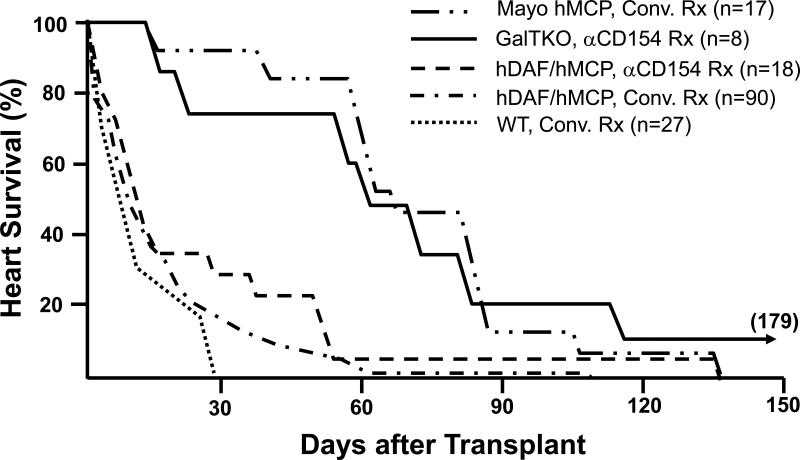
Figure 3. Effect of genetic modifications and treatment regimens on survival of pig hearts in baboons.
Survival in immunosuppressed baboons of heterotopic hearts from wild-type (WT) pigs (n=26), pigs transgenic for human decay-accelerating factor (hDAF), human membrane cofactor protein (hMCP), and/or human CD59 (n=125), and GalT-KO pigs (n=8). In conjunction with neutralization of anti-Gal antibodies, conventional or anti-CD154-based immunosuppression (using a monoclonal antibody that selectively blocks the CD154-CD40 “costimulation” pathway important to T- and B-cell activation) was associated with median survival of hDAF or hMCP transgenic hearts approaching one month in some series, and for over 2 months in the Mayo Clinic's recent experience. Infectious or treatment-associated complications caused the death of over 50% of recipients treated with conventional immunosuppression, but were unusual with anti-CD154-based treatment. Lymphocyte and antibody responses against pig antigens were generally undetectable during either anti-CD154 or intensive conventional therapy. Grafts failed with DXR histology in association with both conventional and CD154-based treatment regimens.
Eight GalT-KO hearts in baboons treated with anti-CD154 antibody, mycophenlate mofetil, and perioperative T-cell depletion, did not exhibit early graft failure (<3 days), and median survival exceeded two months. Typical DXR was rare in GalT-KO hearts, but thrombotic microangiopathy, which was also observed in long-surviving hDAF and hMCP hearts, was prominent in association with GalT-KO cardiac xenograft failure.
Data are abstracted from all peer-reviewed pig-to-baboon heart transplant studies published since 1988, aggregating data from studies that used similar therapeutic approaches. Pig phenotype (GalT-KO, hDAF, hMCP, or WT) and treatment regimen (anti-CD154-based or conventional (Conv.) treatment (Rx)) are indicated. Similar results were achieved with conventional immunosuppression in over 65 cynomolgus recipients of hDAF hearts.