Abstract
BACKGROUND
Trauma survivors with posttraumatic stress disorder (PTSD) report heightened physiological responses to a wide range of stimuli. It has been suggested that associative learning and stimulus generalization play a key role in the development of these symptoms. Some studies have found that trauma survivors with PTSD show greater physiological responses to individualized trauma reminders in the initial weeks after trauma than those without PTSD. This study investigated whether heart rate and skin conductance responses (HRR, SCR) to standardized trauma-related pictures at 1 month after the trauma predict chronic PTSD.
METHOD
Survivors of motor vehicle accidents or physical assaults (N=166) watched standardized trauma-related, generally threatening and neutral pictures at 1 month post- trauma while their HRR and SCR were recorded. PTSD symptoms were assessed with structured clinical interviews at 1 and 6 months; self-reports of fear responses and dissociation during trauma were obtained soon after the trauma.
RESULTS
At 1 month, trauma survivors with PTSD showed greater HRR to trauma-related pictures than those without PTSD, but not to general threat or neutral pictures. HRR to trauma-related pictures predicted PTSD severity at 1 and 6 months, and were related to fear and dissociation during trauma. SCR was not related to PTSD.
CONCLUSION
HRR to standardized trauma reminders at 1 month after the trauma differentiate between trauma survivors with and without PTSD, and predict chronic PTSD. Results are consistent with a role of associative learning in PTSD and suggest that early stimulus generalization may be an indicator of risk for chronic PTSD.
Keywords: Posttraumatic stress disorder, psychophysiology, prospective study, associative learning, dissociation, anxiety
People with posttraumatic stress disorder (PTSD) report heightened physiological responses to internal or external cues that symbolize or resemble an aspect of the trauma (1). Clinical observations suggest that these responses can be triggered by a wide range of stimuli. Furthermore, clinical observations suggest that people with PTSD may react with emotional and physiological arousal to situations that have little similarity with the trauma but overlap in particular sensory impressions (e.g. a similar color, smell or sound; 2).
Models of PTSD draw on associative learning mechanisms to explain this heightened physiological and emotional reactivity (2-6). It has been suggested that during trauma fear responses become associated with stimuli that are present at the time, and subsequently generalize more broadly to stimuli and situations that resemble the original trauma (4 - 5).
One way of investigating the role of associative learning in PTSD is to measure physiological responses to trauma reminders. Several studies have demonstrated a heightened physiological reactivity in trauma survivors with PTSD compared to traumatized and non-traumatized controls (for reviews see 7 - 9). This is consistent with the notion that learned fear responses acquired during trauma contribute to PTSD.
There has been a longstanding interest in trauma research whether psychophysiological responses are useful in diagnosing PTSD and in identifying people at risk of chronic PTSD soon after trauma (7). Psychophysiological measures may provide useful additional information to the widely used self-report measures. In Pole’s meta-analysis (9), psychophysiological responses to standardized trauma cues identified PTSD with a mean sensitivity of .77 and a mean specificity of .91. Responses to idiographic trauma cues identified PTSD with a mean specificity of .65 and mean specificity of .83.
However, most of the studies to date were cross-sectional comparisons of survivors of very distant traumas, such as combat or sexual abuse in childhood (e.g. 10, 11). This limits the conclusiveness of the results for the development of PTSD, as the heightened physiological reactivity may be a consequence of chronic PTSD rather than a factor contributing to its development. It is thus unclear whether the reasonable sensitivity and specificity observed in these studies also applies for the early identification of trauma survivors at risk of chronic PTSD. This question is of considerable interest as many survivors recover on their own (12) and it is unclear how best to identify those who need intervention.
Few studies to date have investigated physiological responses to trauma reminders soon after trauma. Elsesser et al. (13) found that chronic PTSD patients and recent trauma survivors who met criteria for acute stress disorders (ASD) at 6 weeks after the trauma showed heart rate acceleration to individualized trauma-related pictures, whereas nontraumatized controls and survivors without ASD showed heart rate deceleration. The groups did not differ in heart rate responses (HRR) to generally threatening or neutral pictures. Blanchard et al. (14) studied survivors of motor vehicle accidents (MVA) at about 2.5 months after the trauma and found that HRR to audiotaped individualized scripts describing the participants’ accident, but not responses to other stressors, distinguished survivors with PTSD from those without PTSD and nontraumatized controls. These results are in line with the notion that in the initial months after trauma, PTSD is characterized by strong learned fear responses to reminders of the trauma.
There is also preliminary evidence that HRR to trauma reminders can be used to predict the chronicity of PTSD. Elsesser et al. (15) followed up 35 recent trauma survivors from their 2004 study and found that greater HRR to the individualized trauma-related pictures predicted PTSD symptoms 3 months later. Blanchard et al. (14) found that HR acceleration to individualized MVA scripts predicted chronicity of PTSD at 1 year in 48 participants who had PTSD at the initial assessment. Kleim, Ehlers and Glucksman (16) found that HRR to guided imagery of the trauma at 2 weeks predicted PTSD severity at 6 months after the trauma in female, but not male assault survivors.
These studies are of possible clinical relevance as they suggest that early psychophysiological responses may be useful in identifying trauma survivors at risk of chronic PTSD. So far, the studies that investigated whether early physiological responses to trauma reminders predict PTSD used idiographic trauma reminders that were selected because of their personal relevance to the participants, mainly script-driven-imagery of one’s trauma (14, 16) or idiographic pictures selected for their personal relevance to each participant (13). This raises the question of whether HRR to standardized sets of trauma reminders would also be predictive of chronic PTSD. If associative learning theories of PTSD are correct, then one would expect stimulus generalization soon after the trauma to contribute to the chronicity of PTSD. The present study was designed to investigate whether HRR to standardized trauma-related pictures can be used to identify people who will develop chronic PTSD. This question is of potential practical interest as many trauma survivors recover from initial symptoms of PTSD (12) and screening tools that allow the identification of those at risk of chronic PTSD are needed for the efficient allocation of scarce treatment resources. Currently, such screening relies on self-report symptom measures (17), as studies have shown that initial symptom severity is a relatively good predictor of chronic PTSD (18). It was therefore of particular interest to investigate whether HRR to standardized trauma pictures predicts chronic PTSD over and above what could be predicted from self-reported symptoms at one month after the trauma. The present prospective study assessed trauma survivors at 1 and 6 months. The study built on two earlier studies suggesting that recent trauma survivors with PTSD and patients with chronic PTSD may show heightened HRR to standardized trauma-related pictures compared to those without PTSD (20, 21). In contrast, however, Blanchard et al. (14, 19) found that HRR to guided imagery of a standard MVA script or videotapes of car crashes did not distinguish between survivors with and without PTSD.
The present study also explored whether skin conductance responses to trauma reminders are related to PTSD. Previous studies have suggested that HRR are particularly sensitive in detecting response differences between people with and without PTSD (9). In studies of early responses after trauma, HRR also showed the most robust findings. In Elsesser et al.’s (13) study, startle responses did not show an interaction between group and picture type. Similarly, in Blanchard et al.’s (14) study, EMG and blood pressure responses did not distinguish between the PTSD and no PTSD groups. Skin conductance responses (SCR) were chosen for this study because SCR are widely used as a measure of conditioned emotional responses in laboratory studies (e.g. 22) and because SCR has been shown to differentiate between people with chronic PTSD and controls in some, but not all idiographic trauma cue studies (9). Furthermore, Elsesser et al.’s study (13) did not find any differences in SCR between participants with and without PTSD (unpublished data, personal communication, Dr. Karin Elsesser, September 18, 2009).
Finally, the present study examined whether HRR to trauma reminders are related to the participants’ emotional and cognitive responses during the trauma, in particular to the degree of peri-traumatic fear and dissociation. These responses have been shown to predict PTSD (23- 25). The literature on conditioning suggests that stronger emotional arousal during trauma leads to stronger conditioned emotional responses (26, 27). Peri-traumatic dissociation is thought to decrease focal attention, and to promote a perceptual processing style that is characteristic of PTSD (28, 29). Ehlers, Hackmann and Michael (30) proposed that perceptual processing during trauma facilitates memory processes that rely on perceptual operations, such as associative learning.
In sum, the present study investigated the following hypotheses:
Hypothesis 1: Participants with PTSD show greater HRR to trauma-related pictures than participants without PTSD, but not to generally threatening or neutral pictures.
Hypothesis 2: Greater HRR to trauma-related pictures at 1 month predict greater PTSD symptom severity at 6 months.
Hypothesis 3: Peri-traumatic dissociation and fear during trauma predict greater HRR to trauma-related pictures at 1 month.
Furthermore, the study explored whether SCR to standardized trauma cues is associated with PTSD as the previous findings on this response are mixed.
Methods
Sample
Participants were recruited from assault or MVA survivors who were treated for their injuries at the Emergency Department of a large urban teaching hospital during the period of August 2006 and February 2008. To be eligible for the study, participants had to meet the trauma (A) criterion of DSM-IV (1), and understand and speak English fluently enough to be able to answer interview questions and fill in questionnaires. Participants with current psychosis and substance dependence, as well as those who could not remember the event (e.g., due to a head injury) were excluded. A total of 213 trauma survivors were recruited shortly after their trauma and attended the research session. Of these, 15 (4 with PTSD, 11 without PTSD) had to be excluded prior to analysis for the following reasons: use of medication that may affect HR such as β- blockers or tricyclic antidepressants (n = 7); participant fell asleep during the experiment (n = 2); movement artefacts (n = 5); and experiment stopped early due to distress (n = 1). Data from 22 participants (4 with PTSD, 18 without PTSD) were missing due to technical and recording problems. Therefore, the final sample size comprised 166 trauma survivors (56 with PTSD, 110 without PTSD). 131 participants (79%) took part in the follow-up interview 6 months post-trauma. Participants who dropped out did not differ from participants who completed the follow-up on sex, age, ethnic group, PTSD diagnosis and symptom severity, depressive symptoms, and tobacco and alcohol consumption (pmin=.21 to pmax=.58). If participants still had PTSD at the 6 month follow-up (or earlier if the participant was very distressed or at risk), we liaised with their family doctors to arrange treatment. Two participants received an effective psychological treatment for PTSD before the 6 month-follow up; their pretreatment scores were used for data analysis.
Table 1 shows sample characteristics. Participants with and without PTSD did not differ in sex, age, ethnic group, alcohol consumption, time since the trauma at research session, and injury severity. Participants with PTSD had lower educational attainment, were more likely to be smokers, and were more likely to have been injured in an assault than the no PTSD group. As expected, the PTSD group reported more severe PTSD and depressive symptoms, and more dissociation and fear during trauma, than the no PTSD group.
Table 1.
Sample and Trauma Characteristics
| Diagnosis at 1 month | |||||
|---|---|---|---|---|---|
| Variables | Total (N=166) |
PTSD (N=56) |
No PTSD (N=110) |
Statistic for comparison between the PTSD and no PTSD groups |
|
| Sex | χ2 (1)=3.98 | p=.06 | |||
| Female | 57 | 25 | 32 | ||
| Male | 109 | 31 | 78 | ||
| Age | 35.5 (10.8) | 34.8 (11.6) | 34.6 (10.0) | t(164)=.13 | p=.90 |
| Type of trauma | χ2(2)=7.13 | p=.01 | |||
| Assault | 71 | 32 | 39 | ||
| Motor vehicle accident | 95 | 24 | 71 | ||
| Ethnic origin | χ2 (1)=.31 | p=.62 | |||
| Caucasian | 92 | 29 | 63 | ||
| Non-Caucasian | 73 | 26 | 47 | ||
| Years of Education | 15.4 (6.5) | 13.3 (3.8) | 16.3 (7.2) | t(123)=2.37 | p=.02 |
| Alcohol (units per week) | 12.4 (16.3) | 11.4 (16.8) | 12.8 (16.2) | t(125)=.43 | p=.67 |
| Tobacco dependency (%) | 32.6 | 44.4 | 27.1 | χ2(1)=4.2 | p=.05 |
| Time since trauma (days) | 37.5 (9.9) | 38.5 (10.1) | 36.9 (9.8) | t(164)=.97 | p=.33 |
| Dissociation (during trauma) | 7.4 (5.9) | 10.7 (5.7) | 5.8 (5.3) | t(155)=5.3 | p<.001 |
| Fear (during trauma) | 6.6 (3.6) | 7.8 (3.8) | 5.9 (3.4) | t(155)=3.1 | p=.001 |
| Injury severity score (ISS) | 1.9 (2.1) | 1.9 (1.7) | 2.0 (2.3) | t(133)=.35 | p=.72 |
|
| |||||
| PDS Score (1 month) | 16.10 (10.82) | 26.0 (9.2) | 11.07 (7.7) | t(164)=11.03 | p<.001 |
|
| |||||
| BDI Score (at 1 month) | 9.8 (8.7) | 17.8 (9.1) | 5.8 (4.9) | t(164)=11.1 | p<.001 |
|
| |||||
| PSSI Score (at 6 month) | 7.8 (9.8) | 28 (9.1) | 4.6 (4.7) | t(129)=16.7 | p<.001 |
Note. PTSD = Posttraumatic stress disorder; PSSI= PTSD Symptom Scale Interview; PDS = Posttraumatic Stress Diagnostic Scale; BDI= Beck Depression Inventory; ISS = Injury Severity Score.
Material
Participants viewed a series of pictures; 14 pictures were related to the participants’ trauma (i.e., assault-related pictures such as a person being threatened with a knife for assault survivors; and accident-related pictures such as a crashed car for MVA survivors), 12 generally threatening pictures (e.g. a spider on someone’s shoulder), and 12 neutral pictures (e.g. children playing soccer)1. The order of presentation was randomized for each individual, with the restriction that pictures of the same category were never presented consecutively to minimize habituation effects. Each picture was presented for 6 seconds followed by an inter-stimulus interval which varied randomly between 9 and 12 seconds. During picture presentation the participant’s heart rate and skin conductance were continuously recorded. After picture presentation, participants watched the trauma-related pictures again and rated how relevant each picture was for their personal trauma on a scale from 0 (not at all relevant) to 4 (very much relevant).
Pictures were selected in a pilot study that tested the suitability of the stimulus material. Healthy volunteers (N = 21, 7 males, mean age 27.4 years, SD = 4.5) rated the valence and arousal of the pictures on a Likert scale ranging from −10 (extremely unpleasant or relaxing) to +10 (extremely pleasant or arousing). Trauma and general threat pictures were rated as moderately to very unpleasant (M = −6.6, SD = 0.6; and M = −6.7, SD = 0.6, respectively) and as moderately arousing (M = 4.8; SD = 1.5; and M = 4.7; SD = 1.4, respectively); neutral pictures were rated as somewhat pleasant (M = 3.3; SD = 1.0) and arousing (M = 1.8; SD = 0.7). Arousal and valence ratings for trauma versus general threat pictures did not differ significantly from each other (p = .30 and p = .19, respectively). As intended, arousal ratings for trauma and general threat pictures were significantly higher than those for neutral pictures (ps < .001) and valence ratings were more negative (ps < .001).
Apparatus and physiological recording
Heart rate, skin conductance and respiration were recorded using the Varioport bio-signal recording device (Vitaport system, Becker Meditec). ECG electrodes were placed on the manubrium sterni and the left lower rib cage. The reference electrode was attached to the right lower rib cage and the ECG was recorded with a sampling rate of 256 Hz. Electrodermal activity was measured using a constant voltage system (0.5 V) and a bipolar recording with two Ag/AgCl electrodes filled with a 0.05 M NaCl electrolyte paste. SC electrodes were placed on the thenar and hypothenar palmar eminences of the non-dominant hand and SCR were recorded with a sampling rate of 256 Hz. To check for possible respiration artefacts (sighs, coughs), respiration was recorded with a Pneumotrace II transducer which was attached around the participant’s upper chest.
Questionnaire Measures and Clinical Interview
PTSD measures. The PTSD section of the Structured Clinical Interview for the DSM-IV (SCID) (32) was carried out to diagnose PTSD. PTSD symptom severity was assessed with the Posttraumatic Stress Symptom Scale Interview (PSSI) (33). The interviewer rated each of the PTSD symptoms during the past 2 weeks on a scale from 0 (not at all) to 3 (5 or more times per week/very much). The total PSS-I score is the sum of the ratings for the 17 items. Interrater-reliability for this sample was κ = 0.96 for PTSD diagnosis and κ = 0.96 for PTSD symptom severity. In addition, participants completed the Posttraumatic Stress Diagnostic Scale (PDS) (34) at 1 month post-trauma. The PDS is a reliable, validated and widely used self-report measure in research with traumatised individuals. Participants rate how often they were bothered by each PTSD symptom as defined in the DSM-IV (1) on a scale ranging from 0 (not at all or only one time) to 3 (5 or more times a week/almost always). The total severity score is the sum of all items. For the current sample, the internal consistency of the PDS was α = .93.
Depressive symptoms
Severity of depressive symptoms was assessed with the Beck Depression Inventory (BDI) (35), a standardized questionnaire with established reliability and validity.
Peritraumatic responses
Participants rated how much fear they experienced during the trauma (3 items). Each item was rated on a scale from 0 ‘not at all’ to 4 ‘very strongly’ (36). Dissociation during trauma was assessed with a short version of the State Dissociation Questionnaire α (36, α = .88), which comprises 5 items assessing different aspects of dissociation such as derealization, depersonalization, detachment, altered time sense, and emotional numbing. This measure has shown good reliability and validity in traumatised and non-traumatised samples and predicted PTSD after MVA and assault (38, 39). It correlates strongly with the Peri-traumatic Dissociation Scale (r = .79, see 35).
Injury severity score (ISS) (40) is an anatomical scoring system which is based on the medical hospital notes and provides an overall score of the severity of injuries. A trained research nurse experienced in Accident and Emergency Medicine performed the ratings.
Further measures for characterization of sample
Participants completed a General Information Questionnaire (GIQ) (36, 37), which assessed demographic and trauma characteristics and the Alcohol, Smoking and Substance Involvement Screening Test (40) to screen for the use of psychoactive substances.
Procedure
The present study used a prospective design. Participants were recruited in two ways: where possible, participants (39%) were recruited in the Emergency Department on the day of their trauma. Those participants who were admitted to the Emergency Room when no recruiter was present (61%) received an information sheet about the study and invitation letter 3 to 5 days after their trauma. Participants were assessed at 3 different time points following their trauma: (1) Upon recruitment, shortly after the trauma, participants rated their peri-traumatic fear and dissociation. ISS ratings were obtained on the basis of hospital notes. (2) Approximately 1 month after the incident, participants attended the research session that involved the picture viewing task, SCID, PSSI, PDS, BDI, and GIQ. The session also involved filling out other questionnaires that will be reported elsewhere. (3) Six months post-trauma, the PSSI was conducted again over the telephone by the same interviewer.
Data reduction and statistical analyses
HRR and SCR data were pre-processed and analyzed with a software package developed by Gamer (42).
Heart rate responses
In a first step, R-waves were detected from the ECG data. R-R-intervals were then converted into HR (in beats per minute) and sampled second-by-second. For each picture, the pre-stimulus baseline HR was defined as the HR during the last second prior to picture onset. HRR was assessed as the relative change from baseline during the 6 seconds of stimulus presentation. For each second of stimulus presentation, the pre-stimulus baseline HR was subtracted from the HR during that second. Mean HRR was the mean of the HRR during the 6 seconds for each picture of the respective picture type.
Skin conductance responses
Raw skin conductance (SC) data were downsampled to 64 Hz and smoothed with a Gaussian filter of 16 Hz. The first artefact free SCR amplitude with an onset between 1 and 3 seconds post stimulus (latency criterion) was measured (inflection to maximum) when exceeding a threshold of 0.02 μS. Finally, SCR amplitudes were log-transformed using the formula log (X+1) as recommended by Venables and Christie (43).
Statistical analyses
In this study physiological responses were measured repeatedly across time. HRR and SCR data were analyzed with Generalized Estimating Equations (GEE) to take account for the correlation between the temporal measures. Specifically, an exchangeable correlation structure was assumed to account for the within-subject correlation.
GEE provides unbiased estimates of the marginal effects, even if the assumed correlation structure is misspecified (44, 45). To safeguard a possible misspecification against the variance/covariance matrix, robust Hubert White sandwich estimators were used to adjust standard errors and hence confidence intervals and p-values (46). The following factors were included in the GEE model: the between-group factor diagnostic group (PTSD vs. no PTSD), the within-subject factor picture type (trauma, general threat and neutral), and for the HRR data the within-subject factor second (second one to six after stimulus onset). Furthermore, we included the timing when a stimulus was presented during the experiment as a covariate in the analysis, thus controlling for effects of overall habituation or sensitization during the experiment. The covariate time was coded as the position of the picture in the overall order of presentation. All possible interaction terms were added to the model. Terms which increased the model fit of the HRR / SCR data were retained in the model, and others were excluded (47).
As the PTSD and no PTSD groups differed in the proportion of participants who had experienced MVA or assault, we tested whether trauma type interacted with any of the factors specified in the GEE model. As this was not the case, data for MVA and AST participants were collapsed. Education, nicotine dependency, sex, and time since the trauma were also entered into the GEE model but dropped as no significant main effects or interactions emerged.
Correlation analyses and hierarchical multiple regression analyses were carried out using SPSS 15.0. Data were tested for normality using the Kolmogorov Smirnov test and transformed, where appropriate.
A discriminant function analysis with the mean HRR to trauma-related pictures as the independent variable and diagnostic group as the dependent variable was computed to assess how well participants could be classified into the PTSD and no PTSD groups on the basis of their HRR (sensitivity and specificity).
Results
The PTSD and no PTSD groups did not differ in their relevance ratings for the trauma-related pictures: PTSD: M = 1.5, SD = 1.0; no PTSD: M = 1.3, SD = 0.9; F (1,152) = 2.4, p = .12, η2 = .02.
Heart rate reactivity and PTSD
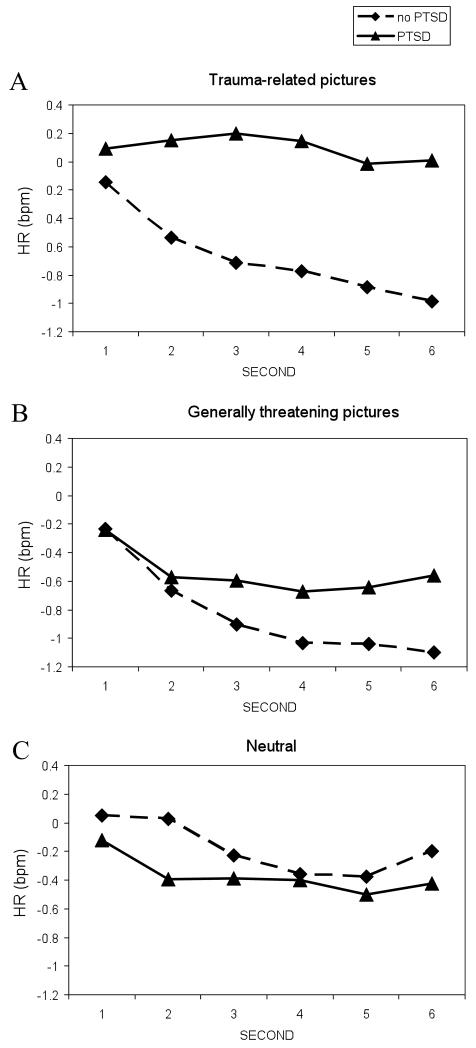
Figure 1 shows the mean HRR to the trauma, general threat and neutral pictures for the PTSD and no PTSD groups for each of the 6 seconds of stimulus presentation.
Figure 1.
Mean heart rate (HR) responses to trauma-related (A), general threat (B), and neutral (C) pictures for the PTSD and no PTSD groups in changes from pre-stimulus baseline (beats per minute). The PTSD group showed greater HR responses to the trauma-related pictures than the no PTSD group; but not to general threat or neutral pictures.
The 2 × 3 × 6 GEE model showed main effects for the factor second (χ2(5) = 27.0, p < .001), and the covariate time (χ2(1) = 10.6, p = .001), but not for diagnostic group (χ2(1) = 1.08, p = .299) and picture type (χ2(2) = 4.4, p = .111). The following interactions were included in the model: ‘diagnostic group X picture type’ (χ2(2) = 12.3, p = .002), ‘diagnostic group X second’ (χ2(2) = 4.36, p = .037), ‘picture type X time (χ2(2) = 6.90, p = .032), and ‘diagnostic group X time (χ2(1) = 1.70, p = .192). Post hoc analyses of the interaction ‘diagnostic group X picture type’ revealed that, in line with the hypothesis, the PTSD group showed greater HRR to trauma pictures than the no PTSD group (χ2(1) = 5.71, p = .017). There were no such group differences for generally threatening (χ2(1) = .74, p = .390) or neutral pictures (χ2(1) = .79, p = .372). A significant main effect of the covariate time indicated a small increase in HRR across all picture categories over the course of the experiment.
The discriminant function analysis showed that the mean HRR to the trauma-related pictures classified 63.3% of the participants correctly into the PTSD and no PTSD groups. Fifty three percent of the participants who received a PTSD diagnosis were classified as responsive (sensitivity); and 68% of the individuals without a PTSD diagnosis were classified as non-responsive (specificity).
The PTSD and no PTSD groups did not differ in pre-stimulus baseline (F (1,164) = .41, p = .52), nor was there an interaction between diagnostic group and picture type on baseline HR (F (2,163) = 1.29, p = .28) (HR before trauma-related pictures: PTSD: M = 71.4, SD = 9.1; no PTSD: M = 70.6, SD = 11.0; before general threat pictures PTSD: M = 71.8, SD = 9.2; no PTSD: M = 70.7, SD = 11.1; before neutral pictures PTSD: M = 71.6, SD = 9.3; no PTSD: M = 70.4, SD = 11.1).
Skin conductance responses
Parallel analyses for SCR showed neither significant main effects nor interactions.
Relationship of HRR with peri-traumatic responses and subsequent PTSD symptoms
The mean PSSI score at 6 months post-trauma was M = 7.8, SD = 9.8. In accordance with Hypothesis 2, greater mean HRR to trauma-related pictures at 1 month predicted PTSD symptom severity (PSSI) at 6 months (r = .27, p < .001). This correlation remained significant when controlling for self-reported PTSD symptoms (PDS) at 1 month after the trauma (r = .17, p = .046, suggesting that HRR to trauma reminders explain variance of chronic PTSD over and above initial symptoms. A multiple regression analysis showed that PDS scores and HRR to trauma pictures at 1 month together explained 28.1% of the variance of PSSI scores at 6-month follow-up, R = .53, F (2,129) = 25.22, p < .001. Entering other variables that distinguished the PTSD and no PTSD groups in the second step of the multiple regression function (sex, trauma type, level of education, fear and dissociation during the trauma, BDI), did not significantly add to the prediction, Fchange (6, 114) = 1.11, p = .36.
In line with Hypothesis 3, fear and dissociation during trauma significantly predicted mean HRR to trauma-related pictures at 1 month post-trauma (both rs = .17, ps = .02).
Discussion
The present study used a prospective design to investigate whether HRR to trauma-related pictures at 1 month after the trauma predict acute and chronic PTSD. In line with the first hypothesis, MVA and assault survivors with PTSD showed greater HRR to trauma-related pictures, but not to generally threatening or neutral pictures than those without PTSD. These results are consistent with previous findings of heightened physiological responding to idiographic trauma reminders in the initial weeks after trauma in civilian trauma survivors with PTSD (13, 14).
The present study extends these findings by demonstrating that trauma survivors with PTSD exhibit heightened HRR to standardized trauma-related pictures compared to survivors without PTSD as early as 1 month after the trauma. This result is in line with suggestions that in PTSD learned fear responses acquired during the trauma generalize to stimuli that resemble the original traumatic situation so that more and more situations trigger fear and physiological arousal (4, 5). Note that both groups of participants rated the trauma pictures as not very relevant to their personal trauma. Nevertheless, the PTSD and no PTSS group differed in their HRR. Whereas the no PTSD group showed the HR deceleration usually observed in healthy participants (48, 49), the PTSD group tended to show a more accelerative cardiac response, which is generally seen as a sign of a phobic reaction (50). This suggests that by 1 month, the PTSD group’s fear responses had generalized to general reminders of the trauma that did not have great similarity to their own trauma. Generalization of conditioned fear responses is a well-established phenomenon. Animal studies have shown that conditioned emotional responses progressively generalize to more remote stimuli (51, 52).
The present study also demonstrated that HRR to standardized trauma reminders predicted PTSD symptom severity at 6 months after the trauma. This finding extends previous prospective studies showing that HRR to individualized trauma reminders predicts chronicity of PTSD symptoms (15 - 17). The current findings suggest that the degree of generalization of learned fear responses or the speed with which it takes place may be indicators of risk for chronic PTSD. This has possible applications for the early detection of those at risk of chronic PTSD. While many trauma survivors initially develop PTSD symptoms, the majority recover in the following months. Thus, measures of risk for chronic PTSD are needed that would allow the identification of those who need early intervention. The present study suggests that HRR responses may be a useful addition to self-reports as they predicted over and above self-reported symptom severity at 1 months.
Overall, while the absence of relative HR acceleration to standardized trauma reminders was related to the absence of a PTSD diagnosis, as indicated by a satisfactory specificity of 68%, a more positive HR was less predictive of PTSD and the sensitivity was only 53%. This indicates that there may be several pathways to chronic PTSD, and generalized fear responses may only be one of them. This pattern of findings is in line with theories of PTSD that suggest several maintenance factors. For example, appraisals leading to feelings of guilt, shame or anger have also been implicated in chronic PTSD, and participants who score high on these appraisals may not show HRR (2).
The present study also explored electrodermal responding to trauma pictures but the PTSD and no PTSD groups did not differ in their SCR responses. Previous studies investigating physiological responses to standardized trauma reminders also found that HRR differentiated better between the PTSD and no PTSD groups than SCR and other measures (9). One possible explanation accounting for the differences between heart rate and skin conductance measures might be that these response systems require a different degree of contingency awareness about the relationship between triggers (CS) and the trauma (US) (53, 54). Whereas conditioned HRR do not appear to depend on contingency awareness, conditioned SCR appear to require such awareness (54). Thus, the pattern of HRR results (HR acceleration despite low perceived relevance to one’s trauma) appears to fit with clinical observations that patients with PTSD often report that their anxiety and physiological arousal appear to come “out of the blue” (2).
The results for peri-traumatic responses are in line with associative learning models of PTSD (4, 5). Fear during the trauma predicted greater HRR to trauma-related pictures at 1 month follow-up. High fear during trauma may indicate a strong activation of the sympathetic nervous system and thus lead to stronger conditioning of emotional responses, which in turn may increase the risk for PTSD. The finding that dissociation during the trauma also predicted HRR to trauma-related pictures lends some preliminary support to the suggestion that engaging in perceptual processing during trauma promotes associative learning (28). Note that some studies have found a negative relationship between dissociation and HRR to intentional recall of trauma memories in the laboratory (55, 56). In these studies, trauma survivors were asked to give a narrative of the trauma while their HR was recorded. Peritraumatic dissociation and PTSD symptoms were related to smaller HR increases during the narrative. Thus, in line with current models of PTSD (2), physiological responses during cue-driven unintentional retrieval of traumatic material (reexperiencing symptoms, response to trauma pictures) may differ from physiological responses during intentional retrieval of trauma memories.
The present study has strengths and limitations. Among its strengths are the prospective design and the large sample size. Furthermore, all trauma survivors were diagnosed with reliable structured clinical interviews. A limitation is that although this study employed a prospective design, physiological responses to trauma reminders were only recorded at one time point. It would have been desirable to administer the picture viewing task again at follow-up to test whether the heightened HRR to trauma reminders changes with recovery from PTSD and whether those with chronic PTSD show further generalization to other classes of threat stimuli (14, 15). Furthermore, arousal and valence ratings for the pictures were not taken in the main study so that possible differences between the PTSD and no PTSD groups could not be assessed; in addition it would have been interesting to examine the concordance between self-reported arousal and valence with physiological responses to trauma reminders. Finally, HRR only had limited sensitivity, but satisfactory specificity, in identifying participants at risk of chronic PTSD.
In conclusion, we found that trauma survivors with PTSD showed greater HRR to standardized visual trauma reminders at 1 month after the trauma than those without PTSD. HRR were related to fear and dissociation during the trauma. HRR at 1 month predicted PTSD symptom severity at 6 months post-trauma, and predicted over and above what could be predicted from self-reported symptoms at 1 month. The results may have practical implications for identifying people at risk of chronic PTSD after trauma. HR responders had an increased risk of chronic PTSD.
Acknowledgments
The study was funded by Wellcome Trust programme grant 069777 (Anke Ehlers). Oliver Suendermann was supported by a scholarship from the German National Academic Foundation. We are grateful to Drs. Elsesser and Sartory for providing some of the stimulus material, and to Jonathan Howard for programming the picture viewing task. We thank Emma Briddon, Judith Kalthoff, Linda Horrell, Melanie Walwyn Martin, Franziska Wallott, Marit Hauschildt, Benjamin Boecking, Anne Reitz, Sarah Auerbach and Laura Pielmaier, and the staff of King’s College Accident and Emergency Department for their help with recruitment, testing and data entry; and Daniel Stahl for statistical advice.
Supported by the Wellcome Trust and the German National Academic Foundation
ACRONYMS
- PTSD
Posttraumatic Stress Disorder
- HRR
Heart rate response
- SCR
Skin conductance response
- SCID
Structured Clinical Interview for DSM-IV
- PSSI
PTSD Symptom Scale - Interview Version
- PDS
Posttraumatic Diagnostic Scale
- MVA
motor vehicle accident
Appendix
Appendix. Content of Pictures.
| Picture | Assault-related (for assault survivors) |
MVA-related (for MVA survivors) |
General threat (all participants) |
Neutral (all participants) |
|---|---|---|---|---|
| 1 | Man threatening woman with gun. IAPS No: 6560 |
Ambulance and stretcher |
Jet fighter firing missile |
Child’s room |
| 2 | Gang beating up man | Car on dark wet street |
Man with bomb IAPS No: 2692 |
Boy playing with sailing boat |
| 3 | Gang stopping car with baseball bat IAPS No: 6821 |
Cyclist being cut off by car |
Junkie with syringe | Ice cream kiosk |
| 4 | Man pointing gun IAPS No: 6243 |
Swerving motorcyclist |
Skulls piled up IAPS No: 9440 |
Man tidying room |
| 5 | Masked man with knife IAPS No: 6510 |
Crashed motorcyclist |
Spider on shoulder IAPS No:1201 |
Surfer in wave IAPS No:5623 |
| 6 | Gang attacking man | Car crashed into tree |
Tanks rolling over street |
Man sitting under sun shade |
| 7 | Brawl in park | Cyclist in busy traffic |
Helicopter over flooded area |
Children playing soccer |
| 8 | Woman with blood in face |
Crashed bicycle | Crashed airplane | Two men chatting in living room |
| 9 | Man stalking woman | Car crashed into concrete bollard |
Dead bird covered in oil |
Boy drying his hair |
| 10 | Man being kicked on floor |
Collision of car and motorbike |
Fire fighter rescuing woman IAPS No: 9921 |
Camping site |
| 11 | Pedestrian in dark street |
Car hitting into pedestrian |
Noose of gallow | Business meeting |
| 12 |
Man beating other man with elbow |
Wrecked motorbike |
Starving child |
Business meeting |
| 13 | Man attacking woman IAPS No: 6312 |
Injured woman behind steering wheel |
||
| 14 | Man covered with blood IAPS No: 3550 |
Injured person lying on street |
Legend: MVA: motor vehicle accident; IAPS: International Affective Picture System
Footnotes
Pictures were partly drawn from the International Affective Picture System (31), namely some of the trauma pictures (6560, 6821, 6243, 6510, 6312, 3550); general threat pictures (2692, 9440, 1201, 9921), and neutral pictures (5623). All other pictures were either downloaded from online picture databases, or taken from digitalised movies or photos from magazines to create sets that were comparable in complexity. The picture sets are available from the authors.
Conflicts of Interest: None
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th edition American Psychiatric Association; Washington, D.C.: 1994. [Google Scholar]
- 2.Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behav Res Ther. 2000;38:319–45. doi: 10.1016/s0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- 3.Litz BT, Keane TM. Information processing in anxiety disorders: application to the understanding of post-traumatic stress disorder. Clin Psych Rev. 1989;9:243–257. [Google Scholar]
- 4.Keane TM, Zimering RT, Caddell JM. A behavioral formulation of posttraumatic stress disorder in Vietnam veterans. Behavior Therapist. 1985;8:9–12. [Google Scholar]
- 5.Foa EB, Steketee G, Rothbaum BO. Behavioral/cognitive conceptualizations of post-traumatic stress disorder. Behavior Therapist. 1989;20:155–76. [Google Scholar]
- 6.Brewin CR, Dalgleish T, Joseph S. A dual representation theory of posttraumatic stress disorder. Psychol Rev. 1996;103:670–86. doi: 10.1037/0033-295x.103.4.670. [DOI] [PubMed] [Google Scholar]
- 7.Orr SP, Roth WT. Psychophysiological assessment: Clinical applications for PTSD. J Affect Disord. 2000;61:225–40. doi: 10.1016/s0165-0327(00)00340-2. [DOI] [PubMed] [Google Scholar]
- 8.Orr SP, McNally RJ, Rosen GM, Shalev A. Psychophysiological reactivity: implications for conceptualising PTSD. In: Rosen GM, editor. Posttraumatic stress disorder: issues and controversies. Wiley; Chichester, West Sussex: 2004. [Google Scholar]
- 9.Pole N. The psychophysiology of posttraumatic stress disorder: a meta-analysis. Psychol Bull. 2007;133:725–46. doi: 10.1037/0033-2909.133.5.725. [DOI] [PubMed] [Google Scholar]
- 10.Orr SP, Pitman RK, Lasko NB, Herz LR. Psychophysiological assessment of posttraumatic stress disorder imagery in World War II and Korean combat veterans. J Abn Psychol. 1993;102:152–9. doi: 10.1037//0021-843x.102.1.152. [DOI] [PubMed] [Google Scholar]
- 11.Donagh-Coyle A, McHugo GJ, Friedman MJ, Schnurr PP, Zayfert C, Descamps M. Psychophysiological reactivity in female sexual abuse survivors. J Trauma Stress. 2001;14:667–83. doi: 10.1023/A:1013081803429. [DOI] [PubMed] [Google Scholar]
- 12.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–60. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 13.Elsesser K, Sartory G, Tackenberg A. Attention, Heart Rate, and Startle Response during Exposure to Trauma-Relevant Pictures: A Comparison of Recent Trauma Victims and Patients with Posttraumatic Stress Disorder. J Abn Psychol. 2004;113:289–301. doi: 10.1037/0021-843X.113.2.289. [DOI] [PubMed] [Google Scholar]
- 14.Blanchard EB, Hickling EJ, Buckley TC, Taylor AE, Vollmer A, Loos WR. Psychophysiology of posttraumatic stress disorder related to motor vehicle accidents: replication and extension. J Consult Clin Psychol. 1996;64:742–51. doi: 10.1037//0022-006x.64.4.742. [DOI] [PubMed] [Google Scholar]
- 15.Elsesser K, Sartory G, Tackenberg A. Initial symptoms and reactions to trauma-related stimuli and the development of posttraumatic stress disorder. Depress Anxiety. 2005;21:61–70. doi: 10.1002/da.20047. [DOI] [PubMed] [Google Scholar]
- 16.Kleim B, Wilhelm FH, Glucksman E, Ehlers A. Heart rate reactivity to script-driven imagery predicts PTSD in female, but not in male assault survivors. 2009. Manuscript submitted for publication. [Google Scholar]
- 17.Brewin CR. Systematic review of screening instruments for adults at risk of PTSD. J Trauma Stress. 2005;18:53–62. doi: 10.1002/jts.20007. [DOI] [PubMed] [Google Scholar]
- 18.Rothbaum BO, Foa EB, Riggs DS, Murdock T. A prospective examination of post-traumatic stress disorder in rape victims. J Trauma Stress. 1992;5:455–475. 1992. [Google Scholar]
- 19.Blanchard EB, Hickling EJ, Taylor AE, Loos WR, Gerardi RJ. The psychophysiology of motor vehicle accident related posttraumatic stress disorder. Behav Ther. 1994;25:453–67. doi: 10.1007/BF00999995. [DOI] [PubMed] [Google Scholar]
- 20.Rabe S, Dorfel D, Zollner T, Maercker A, Karl A. Cardiovascular correlates of motor vehicle accident related posttraumatic stress disorder and its successful treatment. Appl Psychophysiol Biofeedback. 2006;31:315–30. doi: 10.1007/s10484-006-9027-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ehlers A, Suendermann O, Vossbeck-Elsebusch A, Boellinghaus I, Briddon E, Walwyn Martin M, Gamer M. Heart rate responses and psychopathology after trauma. 2009. Submitted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Orr SP, Metzger LJ, Laski N, Macklin ML, Peri T, Pitman RK. De novo conditioning in trauma-exposed individuals with and without posttraumatic stress disorder. J Abn Psychol. 2000;109:290–8. [PubMed] [Google Scholar]
- 23.Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychol Bull. 2003;129:52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- 24.Nixon RD, Bryant RA, Moulds ML, Felmingham KL, Mastrodomenico JA. Physiological arousal and dissociation in acute trauma victims during trauma narratives. J Trauma Stress. 2005;18:107–13. doi: 10.1002/jts.20019. [DOI] [PubMed] [Google Scholar]
- 25.Ehring T, Ehlers A, Glucksman E. Do cognitive models help in predicting the severity of posttraumatic stress disorder, phobia, and depression after motor vehicle accidents? A prospective longitudinal study. J Consult Clin Psychol. 2008;76:219–30. doi: 10.1037/0022-006X.76.2.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.LeDoux JE. Emotion circuits in the brain. Annu Rev Neurosci. 2000;23:155–84. doi: 10.1146/annurev.neuro.23.1.155. [DOI] [PubMed] [Google Scholar]
- 27.Charney DS, Deutch AY, Krystal JH, Southwick SM, Davis M. Psychobiologic mechanisms of posttraumatic stress disorder. Arch Gen Psychiatry. 1993;50:295–305. doi: 10.1001/archpsyc.1993.01820160064008. [DOI] [PubMed] [Google Scholar]
- 28.Brewin CR, Dalgleish T, Joseph S. A dual representation theory of posttraumatic stress disorder. Psychol Rev. 1996;103:670–86. doi: 10.1037/0033-295x.103.4.670. [DOI] [PubMed] [Google Scholar]
- 29.Siegel DJ. Memory, trauma, and psychotherapy. J Psychother Pract Res. 1995;4:93–122. [PMC free article] [PubMed] [Google Scholar]
- 30.Ehlers A, Hackmann A, Michael T. Intrusive re-experiencing in post-traumatic stress disorder: Phenomenology, theory, and therapy. Memory. 2004;12:403–15. doi: 10.1080/09658210444000025. [DOI] [PubMed] [Google Scholar]
- 31.Lang PJ, Bradley MM, Cuthbert BN. International Affective Picture System (IAPS): Affective rating of measures and instruction manual (Tech. Rep.A-6) University of Florida; Gainesville, FL: 2005. [Google Scholar]
- 32.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV axis I disorders. American Psychiatric Press; Washington, D.C.: 1996. [Google Scholar]
- 33.Foa EB, Tolin DF. Comparison of the PTSD Symptom Scale-Interview Version and the Clinician-Administered PTSD scale. J Trauma Stress. 2000;13:181–91. doi: 10.1023/A:1007781909213. [DOI] [PubMed] [Google Scholar]
- 34.Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychol Assess. 1997;9:445–51. [Google Scholar]
- 35.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 36.Halligan SL, Michael T, Clark DM, Ehlers A. Posttraumatic stress disorder following assault: The role of cognitive processing, trauma memory, and appraisals. J Consult Clin Psychol. 2003;71:419–31. doi: 10.1037/0022-006x.71.3.419. [DOI] [PubMed] [Google Scholar]
- 37.Murray J, Ehlers A, Mayou RA. Dissociation and posttraumatic stress disorder: Two prospective studies of motor vehicle accident survivors. Br J Psychiatry. 2002;180:363–8. doi: 10.1192/bjp.180.4.363. [DOI] [PubMed] [Google Scholar]
- 38.Ehring T, Ehlers A, Glucksman E. Contribution of cognitive factors to the prediction of post-traumatic stress disorder, phobia and depression after motor vehicle accidents. Behav Res Ther. 2006;44:1699–716. doi: 10.1016/j.brat.2005.11.013. [DOI] [PubMed] [Google Scholar]
- 39.Kleim B, Ehlers A, Glucksman E. Early predictors of chronic post-traumatic stress disorder in assault survivors. Psychol Med. 2007;37:1457–67. doi: 10.1017/S0033291707001006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Baker SP. The Injury Severity score: A method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–96. [PubMed] [Google Scholar]
- 41.ASSIST Working Group . The Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST 2.0) World Health Organization; Geneva: 2002. [Google Scholar]
- 42.Gamer M. Software package for the analysis of physiological data. 2007. Computer Program. [Google Scholar]
- 43.Venables PH, Christie MJ. Electrodermal activity. In: Martin I, Venables PH, editors. Techniques in Psychophysiology. Wiley; Chichester: 1980. pp. 3–67. [Google Scholar]
- 44.Hardin JW, Hilbe JM. Generalized Estimating Equations. Chapman & Hall/CRC; Boca Raton, FL: 2003. [Google Scholar]
- 45.Rabe-Hesketh S, Skrondal A. Multilevel and longitudinal modelling using Stata. Stata Press; College Station, TX: 2005. [Google Scholar]
- 46.Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000;56:645–6. doi: 10.1111/j.0006-341x.2000.00645.x. [DOI] [PubMed] [Google Scholar]
- 47.Burnham K, Anderson DR. Model selection and multimodel inference. Springer; New York: 2002. [Google Scholar]
- 48.Lang PJ, Greenwald MK, Bradley MM, Hamm AO. Looking at pictures: affective, facial, visceral, and behavioral reactions. Psychophysiol. 1993;30:261–73. doi: 10.1111/j.1469-8986.1993.tb03352.x. [DOI] [PubMed] [Google Scholar]
- 49.Bradley MM, Codispoti M, Cuthbert BN, Lang PJ. Emotion and motivation I: defensive and appetitive reactions in picture processing. Emotion. 2001;1:276–298. 2001. [PubMed] [Google Scholar]
- 50.Sartory G. Orienting and psychopathology: Anxiety and phobias. In: Siddle DA, editor. Orienting and habituation: Perspectives in human research. Wiley; 1983. pp. 449–74. [Google Scholar]
- 51.Delgado MR, Olsson A, Phelps EA. Extending animal models of fear conditioning to humans. Biol Psychol. 2006;73:39–48. doi: 10.1016/j.biopsycho.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 52.Bouton ME, Moody EW. Memory processes in classical conditioning. Neurosci Biobehavi Rev. 2004;28:663–74. doi: 10.1016/j.neubiorev.2004.09.001. [DOI] [PubMed] [Google Scholar]
- 53.Weisz N, Kostadinov B, Dohrmann K, Hartmann T, Schlee W. Tracking short-term auditory cortical plasticity during classical conditioning using frequency-tagged stimuli. Cereb Cortex. 2007;17:1867–76. doi: 10.1093/cercor/bhl095. [DOI] [PubMed] [Google Scholar]
- 54.Klucken T, Kagerer S, Schweckendiek J, Tabbert K, Vaitl D, Stark R. Neural, electrodermal and behavioral response patterns in contingency aware and unaware subjects during a picture-picture conditioning paradigm. Neuroscience. 2009;158:721–31. doi: 10.1016/j.neuroscience.2008.09.049. [DOI] [PubMed] [Google Scholar]
- 55.Griffin MG, Resick PA, Mechanic MB. Objective assessment of peritraumatic dissociation: Psychophysiological indicators. Am J Psychiatry. 1997;154:1081–1088. doi: 10.1176/ajp.154.8.1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Halligan SL, Michael T, Wilhelm F, Clark DM, Ehlers A. Reduced heart rate responding to trauma reliving in trauma survivors with PTSD: correlates and consequences. J Trauma Stress. 2006;19:721–734. doi: 10.1002/jts.20167. [DOI] [PubMed] [Google Scholar]