Abstract
In our study of nursing home residents with clinically suspected urinary tract infection who did not require the use of an indwelling catheter, we identified bacteria isolated from urine samples, the resistance patterns of these isolated bacteria, and the antibiotic therapy prescribed to the residents. Escherichia coli, the predominant organism isolated, frequently was resistant to commonly prescribed oral antibiotics. Trimethoprim-sulfamethoxazole remains the best empiric antimicrobial therapy for a urinary tract infection, but nitrofurantoin should be considered if E. coli is identified.
Asymptomatic bacteriuria and urinary tract infection (UTI) are highly prevalent among nursing home residents, and UTI is the most common indication for antimicrobial therapy.1 Of all the cases of antimicrobial use in nursing homes, 20%–60% of cases can be attributed to UTI, even though only 30%–60% of those cases are considered appropriate for antimicrobial therapy.2 With the emergence of antimicrobial-resistant bacteria, the role that nursing homes play in the development and spread of these organisms becomes an important focus of investigation.3
Prior studies have examined the prevalence of antimicrobial-resistant uropathogens among nursing home residents. In 4 nursing homes in Pennsylvania, Escherichia coli and Proteus mirabilis demonstrated increasing resistance to fluoroquinolones over the course of 5.5 years.4 Prior fluoroquinolone use has been identified as a risk factor for infection with fluoroquinolone-resistant E. coli.5 In contrast, in a Norwegian study, bacteria isolated from urine samples continued to be highly susceptible to commonly prescribed oral antibiotics.6
Among nursing home residents, treatment for asymptomatic bacteriuria does not eradicate bacteriuria, decrease the number of UTI episodes, or improve mortality.1 Because the diagnosis and empiric management of UTI is challenging, greater attention must be placed on the epidemiology of the bacteria isolated from urine samples and on antimicrobial prescribing practices. In our study of nursing home residents with clinically suspected UTI who did not require the use of an indwelling catheter, we identified bacteria isolated from urine samples, the resistance patterns of these isolated bacteria, and the antibiotic therapy prescribed to the residents.
METHODS
The cohort was comprised of residents from 5 nursing homes in New Haven, Connecticut, during the study period from May 2005 through May 2007; these nursing homes ranged in size from 120 to 360 beds. Residents were excluded from our study if (1) it was anticipated that they would remain in the nursing home for a short time, because they were either short-term rehabilitation residents, were going to be discharged soon, or were terminally ill (ie, had an anticipated life expectancy of less than 4 weeks); (2) they were less than 65 years old; (3) they required the use of an indwelling catheter; (4) they were receiving dialysis; (5) they were undergoing chronic suppressive anti-infective therapy for recurrent UTI; or (6) they were residence for less than 4 weeks. All eligible residents (or their surrogates) who could be contacted were approached for verbal consent. Of the 942 residents who were screened, 644 met the eligibility criteria, and 551 enrolled (86% response rate).
Participants were followed for 1 year or until any of the following occurred: death, placement on chronic suppressive antibiotic therapy, discharge, or insertion of a long-term indwelling catheter. Our study was approved by the Yale University Human Investigation Committee, the Hospital of St. Raphael's institutional review board, and each nursing home's medical board.
At baseline, demographic information was obtained by chart review. At the time of diagnosis of clinically suspected UTI, defined as a report of clinical suspicion of UTI by the nursing home resident's physician or nurse,7 nursing home staff obtained a urine sample for culture. Descriptive statistics were generated using SAS, version 9.2 (SAS).
RESULTS
Of the 551 residents who participated in our study, 311 had no episodes of clinically suspected UTI episodes, whereas 240 had a total of 454 episodes. For 411 (91%) of the 454 episodes, urine samples were sent to the laboratory for testing. For 301 of these episodes, bacterial growth was detected in the urine samples obtained from the residents (211 episodes with a urine sample with more than 100,000 colony-forming units [cfu] of bacteria per milliliter, 63 episodes with 10,000–100,000 cfu/mL, and 27 episodes with less than 10,000 cfu/mL). For 105 of these episodes, no bacterial growth was detected in the urine samples obtained from the residents. For 5 of these episodes, the urine samples obtained from the residents were contaminated (defined on the basis of growth of more than 3 different bacteria). There were 267 isolates identified with bacterial growth of more than 10,000 cfu/mL and with antimicrobial susceptibility information available.
The 267 isolates, which were recovered from urine samples obtained from 171 participating residents (during a total of 240 episodes of clinically suspected UTI), were sent to the laboratory for testing. Antibiotics were prescribed for residents in 200 of the 240 episodes. The participants were predominantly female (ie, 153 [89%] of 171 residents) and white (ie, 156 residents [91%]), with a mean (± standard deviation [SD]) age of 87.1 ± 6.7 years. They had an average (±SD) of 2.2 ± 1.1 comorbidities, with approximately two-thirds of the residents receiving a diagnosis of dementia (ie, 105 [61%] of 171 residents). They took an average (±SD) of 9.1 ± 3.5 medications daily.
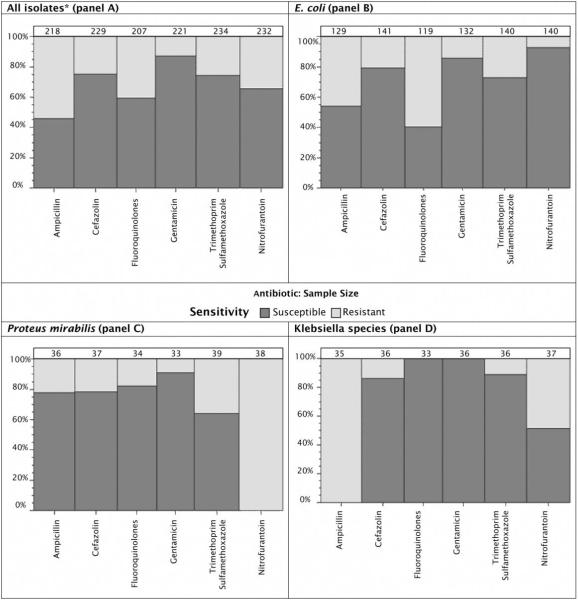
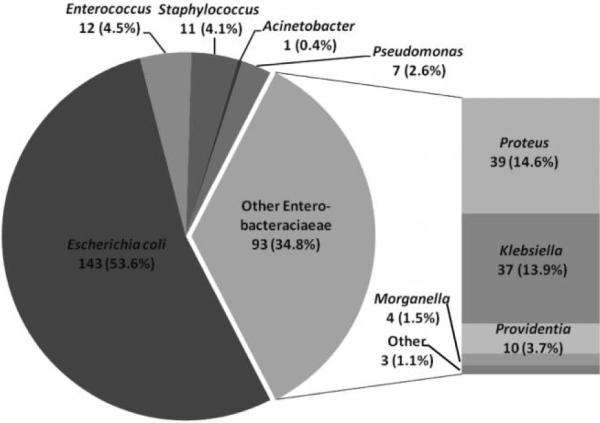
E. coli was the predominant organism isolated, followed by other Enterobacteriaceae, of which P. mirabilis was identified most frequently, followed by Klebsiella species (Figure 1). Of all the bacterial isolates (excluding the gram-positive organisms), among the oral antibiotics available, 75% were susceptible to cefazolin, and 74% were susceptible to trimethoprim-sulfamethoxazole (TMP-SMX; Figure 2A). Of the E. coli isolates, 40% were susceptible to fluoroquinolones (ie, ciprofloxacin or levofloxacin), 93% were susceptible to nitrofurantoin, and 73% were susceptible to TMP-SMX (Figure 2B). Of the P. mirabilis isolates, 82% were susceptible to fluoroquinolones, and 64% were susceptible to TMP-SMX (Figure 2C). Of Klebsiella isolates, 89% were susceptible to TMP-SMX, and 100% were susceptible to fluoroquinolones (Figure 2D). Of the 12 Enterococcus isolates, 11 (92%) were susceptible to ampicillin and nitrofurantoin; of the 7 Enterococcus isolates that were tested for susceptibility to vancomycin, all 7 were found to be susceptible. Of the 10 Staphylococcus isolates that were tested for susceptibility to methicillin, 7 (70%) were found to be resistant. Of the 9 Staphylococcus isolates that were tested for susceptibility to vancomycin, all were found to be susceptible. Of the 9 Staphylococcus isolates that were tested for susceptibility to nitrofurantoin, all were found to be susceptible. Of the 8 Staphylococcus isolates that were tested for susceptibility to TMP-SMX, all were found to be susceptible.
Figure 1.
Microbiology results of bacterial isolates recovered from urine samples obtained from 171 participating nursing home residents (during a total of 240 episodes of clinically suspected UTI) from 5 nursing homes in New Haven, Connecticut (May 2005–May 2007). There were 267 isolates identified with bacterial growth of more than 10,000 cfu/mL and with antimicrobial susceptibility information available.
Figure 2.
Antibiotic susceptibility patterns of bacterial isolates recovered from urine samples obtained from 171 participating nursing home residents (during a total of 240 episodes of clinically suspected UTI) from 5 nursing homes in New Haven, Connecticut (May 2005–May 2007). The varying widths of vertical bars are proportional to the varying sample sizes, which are noted at the top of each bar. *All gram-positive organisms have been excluded.
For 255 of the 454 clinically suspected UTI episodes, antimicrobial therapy was prescribed for the nursing home resident. For 196 of these 255 episodes, the resident had bacteriuria (ie, more than 100,000 cfu/mL). Fluoroquinolones were most frequently prescribed (for 104 [41%] of 254 episodes), followed by nitrofurantoin (58 episodes [23%]) and TMP-SMX (43 episodes [17%]). Other oral antibiotics, including amoxicillin, amoxicillin–clavulanic acid, cefuroxime, and cephalexin, were prescribed during 36 (14%) of 254 episodes. Parenteral antibiotics (ie, ceftriaxone, cefepime, piperacillin-tazobactam, and gentamicin) were prescribed during only 13 (5%) of 254 episodes. There were 47 courses of antibiotic therapy that were changed. For 28 (60%) of the 47 courses of therapy that were changed, the residents' initial therapy with fluoroquinolones was changed. For 6 (13%) of the 47 courses of therapy that were changed, the residents' initial therapy with TMP-SMX was changed. For 3 (6%) of the 47 courses of therapy that were changed, the residents' initial therapy with nitrofurantoin was changed. There were 124 participating residents who had E. coli identified in their urine sample and who received antibiotic therapy; of these, 37 (30%) received nitrofurantoin therapy, only 1 of whom had a change in antibiotic therapy. The reason for the change was not determined from the resident's medical record.
In 154 (77%) of 199 episodes, the organisms isolated from urine samples were susceptible to the initial empiric antibiotic therapy prescribed. In 31 episodes, the organisms were resistant to the empiric regimen; the course of antibiotic therapy was changed in 17 (55%) of these 31 episodes and continued in 14 (45%) of these 31 episodes.
DISCUSSION
Our study demonstrates that, although the distribution of bacterial isolates resembles that expected in an outpatient population more than 65 years of age,2 these isolates often were resistant to one or more of the frequently prescribed oral antibiotics for UTI. The susceptibility of all isolates, especially E. coli, to fluoroquinolones was inconsistent. TMP-SMX and first-generation cephalosporins maintained the best overall susceptibility pattern, whereas nitrofurantoin was most consistent for use as therapy for UTI due to E. coli.
TMP-SMX continues to be recommended as the first-line antibiotic for acute cystitis among young women and nursing home residents,8,9 but the trend of emerging resistance to different types of drugs among E. coli isolates recovered from urine samples is cause for concern. In our study, E. coli resistance to TMP-SMX was 27%. Fluoroquinolones are recommended as a second-line agent for antibiotic-resistant organisms.8 However, in our study, E. coli resistance to fluoroquinolones was 60%, which is higher than the 45% reported from a Philadelphia Veterans Administration Nursing Home Care Unit.5 Because prior fluoroquinolone use is a known risk factor for fluoroquinolone-resistant E. coli infection,5 it is plausible that frequent fluoroquinolone prescriptions in these nursing homes may be contributing to the observed resistance.
Because of the increasing antibiotic resistance among isolates of E. coli, more attention has been focused on nitrofurantoin as a first-line agent for treating acute uncomplicated cystitis among young women.10 In our study, nitrofurantoin emerged as the antibiotic with the most consistent susceptibility pattern among E. coli isolates (93%), which suggests that further study of its use as the choice agent for treating UTI in a nursing home population is warranted. Those participants initially prescribed nitrofurantoin experienced the fewest changes in antibiotic therapy. However, many other Enterobacteriaceae besides E. coli are intrinsically resistant to nitrofurantoin, such that 68% of all isolates recovered from the urine samples in our study were susceptible to nitrofurantoin. In addition, nitrofurantoin is contraindicated, and cephalexin and TMP-SMX should be used with caution for patients with chronic kidney disease. In our study, only 5.9% of participants had chronic kidney disease, which suggests that most of them could have been treated with these therapies.
The main strength of our study is that we identified all isolated uropathogens from nursing home residents with clinically suspected UTI who did not require the use of an indwelling catheter. Consequently, our findings may be unique to patients who do not require the use of an indwelling catheter in the New Haven area, making it uncertain whether these results can be generalized to patients who do require the use of an indwelling catheter. The catheterization rate among screened residents in our study was 3% (28 of 942 residents), which suggest that these results can be extrapolated to the vast majority of nursing home residents.
Our study highlights the resistance of isolates (recovered from urine samples obtained from nursing home residents) to widely prescribed oral antibiotics. The resistance to fluoroquinolones among isolates of E. coli was high, and the prescription of these agents as empiric therapy for suspected UTI should be avoided. Although TMP-SMX resistance among E. coli isolates is increasing, it still remains the best empiric oral option for treatment of clinically suspected UTI. E. coli isolates maintained susceptibility to nitrofurantoin, which should be considered a preferred therapeutic agent once the organism is identified. Future directions for this research include assessing the risks and benefits of nitrofurantoin use for the treatment of UTI among nursing home residents who do not require the use of an indwelling catheter.
ACKNOWLEDGEMENTS
We are grateful to all of the nursing home staff who assisted in the conduct of our study.
Financial support. National Institute on Aging (grants T32-AG019134, R03-AG028057, and K23-AG028691); National Institutes of Health and National Institute on Aging Claude D. Pepper Older Americans Independence Center (grant P30-AG21342); Atlantic Philanthropies; Infectious Diseases Society of America and National Foundation for Infectious Diseases; John A. Hartford Foundation; Association of Specialty Professors; and National Center for Research Resources (Clinical and Translational Science Awards grant UL1 RR024139).
Footnotes
Potential conflicts of interest. All authors report no conflicts of interest relevant to this article.
REFERENCES
- 1.Nicolle LE. Urinary tract infection in long-term-care facility residents. Clin Infect Dis. 2000;31:757–761. doi: 10.1086/313996. [DOI] [PubMed] [Google Scholar]
- 2.Nicolle LE. Resistant pathogens in urinary tract infections. J Am Geriatr Soc. 2002;50(7 Suppl):S230–S235. doi: 10.1046/j.1532-5415.50.7s.3.x. [DOI] [PubMed] [Google Scholar]
- 3.Bonomo RA. Multiple antibiotic-resistant bacteria in long-term-care facilities: an emerging problem in the practice of infectious diseases. Clin Infect Dis. 2000;31:1414–1422. doi: 10.1086/317489. [DOI] [PubMed] [Google Scholar]
- 4.Viray M, Linkin D, Maslow JN, et al. Longitudinal trends in antimicrobial susceptibilities across long-term-care facilities: emergence of fluoroquinolone resistance. Infect Control Hosp Epidemiol. 2005;26:56–62. doi: 10.1086/502487. [DOI] [PubMed] [Google Scholar]
- 5.Cohen AE, Lautenbach E, Morales KH, Linkin DR. Fluoroquinolone-resistant Escherichia coli in the long-term care setting. Am J Med. 2006;119:958–963. doi: 10.1016/j.amjmed.2006.05.030. [DOI] [PubMed] [Google Scholar]
- 6.Grude N, Tveten Y, Kristiansen BE. Urinary tract infections in Norway: bacterial etiology and susceptibility. A retrospective study of clinical isolates. Clin Microbiol Infect. 2001;7:543–547. [PubMed] [Google Scholar]
- 7.Juthani-Mehta M, Quagliarello VM, Perrelli E, Towle V, Van Ness P, Tinetti M. Clinical features to identify urinary tract infection in nursing home residents: a cohort study. J Am Geriatr Soc. 2009;57:963–970. doi: 10.1111/j.1532-5415.2009.02227.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nicolle LE, Bentley D, Garibaldi R, Neuhaus E, Smith P. Antimicrobial use in long-term-care facilities. Infect Control Hosp Epidemiol. 1996;17:119–128. doi: 10.1086/647256. [DOI] [PubMed] [Google Scholar]
- 9.Warren JW, Abrutyn E, Hebel JR, Johnson JR, Schaeffer AJ, Stamm WE. Guidelines for antimicrobial treatment of uncomplicated acute bacterial cystitis and acute pyelonephritis in women. Infectious Diseases Society of America (IDSA) Clin Infect Dis. 1999;29:745–758. doi: 10.1086/520427. [DOI] [PubMed] [Google Scholar]
- 10.Gupta K, Hooton TM, Roberts PL, Stamm WE. Short-course nitrofurantoin for the treatment of acute uncomplicated cystitis in women. Arch Intern Med. 2007;167:2207–2212. doi: 10.1001/archinte.167.20.2207. [DOI] [PubMed] [Google Scholar]