Abstract
Background
Little is known about the effect of different types of inpatient rehabilitation on outcomes of patients undergoing lower extremity amputation for nontraumatic reasons.
Objective
To compare outcomes between patients who received inpatient rehabilitation on specific rehabilitation bed units (specialized) to patients who received rehabilitation on general medical/surgical units (generalized) during the acute postoperative period.
Methods
This was an observational study including 1339 veterans who underwent lower extremity amputation between October 1, 2002 and September 30, 2004. Data were compiled from 9 administrative databases from the Veterans Health Administration. Propensity score risk adjustment methodology was used to reduce selection bias in looking at the effect of type of rehabilitation on outcomes (1-year survival, home discharge from the hospital, prescription of a prosthetic limb within 1 year post surgery, and improvement in physical functioning at rehabilitation discharge).
Results
After applying propensity score risk adjustment, there was strong evidence that patients who received specialized versus generalized rehabilitation were more likely to be discharged home (risk difference = 0.10), receive a prescription for a prosthetic limb (risk difference = 0.13), and improve physical functioning (gains on average 6.2 points higher). Specialized patients had higher 1-year survival (risk difference = 0.05), but the difference was not statistically significant. The sensitivity analysis demonstrated our findings to be unaffected by a moderately strong amount of unmeasured confounding.
Conclusions
Receipt of specialized compared with generalized rehabilitation during the acute postoperative inpatient period was associated with better outcomes. Future studies will need to look at different intensity, timing, and location of rehabilitation services.
Keywords: rehabilitation, lower extremity, amputation, outcome assessment, selection bias
Studying outcomes after rehabilitation is critical. For persons with trauma-related amputations, Pezzin et al found that inpatient rehabilitation led to better outcomes.1 Unfortunately, outcomes after rehabilitation for persons with lower extremity (LE) amputation for nontraumatic etiologies are under studied with little knowledge about how the types or intensities of rehabilitation influence outcomes.
We found that for patients with LE amputation, inpatient rehabilitation compared with no inpatient rehabilitation (regardless of type) during the acute postoperative period was associated with improved 1-year survival and greater likelihood of home discharge from the hospital.2 In this study, we determine if there are incremental benefits of receiving rehabilitation on specialized rehabilitation bed units (SRUs) (specialized) compared with rehabilitation on general medical/ surgical units (generalized) among those who received inpatient rehabilitation during the acute postoperative period.
Patients who received generalized rehabilitation may have one to many sessions while hospitalized, therapy may vary from intermittent to regular sessions, and functional restoration is not the primary focus. Conversely, specialized rehabilitation occurs in designated units, which consist of a cluster of beds located in a distinct area in the hospital specifically accredited for rehabilitation services by the Commission on Accreditation of Rehabilitation Facilities (CARF). Restorative therapy typically occurs daily, with rehabilitation the primary focus. To achieve accreditation, SRUs must meet CARF’s explicitly defined standards developed to ensure high quality services. In the Veterans Health Administration (VHA), subacute and acute rehabilitation beds are considered similar, and both were categorized as SRUs if they were CARF accredited for LE amputees.
Our objective was to determine the effect of receiving specialized versus generalized rehabilitation after LE amputation on 4 patient outcomes: 1-year survival, discharge home from the hospital, prescription of a prosthetic limb within 1 year post surgery, and improvement in physical functioning at rehabilitation discharge. Type of rehabilitation received can be influenced by patient- and facility-level characteristics and clinical practice variations, which may be associated with outcomes. Conclusions drawn about outcome differences that do not adjust for these factors suffer from selection bias and may be inaccurate. To adjust for selection bias due to measured patient- and facility-level characteristics, we applied propensity score (p score) risk adjustment methods.3 We conducted a sensitivity analysis to determine how the presence of an unmeasured characteristic with a moderately strong effect on the outcome and on the probability of receiving specialized would affect our findings.4,5
METHODS
This observational study was approved by the Institutional Review Boards at the University of Pennsylvania in Philadelphia, Pennsylvania, the Samuel S. Stratton Veterans Affairs Medical Center (VAMC) in Albany, New York, and the Kansas City VAMC in Kansas City, Missouri.
Databases Description
Data were obtained from 9 VHA administrative databases used to track the health status and health care utilization of veterans. The databases included 4 inpatient datasets called the Patient Treatment Files (PTF) (main, procedure, bed section, surgery),6 2 Outpatient Care Files (visit, event),7 the Beneficiary Identification Record Locator System death file,8 the National Prosthetics Patient Database,9 and the Functional Status and Outcomes Database (FSOD).10 Description of the databases and our data extraction have been described previously.11-14
Subjects
Patients were included from 92 VAMCs with hospital discharge dates between October 1, 2002 and September 30, 2004, for a new transtibial or transfemoral amputation (surgical procedure codes: 84.10, 84.13–84.19, and 84.91).15 Cases were excluded if the amputation involved toes only or if there was a record of a previous LE amputation within 12 months preceding the amputation of interest. We linked records from the PTF bed section file with admission dates within 1 day of the main hospitalization discharge date to capture the entire acute amputation hospitalization.
We identified a total of 4727 veterans with LE amputations. Seven patients were then excluded because their records lacked information. Here, we focused only on inpatient rehabilitation (episodes with distinct rehabilitation admission and discharge dates) provided during the acute postoperative period. Our purpose was to define the most homogenous cohort that we could to compare the outcomes of generalized to specialized patients. Thus, the following patients were excluded: 1255 with no evidence of inpatient rehabilitation, 304 who began inpatient rehabilitation before surgery, 206 who had inpatient rehabilitation extending beyond or beginning more than 1 day after the index hospitalization discharge date, 1216 who received inpatient rehabilitation in the acute postoperative period and after the index hospitalization discharge date, and 321 with missing inpatient rehabilitation discharge dates. Among the remaining 1418 patients who received inpatient rehabilitation during the acute postoperative period only, 79 patients were missing initial cognitive or motor functional independence measure (FIM)16 scores and were also excluded. There were 1339 patients included in the analyses, unless otherwise specified (Fig. 1).
FIGURE 1.
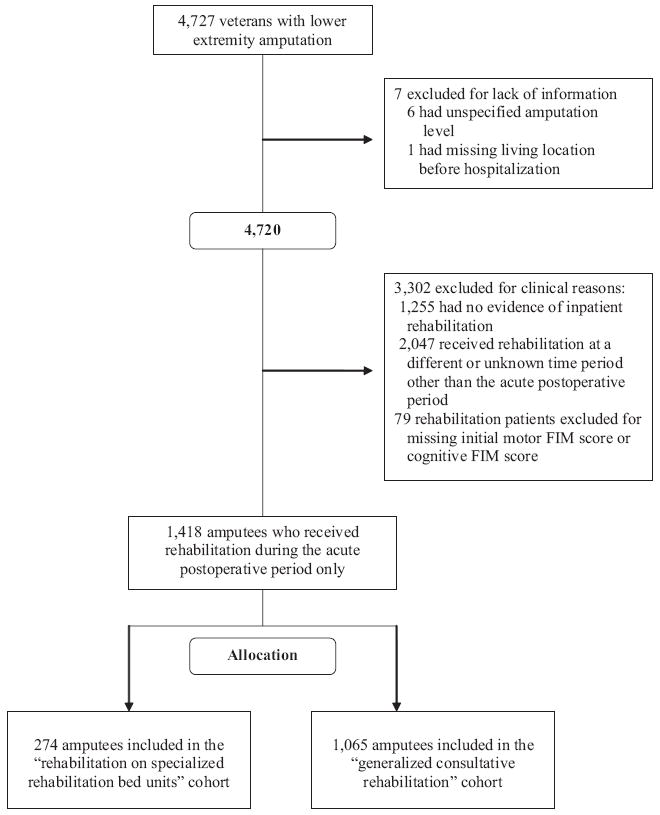
Flow diagram of veterans with lower extremity amputations included in the study.
Variables
Patient-level characteristics included age, gender, marital status (married, not married), and living location before the hospitalization (extended care, home, hospital). Amputation level consisted of 4 categories (unilateral transtibial, unilateral transfemoral, bilateral transtibial, bilateral transfemoral). Patients with a transtibial and transfemoral amputation were combined and classified as bilateral transfemoral amputees because of low prevalence and because functional prognosis declines sharply once the knee is lost.17
Diagnoses incorporated both amputation etiologies and comorbidities, which were identified using International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) diagnosis codes from outpatient care files 3 months before hospital admission and from the main and bed section files up to the surgical date. Ten of the original 12 etiologies were included in our analysis.11 Congenital deformity and lower-limb cancer had insufficient prevalence. We used the 2003 version of the Elixhauser comorbidity measure that distinguishes hypertension from hypertension with complication.18,19 No cases had the ICD-9-CM code for obesity.
Length of time from hospital admission to the surgical date and from the surgical date to the rehabilitation admission date (both in days), intensive care unit admission, total number of bed sections, and selected procedures13 approximated patient complexity. Initial motor and cognitive FIM scores16 captured physical and cognitive and communication function,20 respectively, during rehabilitation admission. The FIM is the standard measure of functional status used in inpatient rehabilitation in the VHA.
Facility-level characteristics included geographic region (Veterans Integrated Service Networks mapped into Centers for Medicare and Medicaid Service regions: Northeast, Southeast, Midwest, South Central, Pacific Mountain) and hospital bed size (≤126, 127–244, 245–362, >362). A year variable was to account for any practice pattern changes over time.
Inpatient rehabilitation was determined using FSOD data. Services were classified according to the “Time, Place, and Type” framework, developed and described previously,2 to account for the substantial variability in when services began, where services occurred, and what types of services were received. “Time” is measured relative to the amputation and hospital admission and discharge dates (acute preoperative, acute postoperative, postacute periods). “Place” reflects setting (inpatient, outpatient, home). “Type” refers to the types of services received (specialized, generalized).
This study, which restricted time to the acute postoperative period and place to the inpatient setting, represented the most common care pattern received among veteran amputees.2 Only type of service (specialized vs. generalized) varied.
Description of Inpatient Rehabilitation
Once the patient is admitted to the rehabilitation continuum, a team of rehabilitation professionals assesses the patient’s physical and cognitive status, measured according to motor and cognitive FIM scores, respectively,21 over a span of up to 3 days to develop a rehabilitation care plan. The plan options may range from no further treatment beyond the initial assessment to admission onto a SRU. If veterans are referred for rehabilitation, 2 types are available: generalized or specialized. Once the patient has either met the rehabilitation goals or has achieved maximum rehabilitation potential, the patient is discharged from the rehabilitation continuum.
Outcome Measures
Patients were followed from the surgical date through the 1-year amputation anniversary. Outcomes included 1-year survival, discharge home from the hospitalization, prescription of a prosthetic limb within 1 year post amputation, and improvement in physical functioning at rehabilitation discharge. The PTF main and Beneficiary Identification Record Locator System files were used to acquire mortality information and our methods have been described previously.13
Discharge home from the hospitalization compared with other settings (hospital, extended care, death, other) was determined by the PTF main. Because our study end point was 1 year post amputation, patients still hospitalized at that point were coded as “hospital.” Prescription of a prosthetic limb within 1 year post amputation was determined from the National Prosthetics Patient Database. Change in physical functioning at rehabilitation discharge was obtained by subtracting the initial from discharge motor FIM scores in the FSOD.
Statistical Methods
Propensity Score Risk-Adjustment Method
Because patients were not randomized, patients who received specialized may not have comparable characteristics to those who received generalized, creating selection bias. In an attempt to control for selection bias, we collected information on characteristics that are important for deciding which patients receive specialized versus generalized and then used p score risk-adjustment methods3; p score is the probability of a patient receiving specialized, given the patient’s observed characteristics. We estimated p score by a logistic regression model with the receipt of specialized as the dependent variable and all measured patient- and facility-level characteristics as independent variables. We tested the significance of interactions between amputation level and all continuous variables, as well as squared and cubic forms of the continuous variables, and added the significant interaction terms to the model. The p score has the property that if we group patients with similar p scores, patients who receive specialized within the p score group will have a similar distribution of measured characteristics as patients who receive generalized within the p score group.3,22-24 Consequently, by making comparisons of specialized versus generalized within strata of patients with similar p scores, any difference in outcomes between specialized and generalized patients will not be due to differences in measured characteristics.3,22-24 This method thus controls for selection bias due to measured patient- and facility-level characteristics. It does not control for selection bias due to unmeasured characteristics. We attempted to minimize this type of selection bias by collecting information on as many important patient- and facility-level characteristics as possible.25
We stratified patients into quintiles by their estimated p scores. If there were not at least 5 cases in the specialized or generalized groups in each quintile, patients could not be compared accurately in this quintile–the treatment groups lacked common support.23 If this occurred, we removed the patients in the quintile(s) and regrouped the remaining patients. This was performed until common support was achieved. Our subsequent analyses applied only to patients with p scores that achieved common support.
We then determined the degree to which balance was improved by stratification on the p score quintile. Balance refers to how similar the compared groups are on patient- and facility-level characteristics. To test whether stratification on p score quintile balanced for each characteristic, we fit a linear or logistic regression model, depending on the type of variable, with the patient- and facility-level characteristic as the dependent variable (all variables from Table 1) and treatment group and p score quintiles as independent variables.24 If the coefficient on treatment group was not statistically significant for a given characteristic, then there was no evidence of a difference within p score quintiles between generalized and specialized patients on that characteristic (no evidence of imbalance after p score adjustment). If the coefficient on treatment group was significant, then we included the characteristic as a predictor in the outcome models.22,26 We also assessed balanced by comparing standardized differences for patient- and facility-level characteristics before and after p score stratification.27 Standardized differences less than 20 are thought to represent good balance of a characteristic.4,27
TABLE 1.
Baseline Characteristics According to the Receipt of Inpatient Rehabilitation Services
| Treatment* | Control | |
|---|---|---|
| Received Rehabilitation on Specialized Rehabilitation Bed Units (n = 274) | Received General Rehabilitation on Medical or Surgical Units (n = 1065) | |
| Demographics | ||
| Age, yrs‡ | ||
| Average | 65.0 | 67.5 |
| Range | 41–88 | 35–97 |
| Gender | ||
| Male | 274 (100.0) | 1053 (98.9) |
| Female | 0 (0.0) | 12 (1.1) |
| Marital status | ||
| Married | 122 (44.5) | 497 (46.7) |
| Not married | 152 (55.5) | 568 (53.3) |
| Living location before the hospitalization† | ||
| Extended care | 8 (2.9) | 69 (6.5) |
| Home | 261 (95.3) | 966 (90.7) |
| Hospital | 5 (1.8) | 30 (2.8) |
| Amputation level‡ | ||
| Unilateral transtibial | 163 (59.5) | 510 (47.9) |
| Unilateral transfemoral | 99 (36.1) | 451 (42.4) |
| Bilateral transtibial | 6 (2.1) | 31 (2.9) |
| Bilateral transfemoral | 6 (2.1) | 73 (6.9) |
| Contributing etiologies | ||
| Chronic osteomyelitis | 12 (4.4) | 80 (7.5) |
| Device infection† | 39 (14.2) | 107 (10.1) |
| Diabetes mellitus type I | 50 (18.3) | 160 (15.0) |
| Diabetes mellitus type II‡ | 202 (73.7) | 690 (64.8) |
| Local significant infection | 210 (76.6) | 817 (76.7) |
| Peripheral vascular disease | 235 (85.8) | 934 (87.7) |
| Previous amputation complication | 26 (9.5) | 99 (9.3) |
| Skin breakdown | 169 (61.7) | 692 (65.0) |
| Systemic sepsis† | 18 (6.6) | 116 (10.9) |
| Trauma | 42 (15.3) | 140 (13.2) |
| Comorbidities | ||
| AIDS | 1 (0.4) | 12 (1.1) |
| Alcohol abuse | 19 (6.9) | 57 (5.4) |
| Arrhythmias | 41 (15.0) | 178 (16.7) |
| Chronic blood loss anemia | 6 (2.2) | 19 (1.8) |
| Chronic pulmonary disease | 45 (16.4) | 230 (21.6) |
| Coagulopathy | 13 (4.7) | 56 (5.3) |
| Congestive heart failure | 53 (19.3) | 242 (22.7) |
| Deficiency anemias | 48 (17.5) | 245 (23.0) |
| Depression | 30 (11.0) | 95 (8.9) |
| Drug abuse | 7 (2.6) | 21 (2.0) |
| Fluid and electrolyte disorders | 58 (21.2) | 213 (20.0) |
| Hypertension | 182 (66.4) | 687 (64.5) |
| Hypertension with complication | 3 (1.1) | 3 (0.3) |
| Hypothyroidism | 9 (3.3) | 38 (3.6) |
| Liver disease | 15 (5.5) | 37 (3.5) |
| Lymphoma | 2 (0.7) | 10 (0.9) |
| Metastatic cancer | 7 (2.6) | 22 (2.1) |
| Other neurological disorders† | 3 (1.1) | 36 (3.4) |
| Paralysis† | 5 (1.8) | 57 (5.4) |
| Peptic ulcer | 4 (1.5) | 11 (1.0) |
| Psychoses | 12 (4.4) | 80 (7.5) |
| Pulmonary circulation disease | 3 (1.1) | 8 (0.8) |
| Renal failure† | 31 (11.3) | 188 (17.7) |
| Rheumatoid arthritis | 5 (1.8) | 9 (0.9) |
| Solid tumor without metastasis† | 16 (5.8) | 110 (10.3) |
| Valvular disease | 7 (2.6) | 48 (4.5) |
| Weight loss | 16 (5.8) | 55 (5.2) |
| Baseline complexity | ||
| Time from hospital admission to surgery‡ | ||
| Average | 10.4 | 7.9 |
| Range | 1–109 | 1–198 |
| Time from surgery to rehabilitation admission§ | ||
| Average | 10.6 | 5.0 |
| Range | 1–132 | 1–176 |
| ICU admission | ||
| No. bed sections§ | 105 (38.3) | 384 (36.1) |
| Average | 3.5 | 2.3 |
| Range | 1–18 | 1–15 |
| Procedures | ||
| Active pulmonary pathology† | 0 (0.0) | 15 (1.4) |
| Acute central nervous system | 24 (8.8) | 93 (8.7) |
| Ongoing active cardiac pathology | 41 (15.0) | 118 (11.1) |
| Ongoing wound problems | 18 (6.6) | 71 (6.7) |
| Serious nutritional compromise‡ | 2 (0.7) | 53 (5.0) |
| Severe renal disease† | 13 (4.7) | 94 (8.8) |
| Substance abuse or mental health issues† | 8 (2.9) | 11 (1.0) |
| Functional status | ||
| Initial motor FIM score§ | ||
| Average | 48.7 | 36.4 |
| Range | 13–78 | 13–91 |
| Initial cognitive FIM score§ | ||
| Average | 28.9 | 25.6 |
| Range | 5–35 | 5–35 |
| Hospital characteristics | ||
| Regions | ||
| Northeast | 40 (14.6) | 174 (16.3) |
| Southeast | 74 (27.0) | 361 (33.9) |
| Midwest | 44 (16.1) | 142 (13.3) |
| South Central | 68 (24.8) | 240 (22.5) |
| Mountain Pacific | 48 (17.5) | 148 (13.9) |
| Total bed size§ | ||
| Bed size ≤126 | 25 (9.1) | 321 (30.1) |
| Bed size 127–244 | 78 (28.5) | 285 (26.8) |
| Bed size 245–362 | 155 (56.6) | 368 (34.6) |
| Bed size >362 | 16 (5.8) | 91 (8.5) |
Numbers in parentheses are percentages of column totals for gender, marital status, living location before hospitalization, amputation level, regions, and total bed size.
Comparisons were treatment group (rehabilitation on specialized rehabilitation bed units) versus control group (generalized consultative rehabilitation).
P < 0.05;
P < 0.01;
P < 0.0001.
Modeling Outcome Differences
We compared outcomes of specialized versus generalized by regression models that adjust for p score quintile. By adjusting for p score quintile in the model, we are comparing specialized and generalized patients within p score quintiles. This greatly reduces selection bias due to measured patient- and facility-level characteristics because these characteristics are balanced between the groups within p score quintiles. Because patients are clustered into facilities, we included facilities as random effects in the outcome models to properly account for clustering.28 Specifically, the models contained fixed effects for treatment group, p score quintiles, any variable that was not balanced within p score quintiles, and random effects for the facilities. Linear mixed effects regression models were used for all the outcomes.
Sensitivity Analysis
To assess the possible impact of an unmeasured characteristic, we conducted a sensitivity analysis on the 3 binary outcomes (home discharge, prosthetic prescription, survival).4,5 Propensity risk score adjustment methods were performed using SAS Version 9.1,29 and the sensitivity analysis was conducted using R.30
RESULTS
Patient Characteristics
There were 1339 veteran amputees who received inpatient rehabilitation during the acute postoperative period. Over 99% were men, average age was 67.0 years (SD = 11.3), and half the amputations were unilateral transtibial (50.3%). Problems with peripheral circulation (87.3%) and diabetes mellitus type II (66.6%) were the most common amputation etiologies. Traumatic injury occurred in only a few cases (13.6%). Patients were hospitalized for an average of 31.1 days (SD = 37.0), 22.9 days (SD = 31.0) during the acute postoperative period, and were treated on an average of 2.6 bed sections (SD = 2.0). One patient was still hospitalized 1 year after amputation. Average rehabilitation treatment lasted 16.5 days (SD = 10.0) for the 274 patients (20.5%) receiving specialized and 11.4 days (SD = 20.3) for the 1065 patients (79.5%) receiving generalized (P < 0.0001).
Baseline characteristics of patients receiving specialized and generalized are shown in Table 1. Compared with patients who received generalized, patients who received specialized were on average younger and more likely to have lived at home before amputation, have a unilateral transtibial amputation, and have been provided rehabilitation services in hospitals with 127 to 362 beds. They also had more days between hospital admission and amputation, as well as from surgery to rehabilitation admission, and were provided services in more bed sections. Moreover, these patients had higher initial cognitive and motor FIM scores. Patients who received generalized had more amputation etiologies and comorbidities.
Propensity Adjustment Models
We estimated p scores and calculated p score quintiles. Common support was not initially achieved. The first 2 quintiles each contained <5 patients receiving specialized, so all cases in those quintiles were removed (535 cases), and 5 new p score quintiles were recalculated based on estimated p scores of the remaining 804 cases. Common support was then achieved. Comparing the 535 patients whose p scores were too low to be included in the analysis to the 804 remaining patients, the patients who were excluded were generally older, more likely to be admitted to the hospital from extended care, have unilateral transfemoral amputations, particular comorbidities such as chronic pulmonary disease, paralysis, and other neurologic disorders, and have undergone procedures for serious nutritional compromise. This suggests that the excluded patients were sicker than the included ones. Patients who are too frail to benefit from intensive rehabilitation or who are highly functional are generally not given specialized rehabilitation. Our analysis only applies to patients in the middle band of functionality who have a higher likelihood of receiving specialized rehabilitation.
Linear and logistic regression models were run to assess whether there were differences in patient- and facility-level characteristics between specialized and generalized patients within p score quintiles. For all characteristics, the P values for the tests were >0.05, indicating there was no evidence of imbalance on any characteristic within p score quintiles between groups. Table 2 compares the P values from these tests to the P values from Table 1 that compares all specialized to all generalized patients for several of the statistically significant variables from Table 1. Table 2 shows that by comparing specialized and generalized patients within p score quintiles, selection bias due to important characteristics such as initial cognitive FIM score and time from surgery to rehabilitation admission is greatly reduced. Figure 2 illustrates the standardized difference before and after propensity risk adjustment. The propensity adjustment has greatly reduced selection bias. After stratification on the p score, all variables have standardized differences less than 10%, indicating the selection bias due to measured characteristics has been greatly reduced.
TABLE 2.
Comparison of P Values
| Variable | P Comparing all Specialized to all Generalized Patients | P Comparing Specialized to Generalized Patients Within P-Score Quintiles |
|---|---|---|
| Living location before the hospitalization: home | 0.047 | 0.51 |
| Amputation level: Bilateral trans-Femoral | 0.001 | 0.99 |
| Diabetes mellitus type II | 0.005 | 0.55 |
| Systemic sepsis | 0.034 | 0.64 |
| Paralysis | 0.013 | 0.67 |
| Time from hospital admission to Surgery | 0.009 | 0.95 |
| Time from surgery to rehabilitation admission | <0.0001 | 0.28 |
| No. bed sections | <0.0001 | 0.26 |
| Initial cognitive FIM score | <0.0001 | 0.82 |
FIGURE 2.
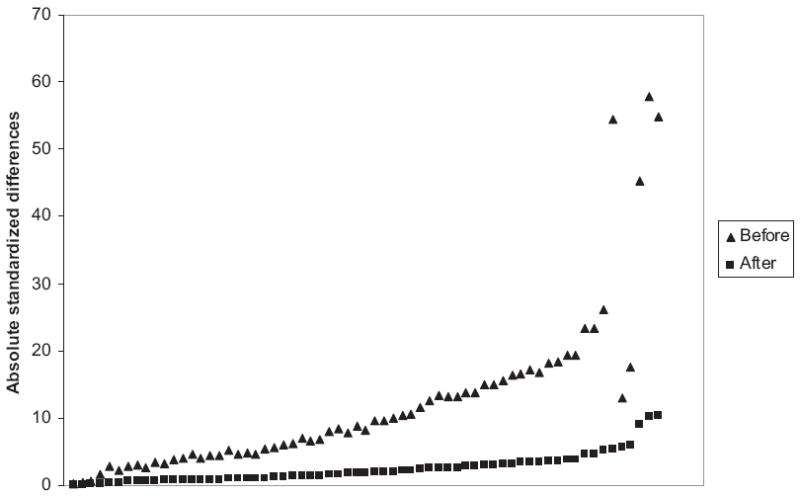
Standardized differences before and after propensity risk adjustment methodology. The propensity adjustment has substantially reduced selection bias. The variables with the largest standardized difference include bed size ≤126, number of bed sections, bed size 245 to 362, time from hospital admission to surgery, unilateral transfemoral amputation, and time from surgery to rehabilitation admission.
Outcome Differences
We first considered the raw differences between specialized and generalized patients without adjusting for patient- and facility-level characteristics. Overall, patients who received specialized had better outcomes (Table 3). Over 90% of patients who received specialized survived to 1 year post surgery compared with 76% of generalized patients. Similarly, a higher percentage of patients who received specialized compared with generalized were discharged home from the hospital (83.9% vs. 72.7%) and received a prescription for a prosthetic limb within 1 year post surgery (39.8% vs. 18.6%). Patients who received specialized compared with generalized achieved a greater average improvement in physical functioning (18.7 vs. 9.8 motor FIM points).
TABLE 3.
Frequency and Unadjusted and Adjusted Outcomes
| N (%)* | Adjusted Risk (Specialized to Generalized) | |
|---|---|---|
| Specialized | ||
| 1-year survival | 250 (91.2)§ | 0.05 (−0.02 to 0.12) |
| Home discharge | 230 (83.9)§ | 0.10 (0.02-0.18)† |
| Prescription of a prosthetic limb | 109 (39.8)§ | 0.13 (0.04-0.21)§ |
| Improvement in physical functioning | Average = 18.7§ | Gain 6.2 points§ |
| Generalized consultative | ||
| 1-year survival | 805 (75.6) | |
| Home discharge | 774 (72.7) | |
| Prescription of a prosthetic limb | 198 (18.6) | |
| Improvement in physical functioning | Average = 9.8 |
Data are presented as risk difference (95% CI) unless otherwise specified.
Comparisons were treatment group (rehabilitation on specialized rehabilitation bed units) versus control group (generalized consultative).
P < 0.05;
P < 0.01;
P < 0.0001.
To control for selection bias using the p score risk-adjustment method, we added dummy variables for the p score quintiles to the outcome models as well as random effects for facilities to account for clustering. When controlling for p score quintile, specialized patients continued to generally have better outcomes than generalized patients. Patients receiving specialized were more likely to be discharged home [risk difference = 0.10, 95% confidence interval (CI): 0.02–0.18] and to receive a prescription for a prosthetic limb (risk difference = 0.13, 95% CI: 0.04–0.21) compared with patients receiving generalized. Patients receiving specialized had higher average gains in physical functioning (gain of 6.2 points on a 78-point scale, 95% CI: 3.6–8.8). Patients receiving specialized were estimated to have a 0.05 higher survival rate, but the difference was not statistically significant. To allow for different effects in different p score quintiles, we added interactions between p score quintile and specialized to the outcome models and computed the average risk difference across the 5 quintiles. We obtained similar estimates of the risk differences as when we did not include the interactions (0.11 for home discharge, 0.06 for prosthetic limb prescription, and 0.08 for 1-year survival).
To consider the sensitivity of our findings to there being a moderately strong unmeasured confounder, we consider a binary unmeasured confounder that occurs in either 20% or 80% of the population and that would triple both the odds of receiving specialized and having a successful outcome. Taking into account such an unmeasured confounder for the binary outcomes, we would still estimate that specialized has a positive effect on each outcome and the estimated effect would still be statistically significant for home discharge and prosthetic limb prescription.
DISCUSSION
The goal of our study was to estimate the effect of receiving inpatient rehabilitation on SRUs compared with generalized consultation rehabilitation on general medical/surgical units. We found that for veterans after LE amputation, there were incremental benefits of receiving specialized compared with generalized during the acute postoperative period. Veterans receiving specialized rehabilitation were more likely to be discharged home from the hospital and to receive a prescription for a prosthetic limb within 1 year post amputation. Most noticeably, these patients had a 33% greater improvement in physical functioning at rehabilitation discharge. It is noteworthy that only 20.5% of patients who received inpatient rehabilitation during the acute postoperative period received rehabilitation on a SRU, and only 28% of the amputees in this sample had evidence of inpatient rehabilitation during that time period.
If we consider 2 patients with different clinical characteristics, the patient more likely to be discharged home based on these clinical variables is also less likely selected for specialized rehabilitation. The fact that selection bias seems to be operating in favor of generalized suggests that rehabilitation professionals are preferentially selecting those amputees for more intensive services with circumstances that complicate discharge planning. Factors that confound home discharge need to be recognized by rehabilitation professionals and policy makers alike as being legitimate determinants of rehabilitation need on par with traditional concepts of medical necessity.
Persons with dysvascular amputations rarely receive a prosthetic limb during inpatient rehabilitation because the residual limb is not fully healed.31 It may be that specialized rehabilitation better prepares amputees for the training and use of a prosthesis in the follow-up period. The relationship between type of rehabilitation and receipt of a prosthetic limb needs to be studied further.
Similar to our findings of improvement in physical functioning, Turney et al found that the majority (63%) of lower limb amputees who were appropriately referred to intensive inpatient rehabilitation were able to ambulate independently after rehabilitation.32 There is a great deal of interaction among patients and staff on SRUs because treatment occurs in a designated area. Patients may benefit from reinforcement and encouragement as they watch other patients improve their functional status. This interaction, along with more opportunity to focus on functional goals and more aggressive therapy, is part of the intentional process of specialized rehabilitation, which applies treatments in a supportive and hopefully empowering setting. These differences may account for some of the incremental improvements in physical functioning.
In our previous work, we found that patients who received inpatient rehabilitation during the acute postoperative period were 1.5 times more likely to survive compared with patients with no inpatient rehabilitation.2 In this study, we found that once inpatient rehabilitation is made available, there is no strong evidence of incremental benefit of receiving specialized over generalized rehabilitation in terms of survival. The greatest incremental benefit of specialized over generalized inpatient rehabilitation seems in improving quality of life (functional status, receipt of a prosthetic limb, and the chance of home discharge). Rehabilitation clinicians on a SRU may have opportunity to focus on achieving optimal rather than the minimally necessary outcomes. With the known short life spans among this population,11 focus on quality of life outcomes seems vital.
This study had several limitations. Our p score analysis properly controlled for selection bias due to measured patient- and facility-level characteristics, but could not control for selection bias due to unmeasured characteristics. We attempted to measure all relevant characteristics, but further research is needed on additional clinical differences that might not have been available to us in the data. Certain findings in this VHA amputee population may not generalize to patients in the private sector. The majority of veterans are males, and it is unknown if findings can be applied to females. Race and ethnicity were not included because of the large amount of missing or unknown information. Moreover, although the acute postoperative inpatient rehabilitation care pattern used in this study was the most common among veteran amputees, it comprises less than half the veterans who received inpatient rehabilitation. Future studies will need to be directed towards studying the outcome implications of different rehabilitation care patterns, for example, inpatient rehabilitation after discharge from the index surgical stay or as outpatients.
Our observational study provides evidence that rehabilitation on an SRU during the acute postoperative period has incremental benefits after LE amputation compared with receiving rehabilitation on general medical/surgical units. Confidence in our findings is bolstered by the results of our sensitivity analysis, which showed that that our findings would remain the same even if there was an unmeasured characteristic that had a moderately strong effect on both receiving specialized rehabilitation and the outcome. We acknowledge that the results of observational studies must be interpreted cautiously and that only randomized controlled trials (RCT) can definitively determine causal relationships. However, as noted during a December 2007 Institute of Medicine meeting, RCTs are not always optimal or possible because of timing, cost, etc.33 That meeting called for “comparative effectiveness research” defined as a process “comparing biologically focused interventions controlling for patient and system attributes.”34 The p score risk-adjustment methods applied in this study meet this definition. RCTs cannot be undertaken for all interventions in which benefit is unknown, particularly when strong beliefs about the advantages of services make randomization ethically difficult.
To our knowledge, our study was the first study that examined outcomes of different types of rehabilitation after LE amputation. Care of persons after LE amputation is gaining more attention due to the increased media attention of soldiers returning from the conflicts in Afghanistan and Iraq. In July 2007, CARF published new accreditation standards for amputation specialty programs effective January 2008.35 These new standards reflect consensus among rehabilitation professionals that persons with new amputations benefit from intensive, organized interdisciplinary rehabilitation services. Future outcome studies are needed not only to identify those patients who will benefit most from rehabilitation interventions but also to determine which levels of rehabilitation are cost-effective with respect to the outcomes attained.
Acknowledgments
The authors thank Sharon Jayne and Janice Duglas, who provided support in the preparation of the manuscript, and Dean M. Reker and Clifford Marshall, who guided the group in applications of the FSOD data.
Supported by grants from the National Institutes of Health (RO1-HD042588). It was also supported by resources and the use of facilities at the Samuel S. Stratton VAMC in Albany, NY, and the Kansas City VAMC in Kansas City, MO.
Footnotes
The findings of this study were presented in part in a poster presentation at the 2007 Symposium on Post-Acute Rehabilitation State of the Science Meeting, February 12–13, 2007, Crystal City, VA; and in a poster presentation at the 2007 University of Pennsylvania Institute on Aging Poster Session on Aging, May 8, 2007, Philadelphia, PA.
The opinions and conclusions of the authors are not necessarily those of the sponsoring agencies.
References
- 1.Pezzin LE, Dillingham TR, MacKenzie EJ. Rehabilitation and the long-term outcomes of persons with trauma-related amputations. Arch Phys Med Rehabil. 2000;81:292–300. doi: 10.1016/s0003-9993(00)90074-1. [DOI] [PubMed] [Google Scholar]
- 2.Stineman MG, Kwong PL, Kurichi JE, et al. The effectiveness of inpatient rehabilitation in the acute postoperative phase of care after trans-tibial or trans-femoral amputation: study of an integrated health care delivery system. Arch Phys Med Rehabil. 2008;89:1863–1872. doi: 10.1016/j.apmr.2008.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- 4.Murray PK, Singer M, Dawson NV, et al. Outcomes of rehabilitation services for nursing home residents. Arch Phys Med Rehabil. 2003;84:1129–1136. doi: 10.1016/s0003-9993(03)00149-7. [DOI] [PubMed] [Google Scholar]
- 5.Rosenbaum PR, Rubin DB. Sensitivity to an unobserved binoary covariate in an observational study with binary outcome. J R Stat Soc. 1983;45:212–218. [Google Scholar]
- 6.Hines Edward J., Jr VIReC Research User Guide. FY2000 VHA Medical SAS Inpatient Datasets. VA Hospital, Hines, IL: Veterans Affairs Information Resource Center; 2003. [Google Scholar]
- 7.Hines Edward J., Jr VIReC Research User Guide. FY2000 VHA Medical SAS Outpatient Datasets. VA Hospital, Hines, IL: Veterans Affairs Information Resource Center; 2003. [Google Scholar]
- 8.Kubal JD, Webber S, Cooper DC, et al. VIReC Insights No 5. Hines, IL: Veterans Affairs Information Resource Center; 2000. A primer on US mortality databases used in health services research. [Google Scholar]
- 9.Pape T, Maciejewski M, Reiber G. The National Prosthetics Patient Database (Nppd): A Primary Resource for Nationwide VA Durable Medical Equipment Data. Hines, IL: Veterans Affairs Information Resource Center; 2001. [Google Scholar]
- 10.Department of Veterans Affairs, VHA Office of Information. VHA Corporate Databases Monograph [VA web site] [April 18, 2007];2006 March; Available at: http://www.virec.research.va.gov/References/links/VHACorporateDatabaseMonograph2006Final.pdf.
- 11.Bates B, Stineman MG, Reker D, et al. Risk factors associated with mortality in a male veteran population following transtibial or trans-femoral amputation. J Rehabil Res Dev. 2006;43:917–928. doi: 10.1682/jrrd.2006.03.0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bates BE, Kurichi JE, Marshall CR, et al. Does the presence of specialized rehabilitation units influence access to comprehensive services? Arch Phys Med Rehabil. 2007;88:1249–1255. doi: 10.1016/j.apmr.2007.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kurichi JE, Kwong PL, Reker DM, et al. Clinical factors associated with prescription of a prosthetic limb in elderly veterans. J Am Geriatr Soc. 2007;55:900–906. doi: 10.1111/j.1532-5415.2007.01187.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kurichi JE, Stineman MG, Kwong PL, et al. Assessing and using comorbidity measures in elderly veterans with lower extremity amputations. Gerontology. 2007;53:255–259. doi: 10.1159/000101703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mayfield JA, Reiber GE, Maynard C, et al. Survival following lower-limb amputation in a veteran population. J Rehabil Res Dev. 2001;38:341–345. [PubMed] [Google Scholar]
- 16.Granger CV, Hamilton BB, Keith RA, et al. Advances in functional assessment for medical rehabilitation. Top Geriatr Rehabil. 1986;1:59–74. [Google Scholar]
- 17.McWhinnie DL, Gordon AC, Collin J, et al. Rehabilitation outcome 5 years after 100 lower-limb amputations. Br J Surg. 1994;81:1596–1599. doi: 10.1002/bjs.1800811110. [DOI] [PubMed] [Google Scholar]
- 18.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 19.HCUP Comorbidity Software [computer program]. Healthcare Cost and Utilization Project (HCUP). Version 3.1. Rockville, MD: Agency for Healthcare Research and Quality; 2006. [PubMed] [Google Scholar]
- 20.Stineman MG, Shea JA, Jette A, et al. The functional independence measure: tests of scaling assumptions, structure, and reliability across 20 diverse impairment categories. Arch Phys Med Rehabil. 1996;77:1101–1108. doi: 10.1016/s0003-9993(96)90130-6. [DOI] [PubMed] [Google Scholar]
- 21.Hamilton BB, Granger CV, Sherwin FS. A uniform national data system for medical rehabilitation. In: Fuhrer MG, editor. Rehabilitation Outcomes: Analysis and Measurement. Baltimore, MD: Paul H. Brookes; 1987. [Google Scholar]
- 22.D’Agostino RB., Jr Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17:2265–2281. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 23.Dehijia RH, Wahba S. Causal effects in nonexperimental studies: reevaluation the evaluation of training programs. Am Stat Assoc. 1999;94:1053–1062. [Google Scholar]
- 24.Rosenbaum PR, Rubin DB. Reducing bias in observational studies using subclassification on the propensity score. J Am Stat Assoc. 1984;79:516–524. [Google Scholar]
- 25.Rosenbaum PR. Observational Studies. New York, NY: Springer-Verlag; 2002. [Google Scholar]
- 26.Rubin D. Combining propensity score matching with additional adjustments for prognostic covariates. Am Stat Assoc. 2000;95:573–585. [Google Scholar]
- 27.Normand ST, Landrum MB, Guadagnoli E, et al. Validating recommendations for coronary angiography following acute myocardial infarction in the elderly: a matched analysis using propensity scores. J Clin Epidemiol. 2001;54:387–398. doi: 10.1016/s0895-4356(00)00321-8. [DOI] [PubMed] [Google Scholar]
- 28.Agresti A. Categorical Data Analysis. Hobeken, NJ: John Wiley & Sons, Inc; 2002. [Google Scholar]
- 29.SAS [computer program]. Version 9.1. Cary, NC: SAS Institute; 2005. [Google Scholar]
- 30.Vienna, Austria: R Development Core Team; 2008. R: A language and environment for statistical computing [computer program[ Available at: http://www.R-project.org. [Google Scholar]
- 31.Dillingham TR, Pezzin LE. Postacute care services use for dysvascular amputees: a population-based study of Massachusetts. Am J Phys Med Rehabil. 2005;84:147–152. doi: 10.1097/01.phm.0000154899.49528.05. [DOI] [PubMed] [Google Scholar]
- 32.Turney BW, Kent SJ, Walker RT, et al. Amputations: no longer the end of the road. J R Coll Surg Edinb. 2001;46:271–273. [PubMed] [Google Scholar]
- 33.Roberts MS. Using physiology-based prediction models to enhance clinical trials. IOM annual Meeting: Evidence-Based Medicine and the Changing Nature of Health Care. [February 1, 2008]; Available at: http://www.iom.edu/CMS/46897.aspx.
- 34.Fisher ES. Relationship between health care and the evidence base: Current profile. 2007 IOM annual Meeting: Evidence-Based Medicine and the Changing Nature of Health Care. [February 1, 2008]; Available at: http://www.iom.edu/CMS/46897.aspx.
- 35.Commission on Accreditation of Rehabilitation Facilities, CARF Service Providers [web site] [August 6, 2007]; Available at: http://www.carf.org/Providers.aspx?content=content/providers/amputation.htm.


