Abstract
Purpose
We reviewed the epidemiological literature on the association of obesity and urinary incontinence, and summarized clinical trial data on the effect of weight loss on urinary incontinence.
Materials and Methods
We systematically searched for published community based prevalence studies with bivariate or multivariate analysis of the association of urinary incontinence and overweight/obesity in women. Case series and randomized controlled trials of the effect of surgical, behavioral and pharmacological weight loss on urinary incontinence are summarized.
Results
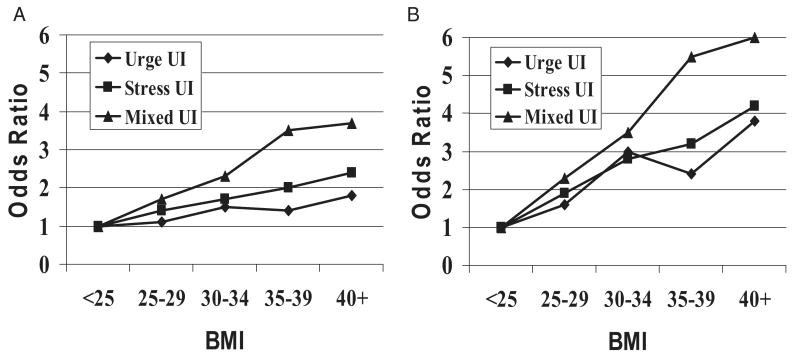
Epidemiological studies showed that obesity is a strong independent risk factor for prevalent and incident urinary incontinence. There was a clear dose-response effect of weight on urinary incontinence with each 5-unit increase in body mass index associated with about a 20% to 70% increase in the urinary incontinence risk, and the maximum effect of weight rarely exceeded an OR of greater than 4 to 5 on well controlled analyses. The odds of incident urinary incontinence during 5 to 10 years increased by approximately 30% to 60% for each 5-unit increase in body mass index. There may be a stronger association of increasing weight with prevalent and incident stress incontinence, including mixed incontinence, than with urge incontinence and overactive bladder syndrome. Weight loss studies indicated that surgical and nonsurgical weight loss led to significant improvements in urinary incontinence symptoms.
Conclusions
Epidemiological studies document overweight and obesity as important risk factors for urinary incontinence. Weight loss by surgical and more conservative approaches is effective to decrease urinary incontinence symptoms and should be strongly considered a first line treatment in this patient population.
Keywords: urinary bladder, urinary incontinence, obesity, female, epidemiology
Obesity and UI are common, costly disorders. More than 50% of American women are overweight (BMI 25 to 29.9 kg/m2) or obese (BMI 30 kg/m2 or greater) and the prevalence of obesity is increasing almost 6% per year.1 Obesity directly contributes to more than 300,000 deaths per year, accounts for expenditures of more than $100 billion per year, is associated with medical co-morbidities such as heart disease, hypertension, diabetes, cancer and depression, and adversely affects quality of life.1,2 Urinary incontinence affects almost 50% of middle-aged and older women,3–5 is associated with a profound adverse effect on quality of life5–7 and accounts for more than $30 billion in annual direct costs in the United States.8
Methods
We systematically searched for published community based prevalence studies with bivariate or multivariate analysis of the association of UI and overweight/obesity in women. Prospective case series, longitudinal studies and randomized, controlled trials of the effect of surgical, behavioral and pharmacological weight loss on UI are summarized. Methods were similar to those described completely in a recent systematic literature review.9 Systematic searches were done using MEDLINE® (1966 and thereafter), the Cochrane Central Register of Controlled Trials, the Cochrane Database of Systematic Reviews and the Database of Abstracts of Reviews of Effects. Searches were updated, thereby including evidence published and included in the databases up to June 2009.
Results
Epidemiological Evidence for Obesity as UI Risk Factor
Cross-sectional epidemiological studies showed that obesity is a strong risk factor for urinary incontinence. A recent systematic literature review including population based UI prevalence studies with bivariate or multivariate analysis examined the association between UI and overweight/obesity in women.9 While the definition of UI varies from ever to occurring within a defined period, data from a large number of studies indicated that UI in women is associated with higher BMI and weight.10–26 Most series were similar to the Norwegian Epidemiology of Incontinence in the County of Nord-Trøndelag study of almost 28,000 women, in which a clear dose-response effect of weight on UI prevalence was found (see figure).9,12 The maximum effect of weight on incontinence rarely exceeded an OR of 4 to 5 on well controlled analyses. In most studies a stronger association was observed between increasing weight and stress predominant incontinence, including mixed incontinence, than for urge predominant incontinence and overactive bladder syndrome.11,12,19,24,28 Each 5-unit increase in BMI was associated with about a 20% to 70% increase in the risk of daily incontinence.10,11,13,14,19,22,23 In 1 study obesity had the largest attributable risk for daily incontinence compared to other risk factors.10 In obese women with a BMI of greater than 40 kg/m2 who were planning weight reduction surgery the prevalence of incontinence was 60% to 70%28–30 with a prevalence of 28% for pure stress type, 4% for pure urge type and 32% for mixed type.28
BMI and UI by type, adjusted for age, parity, coughing and dyspnea.9,12 A, any UI. B, severe UI.
Obesity and incident UI
In population based, longitudinal cohort studies overweight and obesity were associated with new onset UI or incident UI, providing documentation for a temporal relationship between a possible cause and an outcome. In 5 to 10 years of followup the odds of incident UI increased by approximately 7% to 12% for each 1 kg/m2 unit increase in BMI.31,32 This association was strongest for stress and mixed incontinence, and somewhat weaker for urge incontinence and overactive bladder syndrome. While UI remission occurred, this was usually not analyzed in UI incidence studies.
In a study of 6,424 women with overweight and obesity in the United Kingdom multivariate analysis revealed significantly increased risks associated with BMI for the onset of stress incontinence (OR 1.4 and 2.3) and overactive bladder (OR 1.3 and 1.2, respectively).33,34 Only the stress incontinence trend attained statistical significance. In a 5-year annual followup of 3,301 women 42 to 52 years old the incidence of incontinence was 56% for an annual 11% incidence per year.31 Multivariate analysis showed that BMI per unit increase was associated with any (OR 1.05), frequent (OR 1.12), stress (OR 1.06), urge (OR 1.03) and mixed (OR 1.09) UI (all p <0.05). In the American Nurses' Health Study II in 35,754 women increasingly higher BMI was associated with higher odds of incident UI.32 When comparing women with a BMI of 35 kg/m2 or greater to lean women with a BMI of 21 to 22.9 kg/m2, the OR was 2.11 (95% CI 1.84–2.42) for at least monthly UI, 3.85 (95% CI 3.05–4.85) for at least weekly UI and 5.52 (95% CI 3.72–8.18) for severe UI.
The odds of incident UI also increased with increasing adult weight gain.32 Compared with women who maintained their weight within 2 kg, the OR for at least weekly incontinence was 1.44 (95% CI 1.05–1.97) in women who gained 5.1 to 10 kg and 4.04 (95% CI 2.93–5.56) in women who gained more than 30 kg since early adulthood (p for trend <0.001). Compared to women with a BMI of 21 to 22.9 kg/m2 women with a BMI of 35 kg/m2 or greater had an OR of 3.42 (95% CI 2.48–4.72) for stress incontinence, 6.10 (95% CI 3.11–11.98) for urge incontinence and 5.60 (95% CI 3.17–9.88) for mixed incontinence. In a longitudinal study of 1,201 British women high BMI at ages 20 to 36 years was associated with stress UI and severe UI in middle age.26 Longstanding overweight was more important than becoming overweight/obese after age 43 years (OR 1.85, 95% CI 0.97–3.51).
Body fat distribution and UI
Little is known about the association of UI and fat distribution, for example abdominal adiposity estimated by waist circumference or the waist-to-hip ratio. On multivariable analysis including BMI an increasing waist-to-hip ratio was an independent risk factor for stress incontinence (OR 1.18 per 0.1 unit) but not for urge and mixed incontinence.11 In a cohort of Korean women compared with women in the lowest quartile of waist circumference the OR for stress incontinence increased significantly in a dose dependent relationship in the next quartiles after adjusting for BMI (OR 1.79, 3.50 and 6.07, respectively).18 In women in the Nurses' Health Study there were highly significant trends toward an increasing risk of incontinence with increasing BMI and waist circumference.35 When BMI and waist circumference were included in models simultaneously, BMI was associated with urge and mixed incontinence but not with stress incontinence. Waist circumference was associated only with stress incontinence. In the Norwegian Epidemiology of Incontinence in the County of Nord-Trøndelag study of 6,876 incontinent Norwegian women multivariate analysis adjusting for age, parity and BMI showed a statistically significant association for the waist-to-hip ratio, and any and mixed incontinence (each OR 1.1).36 In the American Boston Area Community Health survey each 10 cm increase in waist circumference in women was independently associated with a higher prevalence of weekly UI (OR 1.15, 95% CI 1.01–1.31).37 In Hispanic women the OR was 1.43 (95% CI 1.14–1.78).
Clinical Trials of Weight Loss to Treat UI
Since obesity is a potentially modifiable risk factor for urinary incontinence, weight reduction may be an effective treatment option. A beneficial effect of weight loss on incontinence prevalence and frequency was found in surgical and behavioral weight reduction interventions (see table).9
Effects of weight loss on UI
| References | No. Pts | Design | BMI or Wt Change | UI Prevalence or Episode Change (p value) | Other Outcomes (p value) |
|---|---|---|---|---|---|
| Surgical wt loss case + cohort studies: | |||||
| Deitel et al29 | 138 | Unknown | Wt 124–79 kg | 61%–12% Stress UI prevalence (<0.001) | Improved infertility + menstrual irregularities |
| Bump et al36 | 13 | 12-mo Followup | BMI 49–33 kg/m2, wt 132–88 kg | 92%–23% UI prevalence (0.004) | Differences in urodynamic parameters + urethral mobility |
| Sugerman et al39 | 15 | 12-mo Followup | BMI 52–33 kg/m2, wt 140–87 kg | 47%–0% IU prevalence (<0.001) | Significantly changed sagittal abdominal diameter 32–20 cm (0.0001) + bladder pressure 17–10 cm H2O (0.001) |
| Frigg et al3 | 233 | 44-mo Followup | 54% Excess wt loss at 4-yr followup | 26%–11% Stress UI prevalence at 2-yr followup | Improved other medical comorbidities |
| Burgio et al28 | 101 | 12-mo Followup | BMI 49–30 kg/m2 | 67%–37% (<0.001) | Decreased fecal incontinence prevalence 19%–9% (0.018) + UI decrease significantly associated with BMI |
| Nonsurgical wt loss cohort studies + randomized trials: | |||||
| Subak et al40 | 10 | Low calorie liquid diet wt loss program, 3-mo followup | BMI 38–33 kg/m2, wt −14 kg (<0.03) | 13–8 Episodes/wk after wt loss (<0.07) | Of 10 women 6 with 5% or greater body wt loss had greater than 50% UI frequency decrease (<0.03) |
| Subak et al41 | 40 | Randomized to groups 1—low calorie liquid diet in 20 pts + 2—20 controls, 3-mo intervention, 9-mo followup | Wt change at 3 mos −16 kg in group 1 vs none in group 2 (<0.0001) | No. wkly UI episodes at 3 mos decreased 60% in group 1 vs 15% in group 2 (<0.0005) | No. stress (0.003) + urge (0.03) UI episodes decreased in group 1 vs 2, group 2 had intervention after 3 mos with 71% wkly UI decrease after wt loss, + Incontinence Impact Questionnaire + Urogenital Distress Inventory scores significantly improved after wt loss |
| Brown et al42 | 1,957 | Randomized to groups 1— lifestyle intervention* in 660 pts, 2—metformin in 636 + 3—placebo in 661, mean 2.9-yr followup | Wt change −3.4, −1.5 + 0.5 kg in groups 1–3, respectively (<0.001) | Wkly UI prevalence 38%, 48% + 46% in groups 1–3, respectively (0.001) | Wkly stress UI 31% vs 40% + 37% in groups 1 vs 2 + 3 (0.006), + urge UI prevalence 24%, 29% + 26% in groups 1–3, respectively (not different, 0.12) |
| Subak et al43 | 338 | Randomized to group 1—6-mo lifestyle intervention* in 226 pts + 2—structured education program in 112, 6-mo followup | Wt change −7.8 in 8% of pts + −1.5 in 1.6% in groups 1 + 2, respectively (<0.001) | Wkly total/stress UI decreased 47%/58% + 28%/33% in groups 1 + 2, respectively (0.01/<0.02) | More pts in group 1 vs 2 had 70% or greater decrease in all (<0.001), stress (0.009) + urge (0.04) UI episode frequency, + greater perceived improvement in UI frequency, lower urine vol lost, UI as less problem + higher satisfaction with UI change (each 0.001) |
Diet, exercise and behavior modification program.
Surgical weight loss
In observational studies severely obese women (greater than 45 kg above ideal weight) with incontinence who had dramatic weight loss after bariatric surgery (45 to 50 kg) had significant improvement in UI.29,38,39 In a study of 138 women the prevalence of stress UI decreased from 61% at baseline to 12% after weight stabilization in 2 to 5 years (p <0.001).29 In another study of 101 women the prevalence of any incontinence decreased from 67% at baseline to 37% at 12 months (p <0.001).28 Statistically significant changes were also noted in urodynamic parameters, incontinence episode frequency and the need for absorptive pads.38
Behavioral weight loss
Decreased UI episode frequency was also observed after enrollment in behavioral weight loss programs, including low calorie liquid diet and intensive lifestyle diet and exercise interventions.40–43 In a small prospective cohort study of overweight and obese incontinent women enrolled in low calorie liquid diet weight reduction programs 6 of 6 achieving a weight loss of 5% or greater had at least a 50% decrease in UI frequency compared to 1 of 4 with less than a 5% weight loss (p = 0.03).40 A randomized trial of a 3-month low calorie liquid diet program compared to no intervention in 42 women showed greater weight loss in those randomized to diet intervention compared to controls (14 vs 0 kg) and a greater decrease in weekly incontinence episode frequency from baseline (60% vs 15%, p <0.001) with decreases in stress and urge incontinence episodes (p = 0.003 and 0.03, respectively).41 Weight and UI decreases were maintained for 6 months.
A total of 1,957 overweight prediabetic women enrolled in the Diabetes Prevention Program were randomized to intensive lifestyle therapy, metformin or placebo with standard lifestyle advice.42 At 2.9 years of followup the prevalence of total weekly incontinence was lower in women in the intensive lifestyle group than in those randomized to metformin or placebo (38% vs 48% and 46%, respectively, p <0.001). This difference was most apparent in women with stress incontinence (weekly stress incontinence 31% in the intensive lifestyle group vs 40% for metformin vs 37% for placebo, p = 0.006). The weight change accounted for 35% of the incontinence effect with the change in exercise and incident diabetes each explaining only 5%.
The first large randomized trial of the effect of weight reduction on incontinence included 338 overweight and obese women with at least 10 UI episodes per week randomized to an intensive 6-month weight loss program of diet, exercise and behavior modification (226) or a structured education program (112).43 Each group received an instructional booklet describing standard behavioral therapy for incontinence. After 6 months women in the intervention group achieved a mean weight loss of 8% compared with 2% in controls (p <0.0001). The mean number of weekly incontinence episodes decreased by 47% in the intervention group compared with 28% in controls (p = 0.01). Compared with controls the intervention group had a greater decrease in stress incontinence episode frequency but not in urge incontinence episodes (p = 0.02 and 0.14, respectively). Women in the weight loss group perceived greater improvement in the frequency of UI, lower volume of urine lost, UI as less of a problem and higher satisfaction with the change in incontinence at 6 months compared to women in the control group (p <0.001).
Mechanism of Obesity-Incontinence Association
While to our knowledge the mechanism of the obesity-UI association is unknown, it is theorized that excess body weight increases abdominal pressure, which in turn increases bladder pressure and urethral mobility, leading to stress UI and also exacerbating detrusor instability and overactive bladder.38,41 Like pregnancy, obesity may cause chronic strain, stretching and weakening the muscles, nerves and other pelvic floor structures.
A strong association was noted between BMI, and intra-abdominal and intravesical pressure (Pearson coefficient correlation 0.76 and 0.71, respectively).44 Also, weight loss is associated with changes in urodynamic measures, leading to decreased incontinence. After large, surgically induced weight loss statistically significant changes were reported in urodynamic measures, including decreased intravesical pressure, greater bladder pressure increases with coughing, bladder-to-urethra pressure transmission with cough and urethral axial mobility.38,39 With a moderate loss of 13% of baseline weight significant correlations between weight change and decreased initial intravesical pressure (Spearman r = 0.52, p = 0.01), decreased intravesical pressure at maximum capacity (r = 0.62, p = 0.001) and increased Valsalva leak point pressure (r = 0.57, p = 0.03) were noted.41
Conclusions
Epidemiological studies reveal that obesity is a strong, independent risk factor for prevalent and incident UI. There is a clear dose-response effect of weight on UI with each 5-unit increase in BMI associated with about a 20% to 70% increase in the risk of UI. The maximum effect of weight rarely exceeds an OR of greater than 4 to 5 on well controlled analyses. The odds of incident UI during 5 to 10 years increase by approximately 30% to 60% for each 5-unit increase in BMI. There may be a stronger association between increasing weight, and prevalent and incident stress incontinence, including mixed incontinence, than for urge incontinence and overactive bladder syndrome. However, to our knowledge the mechanism of the association of obesity and incontinence is unknown. Additional neurophysiological and urodynamic studies are needed to better define the obesity-UI relationship.
Weight loss studies indicate that surgical and nonsurgical weight loss lead to significant improvements in UI symptoms. Data support that a weight loss of 5% to 10% has efficacy similar to that of other nonsurgical UI treatments and should be strongly considered first line therapy for incontinence. Also, moderate weight reduction is associated with extensive health improvements.
Future Research in Obesity and Lower Urinary Tract Function
Current research shows that obesity is a strong risk factor for UI and weight loss is an effective treatment for UI. Based on review and analysis of the available literature, we propose certain areas of highest priority for future research. 1) In terms of UI prevention, can healthier lifestyle choices such as weight control and physical activity prevent the onset or worsening of UI and LUTS in women? 2) In terms of clinical trials, is weight loss intervention generalizable? What is the effectiveness of weight loss for UI in a general population of overweight and obese women with UI? 3) In terms of the mechanism, what are the mechanisms of how weight affects UI and weight loss improves UI? What is the role of adipocytokines, inflammation or other biologically active substances? 4) For ancillary studies, UI could be included in prospective cohort studies and clinical trials of weight loss and behavioral/lifestyle interventions, and cost-effectiveness could be included in clinical trials of weight loss. 5) For epidemiological research, the independence and synergy of risk factors for prevalent and incident UI could be evaluated, including BMI, body habitus, diabetes and cardiovascular risk factors. 6) For comparative effectiveness research, what is the comparative effectiveness of standard surgical, pharmacological and behavioral UI treatments in overweight and obese women? 7) In terms of translation to the community, does the dual diagnosis of obesity and UI create a teachable moment to motivate weight loss and improve long-term weight maintenance?
Abbreviations and Acronyms
- BMI
body mass index
- UI
urinary incontinence
References
- 1.Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289:76. doi: 10.1001/jama.289.1.76. [DOI] [PubMed] [Google Scholar]
- 2.Allison DB, Fontaine KR, Manson JE, et al. Annual deaths attributable to obesity in the United States. JAMA. 1999;282:1530. doi: 10.1001/jama.282.16.1530. [DOI] [PubMed] [Google Scholar]
- 3.Frigg A, Peterli R, Peters T, et al. Reduction in co-morbidities 4 years after laparoscopic adjustable gastric banding. Obes Surg. 2004;14:216. doi: 10.1381/096089204322857591. [DOI] [PubMed] [Google Scholar]
- 4.Thom DH, van den Eeden SK, Ragins AI, et al. Differences in prevalence of urinary incontinence by race/ethnicity. J Urol. 2006;175:259. doi: 10.1016/S0022-5347(05)00039-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wetle T, Scherr P, Branch LG, et al. Difficulty with holding urine among older persons in a geographically defined community: prevalence and correlates. J Am Geriatr Soc. 1995;43:349. doi: 10.1111/j.1532-5415.1995.tb05806.x. [DOI] [PubMed] [Google Scholar]
- 6.Grimby A, Milsom I, Molander U, et al. The influence of urinary incontinence on the quality of life of elderly women. Age Ageing. 1993;22:82. doi: 10.1093/ageing/22.2.82. [DOI] [PubMed] [Google Scholar]
- 7.Hunskaar S, Vinsnes A. The quality of life in women with urinary incontinence as measured by the sickness impact profile. J Am Geriatr Soc. 1991;39:378. doi: 10.1111/j.1532-5415.1991.tb02903.x. [DOI] [PubMed] [Google Scholar]
- 8.Wilson L, Brown JS, Park GE, et al. Annual costs of urinary incontinence. Obstet Gynecol. 2001;98:398. doi: 10.1016/s0029-7844(01)01464-8. [DOI] [PubMed] [Google Scholar]
- 9.Hunskaar S. A systematic review of overweight and obesity as risk factors and targets for clinical intervention for urinary incontinence in women. Neurourol Urodyn. 2008;27:749. doi: 10.1002/nau.20635. [DOI] [PubMed] [Google Scholar]
- 10.Brown J, Seeley D, Fong J, et al. Urinary incontinence in older women: who is at risk? Study of Osteoporotic Fractures Research Group. Obstet Gynecol. 1996;87:715. doi: 10.1016/0029-7844(96)00013-0. [DOI] [PubMed] [Google Scholar]
- 11.Brown JS, Grady D, Ouslander JG, et al. Prevalence of urinary incontinence and associated risk factors in postmenopausal women. Heart and Estrogen/Progestin Replacement Study (HERS) Research Group. Obstet Gynecol. 1999;94:66. doi: 10.1016/s0029-7844(99)00263-x. [DOI] [PubMed] [Google Scholar]
- 12.Hannestad YS, Rortveit G, Daltveit AK, et al. Are smoking and other lifestyle factors associated with female urinary incontinence? The Norwegian EPINCONT Study. BJOG. 2003;110:247. [PubMed] [Google Scholar]
- 13.Mommsen S, Foldspang A. Body mass index and adult female urinary incontinence. World J Urol. 1994;12:319. doi: 10.1007/BF00184112. [DOI] [PubMed] [Google Scholar]
- 14.Sampselle CM, Harlow SD, Skurnick J, et al. Urinary incontinence predictors and life impact in ethnically diverse perimenopausal women. Obstet Gynecol. 2002;100:1230. doi: 10.1016/s0029-7844(02)02241-x. [DOI] [PubMed] [Google Scholar]
- 15.Thom DH, Brown JS. Reproductive and hormonal risk factors for urinary incontinence in later life: a review of the clinical and epidemiologic literature. J Am Geriatr Soc. 1998;46:1411. doi: 10.1111/j.1532-5415.1998.tb06009.x. [DOI] [PubMed] [Google Scholar]
- 16.Yarnell J, Voyle G, Sweetham P, et al. Factors associated with urinary incontinence in women. J Epidemiol Community Health. 1982;36:58. doi: 10.1136/jech.36.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Danforth KN, Townsend MK, Lifford K, et al. Risk factors for urinary incontinence among middle-aged women. Am J Obstet Gynecol. 2006;194:339. doi: 10.1016/j.ajog.2005.07.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Han MO, Lee NY, Park HS. Abdominal obesity is associated with stress urinary incontinence in Korean women. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17:35. doi: 10.1007/s00192-005-1356-8. [DOI] [PubMed] [Google Scholar]
- 19.Jackson RA, Vittinghoff E, Kanaya AM, et al. Urinary incontinence in elderly women: findings from the Health, Aging, and Body Composition Study. Obstet Gynecol. 2004;104:301. doi: 10.1097/01.AOG.0000133482.20685.d1. [DOI] [PubMed] [Google Scholar]
- 20.Melville JL, Katon W, Delaney K, et al. Urinary incontinence in us women: a population-based study. Arch Intern Med. 2005;165:537. doi: 10.1001/archinte.165.5.537. [DOI] [PubMed] [Google Scholar]
- 21.Burgio KL, Matthews KA, Engel BT. Prevalence, incidence and correlates of urinary incontinence in healthy, middle-aged women. J Urol. 1991;146:1255. doi: 10.1016/s0022-5347(17)38063-1. [DOI] [PubMed] [Google Scholar]
- 22.Kuh D, Cardozo L, Hardy R. Urinary incontinence in middle aged women: childhood enuresis and other lifetime risk factors in a British prospective cohort. J Epidemiol Community Health. 1999;53:453. doi: 10.1136/jech.53.8.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nygaard I, Turvey C, Burns TL, et al. Urinary incontinence and depression in middle-aged United States women. Obstet Gynecol. 2003;101:149. doi: 10.1016/s0029-7844(02)02519-x. [DOI] [PubMed] [Google Scholar]
- 24.Teleman PM, Lidfeldt J, Nerbrand C, et al. Overactive bladder: prevalence, risk factors and relation to stress incontinence in middle-aged women. BJOG. 2004;111:600. doi: 10.1111/j.1471-0528.2004.00137.x. [DOI] [PubMed] [Google Scholar]
- 25.Hall SA, Cinar A, Link CL, et al. Do urological symptoms cluster among women? Results from the Boston Area Community Health Survey. BJU Int. 2008;101:1257. doi: 10.1111/j.1464-410X.2008.07557.x. [DOI] [PubMed] [Google Scholar]
- 26.Mishra GD, Hardy R, Cardozo L, et al. Body weight through adult life and risk of urinary incontinence in middle-aged women: results from a British prospective cohort. Int J Obes (Lond) 2008;32:1415. doi: 10.1038/ijo.2008.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lawrence JM, Lukacz ES, Liu IL, et al. Pelvic floor disorders, diabetes, and obesity in women: findings from the Kaiser Permanente Continence Associated Risk Epidemiology Study. Diabetes Care. 2007;30:2536. doi: 10.2337/dc07-0262. [DOI] [PubMed] [Google Scholar]
- 28.Burgio KL, Richter HE, Clements RH, et al. Changes in urinary and fecal incontinence symptoms with weight loss surgery in morbidly obese women. Obstet Gynecol. 2007;110:1034. doi: 10.1097/01.AOG.0000285483.22898.9c. [DOI] [PubMed] [Google Scholar]
- 29.Deitel M, Stone E, Kassam HA, et al. Gynecologic-obstetric changes after loss of massive excess weight following bariatric surgery. J Am Coll Nutr. 1988;7:147. doi: 10.1080/07315724.1988.10720232. [DOI] [PubMed] [Google Scholar]
- 30.Richter HE, Burgio KL, Clements RH, et al. Urinary and anal incontinence in morbidly obese women considering weight loss surgery. Obstet Gynecol. 2005;106:1272. doi: 10.1097/01.AOG.0000187299.75024.c4. [DOI] [PubMed] [Google Scholar]
- 31.Waetjen LE, Liao S, Johnson WO, et al. Factors associated with prevalent and incident urinary incontinence in a cohort of midlife women: a longitudinal analysis of data: study of women's health across the nation. Am J Epidemiol. 2007;165:309. doi: 10.1093/aje/kwk018. [DOI] [PubMed] [Google Scholar]
- 32.Townsend MK, Danforth KN, Rosner B, et al. Body mass index, weight gain, and incident urinary incontinence in middle-aged women. Obstet Gynecol. 2007;110:346. doi: 10.1097/01.AOG.0000270121.15510.57. [DOI] [PubMed] [Google Scholar]
- 33.Dallosso HM, McGrother CW, Matthews RJ, et al. The association of diet and other lifestyle factors with overactive bladder and stress incontinence: a longitudinal study in women. BJU Int. 2003;92:69. doi: 10.1046/j.1464-410x.2003.04271.x. [DOI] [PubMed] [Google Scholar]
- 34.McGrother CW, Donaldson MM, Hayward T, et al. Urinary storage symptoms and comorbidities: a prospective population cohort study in middle-aged and older women. Age Ageing. 2006;35:16. doi: 10.1093/ageing/afi205. [DOI] [PubMed] [Google Scholar]
- 35.Townsend MK, Curhan GC, Resnick NM, et al. BMI, waist circumference, and incident urinary incontinence in older women. Obesity (Silver Spring) 2008;16:881. doi: 10.1038/oby.2008.14. [DOI] [PubMed] [Google Scholar]
- 36.Hannestad YS, Huskaar S. Waist-hip ratio associated with urinary incontinence in women. Presented at annual meeting of International Continence Society; Montreal, Quebec, Canada. August 31, 2005; abstract 168. [Google Scholar]
- 37.Tennstedt SL, Link CL, Steers WD, et al. Prevalence of and risk factors for urine leakage in a racially and ethnically diverse population of adults: the Boston Area Community Health (BACH) Survey. Am J Epidemiol. 2008;167:390. doi: 10.1093/aje/kwm356. [DOI] [PubMed] [Google Scholar]
- 38.Bump R, Sugerman H, Fantl J, et al. Obesity and lower urinary tract function in women: effect of surgically induced weight loss. Am J Obstet Gynecol. 1992;166:392. doi: 10.1016/s0002-9378(11)91418-5. [DOI] [PubMed] [Google Scholar]
- 39.Sugerman H, Windsor A, Bessos M, et al. Effects of surgically induced weight loss on urinary bladder pressure, sagittal abdominal diameter and obesity co-morbidity. Int J Obes Relat Metab Disord. 1998;22:230. doi: 10.1038/sj.ijo.0800574. [DOI] [PubMed] [Google Scholar]
- 40.Subak LL, Johnson C, Whitcomb E, et al. Does weight loss improve incontinence in moderately obese women? Int Urogynecol J Pelvic Floor Dysfunct. 2002;13:40. doi: 10.1007/s001920200008. [DOI] [PubMed] [Google Scholar]
- 41.Subak LL, Whitcomb E, Shen H, et al. Weight loss: a novel and effective treatment for urinary incontinence. J Urol. 2005;174:190. doi: 10.1097/01.ju.0000162056.30326.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brown JS, Wing R, Barrett-Connor E, et al. Lifestyle intervention is associated with lower prevalence of urinary incontinence: the Diabetes Prevention Program. Diabetes Care. 2006;29:385. doi: 10.2337/diacare.29.02.06.dc05-1781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Subak LL, Wing R, West DS, et al. Weight loss to treat urinary incontinence in overweight and obese women. N Engl J Med. 2009;360:481. doi: 10.1056/NEJMoa0806375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Noblett KL, Jensen JK, Ostergard DR. The relationship of body mass index to intra-abdominal pressure as measured by multichannel cystometry. Int Urogynecol J Pelvic Floor Dysfunct. 1997;8:323. doi: 10.1007/BF02765589. [DOI] [PubMed] [Google Scholar]