Abstract
Context:
Sudden cardiac death (SCD) is a relatively rare yet unfortunate risk of athletic participation. To reduce the incidence of SCD, electrocardiogram (ECG) use during athletic preparticipation examinations (PPEs) has been proposed to detect underlying cardiac abnormalities.
Objective:
To estimate the effectiveness of ECG use during athletic PPEs.
Design:
Epidemiologic modeling.
Populations:
Public high school athletes.
Data Collection and Analysis:
Estimates of ECG sensitivity (70%) and specificity (84%) were drawn from the literature, as was the estimate of overall prevalence of cardiac conditions relevant to SCD (0.3%). Participation rate by sex was determined from National Federation of State High School Associations data. Participation by ethnicity was assumed to be proportionate to the public high school attendance rates for grades 9 through 12 (18.4% African American). Population-specific ECG effectiveness (positive predictive value), estimated total costs, cost per year of life saved, and cost to identify 1 additional case were computed. Total annual PPE screening costs reflected a cardiologist's office visit, including echocardiogram for those athletes with a positive ECG screen.
Results:
The model predicted that 16% of all athletes would be expected to have a positive ECG, but only 1.3% of athletes with a positive ECG would have a cardiac abnormality capable of causing SCD, including hypertrophic cardiomyopathy, structural defects, and various conduction abnormalities. Total annual cost estimates for ECG screening and follow-up exceeded $126 million. Average cost per year of life saved across groups was $2693, and the cost to identify 1 additional case averaged $100 827. Compared with females, males had both lower cost per year of life saved and lower cost to identify 1 true case. Similarly, black males exhibited lower costs than white males. Across groups, false-positive ECG screening exams accounted for 98.8% of follow-up costs.
Conclusions:
Large-scale, mass ECG testing would be a costly method to identify athletes with cardiac abnormalities. Targeting high-risk populations can increase the effectiveness of the ECG for athletic PPE screening.
Keywords: cardiac abnormalities, sudden cardiac death, prevalence
Key Points.
Mass electrocardiographic screening during high school preparticipation physical examinations would likely be very costly, due in part to low positive predictive value and high follow-up costs resulting from excessive false-positive tests.
Electrocardiographic screening effectiveness could be improved by testing only those athletes who are identified as being at high risk for cardiac abnormalities that could cause sudden death.
Sudden cardiac death (SCD) is a rare but tragic event associated with athletic participation. Few warning signs exist to indicate the presence of an abnormality capable of causing SCD1,2; as a result, death itself can be the first indication of an underlying cardiac condition.3 Screening for cardiac conditions associated with SCD often occurs via school-based mass preparticipation physical examinations (PPEs) of hundreds of athletes in a single day. At present, however, no method exists to effectively and consistently identify those athletes at risk for SCD in a mass screening scenario. Consequently, many athletes are likely participating in organized athletics even though they harbor underlying cardiac conditions capable of triggering SCD.
The overall prevalence of cardiac abnormalities responsible for SCD has been estimated4 to be 0.3% (3 in 1000) in the general athlete population. Actual incidence rates of SCD are markedly lower; relatively few cardiac abnormalities lead to a fatal event in young athletes. Both sex and ethnicity appear to play roles in the risk of SCD. Males experience SCD nearly 10 times more often than females, and the incidence among African Americans is higher than in other ethnic groups.5 Prevention of SCD in these athlete populations requires early recognition of those conditions known to cause SCD.
Athletic PPE screening standards in the United States are typically determined by state legislation, state athletic associations, or individual school districts4,6 and most often consist of a medical history review and physical examination.4 Despite the lack of a standardized PPE protocol, 2 widely cited monographs offer guidelines. The first publication,7 a joint effort by 6 medical associations, recommends a comprehensive PPE at least every 2 years, including a cardiac-specific medical history and a dynamic cardiac evaluation. The second publication,4 from the American Heart Association (AHA), recommends a thorough medical history in conjunction with a dynamic cardiac evaluation. Although these guidelines present a rational approach for reducing the incidence of SCD in athletes, a universal standard for screening high school athletes does not presently exist.4 In 2005, only 3 states had PPE forms containing all 12 recommended AHA screening items; 19 states were missing 3 or more AHA items, and 2 states had no approved questionnaire forms to use for the PPE.6
One mechanism proposed to reduce the incidence of SCD in athletes involves the integration of an electrocardiography (ECG) examination into athletic PPE screening.8–11 Those in support of ECG use during athletic physical examinations often point to the success of Italy's athletic screening protocol, which includes cardiac evaluation via 12-lead ECG.9 Since implementation of this program in 1982, the annual incidence of SCD in the Veneto region of Italy has decreased by nearly 90%, falling from 3.6 per 100 000 person-years in 1980 to 0.4 per 100 000 person-years in 2004.12 Critics argue that mass ECG screenings create multiple problems, including practical difficulties in screening large populations, the relatively high number of athletes who will need follow-up cardiac testing, low sensitivity and specificity of resting ECGs among athletic populations,4 and the lack of a standard for interpreting ECGs in athletes.13
The purpose of our study was to evaluate the population-specific effectiveness and costs of adding ECG screening to the PPE among public high school athletes in the United States using a simulation model. Effectiveness of ECG screening was investigated by determining the positive and negative predictive values of the ECG, based on published diagnostic factors in a similar population as well as the expected number of additional cardiac conditions detected via ECG screening as compared with a traditional PPE screening protocol. Costs were estimated using current (2009) Medicare reimbursement rates for Current Procedural Terminology (CPT)14 for a follow-up cardiology examination for all athletes with positive ECG findings during screening. Costs related to ECG screening were evaluated by determining specific total costs per population, cost per year of life saved, and cost to identify 1 additional case.
METHODS
We estimated high school athlete populations by using the overall public high school athletic participation rates stratified by sex and ethnicity, because these factors are associated with the rate of SCD. Population data for male and female participation in public high school athletics were drawn from the National Federation of High School Association's 2006–2007 rates.15 High school athletic participation data were not available by ethnicity,16 so we estimated ethnic participation rates using the 2005 US Census Bureau School Enrollment17 statistics for the census groups black and all students enrolled in grades 9 through 12, and we assumed that high school athletic participation rates by ethnicity were proportional to enrollment. Data from the Census Bureau indicated that 18.4% of students in grades 9 through 12 would fall into the black category and 81.6% into the nonblack category, which we defined as white for the purposes of this study. We used a dichotomous ethnic categorization as a result of prior SCD estimates, which were based on a similar comparison of African American versus white athletes and the lack of published prevalence or ECG sensitivity or specificity data for other ethnicities, such as Hispanic or Asian. In our model, we assumed that the prevalence of cardiac abnormalities and sensitivity and specificity of ECG for detecting those abnormalities among non–African American, nonwhite high school athletes were equivalent to those in white athletes. All participation estimates were then divided by 4 to represent each athlete receiving an ECG during the PPE only once during a 4-year high school career.
For purposes of this study, cardiac abnormalities included those potentially fatal conditions previously reported18 to be detectable by ECG, including hypertrophic cardiomyopathy (HCM), anomalous coronary artery, dilated cardiomyopathy, congenital aortic stenosis, myocarditis, arrhythmogenic right ventricular dysplasia, and primary conduction abnormalities. Although HCM is the primary cause of SCD in the United States, the prevalence value of HCM alone would be somewhat lower than that for the combined prevalence of any of these abnormalities. We applied the combined prevalence in our model under the assumption that the purpose of adding ECG to the PPE process would be to detect any potential cardiac abnormality, rather than a single disease entity. Overall prevalence of cardiac abnormalities capable of causing SCD across both sex and ethnicity groups in the US population has previously been estimated at 0.3%.4 In our model, we assumed that the sex distribution of cardiac abnormalities was the same as the sex distribution of SCD (9∶1 male to female ratio).19,20 Ethnic distribution of events capable of causing a SCD event was based on prior research5 of 286 cases of SCD in predominantly young athletes, indicating that 42% of those cases had occurred in athletes of African American ethnicity, which is consistent with evidence that African Americans experience a disproportionately high rate of SCD.5,21,22 Furthermore, this value is consistent with the reported5,23 range (36%–55%) of SCD due to HCM in black athletes.
Prevalence estimates using the proportions listed above were generated for 4 groups: black males (BM), white males (WM), black females (BF), and white females (WF). We assumed that all athletes would undergo the 12-point AHA cardiovascular screening history and physical examination with the addition of an onsite ECG screen. Prior published sensitivity and specificity estimates were found using a PubMed search for English-language articles with a combination of relevant search terms, including sudden cardiac death, high school athletes, ECG, sensitivity, and specificity. Results from this search were limited to those articles reporting data specific to an athletic population. Sensitivity and specificity of the AHA screening method in high school athletes have been estimated18 to be 6% and 98%, respectively. Sensitivity of ECG among elite and professional athletic populations has been estimated to range from 51% to 70%, and specificity has been reported in the range of 61% to 98%.24,25 For purposes of this study, we used 70% sensitivity and 84.3% specificity, based on observations derived from testing high school athletes, the target population of the current study.25
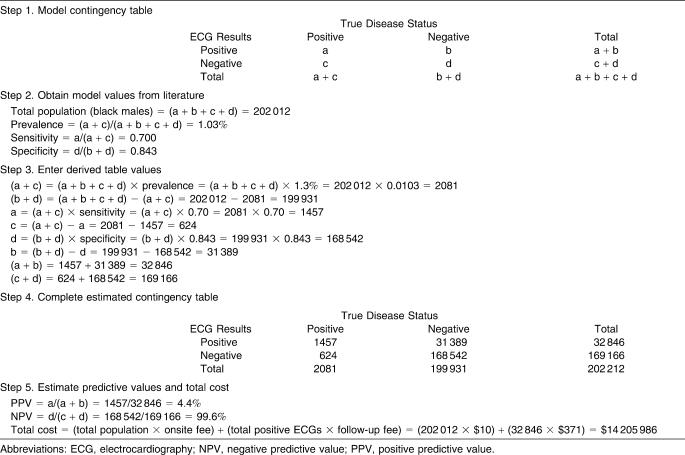
Predictive values and costs were estimated for each sex and ethnic group (Table 1). The positive predictive value (PPV = true positive cases/total positive tests) and negative predictive value (NPV = true negative cases/total negative tests)26 of using ECG during PPE were computed based on the sensitivity and specificity values. The PPV is the probability of a patient with a positive test having the disease, whereas the NPV is the probability of a patient with a negative test being free of the disease. We also estimated the number of additional athletes with cardiac abnormalities who would be identified if ECG was added to the PPE relative to the number identified by the PPE without ECG.
Table 1.
Estimating Sex-Specific and Ethnic-Specific Predictive Values and Cost: Numeric Example
Cost of the onsite history and physical examination with ECG administration was assumed to be $10, based on the cost of mass PPE screenings in our geographic region. We assumed that a cardiologist would not be on site at the PPE to evaluate which athletes would need further medical evaluation, so the ECG results would be evaluated by the physician conducting the PPE. We assumed that all athletes who had an ECG abnormality of any type would be referred to a cardiologist for further testing. Based on consultation with a panel of local cardiologists, follow-up cardiac testing for a positive ECG was assumed to include an office visit and echocardiogram. Costs for office-based follow-up testing were assumed to be $371 based on the 2009 Medicare Physician Fee Schedule (adjusted using the Geographic Practice Cost Index for our region) for CPT codes 99205 (office visit) and 93303 (transthoracic echocardiogram).14 These costs represent an estimate of reimbursement rather than billed amounts or actual expenses for the initial cardiology consultation after a positive ECG in the PPE. Additional office visits and subsequent testing or treatment that may result from the initial consultation were not estimated.
Total years of life saved were determined using a previously reported method18 that assumes 10% of those high school athletes with a diagnosed cardiovascular abnormality will live an additional 40 years and 90% will live an additional 20 years. Total cost per year of life saved was then calculated by dividing the total cost of ECG testing and associated follow-up costs by the total years of life saved. Total cost to identify 1 additional case was calculated by dividing the total costs by the number of additional cases identified by adding the ECG to the PPE.
RESULTS
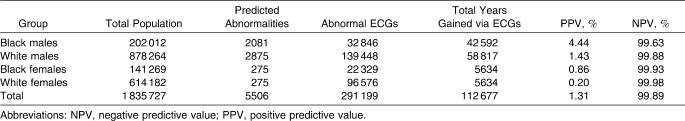
The model predicted that 16% of all athletes would be expected to have a positive ECG, whereas only approximately 2% would have a positive finding representing a potential cardiovascular abnormality on the standard PPE history and physical examination. Across the entire population, only 1.3% of athletes with a positive ECG would be expected to have a cardiac abnormality. The diagnostic capability of the ECG in this model, including expected number of abnormal ECGs, total years of life gained via ECG screening, and predictive capability of ECG screening per group, is presented in Table 2.
Table 2.
Predictive Values for Electrocardiography (ECG) Screening of High School Athletes
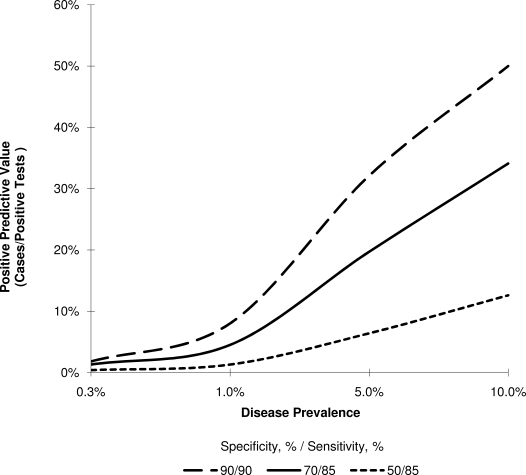
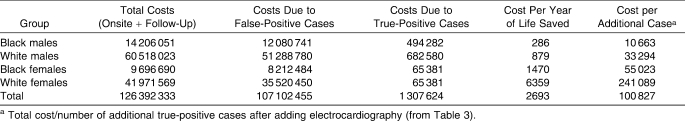
Predictive values of the ECG test were highest when testing male athletes, reflecting the effect of increased disease prevalence on PPV (Figure 1). Screening of BM athletes in particular indicates that approximately 4 of every 100 positive ECGs would result in discovery of a true cardiac abnormality, whereas screening of all female athletes would detect less than 1 true cardiac abnormality per 100 positive ECG examinations. Therefore, a positive ECG would be rather costly for identifying athletes with a cardiac condition, because relatively few athletes who have a positive ECG and receive cardiologist examination, including echocardiography, would actually be expected to have a cardiac abnormality. Across groups, NPV was lowest among BM at 99.63%; all other groups exceeded 99.88%. Such high NPVs across groups indicate that nearly all athletes (≥99.6%) with a negative onsite ECG would, in fact, be free of cardiac abnormalities capable of causing SCD.
Figure 1.
Positive predictive value of electrocardiography and disease prevalence.
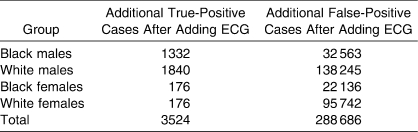
The expected outcomes from adding ECG screening to high school PPEs are listed in Table 3. The ratio of additional true-positive to additional false-positive cases found would be highest among BM (1∶25), followed by WM (1∶76), BF (1∶126), and WF (1∶550). These ratios indicate the respective inefficiencies of ECG screening among the sex-ethnicity populations. For example, for every case of a black male with a cardiac abnormality identified by implementing ECG screening, 25 BM with no abnormality will have a positive ECG that requires further medical testing. Differences in these inefficiency ratios among the groups reflect the respective group differences in the prevalence of cardiac abnormalities.
Table 3.
Expected Results of Adding Electrocardiography (ECG) to Preparticipation Physical Examinations
Costs associated with ECG examination during high school PPEs are listed in Table 4. Total combined annual costs for onsite ECG screening and follow-up cardiac testing for all athletes entering high school (ie, freshmen) exceeded $126 million. Onsite ECG screening accounted for less than 15% of the total cost. Approximately 98.8% of the costs for follow-up evaluation resulting from a positive PPE ECG came from testing athletes who had no cardiac abnormalities.
Table 4.
Costs Associated with Electrocardiography Use in Preparticipation Physical Examinations, $
The cost to identify 1 additional true case was more than 3 times higher for WM than for BM and more than 4 times higher for WF than for BF (Table 4). Within ethnic groups, the cost to identify 1 additional case was 5 times higher for BF than for BM and more than 7 times higher for WF than for WM.
DISCUSSION
Our model shows that use of the resting 12-lead ECG during PPE screening for incoming high school athletes will result in high costs because of a large number of false-positive tests. This finding is consistent with prior reports4,27–30 and is due in part to the relatively low cardiac disease prevalence among high school athletes. When the prevalence of a disease is low, as is the case with cardiac abnormalities associated with SCD among high school athletes, nearly all positive ECG tests occur in individuals who do not have the disease. As the false-positive rate increases, the number of healthy athletes receiving unnecessary cardiology follow-up testing increases, which consequently increases costs.
Identifying any disease within a population depends upon the accuracy (sensitivity and specificity) of the test used in diagnosis. Among well-trained (ie, professional and elite competitive) athletes, the resting 12-lead ECG has been reported24 to have 51% sensitivity and 61% specificity for detecting cardiac abnormalities, indicating that the test has poor diagnostic accuracy in that population.24,31,32 By contrast, high school athletes are often not highly trained; therefore, we used a sensitivity of 70% and specificity of 84.3%, based on prior research18 conducted in a high school population. Using the sensitivity and specificity values observed in trained athletes would result in an increase in false-positive tests and higher costs than we estimated.
The PPV of a diagnostic test decreases as disease prevalence decreases, as observed in the results of this study. For example, the PPV for females was predicted to be less than one-fifth that of males as a result, in large part, of the very low prevalence of cardiac disease among females. This sex discrepancy indicates that ECG screening would be relatively ineffective in screening female athletes, because very few positive ECG results (ie, 1 in 500) would indicate the presence of a true cardiac abnormality. Higher disease prevalence shows similar discrepancies. For instance, our estimates indicate that the participation rate of BM to BF in high school athletics is nearly 3∶2. However, the PPV among BM is 5 times higher than that for BF as a result of the higher expected disease prevalence among BM. Therefore, our model predicts that using mass ECG screening among a high school population would result in many false-positive test results, particularly in those subpopulations with the lowest expected disease prevalence. The NPV of our model (≥99%) was somewhat higher than a prior reported13 expected value of 96%. It is clear from our model and prior work that ECG is very effective at ruling out the presence of cardiac abnormalities, as few athletes (1%–4%) with a negative ECG will have an actual cardiac abnormality. These PPV and NPV results indicate that the primary limitation of the use of ECG during PPE is a high rate of false-positive tests, and most athletes (≥97%) with a positive ECG will have no actual cardiac abnormality.
The lowest total cost to identify 1 additional true case as well as the lowest cost per year of life saved were found in BM, primarily because of the higher expected disease prevalence (resulting in identifying more true cases per total expense) among the BM population. A sex-specific analysis of costs revealed that male athletes had both a lower cost per year of life saved and a lower cost to identify 1 additional case than did female athletes. In contrast, relative to WM, WF accrued more than 10 times the cost in identifying 1 additional case and cost per year of life saved.
Based on our model's prediction of improved diagnostic capability among populations with higher disease prevalence, a screening protocol to identify and provide an ECG test for only those athletes with an increased probability of cardiac potential may be warranted. For example, ECG screening of male athletes can be expected to result in a higher predictive accuracy for recognizing underlying cardiac conditions. Similarly, screening of BM would result in a PPV that is more than 3 times higher than that for all other athlete groups as well as a cost to identify 1 additional case that is one-third the cost of the next lowest group (WM). Although we are not advocating providing ECG screening for specific sex or ethnic groups, substantial improvement in the ECG effectiveness during PPE for high school athletes can be expected by using ECG only for the athletes who are at high risk.
Identifying individuals with a cardiac abnormality that is capable of causing an SCD event and withholding them from competitive athletic activity would be expected to result in a portion of those individuals being saved from a cardiac-related death. Unfortunately, the high false-positive rate associated with mass screening ECG can also be expected to introduce the psychological stress of being falsely labeled with a potentially fatal cardiac abnormality. In addition, the time frame from the positive onsite ECG examination through a full cardiology workup can be weeks, which may prevent the athlete from participating in sport. These factors should be considered when ECG screening as part of the PPE is being contemplated.
Conflicting Protocols
Advocates for ECG implementation often point to the success of the Italian protocol in reducing the incidence of SCD12,33 and identifying cardiomyopathies.10 The incidence of SCD in Italy has decreased dramatically, from 3.6 to 0.4 per 100 000 individuals, since ECG screening was incorporated into athletic physical examinations.12 However, 3 important issues arise when we attempt to generalize these results to American athletes. First, data from the majority of Italian studies were collected from predominantly white males, often localized to the Veneto region of the country. As a result, the athlete population considered in those studies does not represent the sexual and ethnic diversity that is present among high school athletes in the United States. Second, the most common (25%) cause of SCD among Italian athletes is arrhythmogenic right ventricular dysplasia, also known as arrhythmogenic right ventricular cardiomyopathy,1,20,34 a condition representing fewer than 5% of SCD incidents among young athletes in the United States.20,35 Among the cardiovascular conditions capable of causing SCD, HCM is the most common (approximately 40%) cause of SCD in young American athletes.20 Finally, the SCD incidence rate after the addition of ECG screening in Italy is strikingly similar to that reported in the United States without ECG screening3: 1 in 200 000 high school–aged participants. Therefore, based on population demographic discrepancies, varying cardiac abnormality prevalence rates, and differences in the reported rates of SCD, whether the Italian ECG screening protocol will reduce the SCD rate in the United States as effectively as in Italy is uncertain.
Limitations
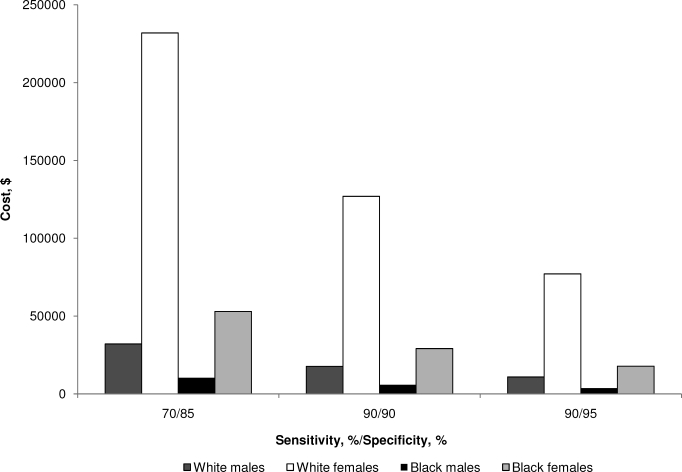
The primary limitation of this simulation study is the estimates used for prevalence, sensitivity, and specificity in our model. A range of values for each factor are reported in the literature. As a result, the data presented in this study could be expected to vary in accordance with alternative estimates for each measure (Figure 2). Despite this variation, the results would be expected to remain in proportion to our findings, in large part as a result of the effect of disease prevalence on the PPV of a diagnostic test. Furthermore, actual costs depend upon follow-up tests selected by the athlete's individual cardiologist. These follow-up tests may differ from the physical examination and echocardiography included in our model, as may the regional reimbursement rates. Another limitation lies in the population used for this study. We evaluated the usefulness of ECG screening among public high school athletes in the United States. Absent from our modeled population are those athletes in private high schools, youth sports, recreational or club teams, and collegiate athletics. The inclusion of these additional athletic populations would result in a substantially higher total cost. Furthermore, accurate ECG interpretation is known to be challenging among the high school athlete population,13 and the variability of interpretation among physicians can be an issue.13 The sensitivity and specificity values used in our model represent averages of the theoretical population of physicians who would be interpreting ECG during PPE. Our model also stipulates that all cardiac conditions detected via ECG would result in cardiology follow-up; however, this may not hold true in practice, thereby potentially decreasing the costs associated with follow-up care.
Figure 2.
Cost of electrocardiography and sensitivity and specificity values.
Application
Accurate detection of cardiac abnormalities associated with SCD in young athletes remains a priority for sports medicine professionals.36 Despite a general perception that athletes represent the healthiest segment of society,20 many remain susceptible to underlying cardiac abnormalities that, when combined with sport participation, increase their risk for SCD. One of the major challenges in preventing SCD is the relative unpredictability with which it occurs in the athletic population.20 Some9,10,37 have proposed that the 12-lead ECG examination be used to diagnose individuals with some types of cardiac abnormalities during preseason cardiac assessments despite ongoing debate regarding its effectiveness.4 The low prevalence of cardiac conditions in a high school population can be problematic in terms of accurate detection. Therefore, in order to increase the accuracy of the onsite ECG test, either the instrumentation must be improved (ie, enhanced sensitivity and specificity), a combination of diagnostic tests should be used to identify high-risk individuals who are more likely to have the disease, or certain tests (eg, ECG) should be used only in populations with a relatively high prevalence of the disease.
Prior authors have investigated risk and prevalence of cardiac abnormalities in relatively small athlete populations. The need exists for a longitudinal study in very large populations of high school athletes to determine actual cardiac disease prevalence, SCD occurrence, and accuracy of ECG during PPE. Until such a study is conducted, the use of a model derived from prior estimates may provide reasonable expectations for adding ECG as a routine component of the PPE.
Conclusions
Mass ECG screening during high school PPEs would be very costly and perhaps cost prohibitive, in large part because of the low PPV and high follow-up costs generated by excessive false-positive tests. These high costs would be expected as a result of inconsistent ECG interpretation, the personnel required for administration and interpretation, and lost participation time during follow-up examinations. Effectiveness of ECG screening could be improved by testing only those athletes who are at high risk for harboring cardiac abnormalities capable of causing SCD.
REFERENCES
- 1.Basilico F. C. Cardiovascular disease in athletes. Am J Sports Med. 1999;27(1):108–121. doi: 10.1177/03635465990270010601. [DOI] [PubMed] [Google Scholar]
- 2.Ellsworth E. G., Ackerman M. J. The changing face of sudden cardiac death in the young. Heart Rhythm. 2005;2(12):1283–1285. doi: 10.1016/j.hrthm.2005.09.025. [DOI] [PubMed] [Google Scholar]
- 3.Maron B. J., Gohman T. E., Aeppli D. Prevalence of sudden cardiac death during competitive sports activities in Minnesota high school athletes. J Am Coll Cardiol. 1998;32(7):1881–1884. doi: 10.1016/s0735-1097(98)00491-4. [DOI] [PubMed] [Google Scholar]
- 4.Maron B. J., Thompson P. D., Ackerman M. J., et al. Recommendations and considerations related to preparticipation screening for cardiovascular abnormalities in competitive athletes: 2007 update. A scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism: endorsed by the American College of Cardiology Foundation. Circulation. 2007;115(12):1643–1655. doi: 10.1161/CIRCULATIONAHA.107.181423. [DOI] [PubMed] [Google Scholar]
- 5.Maron B. J., Carney K. P., Lever H. M., et al. Relationship of race to sudden cardiac death in competitive athletes with hypertrophic cardiomyopathy. J Am Coll Cardiol. 2003;41(6):974–980. doi: 10.1016/s0735-1097(02)02976-5. [DOI] [PubMed] [Google Scholar]
- 6.Glover D. W., Glover D. W., Maron B. J. Evolution in the process of screening United States high school student-athletes for cardiovascular disease. Am J Cardiol. 2007;100(11):1709–1712. doi: 10.1016/j.amjcard.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 7.American Academy of Family Physicians, American Academy of Pediatrics, American Medical Society for Sports Medicine, American Orthopaedic Society for Sports Medicine, American Osteopathic Academy of Sports Medicine. Preparticipation Physical Evaluation. 3rd ed. New York, NY: McGraw-Hill; 2004. pp. 5–6. [Google Scholar]
- 8.Corrado D., Thiene G. Protagonist: routine screening of all athletes prior to participation in competitive sports should be mandatory to prevent sudden cardiac death. Heart Rhythm. 2007;4(4):520–524. doi: 10.1016/j.hrthm.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 9.Corrado D., Pelliccia A., Bjornstad H. H., et al. Cardiovascular pre-participation screening of young competitive athletes for prevention of sudden death: proposal for a common European protocol. Consensus statement of the Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Disease of the European Society of Cardiology. Eur Heart J. 2005;26(5):516–524. doi: 10.1093/eurheartj/ehi108. [DOI] [PubMed] [Google Scholar]
- 10.Pelliccia A., Di Paolo F., Corrado D., et al. Evidence for efficacy of the Italian national pre-participation screening programme for identification of hypertrophic cardiomyopathy in competitive athletes. Eur Heart J. 2006;27(18):2196–2200. doi: 10.1093/eurheartj/ehl137. [DOI] [PubMed] [Google Scholar]
- 11.Bille K., Figueiras D., Schamasch P., et al. Sudden cardiac death in athletes: the Lausanne recommendations. Eur J Cardiovasc Prev Rehabil. 2006;13(6):859–875. doi: 10.1097/01.hjr.0000238397.50341.4a. [DOI] [PubMed] [Google Scholar]
- 12.Corrado D., Basso C., Pavei A., Michieli P., Schiavon M., Thiene G. Trends in sudden cardiovascular death in young competitive athletes after implementation of a preparticipation screening program. JAMA. 2006;296(13):1593–1601. doi: 10.1001/jama.296.13.1593. [DOI] [PubMed] [Google Scholar]
- 13.Lawless C. E., Best T. M. Electrocardiograms in athletes: interpretation and diagnostic accuracy. Med Sci Sports Exerc. 2008;40(5):787–798. doi: 10.1249/MSS.0b013e318164dd18. [DOI] [PubMed] [Google Scholar]
- 14.Physician fee schedule look-up. Centers for Medicare & Medicaid Services Web site. http://www.cms.hhs.gov/PFSlookup. Accessed January 15, 2010.
- 15.National Federation of High School Associations. NFHS Participation Figures. http://www.nfhs.org/custom/participation_figures/default.aspx. Accessed June 18, 2009.
- 16.Rowland T. Sudden unexpected death in young athletes: reconsidering “hypertrophic cardiomyopathy.”. Pediatrics. 2009;123(4):1217–1222. doi: 10.1542/peds.2008-0708. [DOI] [PubMed] [Google Scholar]
- 17.US Census Bureau. School enrollment—social and economic characteristics of students: October 2005. http://www.census.gov/population/www/socdemo/school/cps2005.html. Accessed June 18, 2009.
- 18.Fuller C. M. Cost effectiveness analysis of screening of high school athletes for risk of sudden cardiac death. Med Sci Sports Exerc. 2000;32(5):887–890. doi: 10.1097/00005768-200005000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Maron B., Shirani J., Poliac L. C., Mathenge R., Roberts W. C., Mueller F. O. Sudden death in young competitive athletes; clinical, demographic, and pathological profiles. JAMA. 1996;276(3):199–204. [PubMed] [Google Scholar]
- 20.Maron B. J. Hypertrophic cardiomyopathy and other causes of sudden cardiac death in young competitive athletes, with considerations for preparticipation screening and criteria for disqualification. Cardiol Clin. 2007;25(3):399–414. doi: 10.1016/j.ccl.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 21.Rowland T. Sudden cardiac death in athletes: rethinking “hypertrophic cardiomyopathy.”. Pediatr Exerc Sci. 2007;19(4):373–383. doi: 10.1123/pes.19.4.373. [DOI] [PubMed] [Google Scholar]
- 22.Williams R. A. Sudden cardiac death in blacks, including black athletes. Cardiovasc Clin. 1991;21(3):297–320. [PubMed] [Google Scholar]
- 23.Mueller F., Cantu R., Van Camp S. Catastrophic Injuries in High School and College Sports. Vol 8. Champaign, IL: Human Kinetics; 1996. pp. 23–40. [Google Scholar]
- 24.Pelliccia A., Maron B. J., Culasso F., et al. Clinical significance of abnormal electrocardiographic patterns in trained athletes. Circulation. 2000;102(3):278–284. doi: 10.1161/01.cir.102.3.278. [DOI] [PubMed] [Google Scholar]
- 25.Fuller C. M., McNulty C. M., Spring D. A., et al. Prospective screening of 5,615 high school athletes for risk of sudden cardiac death. Med Sci Sports Exerc. 1997;29(9):1131–1138. doi: 10.1097/00005768-199709000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Kocher M. S., Zurakowski D. Clinical epidemiology and biostatistics: a primer for orthopaedic surgeons. J Bone Joint Surg Am. 2004;86(3):607–620. [PubMed] [Google Scholar]
- 27.Shirley K. W., Adirim T. A. Sudden cardiac death in young athletes. Clin Pediatr Emerg Med. 2005;6(4):194–199. [Google Scholar]
- 28.Viskin S. Antagonist: routine screening of all athletes prior to participation in competitive sports should be mandatory to prevent sudden cardiac death. Heart Rhythm. 2007;4(4):525–528. doi: 10.1016/j.hrthm.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 29.Maron B. J. Sudden death in young athletes. New Engl J Med. 2003;349(11):1064–1075. doi: 10.1056/NEJMra022783. [DOI] [PubMed] [Google Scholar]
- 30.Mick T. M., Dimeff R. J. What kind of physical examination does a young athlete need before participating in sports? Cleve Clin J Med. 2004;71(7):587–597. doi: 10.3949/ccjm.71.7.587. [DOI] [PubMed] [Google Scholar]
- 31.Link M. S., Wang P. J., Estes N. A., III Ventricular arrhythmias in the athlete. Curr Opin Cardiol. 2001;16(1):30–39. doi: 10.1097/00001573-200101000-00005. [DOI] [PubMed] [Google Scholar]
- 32.Maron B. J., Pelliccia A. The heart of trained athletes: cardiac remodeling and the risks of sports, including sudden death. Circulation. 2006;114(15):1633–1644. doi: 10.1161/CIRCULATIONAHA.106.613562. [DOI] [PubMed] [Google Scholar]
- 33.Corrado D., Michieli P., Basso C., Schiavon M., Thiene G. How to screen athletes for cardiovascular diseases. Cardiol Clin. 2007;25(5):391–397. doi: 10.1016/j.ccl.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 34.Corrado D., Basso C., Thiene G. Arrhythmogenic right ventricular cardiomyopathy: diagnosis, prognosis, and treatment. Heart. 2000;83:588–595. doi: 10.1136/heart.83.5.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maron B. J. Hypertrophic cardiomyopathy: a systematic review. JAMA. 2002;287(10):1308–1320. doi: 10.1001/jama.287.10.1308. [DOI] [PubMed] [Google Scholar]
- 36.Maron B. J., Thompson P. D., Puffer J. C., et al. Cardiovascular preparticipation screening of competitive athletes: a statement for health professionals from the Sudden Death Committee (clinical cardiology) and Congenital Cardiac Defects Committee (cardiovascular disease in the young), American Heart Association. Circulation. 1996;94(4):850–856. doi: 10.1161/01.cir.94.4.850. [DOI] [PubMed] [Google Scholar]
- 37.Pelliccia A., Di Paolo F. M., Quattrini F. M., et al. Outcomes in athletes with marked ECG repolarization abnormalities. New Engl J Med. 2008;358(2):152–161. doi: 10.1056/NEJMoa060781. [DOI] [PubMed] [Google Scholar]