Abstract
Objective:
To (1) search the English-language literature for original research addressing the effect of cryotherapy on joint position sense (JPS) and (2) make recommendations regarding how soon healthy athletes can safely return to participation after cryotherapy.
Data Sources:
We performed an exhaustive search for original research using the AMED, CINAHL, MEDLINE, and SportDiscus databases from 1973 to 2009 to gather information on cryotherapy and JPS. Key words used were cryotherapy and proprioception, cryotherapy and joint position sense, cryotherapy, and proprioception.
Study Selection:
The inclusion criteria were (1) the literature was written in English, (2) participants were human, (3) an outcome measure included JPS, (4) participants were healthy, and (5) participants were tested immediately after a cryotherapy application to a joint.
Data Extraction:
The means and SDs of the JPS outcome measures were extracted and used to estimate the effect size (Cohen d) and associated 95% confidence intervals for comparisons of JPS before and after a cryotherapy treatment. The numbers, ages, and sexes of participants in all 7 selected studies were also extracted.
Data Synthesis:
The JPS was assessed in 3 joints: ankle (n = 2), knee (n = 3), and shoulder (n = 2). The average effect size for the 7 included studies was modest, with effect sizes ranging from −0.08 to 1.17, with a positive number representing an increase in JPS error. The average methodologic score of the included studies was 5.4/10 (range, 5–6) on the Physiotherapy Evidence Database scale.
Conclusions:
Limited and equivocal evidence is available to address the effect of cryotherapy on proprioception in the form of JPS. Until further evidence is provided, clinicians should be cautious when returning individuals to tasks requiring components of proprioceptive input immediately after a cryotherapy treatment.
Keywords: cryotherapy, somatosensory system, proprioception, therapeutic modalities
Key Points.
Because of a limited number of publications, the potential for cryotherapy to degrade joint position sense is unknown.
An increase in joint position sense error after cryotherapy has been demonstrated in 3 studies. Therefore, clinicians should be cautious in returning an athlete to dynamic activities immediately after a cryotherapy treatment.
Cold, in the form of cryotherapy, has been used since the time of the ancient Greeks, as an analgesic to reduce inflammation after acute musculoskeletal injury or trauma.1 Cryotherapy is commonly used to reduce tissue temperature, metabolism, inflammation, pain, circulation, tissue stiffness, muscle spasm, and symptoms of delayed-onset muscle soreness.2 Cryotherapy protocols, including ice application, water immersion, and commercially available cooling pads, are used by athletic trainers despite the lack of conclusive scientific research regarding the potential risks facing athletes or patients.3 Although the potential negative effects of cryotherapy itself and its possible influence on proprioception are unknown and despite equivocal evidence supporting its effectiveness, some clinicians continue to use cryotherapy in the treatment of acute soft tissue injury4 and to alleviate the symptoms of delayed-onset muscle soreness.3
The effect of cryotherapy on proprioception, which is a component of the somatosensory system, is poorly understood. Proprioceptive acuity has previously been defined as an individual's ability to sense joint position, movement, and force to discriminate movements of the limbs.5,6 Consequently, proprioceptive acuity is an essential component of injury prevention and rehabilitation, but it is often ignored with devastating consequences, because proprioceptive deficits may be responsible for many acute ankle and knee injuries.4,7–9 The term proprioception, developed as a result of Sherrington's10 landmark work in the early 1900s, is commonly defined as the cumulative neural input to the central nervous system from mechanoreceptors.11 These receptors are located in the joint capsules, ligaments, muscles, tendons, and skin12 to detect stimuli such as pain, pressure, touch, and movement. Therefore, their function is critical to both sport performance and activities of daily living.
A number of techniques for clinically examining proprioceptive acuity are described in the literature, including threshold detection of passive movement, the absolute method,13 and joint position sense (JPS). An individual's JPS primarily determines his or her ability to perceive a target joint angle or limb position and then, after the limb has been returned to its starting position, to reproduce the predetermined angle.14,15 The conscious ability to position a limb is a highly specialized proprioceptive function and is a vitally important clinical outcome measure, involving both the control of movement and stability.16 The JPS tests are routinely administered by clinicians to assess any proprioceptive deficits in the knee joint after anterior cruciate ligament injury,7,17–19 stretching,20 fatigue,14,21,22 pain,16 patellar taping,23,24 and cooling.12,25–30 The primary reason JPS is assessed by clinicians is to identify any reduction that may predispose an individual to proprioception-related injury.4,7–9,12,25–30
A systematic review is necessary to evaluate the effects of locally applied cryotherapy to a joint, specifically in relation to JPS. The brevity of quality research addressing the potential for cryotherapy, when applied to a joint, to reduce JPS and hence to potentially predispose an individual to injury needs to be addressed through further research. Similarly, no review authors have systematically evaluated the available literature regarding the effect of cryotherapy on proprioception or JPS. A comprehensive summary of the available literature is needed, so that both the health care profession and the sporting community alike can make educated clinical decisions as to how soon healthy athletes can train or compete after cryotherapy. Our purpose was to search the English-language literature for original research addressing the effect of cryotherapy on JPS and to recommend how soon healthy athletes can safely return to participation after a cryotherapy treatment.
METHODS
Search Strategy
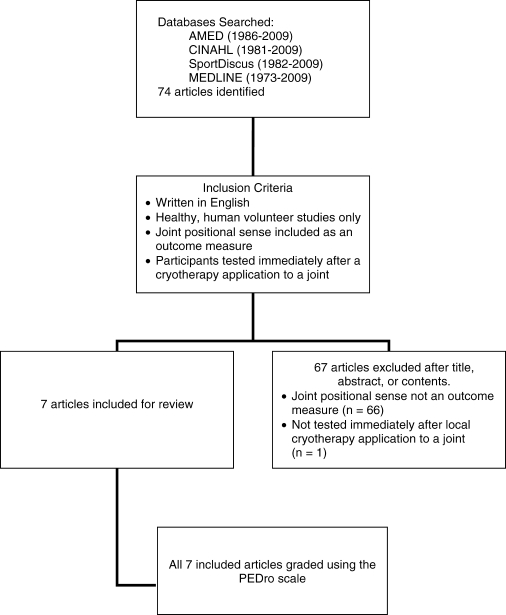
We performed an exhaustive search for original research using AMED (1986–May 2009), CINAHL (1981–May 2009), MEDLINE (1973–May 2009), and SportDiscus (1982–May 2009) to gather information on cryotherapy, proprioception, and JPS. Searches were performed using the key terms cryotherapy and proprioception, cryotherapy and joint position sense, cryotherapy, and proprioception. Potentially relevant articles were also obtained by physically searching the bibliographies of included studies to identify any study that may have escaped the original search. A total of 74 articles were identified (Figure 1).
Figure 1.
Flow chart describing the selection and exclusion of articles. PEDro indicates Physiotherapy Evidence Database.
Study Selection
The criteria for study selection were (1) the literature was written in English, (2) participants were human, (3) JPS was included as an outcome measure, (4) participants were healthy, and (5) participants were tested immediately after a cryotherapy application to a joint. Articles were excluded if the title or abstract did not meet the inclusion criteria. We then obtained the full text of each relevant study to see if the study could be included in this systematic review. Ultimately, the article had to address at least 1 outcome measure of JPS before and after a cryotherapy application.
Assessment of Methodologic Quality
A total of 7 studies, which provided at least 1 outcome measure of JPS before and after a cryotherapy treatment, were included. The Physiotherapy Evidence Database (PEDro) scale was used to rate the quality of the selected articles. The PEDro scale is an 11-item scale designed for rating the methodologic quality of randomized controlled trials.31 Each satisfied item (except for the first item, which relates to external validity) contributes 1 point to the total PEDro score.31 The items include random allocation; concealment of allocation; comparability of groups at baseline; blinding of patients, therapists, and assessors; analysis by intention to treat; and adequacy of follow up.32 The PEDro scale gives a potential scoring range of 0 to 10, where 0 points (the worst possible score) are awarded to a study that fails to satisfy any of the included items and 10 points (the best possible score) are awarded to a study that satisfies all included items. Studies scoring 9 or 10 on the PEDro scale are considered to have methodologically excellent internal validity, those scoring 6 to 8 are considered good, those scoring 4 or 5 are fair, and those scoring less than 4 are poor.33 Two evaluators who had previous experience with the PEDro scale first scored each study individually. Together, the reviewers then discussed the methodologic quality of each study before agreeing on the final score. All studies graded using the PEDro scale were included.
Data Extraction and Statistical Analysis
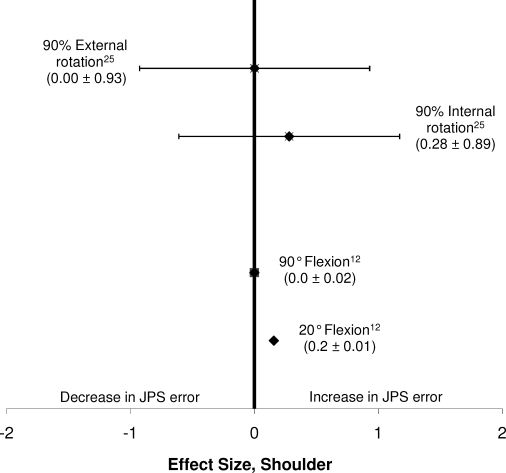
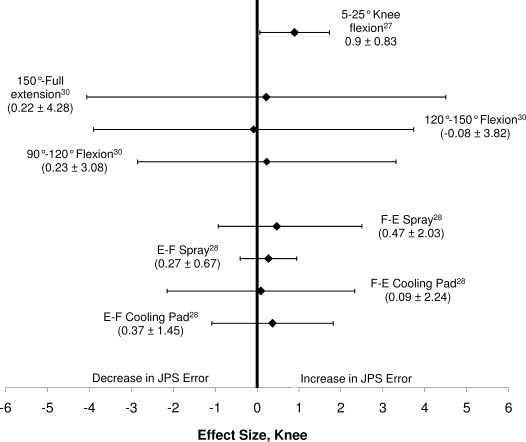
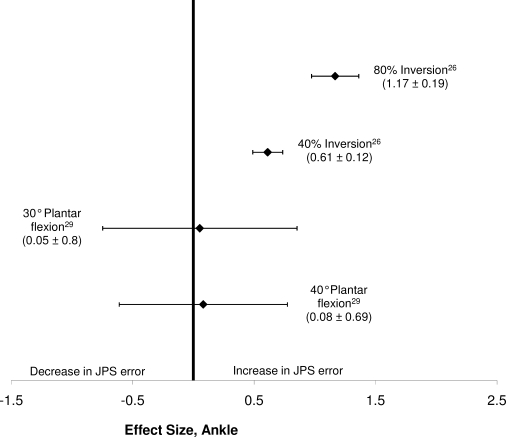
In order to calculate effect sizes and associated 95% confidence intervals for the change in JPS before and after the cryotherapy treatment, we computed the Cohen d by the following method: ([mean of posttest] − [mean of pretest])/(pooled SD of pretest and posttest).34 To interpret the strength of the effect sizes, values from 0 to 0.2 were considered weak; 0.21 to 0.5, modest; 0.51 to 1, moderate; and greater than 1, strong.35 Figures 2 through 4 illustrate the point estimates for the effect sizes and associated 95% confidence intervals for the studies conducted on the shoulder, knee, and ankle, respectively.
Figure 2.
Effect sizes and 95% confidence intervals comparing those who experienced an increase in joint position sense error in the shoulder after cryotherapy and those who did not.
Figure 3.
Effect sizes and 95% confidence intervals comparing those who experienced an increase in joint position sense error in the knee after cryotherapy and those who did not. E-F indicates extension to flexion; F-E, flexion to extension.
Figure 4.
Effect sizes and 95% confidence intervals comparing those who experienced an increase in joint position sense error in the ankle after cryotherapy and those who did not.
The quality of the evidence was then assessed using the Strength of Recommendation Taxonomy (SORT).36 The SORT gives a recommendation level to individual studies of 1 through 3, where 1 indicates good-quality patient-oriented evidence, 2 indicates limited-quality patient-oriented evidence, and 3 indicates non–patient-oriented evidence or other evidence.36,37 The SORT also included a strength of recommendation that ranges from A to C.36 A indicates a recommendation based on consistent and good-quality patient-oriented evidence, B indicates a recommendation based on inconsistent or limited-quality patient-oriented evidence, and C indicates a recommendation based on consensus, usual practice, opinion, disease-oriented evidence, or case series for studies of diagnosis, treatment, prevention, or screening.36
DATA SYNTHESIS
Study Quality
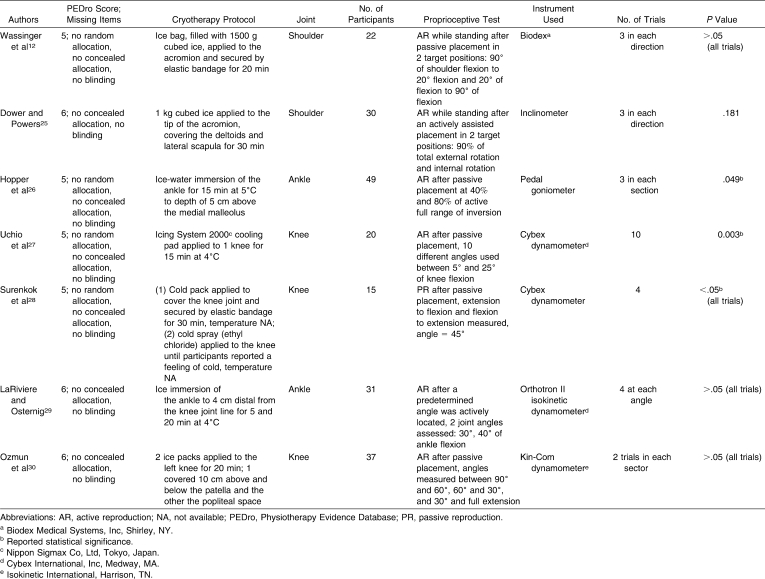
The average PEDro score for the 7 articles was 5.4/10 (range, 5–6; mode = 5, median = 5; Table).
Table.
Details of Articles Included in Systematic Review
The Effects of Cryotherapy on JPS in Healthy Participants
Seven articles met the inclusion criteria for this review (Table). In the 7 studies, 204 participants (77 men, 112 women; the sex of 15 participants was unknown28) were tested. The mean number of volunteers per study was 29.1 ± 11.5, with a mean age of 22 ± 1.6 years.
The 7 studies reviewed herein assessed 3 specific joints after a cryotherapy intervention: the ankle,26,29 knee,27,28,30 and shoulder.12,25 The modality for assessing JPS was primarily unilateral active joint repositioning,12,25–27,29,30 with only Surenkok et al28 using a passive reproduction test. Active joint repositioning was selected primarily because active testing is believed to be more functional than passive testing.16 Two methods of limb positioning or placement at the target angle were reported in the literature, namely passive12,20,27,28,30 and active.29 Three groups12,25,28 assessed individuals' self-reported dominant limb, classified as one's kicking leg or throwing shoulder arm; 1 group30 chose the left limb only; 2 groups26,29 randomly choose the tested limb; and only 1 group27 assessed both limbs.
Cryotherapy was judged to have negatively affected JPS if the degree of positional error was greater posttreatment when compared with baseline or control results. The α level was set at .05 for all 7 studies.12,25–30 Cryotherapy had a negative effect on JPS in 3 studies,26–28 whereas cryotherapy had no effect on JPS in 4 studies.12,25,29,30 All investigators included a pretest-posttest within-subjects design with a cryotherapy application.12,25–30
Three of the groups12,25,30 that administered a superficial ice application reported no change in JPS posttreatment. Dover and Powers25 and Wassinger et al12 both applied cubed ice, contained in a bag, for durations of 30 minutes and 20 minutes, respectively, to the shoulder. Although Wassinger et al12 reported no differences in positional error after the ice application, they noted a decrease in movement patterns and throwing accuracy after treatment. Similarly, Ozmun et al30 applied an ice pack to the knee for 20 minutes, but they did not state if their ice packs were commercially available or constructed by them specifically for this purpose. Also, the focus of Ozmun et al30 appeared to be on movement reproduction pattern and not joint angle reproduction. All the researchers25–30 reported their result in degrees, except Wassinger et al,12 who reported positional error in centimeters of vertical displacement. As a result, although Wassinger et al12 had a substantial intraclass correlation coefficient of 0.61 to 0.8 between trials for the assessment of proprioception on the electromagnetic tracking device, the findings of this study are hard to interpret and correlate with the literature. Nonetheless, all 3 authors12,25,30 using an ice application concluded that cryotherapy did not adversely affect JPS at the location measured. The point estimates of effect sizes for these 3 studies ranged from −0.08 to 0.28 (Figures 2 and 3), with a positive effect size reflecting an increase in JPS error. Most of the 95% confidence intervals around these points crossed zero, which indicates that a reduction in JPS was unlikely. Therefore, a superficial ice application appeared to have little effect on JPS.
Two groups27,28 employing a cooling pad to the knee for a period of 15 minutes and 30 minutes, respectively, between tests, found that knee joint repositioning was affected posttreatment (P < .05). Unfortunately, the results of these studies (Table) are difficult to compare because Surenkok et al28 failed to state the temperature of their cooling pad and used passive joint reposition, compared with Uchio et al,27 who employed active testing after using a cooling pad maintained at 4°C. Despite the methodologic differences, Uchio et al27 found a reduction in their participants' level of accuracy in matching knee joint placement immediately posttreatment of 1.7° ± 2.1° postcooling (P < .05), although the reduction was not significant 15 minutes later (0.9° ± 1.7°, P > .05). This reduction was reported by the authors28 as similar to that of an individual with a cruciate ligament injury who is receiving potentially inadequate position sense feedback for athletic activity. Similarly, Surenkok et al28 reported inaccuracies in JPS posttreatment of 1.05° ± 1.09° and 0.4° ± 2.66° using 2 separate movement protocols (extension to flexion and flexion to extension, respectively). The results of the effect size analysis (Figure 3) for the studies using a cooling pad are less consistent, with point estimates ranging from 0.09 to 0.9 (weak to moderate); positive effect sizes indicate an increase in joint repositioning sense error. Even though Surenkok et al28 reported a reduction in JPS error, the 95% confidence intervals for both trials using the cooling pad crossed zero. However, the study conducted by Uchio et al27 had a moderate effect size, and the 95% confidence interval did not cross zero. These findings suggest that using a cooling pad may be more effective in achieving greater reductions in joint, skin, and intramuscular temperatures but, as temperature changes were not reported by Surenkok et al,28 this possibility is difficult to confirm.
The 2 groups26,29 using a water-immersion cryotherapy protocol found different results for ankle JPS. Both Hopper et al26 and LaRiviere and Osternig29 used similar immersion durations (15 and 20 minutes, respectively) and water temperatures (4°C and 5°C, respectively), and neither group immersed the knee joint (Table). Hopper et al26 found JPS in the ankle reduced by 0.5° ± 0.75° after an ice-water immersion at 4° for 15 minutes. However, they concluded that a decrease of 0.5°, although statistically significant, would not be deemed clinically significant. These results are in contrast to those of LaRiviere and Osternig,29 who found ankle JPS unaffected after water immersion. This difference is also recognizable in relation to effect size (Figure 4). Hopper et al26 unanimously showed a reduction in JPS after immersion, with a modest effect size for 40° of inversion and a strong effect for 80° of inversion; neither 95% confidence interval crossed or came close to crossing zero, indicating a significant effect. Conversely, both tests conducted by LaRiviere and Osternig29 had weak effect sizes, and both 95% confidence intervals crossed zero. Two possible explanations could account for the disparity in the studies26,29: the different predetermined test angles and participant positioning during testing. Hopper et al26 assessed each volunteer's ability to match a predetermined angle of 40% and 80% of the individual's full range of ankle inversion while seated, whereas LaRiviere and Osternig29 assessed 30° and 40° of ankle flexion in a supine position. Because both used similar treatment protocols but found different results, the effect of cold may be angle dependent.
Based on this evidence, it appears that some cryotherapy modalities may adversely affect components of JPS. We have awarded the current evidence a level of 2, with a grade of B on the SORT scale, as the result of methodologic design variations and inconsistencies in the findings of the reviewed studies.
DISCUSSION
Joint position sense has been defined as the awareness of the position of a joint in space,38 and the term is used erroneously as a synonym for proprioception39 within the literature. This is primarily because proprioception encompasses a number of different components, including kinesthesia, somatosensation, balance, reflexive joint stability, and JPS.28,30,39 To date, 7 groups12,25–30 have addressed the effect of cryotherapy on JPS, with conflicting results. Four groups of authors12,25,29,30 found cryotherapy had no effect on JPS, whereas 3 others26–28 found JPS was reduced after cryotherapy. Given the pressure on athletes to maximize their availability and possible performance enhancements in endurance events after cryotherapy, individuals may sometimes be required to either train or return to competition after a cryotherapy treatment.26 Despite the general consensus that cryotherapy is an effective analgesic, clinicians are concerned about the potential effects of cryotherapy on an individual's neuromuscular functioning.12,27,40
Absolute mean error proved the most common measurement in the analysis of JPS throughout the reviewed studies.12,25–29 This method has been defined by Olsson et al41 as the average actual errors on a number of trials, ignoring the direction. Two groups25,29 measured variable error, defined as the SD of a number of trials.41 In addition, only 2 groups25,26 assessed constant error, which is similar to absolute mean except that it takes directional error into account.41 Ozmun et al30 used the most accurate trial, determined as the most accurate reproduction of the predetermined angle, for statistical analysis. We believe that this may be a factor in the authors' finding that ice application had no effect on JPS. However, the authors30 still reported an average 2° error across all 3 trial angles after cryotherapy when compared with control. If the authors had analyzed mean error, they might have found a statistically significant reduction in knee JPS after cryotherapy. Using the most (or the least) accurate trial has the potential to increase the risk of an unbalanced method of data recording when trials that produced either a greater or lower degree of angle error are disregarded. Using the mean of a number of trials would, therefore, give a better indication of an individual's joint position accuracy.
Cryotherapy Modalities and Degrees of Muscle and Joint Cooling
The disparity in findings reported in the literature is likely to result from the methodologic differences in individual studies. Cryotherapy modalities varied from ice-pack application to water immersion and durations from 5 to 30 minutes. Also, the outcome measures assessed varied from active to passive reproduction and incorporated different anatomical locations, including the shoulder, knee, and ankle.
Surenkok et al28 were the only investigators to employ proprioceptive tests (JPS and static balance) after 2 separate cryotherapy interventions in a crossover study design. The tests were completed after the application of cold spray (ethyl chloride applied to the knee until volunteers reported a feeling of cold), and after 1 week, the same testing procedures were repeated after the application of a cooling pad. These procedures presumably were conducted to compare and contrast the effects of different cryotherapy modalities on neuromuscular functioning. The authors28 found similar results using these techniques: both methods negatively affected JPS after treatment. The JPS acuity was reduced by an average of more than 1° during 2 testing procedures (flexion to extension and extension to flexion) after cold-spray application. However, applying spray until participants report a feeling of cold is a subjective measurement. Because neither application duration nor skin temperature was reported, the findings should be treated with caution.
The impairment in JPS reported by 3 groups26–28 posttreatment may be associated with a greater reduction in intramuscular or joint cooling, reduced nerve conduction velocity, shivering, or cold-induced change in proprioceptive sensitivity. This possibility is pertinent when the findings are compared with those of other authors12,25,29,30 who used more superficial applications and reported no effect posttreatment. However, only 3 of these groups25–27 recorded skin temperature and none reported intramuscular temperatures, so this theory is difficult to establish. Riemann and Lephart39 suggested that, even though all 3 groups who measured skin temperature reported reductions in skin temperature, cutaneous afferents play only a minor role in joint proprioception, whereas muscle spindles and joint receptors have a much more significant role. Therefore, whether superficial applications of cryotherapy, such as cold spray or ice, can cool deep tissue sufficiently to elicit a reduction in proprioceptive or joint position acuity is questionable. More research regarding the effects of cryotherapy on intramuscular and joint cooling, reduced nerve conduction velocity, shivering, and cold-induced changes in proprioceptive sensitivity is required before conclusions can be reached as to why JPS error was increased postcryotherapy in these studies.26–28
Previous investigators, however, have also suggested that nerve conduction velocity decreases in a linear fashion with tissue cooling42 and not skin cooling43 and the rate of decrease in muscle tissue temperature depends on the cooling temperature.44 Yet skin temperature is a good indicator of intramuscular temperature.45 Furthermore, ice massage reduces muscle temperature more than an ice-bag application,46 and a cool-whirlpool treatment is better than crushed-ice packs in maintaining muscle temperature reductions.47 Different cooling techniques may produce different degrees of joint cooling, so we believe that the modality of cooling (ice-water immersion, a cooling pad, or ice application) may be critical in governing the effect on JPS.
Although it has caused much debate, the cryotherapy modality applied appears to be an important factor affecting ground reaction force (GRF). According to Hart et al,40 any alteration in the neuromuscular or biomechanical adaptations during landing in the aftermath of a cryotherapy intervention might place an individual at risk of injury. This alteration may result from a reduction in the usually quick and efficient communication of sensory information after cryotherapy.30,48 Two groups40,48 using an ice application found no effects on peak vertical GRF at landing posttreatment when compared with baseline or control measurements. In contrast, Kinzey et al,49 using cold-water immersion, found that peak vertical GRF was negatively affected posttreatment.
A number of authors50–53 have noted similar findings in relation to closed kinetic chain proprioception (balance) or postural sway after cryotherapy. The detection and response to sway during quiet standing or, indeed, dynamic balance is vital in preventing injury,50–52 such as lateral ankle sprain.51 Cryotherapy in the form of an ice application or cold spray had no effect on balance28,50,53 posttreatment when compared with baseline or control measurements. The results of these studies contrast with those of researchers51,52 who used cold-water immersion and found balance was negatively affected immediately after treatment. Therefore, because of the increased area of surface contact, water immersion likely causes more joint and muscle cooling than other, more superficial applications, such as ice. However, although this theory is plausible, it is refuted by those54–56 who found balance unaffected after immersing participants in cold water. This topic will continue to be the subject of debate until a conclusive answer is established.
Study Quality
The average PEDro score for the 7 articles was 5.4/10 (low-high range, 5–6; mode = 5, median = 5; Table). Overall, the quality of the studies was fair to good.33 Disguising a cryotherapy application from the participants or therapists was difficult, so the criteria relating to blinding of volunteers and therapists were not met in any of the included studies. All authors used a single-group precryotherapy and postcryotherapy testing design and, as a result, no study was awarded a point for between-groups statistical comparisons. In terms of statistical power, only Dover and Powers25 performed a priori power analysis to identify the required number of volunteers needed to establish statistical differences between error scores. Similarly, none of the authors12,25–30 reported giving a sham or a placebo treatment to a control group.
Effect Sizes
The relatively small sample sizes of many of the studies reviewed, along with the discrepancies in both the joint assessed and the modality of cryotherapy, have also made comparisons difficult. The number of participants in each study was low, with 3 of the groups testing fewer than 22 volunteers12,27,28 and no group examining more than 50. This is one factor that may influence the strength of the effect size. To interpret the strength of the effect sizes, values from 0 to 0.2 were interpreted as weak, 0.21 to 0.5 as modest, 0.51 to 1 as moderate, and greater than 1 as strong, with the terms weak, modest, moderate, and large describing the difference in JPS between pretest and posttest.35 The average point estimate of the effect size of the included studies was modest, with a weak to modest effect size reported in many studies.
Many of the 95% confidence intervals derived from the studies cross zero. This observation leads us to question how significant an effect, if any, cryotherapy has on JPS. As a result, we cannot report a significant effect on JPS after cryotherapy. In the 3 studies26–28 that showed a decrease in JPS, the magnitude to which cryotherapy modalities influenced JPS appears minimal. However, subtle proprioceptive deficits can both predispose an individual to a greater risk for injury and impair sport performance.12
Recommendations for Future Research
For researchers who intend to study the effects of cryotherapy on JPS further, we have several recommendations. First, research is required to address how much of a reduction in nerve conduction velocity, skin, core, or intramuscular or joint temperature is required before the decline in limb reproduction acuity becomes apparent. Once this is identified, investigators can then establish whether various modalities of cryotherapy, including climatic chambers, ice application, cooling vests, water immersion, and cold spray, are capable of achieving this reduction.
Second, reliable and validated proprioceptive measurements (eg, threshold detection of passive movement, force acuity, and static and dynamic balance) must be conducted in conjunction with joint repositioning tests after a cryotherapy intervention to give a balanced account of the effect of cryotherapy on proprioception and neuromuscular functioning. When assessing proprioceptive acuity, administering the correct number of trials is essential because a single proprioceptive assessment may provide erroneous data postcryotherapy.57 Also, these outcome measures need to be repeated until researchers are satisfied that proprioception acuity has returned to baseline measurements after a deficit has occurred.
Investigators should also recruit sufficient numbers of participants before undertaking future clinical trials involving cryotherapy and JPS. To assist this process, we recommend an a priori analysis be conducted before any testing is undertaken. Within this review, only 1 group25 reported completing such analysis, and the relatively low sample sizes of fewer than 30 participants12,25–30 are troublesome.
To our knowledge, no authors have addressed JPS in the wrist or elbow after cryotherapy, JPS after exposure to cold climatic chambers, knee JPS after water immersion, JPS after cryotherapy in an injured population, or JPS after the use of cooling vests. Future researchers should target these areas.
Finally, we advocate that investigators assessing an individual's ability to reproduce a predetermined joint angle should use absolute mean error as the outcome measure. This method is the most reliable and validated41,57 method of reporting joint error and should be used instead of the most or least accurate trial. Reporting constant error in conjunction with absolute mean may also prove beneficial in determining the trend of directional error during repositioning trials.
Recommendations for Clinicians
We have highlighted a number of concerns for clinicians with regard to the effect of cryotherapy on JPS. First, little is known about the potential for cryotherapy to deteriorate JPS, primarily because of the small number of relevant publications. Second, because clinicians administer cryotherapy using different modalities, durations, and application areas, the variability of these factors may result in different effects on proprioceptive acuity. Finally, with 3 of the 7 reviewed studies26–28 showing an increase in JPS error postcryotherapy, we recommend clinicians consider that proprioceptive functioning may be altered and increase the risk of injury. In light of this review, we would therefore suggest caution when the athlete must perform dynamic activities (such as twisting, turning, landing, or running) immediately after a cryotherapy treatment.
CONCLUSIONS
Based on the limited and ambiguous evidence addressing the effect of cryotherapy on JPS, we are unable to support or discourage its use before athletic participation. In the 7 studies we reviewed, 3 joints were assessed (shoulder, knee, and ankle) in a combined 204 healthy participants after a cryotherapy intervention. Four groups found cryotherapy to have no effect on JPS, whereas 3 others found JPS reduced after a cryotherapy treatment. Because of differences in the joints being assessed, the modality of cooling, measurement techniques, and quality of the reviewed studies, further research is needed before a conclusive answer as to whether cryotherapy reduces JPS can be determined. Given this brevity of research, we are also unable to make a recommendation as to when athletes can safely return to participation after treatment. Despite the suggested benefits of cryotherapy, until further evidence is provided, athletic trainers and clinicians should be cautious when returning individuals to physically demanding or dynamic tasks after cryotherapy.
REFERENCES
- 1.Swenson C., Sward L., Karlsson J. Cryotherapy in sports medicine. Scand J Med Sci Sport. 1996;6(4):193–200. doi: 10.1111/j.1600-0838.1996.tb00090.x. [DOI] [PubMed] [Google Scholar]
- 2.Knight K. L. Cryotherapy in Sport Injury Management. Champaign, IL: Human Kinetics; 1995. pp. 9–11. [Google Scholar]
- 3.Vaile J., Halson S., Gill N., Dawson B. Effect of hydrotherapy on the signs and symptoms of delayed onset muscle soreness. Eur J Appl Physiol. 2008;102(4):447–455. doi: 10.1007/s00421-007-0605-6. [DOI] [PubMed] [Google Scholar]
- 4.Bleakley C., McDonough S., MacAuley D. The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med. 2004;32(1):251–261. doi: 10.1177/0363546503260757. [DOI] [PubMed] [Google Scholar]
- 5.Muaidi Q. I., Nicholson L. L., Refshauge K. M. Proprioceptive acuity in active rotation movements in healthy knees. Arch Phys Med Rehabil. 2007;89(2):371–376. doi: 10.1016/j.apmr.2007.08.154. [DOI] [PubMed] [Google Scholar]
- 6.Gandevia S. C., Refshauge K. M., Collins D. F. Proprioception: peripheral inputs and perceptual interactions. Adv Exp Med Biol. 2002;508:61–68. doi: 10.1007/978-1-4615-0713-0_8. [DOI] [PubMed] [Google Scholar]
- 7.Corrigan J. P., Cashman W. F., Brady M. P. Proprioception in the cruciate deficient knee. J Bone Joint Surg Br. 1992;74(2):247–250. doi: 10.1302/0301-620X.74B2.1544962. [DOI] [PubMed] [Google Scholar]
- 8.Payne K. A., Berg K., Latin R. W. Ankle injuries and ankle strength, flexibility, and proprioception in college basketball players. J Athl Train. 1997;32(3):221–225. [PMC free article] [PubMed] [Google Scholar]
- 9.Zazulak B. T., Hewett T. E., Reeves N. P., Goldberg B., Cholewicki J. The effects of core proprioception on knee injury: a prospective biomechanical-epidemiological study. Am J Sports Med. 2007;35(3):368–373. doi: 10.1177/0363546506297909. [DOI] [PubMed] [Google Scholar]
- 10.Sherrington C. S. The Integrative Action of the Nervous System. New York, NY: Charles Scribner's Sons; 1906. [Google Scholar]
- 11.Lee H. M., Liau J. J., Cheng C. K., Tan C. M., Shih J. T. Evaluation of shoulder proprioception following muscle fatigue. Clin Biomech (Bristol, Avon) 2003;18(9):843–847. doi: 10.1016/s0268-0033(03)00151-7. [DOI] [PubMed] [Google Scholar]
- 12.Wassinger C. A., Myers J. B., Gatti J. M., Conley K. M., Lephart S. M. Proprioception and throwing accuracy in the dominant shoulder after cryotherapy. J Athl Train. 2007;42(1):84–89. [PMC free article] [PubMed] [Google Scholar]
- 13.Waddington G., Adams R. Discrimination of active plantarflexion and inversion movements after ankle injury. Aust J Physiother. 1999;45(1):7–13. doi: 10.1016/s0004-9514(14)60335-4. [DOI] [PubMed] [Google Scholar]
- 14.Ribeiro F., Mota J., Oliveira J. Effect of exercise-induced fatigue on position sense of the knee in the elderly. Eur J Appl Physiol. 2007;99(4):379–385. doi: 10.1007/s00421-006-0357-8. [DOI] [PubMed] [Google Scholar]
- 15.Rozzi S., Yuktananandan P., Pincevero D., Lephart S. M. Role of fatigue on proprioception and neuromuscular control. In: Lephart S. M., Fu F. H., editors. Proprioception and Neuromuscular Control in Joint Stability. Champaign, IL: Human Kinetics; 2000. pp. 375–384. [Google Scholar]
- 16.Bennell K., Wee E., Crossley K., Stillman B., Hodges P. Effects of experimentally-induced anterior knee pain on knee joint position sense in healthy individuals. J Orthop Res. 2005;23(1):46–53. doi: 10.1016/j.orthres.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 17.Adachi N., Ochi M., Uchio Y., Iwasa J., Ryoke K., Kuriwaka M. Mechanoreceptors in the anterior cruciate ligament contribute to the joint position sense. Acta Orthop Scand. 2002;73(3):330–334. doi: 10.1080/000164702320155356. [DOI] [PubMed] [Google Scholar]
- 18.Katayama M., Higuchi H., Kimura M., et al. Proprioception and performance after anterior cruciate ligament rupture. Int Orthop. 2004;28(5):278–281. doi: 10.1007/s00264-004-0583-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barrack R. L., Skinner H. B., Buckley S. L. Proprioception in the anterior cruciate deficient knee. Am J Sports Med. 1989;17(1):1–6. doi: 10.1177/036354658901700101. [DOI] [PubMed] [Google Scholar]
- 20.Ghaffarinejad F., Taghizadeh S., Mohammadi F. Effect of static stretching of muscles surrounding the knee on knee joint position sense. Br J Sports Med. 2007;41(10):684–687. doi: 10.1136/bjsm.2006.032425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miura K., Ishibashi Y., Tsuda E., Okamura Y., Otsuka H., Toh S. The effect of local and general fatigue on knee proprioception. Arthroscopy. 2004;20(4):414–418. doi: 10.1016/j.arthro.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 22.Skinner H. B., Wyatt M. P., Hodgdon J. A., Conard D. W., Barrack R. L. Effect of fatigue on joint position sense of the knee. J Orthop Res. 1986;4(1):112–116. doi: 10.1002/jor.1100040115. [DOI] [PubMed] [Google Scholar]
- 23.Callaghan M. J., Selfe J., Bagley P. J., Oldham J. A. The effects of patellar taping on knee joint proprioception. J Athl Train. 2002;37(1):19–24. [PMC free article] [PubMed] [Google Scholar]
- 24.Jerosch J., Prymka M. Knee joint proprioception in normal volunteers and patients with anterior cruciate ligament tears, taking special account of the effect of a knee bandage. Arch Orthop Trauma Surg. 1996;115(3–4):162–166. doi: 10.1007/BF00434546. [DOI] [PubMed] [Google Scholar]
- 25.Dover G., Powers M. E. Cryotherapy does not impair shoulder joint position sense. Arch Phys Med Rehabil. 2004;85(8):1241–1246. doi: 10.1016/j.apmr.2003.11.030. [DOI] [PubMed] [Google Scholar]
- 26.Hopper D., Whittington D., Davies J. Does ice immersion influence ankle joint position sense? Physiother Res Int. 1997;2(4):223–236. doi: 10.1002/pri.108. [DOI] [PubMed] [Google Scholar]
- 27.Uchio Y., Ochi M., Fujihara A., Adachi N., Iwasa J., Sakai Y. Cryotherapy influences joint laxity and position sense of the healthy knee joint. Arch Phys Med Rehabil. 2003;84(1):131–135. doi: 10.1053/apmr.2003.50074. [DOI] [PubMed] [Google Scholar]
- 28.Surenkok O., Aytar A., Tuzun E. H., Akman M. N. Cryotherapy impairs knee joint position sense and balance. Isokinet Exerc Sci. 2008;16(1):69–73. [Google Scholar]
- 29.LaRiviere J., Osternig L. The effect of ice immersion on joint position sense. J Sport Rehabil. 1994;3(1):58–67. [Google Scholar]
- 30.Ozmun J. C., Thieme H. A., Ingersoll C. D., Knight K. L. Cooling does not affect knee proprioception. J Athl Train. 1996;31(1):8–11. [PMC free article] [PubMed] [Google Scholar]
- 31.Maher C. G., Sherrington C., Herbert R. D., Moseley A. M., Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713–721. [PubMed] [Google Scholar]
- 32.Hubbard T. J., Aronson S. L., Denegar C. R. Does cryotherapy hasten return to participation? A systematic review. J Athl Train. 2004;39(1):88–94. [PMC free article] [PubMed] [Google Scholar]
- 33.Teasell R. W., Foley N. C., Bhogal S. K., Speechley M. R. Stroke rehabilitation evidence-based review: methodology. Top Stroke Rehabil. 2003;10(1):1–7. [PubMed] [Google Scholar]
- 34.Morris S. B. Estimating effect sizes from pretest-posttest-control group designs. Organ Res Meth. 2008;11(2):364–386. [Google Scholar]
- 35.Cohen L., Manion L., Morrison K. Research Methods in Education. New York, NY: Routledge; 2007. pp. 521–522. [Google Scholar]
- 36.Ebell M. H., Siwek J., Weiss B. D., et al. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. J Am Board Fam Pract. 2004;17(1):59–67. doi: 10.3122/jabfm.17.1.59. [DOI] [PubMed] [Google Scholar]
- 37.McKeon P. O., Hertel J. Systematic review of postural control and lateral ankle instability, part I: can deficits be detected with instrumented testing? J Athl Train. 2008;43(3):293–304. doi: 10.4085/1062-6050-43.3.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grob K. R., Kuster M. S., Higgins S. A., Lloyd D. G., Yata H. Lack of correlation between different measurements of proprioception in the knee. J Bone Joint Surg Br. 2002;84(4):614–618. doi: 10.1302/0301-620x.84b4.11241. [DOI] [PubMed] [Google Scholar]
- 39.Riemann B. L., Lephart S. M. The sensorimotor system, part I: the physiologic basis of functional joint stability. J Athl Train. 2002;37(1):71–79. [PMC free article] [PubMed] [Google Scholar]
- 40.Hart J. M., Leonard J. L., Ingersoll C. D. Single-leg landing strategy after knee-joint cryotherapy. J Sport Rehabil. 2005;14(4):313–320. [Google Scholar]
- 41.Olsson L., Lund H., Henriksen M., Rogind H., Bliddal H., Danneskiold-Samsøe B. Test–retest reliability of a knee joint position sense measurement method in sitting and prone position. Adv Physiother. 2004;6(1):37–47. [Google Scholar]
- 42.Ruiz D. H., Myrer J. W., Durrant E., Fellingham G. W. Cryotherapy and sequential exercise bouts following cryotherapy on concentric and eccentric strength in the quadriceps. J Athl Train. 1993;28(4):320–323. [PMC free article] [PubMed] [Google Scholar]
- 43.Todnem K., Knudsen G., Riise T., Nyland H., Aarli J. A. The non-linear relationship between nerve conduction velocity and skin temperature. J Neurol Neurosurg Psychiatry. 1989;52(4):497–501. doi: 10.1136/jnnp.52.4.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yanagisawa O., Homma T., Okuwaki T., Shimao D., Takahashi H. Effects of cooling on human skin and skeletal muscle. Eur J Appl Physiol. 2007;100(6):737–745. doi: 10.1007/s00421-007-0470-3. [DOI] [PubMed] [Google Scholar]
- 45.Hardaker N., Selfe J., Richards J., Sullivan I., Moss A., Jarvis S. Relationship between intramuscular temperature and skin surface temperature as measured by thermal imaging camera. Thermol Int. 2007;17(2):45–50. [Google Scholar]
- 46.Zemke J. E., Andersen J. C., Guion W. K., McMillan J., Joyner A. B. Intramuscular temperature responses in the human leg to two forms of cryotherapy: ice massage and ice bag. J Orthop Sport Phys Ther. 1998;27(4):301–307. doi: 10.2519/jospt.1998.27.4.301. [DOI] [PubMed] [Google Scholar]
- 47.Myrer J. W., Measom G., Fellingham G. W. Temperature changes in the human leg during and after two methods of cryotherapy. J Athl Train. 1998;33(1):25–29. [PMC free article] [PubMed] [Google Scholar]
- 48.Jameson A. G., Kinzey S. J., Hallam J. S. Lower-extremity-joint cryotherapy does not affect vertical ground-reaction forces during landing. J Sport Rehabil. 2001;10(2):132–142. [Google Scholar]
- 49.Kinzey S. J., Cordova M. L., Gallen K. J., Smith J. C., Moore J. B. The effects of cryotherapy on ground-reaction forces produced during a functional task. J Sport Rehabil. 2000;9(1):3–14. [Google Scholar]
- 50.Dewhurst S., Riches P. E., De Vito G. Moderate alterations in lower limbs muscle temperature do not affect postural stability during quiet standing in both young and older women. J Electromyogr Kinesiol. 2007;17(3):292–298. doi: 10.1016/j.jelekin.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 51.Kernozek T. W., Greany J. F., Anderson D. R., et al. The effect of immersion cryotherapy on medial-lateral postural sway variability in individuals with a lateral ankle sprain. Physiother Res Int. 2008;13(2):107–118. doi: 10.1002/pri.393. [DOI] [PubMed] [Google Scholar]
- 52.Magnusson M., Enbom H., Johansson R., Wiklund J. Significance of pressor input from the human feet in lateral postural control: the effect of hyperthermia on galvanically induced body-sway. Acta Otolaryngol. 1990;110(5–6):321–327. doi: 10.3109/00016489009107450. [DOI] [PubMed] [Google Scholar]
- 53.Saam F., Leidinger B., Tibesku C. O. The influence of cryotherapy of the ankle on static balance. Sportverletz Sportschaden. 2008;22(1):45–51. doi: 10.1055/s-2007-963601. [DOI] [PubMed] [Google Scholar]
- 54.Ingersoll C. D., Knight K. L., Merrick M. A. Sensory perception of the foot and ankle following therapeutic applications of heat and cold. J Athl Train. 1992;27(3):231–234. [PMC free article] [PubMed] [Google Scholar]
- 55.Rubley M. D., Gruenenfelder A. R., Tandy R. D., Holcomb W. R. Effects of cold and warm bath immersions on postural stability [abstract] J Athl Train. 2004;39(suppl 2):S-33. [Google Scholar]
- 56.Miniello S., Dover G., Powers M., Tillman M., Wikstrom E. Lower leg cold immersion does not impair dynamic stability in healthy women. J Sport Rehabil. 2005;14(3):234–247. [Google Scholar]
- 57.Selfe J., Callaghan M., McHenry A., Richards J., Oldham J. An investigation into the effect of number of trials during proprioceptive testing in patients with patellofemoral pain syndrome. J Orthop Res. 2006;24(6):1218–1224. doi: 10.1002/jor.20127. [DOI] [PubMed] [Google Scholar]