a weekend were less likely to receive dialysis than those admitted on a weekday, despite their greater severity of illness. In many centers across the United States, access to dialysis may be reduced during the weekend, and the availability of trained personnel may differ on weekends, particularly on Sundays.23,24 If nephrology consultation and the provision (and timing) of renal replacement therapy affect survival in the setting of AKI, improved weekend access to specialist care or dialysis could potentially reduce AKI-related mortality for patients admitted on weekend days; however, further research is required to test this hypothesis. Process-of-care factors may be accentuated in smaller hospitals where we observed the more pronounced increases in risk of death with weekend admission. Because small hospitals were more likely than large hospitals to transfer patients with AKI to another short-term hospital (6.2% versus 2.8% of admission with AKI), and patients who are transferred are likely sicker, the accentuated “weekend effect” in smaller hospitals may be greater than reported here (presumably having discharged a fraction of their sicker patients to medium-sized or larger hospitals).
Our study has several limitations. First, we identified our study population on the basis of the presence of International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes for AKI. These codes for AKI have high specificity but poor sensitivity.25 Although this may result in exclusion of some patients with AKI from our study, this is unlikely to produce selection bias because weekend and weekday admissions are unlikely to differ with respect to the coding of AKI. Indeed, if we failed to identify some patients with AKI (as we suspect), then we would also have underestimated the absolute number of deaths attributable to weekend admission with AKI. Second, classification of weekend admission was defined as a Saturday or Sunday admission and ignored the fact that the provision of health care services on a Friday evening or in the early morning hours on Monday (e.g., midnight to 6:00 a.m.) are likely more similar to those provided on a Saturday or Sunday, respectively. If relevant, the “peri-weekend” misclassification is likely to lead to underestimation of the excess risk of death among patients with weekend admission, thereby biasing our results toward the null. Third, we were only able to identify in-hospital mortality and may have misclassified the outcome of patients who died after transfer to another acute, intermediate, or skilled nursing facility. However, because the length of hospital stay was similar for weekend and weekday admissions, and discharge to intermediate care and skilled nursing facilities was more common among patients admitted on a weekend than on a weekday, these minor differences are unlikely to account for the observed associations. Fourth, despite multivariable adjustment, we cannot exclude residual confounding by unmeasured characteristics that may have influenced our results. However, the elevated adjusted rate of death with weekend admission across seven co-existing conditions strengthens our findings.
This study was conducted using a large administrative health care database. Although this data source provides a large sample of hospital admissions sampled from across the United States, there are limitations to the information available, and data on access to consultants, emergency room waiting times, intensive care unit admissions, and severity of illness scores are not included. Future studies that capture these relevant prognostic and health services utilization variables are required to better understand the relation between time of admission with AKI, management, and clinical outcomes. Given the nature of our study data, the underlying reasons for increased weekend mortality with AKI could not be determined. Further studies are needed to compare the effect of differences in clinical practice related to access and timing of diagnostic and therapeutic interventions for the management of AKI. Studies should focus on health practices amenable to improvement, including the provision of intravenous fluids and/or diuretics, diagnostic testing, and timing of nephrologist consultation and initiation of dialysis.
In conclusion, for patients hospitalized with AKI, mortality was significantly higher among patients admitted on a weekend as compared with those admitted on a weekday. This disparity was most evident among admissions with AKI in smaller hospitals. These findings highlight the need to further investigate the availability and timing of provision of diagnostic and therapeutic strategies to patients hospitalized with AKI.
Concise Methods
Data Source and Study Population
We performed this study using the Nationwide Inpatient Sample (NIS), the largest all-payer database of hospital inpatient stays that is publicly available in the United States. The NIS was developed as part of the Healthcare Cost and Utilization Project and contains data from 5 to 8 million hospital stays from approximately 1000 hospitals sampled each year to approximate a 20% stratified sample of U.S. hospitals. It includes information on all patients regardless of payer, including persons covered by Medicare, Medicaid, private insurance, and the uninsured. Inpatient stay records include clinical and resource use information typically available from hospital discharge abstracts, including ICD-9-CM codes for up to 15 diagnoses and 15 procedures for each admission. To ensure generalizability, the NIS relies on 60 hospital sampling strata with sampling weights provided to generate national estimates.
All admissions captured in the NIS databases from 2003 to 2006 were eligible for this study, with the exclusion of transfers from another acute care hospital and births. We identified admissions with AKI as a primary diagnosis (primary reason for admission to hospital) or with a secondary diagnosis of AKI. A diagnosis of AKI was based on the presence of ICD-9-CM codes according to a validated algorithm (Appendix 1). 25 Previously published algorithms of ICD-9-CM codes were used to identify seven other primary diagnoses of interest (sepsis, pneumonia, acute myocardial infarction, heart failure, gastrointestinal bleed, pancreatitis, or liver failure) for the admissions in which AKI was coded as a secondary diagnosis, as described previously (Appendix 1).13
Appendix 1.
ICD-9-CM codes used to define clinical conditions from NIS data from 2003 to 2006
| Condition | ICD-9-CM Codes |
|---|---|
| AKI | Diagnosis codes 584.5, 584.6, 584.7, 584.8, 584.9 |
| Dialysis | Diagnosis codes for AKI as above + V34.1, V560, V561, or procedure code 39.95 |
| Mechanical ventilation | Procedure codes 93.90, 93.92, 96.01, 96.04, 96.05, 96.70, 96.71, 96.72 |
| Sepsis | Diagnosis codes 038.x, 112.5, 112.81, 02.02, 79.07, 78.559 |
| Pneumonia | Diagnosis codes 460.x, 481, 482.x, 483.x, 484.x, 485, 486 |
| Acute myocardial infarction | Diagnosis codes 410.x |
| Heart failure | Diagnosis codes 428.x |
| Gastrointestinal hemorrhage | Diagnosis codes 578.x |
| Acute pancreatitis | Diagnosis code 577.0 |
| Liver failure | Diagnosis code 570 |
Study Variables
The primary outcome variable was total in-hospital mortality. In-hospital mortality within 3 days of admission was also examined. The primary independent variable was hospital admission on a weekend (Saturday or Sunday) as captured by the NIS. Covariates included patient demographics including age, sex, and race (non-Hispanic white, non-Hispanic black, Hispanic, Asian, Native American, other, and missing). We used the Deyo modification of the Charlson index to estimate comorbidity26,27 and ICD-9-CM codes to identify procedures performed during the hospital admission (mechanical ventilation and dialysis) (Appendix 1). Hospital characteristics included hospital teaching status (teaching and nonteaching) and hospital size as categorized by the NIS (smaller: 1 to 249 beds, medium-sized: 25 to 374 beds, larger: 50 to >450 beds). Hospital size categories are established by the NIS for nationwide comparison on the basis of the number of hospital beds and are thus specific to the hospital's region, location, and teaching status. Bed size categories are chosen so that approximately one-third of the hospitals in a given region, location, and teaching status combination fall within each category.28
Statistical Analysis
We performed all analyses with commercially available statistical software (STATA version 10, College Station, TX) using survey procedures to account for the survey design of the NIS. Characteristics of weekend and weekday admissions were compared with the χ2 test for categorical variables, the t test for normally distributed variables, and the Wilcoxon rank-sum test for non-normally distributed variables. We compared differences in in-hospital mortality among weekend and weekday admissions by day 3 after admission and for the total hospital admission. For our primary analysis, we used logistic regression models adjusted for age, sex, race, Charlson comorbidity index, and use of mechanical ventilation (as a proxy for critical illness) to determine the associations between weekend admission and in-hospital mortality for admissions with a primary diagnosis of AKI. Because we hypothesized that hospital characteristics might modify the association of weekend admission with mortality, we also assessed models including terms for interactions between weekend admission and hospital size and weekend admission and teaching status. To explore the effect of weekend admission in which AKI was coded as a secondary diagnosis, we also performed stratified analyses according to seven accompanying primary diagnoses (sepsis, pneumonia, acute myocardial infarction, heart failure, gastrointestinal hemorrhage, acute pancreatitis, or liver failure) where they co-existed with AKI.
Disclosures
None.
Acknowledgments
Dr. James was a visiting researcher at Stanford University at the time the study was performed and was supported by clinical research trainee awards from the Kidney Foundation of Canada and Canadian Institutes for Health Research and the Alberta Heritage Foundation for Medical Research. Drs. Tonelli and Hemmelgarn were supported by awards from the Alberta Heritage Foundation for Medical Research; and Drs. Wald, Bell, Tonelli, and Hemmelgarn were supported by awards from the Canadian Institutes for Health Research. Dr. Chertow was supported by awards from the U.S. National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related editorial, “Variations in Mortality among Hospitalizations for Acute Kidney Injury,” on pages 728–731.
REFERENCES
- 1. Bell CM, Redelmeier DA: Mortality among patients admitted to hospital on weekends as compared with weekdays. N Engl J Med 345: 633–638, 2001. [DOI] [PubMed] [Google Scholar]
- 2. Cram P, Hillis SL, Barnett M: Effects of weekend admission and hospital teaching status on in-hospital mortality. Am J Med 117: 151–157, 2004. [DOI] [PubMed] [Google Scholar]
- 3. Barba R, Losa JE, Belasco M: Mortality among adult patients admitted to the hospital on weekends. Eur J Intern Med 17: 322–324, 2006. [DOI] [PubMed] [Google Scholar]
- 4. Saposnik G, Baibergenova A, Bayer N: Weekends: A dangerous time for having a stroke. Stroke 38: 1211–1215, 2007. [DOI] [PubMed] [Google Scholar]
- 5. Clark K, Normile LB: Influence of time-to-interventions for emergency department critical care patients on hospital mortality. J Emerg Nurs 33: 6–13, 2007. [DOI] [PubMed] [Google Scholar]
- 6. Foss NB, Kehlet H: Short-term mortality in hip fracture patients admitted during weekends and holidays. Br J Anaesth 96: 450–454, 2006. [DOI] [PubMed] [Google Scholar]
- 7. Hasegawa Y, Yoneda Y, Okuda S, Hamada R, Toyota A, Gotoh J, Watanabe M, Okada Y, Ikeda K, Ibayashi S: The effect of weekends and holidays on stroke outcome in acute stroke units. Cerebrovasc Dis 20: 325–331, 2005. [DOI] [PubMed] [Google Scholar]
- 8. Kostis WJ, Demissie K, Marcella SW, Shao YH, Wilson AC, Moreyra AE: Weekend versus weekday admission and mortality from myocardial infarction. N Engl J Med 356: 1099–1109, 2007. [DOI] [PubMed] [Google Scholar]
- 9. Bell CM, Redelmeier DA: Waiting for urgent procedures on the weekend among emergently hospitalized patients. Am J Med 117: 175–181, 2004. [DOI] [PubMed] [Google Scholar]
- 10. Magid DJ, Wang Y, Herrin J, McNamara RL, Bradley EH, Curtis JP, Pollack CV, French WJ, Blaney ME, Krumholz HM: Relationship between time of day, day of week, timeliness of reperfusion, and in-hospital mortality for patients with acute ST-segment elevation myocardial infarction. JAMA 294: 803, 2005. [DOI] [PubMed] [Google Scholar]
- 11. Halm EA, Chassin MR: Why do hospital death rates vary? N Engl J Med 345: 692–694, 2001. [DOI] [PubMed] [Google Scholar]
- 12. Pannu N, Klarenbach S, Wiebe N, Manns B, Tonelli M: Renal replacement therapy in patients with acute renal failure: A systematic review. JAMA 299: 793–805, 2008. [DOI] [PubMed] [Google Scholar]
- 13. Waikarr SS, Curhan GC, Wald R, McCarthy EP, Chertow GM: Declining mortality in patients with acute renal failure, 1998 to 2002. J Am Soc Nephrol 17: 1143–1150, 2006. [DOI] [PubMed] [Google Scholar]
- 14. Xue JL, Daniels F, Star RA, Kimmel PL, Eggers PW, Molitoris BA, Himmelgarb J, Collins AJ: Incidence and mortality of acute renal failure in Medicare beneficiaries, 1992 to 2001. J Am Soc Nephrol 17: 1142, 2006. [DOI] [PubMed] [Google Scholar]
- 15. Luyt CE, Combes A, Aegerter P, Guidet B, Trouillet JL, Gibert C, Chastre J: Mortality among patients admitted to intensive care units during weekday day shifts compared with “off” hours. Crit Care Med 35: 3–11, 2007. [DOI] [PubMed] [Google Scholar]
- 16. Laupland KB, Shahpori R, Kirkpatrick AW, Stelfox HT: Hospital mortality among adults admitted to and discharged from intensive care on weekends and evenings. J Crit Care 23: 317–324, 2008. [DOI] [PubMed] [Google Scholar]
- 17. Wunsch H, Mapstone J, Brady T, Hanks R, Rowan K: Hospital mortality associated with day and time of admission to intensive care units. Intensive Care Med 30: 895–901, 2004. [DOI] [PubMed] [Google Scholar]
- 18. Seabra VF, Balk EM, Liangos O, Sosa AM, Cendoroglo M, Jaber BL: Timing of renal replacement therapy initiation in acute renal failure: A meta-analysis. Am J Kidney Dis 52: 272–284, 2008. [DOI] [PubMed] [Google Scholar]
- 19. Bouman CS, Oudes-Van Straaten HM, Tijssen JG, Zandstra DF, Kesecioglu L: Effects of early high-volume continuous venovenous hemofiltration on survival and recovery of renal function in intensive care patients with acute renal failure: A prospective, randomized trial. Crit Care Med 30: 2205–2211, 2002. [DOI] [PubMed] [Google Scholar]
- 20. Liu KD, Himmelfarb J, Paganini EP, Ikizler A, Soroko S, Mehta RL, Chertow GM: Timing of initiation of dialysis in critically ill patients with acute kidney injury. Clin J Am Soc Nephrol 1: 915–919, 2006. [DOI] [PubMed] [Google Scholar]
- 21. Fibrinolytic Therapy Trialist (FTT) Collaborative Group: Indications for fibrinolytic therapy in suspected acute myocardial infarction: Collaborative overview of early mortality and major morbidity results from all randomized trials of more than 1000 patients. Lancet 343: 311–322, 1994. [PubMed] [Google Scholar]
- 22. Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M: Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345: 1368–1377, 2001. [DOI] [PubMed] [Google Scholar]
- 23. The VA/NIH Acute Renal Failure Trial Network: Intensity of renal support in critically ill patients with acute kidney injury. N Engl J Med 359: 7–20, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Overberger P, Pesacreta M, Palevsky PM: Management of renal replacement therapy in acute kidney injury: A survey of practitioner prescribing practices. Clin J Am Soc Nephrol 2: 623–630, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Waikarr SS, Wald R, Chertow GM, Curhan G, Winkelmayer WC, Liangos O, Sosa MA, Jaber BL: Validity of International Classification of Diseases, Ninth Revision, Clinical Modification codes for acute renal failure. J Am Soc Nephrol 17: 1688–1694, 2006. [DOI] [PubMed] [Google Scholar]
- 26. Charlson ME, Pompei P, Ales KL, MacKenzie CR: A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chron Dis 40: 373–383, 1987. [DOI] [PubMed] [Google Scholar]
- 27. Deyo RA, Cherkin DC, Ciol MA: Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45: 613–619, 1992. [DOI] [PubMed] [Google Scholar]
- 28. Healthcare Cost and Utilization Project: Introduction to the HCUP Nationwide Inpatient Sample. Available online at http://www.hcup-us.ahrg.gov/db/nation/nis/2006NIS_INTRODUCTION.pdf Accessed March 2, 2009