Abstract
Developing and disseminating a preventive HIV vaccine is a primary scientific and public health objective. However, little is known about HIV vaccine acceptability in the high prevalence setting of South Africa—where young adults are likely to be targeted in early dissemination efforts. In 2007, we conducted six focus groups (n=42) with South Africans aged 18-24 years old. We used a deductive framework approach to identify key motivators and barriers to future HIV vaccine uptake. Participants identified HIV testing, HIV stigma, mistrust of the health care system, and concerns about sexual disinhibition as barriers to vaccine uptake. For women, family members and friends were strong motivators for vaccine uptake, while men were more likely to see vaccines as an opportunity to stop using HIV prevention strategies such as condoms and partner reductions. Implications of these findings for developing HIV vaccine dissemination strategies and policy in South Africa are discussed.
Keywords: HIV vaccines, South Africa, youth, barriers, qualitative research
INTRODUCTION
South Africa carries one of the highest burdens of HIV globally. The overall HIV prevalence rate for South African adults aged 15-49 is 18.8% and young women aged 25-29 have the highest rates of infection in the country (Republic of South Africa: Department of Health, 2007; UNAIDS, 2006). Effective interventions to reduce the alarming rates of new HIV-infections among young South Africans are urgently needed. This includes directly engaging communities and youth in the process of informing and developing appropriate and acceptable HIV prevention strategies, including future HIV vaccines. Despite continued scientific setbacks, many researchers, policy experts, and international institutions believe that a safe, effective, and accessible preventive HIV vaccine represents the best long-term strategy for controlling the HIV/AIDS pandemic (International AIDS Vaccine Initiative (IAVI) & The Futures Group, 2005).
Research specific to post-trial HIV vaccine acceptability among high-risk populations around the world is needed. Studies from South Africa suggest a wide variation of willingness to participate in HIV vaccine trials, ranging from 23%-79% (Jaspan et al., 2006; Smit et al., 2006). However, reasons for participating in vaccine clinical trials may be very different from the factors influencing uptake of an approved HIV vaccine when it becomes available. For example, altruism and desire to contribute to HIV research, commonly described as motivations for vaccine trial participation (Mills et al., 2004; Newman, Duan, Roberts et al., 2006), are unlikely to play a significant role in decisions about uptake of an approved HIV vaccine. Additionally, participants who volunteer for clinical trials are not representative of the wider population that will be targeted with post-trial HIV vaccine dissemination efforts.
Considerably less is known about future HIV vaccine acceptability, and the few studies that exist have been conducted in low prevalence settings of the US and Europe (Newman, Duan, Roberts et al., 2006; Newman, Seiden, Roberts, Kakinami, & Duan, 2007). The stigma of HIV/AIDS and mistrust of the health system and government have been described as barriers to future HIV vaccine uptake in US and Europe, and we hypothesized they would be formidible barriers to uptake in our study of South African youth. HIV/AIDS stigma has been reported as a barrier to HIV testing (Daftary, Padayatchi, & Padilla, 2007; Macphail, Pettifor, Coates, & Rees, 2006) as well as accessing and adhering to HIV treatment in South Africa and many other countries around the world (Ncama et al., 2008; Weiser S, 2003).
Stigma may be further intensified by mistrust of health systems, science, and the government. Mistrust of health systems and the reliability of HIV testing has been described in Uganda and China (Dahl, Mellhammar, Bajunirwe, & Bjorkman, 2008; Wang et al., 2008), and mistrust of the government and scientist in the context of failed large scale international trials have influenced willingness to participate in trials of HIV vaccines and other biomedcial prevention technologies (Bateman, 2005; Excler et al., 2008). Therefore, it is vital to conduct formative research in Africa to ensure that future HIV vaccine availability will be translated into effective dissemination strategies as well as clinical and public health benefits (Esparza et al., 2002; SAAVI (South African AIDS Vaccine Initiative)).
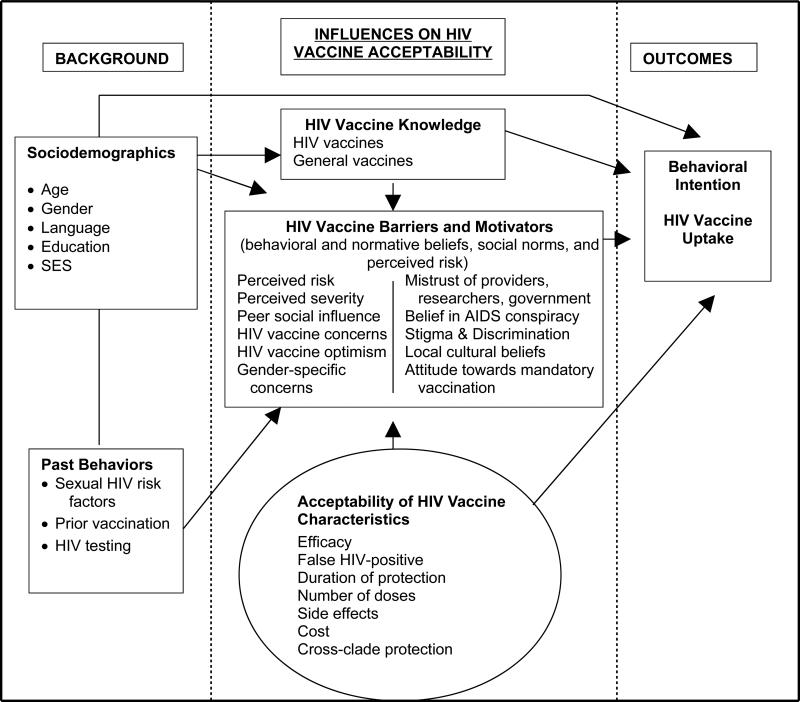
In the present study, we explored future HIV vaccine acceptability among inner-city South African youth, a high prevalence population likely to be targeted in early dissemination efforts. The conceptual model (See Figure 1) for the present study is based on value-expectancy theories and social marketing. The Theory of Reasoned Action (TRA) (Fishbein & Azjen, 1975), the Theory of Planned Behavior (TPB) (Ajzen, 1985), and the Health Belief Model (HBM) (Becker & Joseph, 1988), are well-supported models that form the theoretical underpinnings of social marketing. We employ components of each of these theories, i.e., vaccine attitudes (TRA &TPB), normative vaccine beliefs (TRA &TPB), and perceived risk and severity of HIV (HBM), in order to systematically assess determinants of HIV vaccine uptake. The Theory of Reasoned Action has been used widely to assess determinants of intentions for hypothetical behavior, such as future condom use (Morrison, Gillmore, Baker, & et al., 1995), as well as uptake of other vaccines (Schutten, de Wit, & van Steenbergen, 2002), and is similarly applicable to vaccine uptake after HIV vaccines become available.
Figure 1.
Conceptual Model for Future HIV Vaccine Acceptability
METHODS
Sampling
We utilized a venue-based sampling strategy, as South African public sector clinics are likely to represent the front lines of dissemination efforts once an HIV vaccine becomes available. Our goal was to identify key barriers and motivators to future HIV vaccine uptake among a population that interfaces with the health system and would be likely to be offered a vaccine if it were available. The clinic serves a high-risk inner-city population characterized by poverty, high levels of mobility, and large numbers of migrants from surrounding African countries, particularly Zimbabwe. We purposively sampled young adults aged 18-24, as this is the age group in South Africa when HIV incidence begins to sharply climb; thus young South Africans would ideally be targeted in early dissemination efforts for a preventive HIV vaccine (Johnson, Bekker, & Dorrington, 2007). Additionally, as the clinic services include STI screening and treatment, TB services, reproductive health, and HIV counseling and testing, our sampling frame includes individuals who engage in HIV risk behaviors and would benefit from an HIV vaccine.
Participants
In early 2007, in collaboration with a local community clinic, we conducted two focus groups with young men (n=7; n=10) and four with young women (n=6; n=6; n=6; n=7) seeking health care at a public sector clinic in Johannesburg, South Africa. Participants were recruited by fliers posted at the clinic and clinic staff who referred interested participants to the study staff. Inclusion criteria for the study were: 1) aged 18-24 years; 2) ability to speak in one of two African languages commonly spoken at the clinic; and 3) ability to provide informed consent. Participants were compensated ZAR30.00 (approximately 6 US dollars at the time of data collection) for their participation in the study. The University of the Witwatersrand Human Research Ethics Committee and the Institutional Review Board of the University of California, Los Angeles approved the study.
Data Collection
We chose focus groups to explore future HIV vaccine acceptability, as this method facilitates in depth discussion of individual perspectives within the context of a larger group, which in turn may simulate peer group dynamics that influence decision-making outside of the study setting (Kreuger, 2000). Focus group data was collected using a semi-structured discussion guide (Table 1) that addressed key domains of the conceptual model, including: vaccine knowledge, behavioral intentions to accept HIV vaccination, and barriers and motivators to uptake of a future HIV vaccine (probing for attitudes, subjective norms, perceived control, and perceived HIV risk). Participants were asked to discuss both their own opinions as well as their perceptions of the opinions and attitudes of their peers. The fact that no effective HIV vaccine currently exists, and no vaccine would be given as part of the study was stated in the informed consent document, as well as at the beginning and at the conclusion of each focus group discussion.
Table 1.
Focus Group Discussion Guide
| Focus Group Discussion Questions |
|---|
| KNOWLEDGE OF VACCINES |
| What is a vaccine? |
| What vaccines have you heard about or are you familiar with? |
| What do you know about vaccines or about how they work? |
| KNOWLEDGE OF HIV VACCINES |
| What have you heard about vaccines for HIV/AIDS? |
| BEHAVIORAL INTENTIONS |
| Would you or your close friends be willing to be vaccinated against HIV/AIDS? Why? |
| MOTIVATORS: ATTITUDES, SUBJECTIVE NORM, PERCIEVED CONTROL / RISK |
| What would be the reasons you or your close friends would want to be vaccinated against HIV/AIDS? |
| BARRIERS: ATTITUDES, SUBJECTIVE NORMS, PERCIEVED CONTROL / RISK |
| What are possible concerns or barriers to you or your friends’ taking an HIV/AIDS vaccine? |
| VACCINE CHARACTERISTICS |
| Are there certain characteristics of a vaccine that you think are important or might influence whether you take it? |
Focus groups were conducted in IsiZulu and SeTswana. The interview guide was developed in English, and the focus group moderator reviewed the questions with study investigators in order to determine correct terminology in IsiZulu and SeTswana. A separate study assistant then translated discussion guide questions back into English, and any ambiguities or inconsistencies were clarified. A South African woman fluent in IsiZulu, SeTswana (native language) and English, assisted by a note taker, moderated the focus groups. Each group lasted approximately 90 minutes. Written informed consent was performed at the start of the focus group by the moderator. Participants completed a brief sociodemographic questionnaire at the conclusion of the discussion. Socio-economic status was assessed by collecting information on ownership of household durables ranging from basics such as piped water and electricity, to mobile phones and refrigerators, to luxuries such as satellite TV and domestic workers. Participants received one point for each of the 20 items, and the range and mean score of durables was calculated.
Data Analysis
Discussions were audiotaped with participants’ permission and tapes were independently translated and transcribed in a single step. This single step approach was taken as the discussions involved words and passages in all three languages (IsiZulu, SeTswana and English), and did not have fidelity to one language alone. The multilingual focus group moderator as well as two of the English speaking investigators checked each individual transcript for accuracy. When inconsistencies or questions arose, the passage was transcribed first into IsiZulu or SeTswana, and then translated into English, followed by independent back translation to resolve inaccuracies. During the transcription/translation process a participant code was assigned to each text passage in the focus group transcript, so that each statement may be identified at the participant and the group level. Two principal investigators (JS and CM) read the transcripts to identify major themes. Next, the investigators independently performed a line-by-line review of the transcripts and hand coded for each major theme using a framework analysis approach (Pope, Ziebland, & Mays, 2000). Text corresponding to each of the themes was grouped together and reviewed. Inter-coder reliability was assessed for a random 10% of the text, and the Kappa statistic was calculated to be 0.90.
Analysis continued as an iterative process through discussions and refining of the major themes. Sub-themes were then established using a method of constant comparison (Strauss & Corbin, 1998) to break down higher-level codes (themes) into smaller categories or sub-themes within the framework. Data source triangulation (comparing data across focus groups as well as between male and female groups), as well as collaboration (patients and staff from clinic provided input on wording and orientation of study questions as well as feedback on themes found in interpretive analysis), researcher reflexivity (interpretive commentary considers researchers lens/point of view), and rich description was used to enhance the validity and reliability of the findings (Creswell & Miller, 2000).
RESULTS
Background characteristics
Sociodemographic characteristics of the participants are presented in Table 2. The mean age of participants was 21.5 years, with the majority being involved in full-time study (43%); 30% of the overall sample reported some or no high school education. Of 20 potential durables, the maximum was 19, the minimum 0 and the mean 9. Ownership of household durables ranged from 85% (electricity) to 5% (domestic worker in the home). The vast majority of participants were not married (95%); just over half reported a single sexual partner in the past 3 months and almost two-thirds of these reported using a condom at last intercourse. Two-thirds reported having previously had an HIV test.
Table 2.
Sociodemographic Characteristics of Focus Group Participants
| Characteristics | % Sample (n) |
|---|---|
| Age (n=42) | |
| 18-22 | 64.3 (27) |
| 23-26 | 35.7(15) |
| Gender (n=42) | |
| Male | 40.5 (17) |
| Female | 59.5 (25) |
| Main Occupation (n=41) | |
| Full time student | 41.5 (17) |
| Part time student | 7.3 (3) |
| Employed | 34.1 (14) |
| Unemployed / not student | 17.1 (7) |
| Education (n=40) | |
| No / some high school | 30.0 (12) |
| Completed high school | 30.0 (12) |
| Some tertiary studies but no graduation | 40.0 (16) |
| Marital Status (n=42) | |
| Single | 95.2 (40) |
| Married | 2.4 (1) |
| Separated | 2.4 (1) |
| Ethnic Group (n=40) | |
| Ndebele | 20.0 (8) |
| Zulu | 27.5 (11) |
| Tswana | 10.0 (4) |
| Tshivenda | 17.5 (7) |
| Other ethnic group | 25.0 (10) |
| Partner in the last 3 months (n=41) | |
| None | 31.7 (13) |
| One | 51.2 (21) |
| Two | 12.2 (5) |
| Three or more | 4.9 (2) |
| Condom use last time had sex (n=36) | |
| Yes | 63.8 (23) |
| No | 36.1 (13) |
| Had HIV test (n=42) | |
| Yes | 61.9 (26) |
| No | 38.1 (16) |
| HIV Status (n=41) | |
| HIV + | 7.3 (3) |
| HIV – | 53.7 (22) |
| Don't know | 39.0 (16) |
Knowledge About Vaccines
General knowledge about vaccines was relatively low, particularly for young women who did not have children, and young men.
To be honest I don't know anything [about vaccines] but I think I know what they do... it boosts your immune system and it helps you live longer (Male participant).
Initial discussions about vaccines were introduced within the context of routine childhood and adult vaccinations. About half of female participants, and very few male participants were familiar with childhood vaccines. One participant explains:
When they take (babies) to the clinic to inject them, it is for the children not to be affected by any diseases when they are still young. It is for their survival while they are still young (Female participant).
The most commonly recognized childhood vaccines were polio and measles (mentioned in 5 of the 6 groups), although whooping cough and tetanus were also mentioned in 2 groups. The three female participants with children had the highest knowledge of childhood vaccines. Knowledge about adult vaccinations was limited. A small number of participants had experience with flu vaccines, and others had heard of recent developments in vaccines for prevention of sexually transmitted disease (the HPV vaccine had been recently approved and was in the news at the time of the study). Participants familiar with vaccines were also aware of attributes, such as the need for repeat dosage (or boosters) and minor side effects that may occur immediately after vaccination. One participant explained his understanding of vaccines:
Vaccines I would say are anti body precautions medicines, like you are given maybe anti body of a certain virus in order to make sure that the day you get that virus, it can be battled, like for example... in order to prevent flu you are... injected with anti bodies for flu. (Male participant)
In five of the six focus groups, there was a need for clarification of the role of vaccines as prevention as opposed to treatment. Additionally, participants were curious as to what made some HIV prevention methods vaccines and others not. For example, several participants asked about whether condoms, antiretroviral medication to prevent mother-to-child transmission and microbicides could be considered HIV vaccines. “I think a condom is one of the HIV/AIDS vaccines to prevent people from getting HIV” (Female participant). Interestingly, at least one participant in three of the six focus groups was aware that HIV vaccines were being developed and tested. The majority of participants were not aware of efforts to develop HIV vaccines in the international community. None of the participants thought that an HIV vaccine was available currently.
They are not on the market; they are still discussing the issue. The government, Mantwa [Minister of Health] and everyone you know. Some are saying it is good, some are saying it is bad.’(Female participant)
Barriers To Future HIV Vaccine Uptake
Overall, vaccine acceptability was high among participants in both male and female groups. Approximately three-quarters of participants reported that if an approved HIV vaccine was available, they and their friends/family would take it. However, important barriers to uptake of the vaccine were also identified.
Mistrust of government and scientists
Participants in all of the 6 focus groups brought up concerns about receiving reliable and trustworthy information about an HIV vaccine once it is available. Mistrust of the government and the scientific community was reflected in a belief that the risks or toxicities associated with an HIV vaccine would not be fully disclosed to the public. One participant explains, “We must also be careful if they [government] are trying to make people sick...They just introduce something to the market and don't tell us anything about it and then after that people die from that thing.” (Female participant)
Similarly, participants in each of the six groups expressed concern that the public may be misled into thinking that an HIV vaccine provides a higher level of protection than it actually does.
People may not get the vaccine because they are not trusting...you might find that [scientists] are saying the vaccine does work, and then you get the vaccine and it doesn't help you. People think, “they are just pulling our socks again”...because they have told stories like this before. (female participant)
In this context of mistrust, vaccine efficacy demonstrated by researchers with carefully designed clinical trials was not reliable evidence to participants. The majority of participants who expressed mistrust believed that the most accurate information about the effectiveness of a vaccine comes from the personal experiences of friends, family, and other community members. One example was knowing someone firsthand who got the vaccine, then had an HIV exposure through unprotected sex with a person who was known to be HIV-infected, and did not contract the virus. “I would want to see with my own eyes if this person is getting sick or not, then I would use it. In the papers they would tell you that today it's working, tomorrow it's not...So if I see that it is working for my friend, then I would use it also...” (Male participant)
Associations of vaccine uptake with stereotypes of promiscuity
Another potential barrier to HIV vaccine uptake was fear of being labeled sexually promiscuous because of taking the vaccine. Nearly all participants described how partners, parents, family, church members, and the community overall might question why a young person would “need” an HIV vaccine, equating its use with admission of sexual activity or having multiple partners. For example, one young man says, “If I tell my girlfriend I'm going for a HIV vaccine...She'll go: Why do you need it? You only have me.” Female participants also frequently expressed concerns about being labeled ‘promiscuous’ or a ‘prostitute’ by parents, family members, or the church if they were to take an HIV vaccine. “In my family I would be considered an outcast if I take it...they follow the church teachings without hesitation, and they will call me a prostitute for not using my own behavior alone to prevent AIDS.” (Female participant)
While concerns about the reactions of family and the church were not raised in the male focus groups, several young men described possible stigmatization within the community or medical care setting. One participant said “This guy is going for the HIV vaccine, so he's accusing himself...they are associating it with someone who's been sleeping around...like he has bad behavior. I think one of the reasons he won't get [the vaccine] will be this stigma.” Interestingly, even though HIV is overwhelmingly an epidemic of heterosexual women and men in South Africa, one male participant described concerns about stereotypes of homosexuality, “Some would believe that you are gay, you need vaccines for gays.”
Fear of HIV testing and HIV stigma as barriers to vaccine uptake
Two of the most commonly mentioned barriers to HIV vaccine uptake were fear of having to test for HIV prior to receiving a vaccine, and fear of the stigma that one would encounter if she/he were HIV-positive. Participants in 5 of the 6 focus groups described how a requirement to be tested for HIV prior to being given the vaccine would result in many people forgoing vaccination. One female participant says, “We won't use the vaccine. It's the same as now, I hear that treatment for HIV is for free, but I don't know my status. So it's the same [with] taking the vaccine.” A male participant described how the emotional toll of HIV testing may be a barrier to vaccine uptake, “While I'm waiting for my [HIV test] results there's too much stress, so I will have too much stress and I will end up having depression...I won't agree to go to the clinic first and test.”
Uptake of the HIV vaccine was also described as a way of revealing a person's HIV status, as most participants believed that only HIV-negative persons would be offered a preventive vaccine. Therefore, knowing if a person received the vaccine would also disclose their HIV status and lead to potential stigma and discrimination for those who are HIV-positive. As one male participant describes, “The vaccine will be for negative people, so if you go and get the vaccine, we know you are negative...[I]f this guy didn't go, he's positive and that's why...so that is the stigma for HIV-positive people.” In 4 of the 6 groups participants report that because of low levels of knowledge about vaccines in the community, people who take the vaccine may end up being labeled as HIV-positive and stigmatized:
People will be afraid of rumors because not everyone is educated. People will think that if they take the vaccine others will think they have HIV...The community will stay away from you if they know you took the vaccine...I think they will confuse this vaccine with ARVs [antiretrovirals]. They will think if you take the vaccine it means you are HIV-positive. (Female participant)
Regardless of the direction of the stigma (i.e. for those who take vaccine or those who do not) participants agreed that it could influence decisions about vaccine uptake, “People won't get the vaccine because they are going to be ashamed...they will think they look suspicious when they go to get it...” (Female participant)
Vaccine Characteristics as Barriers to HIV Vaccine Uptake
The potential for side effects was also described as a barrier to future HIV vaccine uptake. Participants were familiar with side effects of childhood vaccines, and one or two in each group had also experienced side effects such as fevers, chills, and general malaise from receiving the influenza vaccine as an adult. One female participant explained:
Last year I had a flu vaccine because I was scared that the flu was gonna come very hectic on me...I became so sick from that vaccine! So I got sick because I was trying to prevent that disease...Since that time I told myself, no I'm not gonna do any vaccine no more.
Another participant shared this perspective, indicating that she preferred nutrition as an alternative to vaccines for disease prevention, “I think vaccines are going to make people sick. People must just eat healthy food to prevent everything.”
Participants also discussed duration of protection as a vaccine characteristic that may affect uptake. Interestingly, nearly all participants said they would prefer a duration of protection of a year or shorter, citing more frequent administrations or boosters as a way of knowing the vaccine is “active” in their body. Many participants believed they would distrust the efficacy of a vaccine that was only administered once or infrequently, “If it's once in my whole life I wouldn't trust it.” (Female participant)
Cost was another potential barrier to vaccine uptake. There was consensus that a high cost vaccine would clearly be a barrier for much of the population, particularly among the young and those unemployed or living on government grants. However, several participants pointed out that a free vaccine might also have poor uptake, particularly among youth. Participants describe a perception among themselves and their peers that free items are inferior to those that come at some cost. One male participant described his opinions about HIV vaccine acceptability and cost:
So if we get that vaccine...if it will be for a thousand rand, people will know and it will motivate them. If it's for free, everyone takes it for granted that he knows that anytime I'm going to get that. But if they know that it's their money they have to work for, sweat for it and then they go to buy the vaccine...that kind of value people will take it serious.
Lack of perceived vulnerability
There was a wide range of perceived vulnerability to HIV-infection in our sample of South African youth. About a quarter of participants in each group expressed concern about contracting HIV themselves and the impact of HIV on the greater community. In the words of one young man, “this disease is killing us, it's killing our society.” However, in five of the six groups, other participants felt they were not personally vulnerable to HIV and didn't need the vaccine because they did not engage in risky sexual behavior, or they used condoms regularly. One female participant explained, “You can perceive me the way you want to, I'm sorry, I won't get it [vaccine]. I haven't had sex without a condom and I will never ever.”
Perceived vulnerability to HIV was also described as varying between urban and rural communities. In four of the six groups participants believed that rural communities were less likely to think that they were at risk for HIV, which may become a barrier to vaccine uptake. One participant explains, “People who live in those [rural] parts, they take AIDS as if it's something that is in Jo'burg only...they don't take it as if in Venda [rural tribal area] there is AIDS and HIV, they don't even take it seriously.”
Community attitudes about HIV
Community attitudes and blame for HIV were described as influencing vaccine uptake in each of the six groups. For example, one participant explained how in his own community the older generations blame the young for behavior that introduced the disease of HIV. Furthermore, he describes how a belief that HIV vaccine will promote promiscuity in youth may be a barrier for parents.
For us in the black community everything is a problem. Like parents believe that HIV-infection comes through children, they themselves don't know it because in their days when they begot children there was not things like HIV...They believe the youth brought AIDS, so when there's a vaccine, they gonna think it's another plan to make children more sexually active...they won't accept it.
Participants also described the role of religion in shaping attitudes about HIV vaccines. One young woman describes how religious beliefs and fatalism may interfere with HIV prevention and vaccines specifically:
People who say they are Christians can say no to that vaccine thing ‘cause in the Bible it's stated that there's this disease that is going to kill people and it can never be prevented...it's gonna stay here, it's going to kill people because it [the Bible] says the world is coming to an end...
Another male participant articulated the need to resist social norms and community beliefs that may be barriers to vaccine uptake, “I want to challenge the moral thing, people should have a chance to really get to discuss, and then go home and think about it, and how am I gonna take the next step? Am I going for the vaccine or not? ‘Cause there will be social conditionings, there will be gender conditionings, if as an individual you still base your thoughts on other people...”
Traditional African healing
In two of the six focus groups, participants discussed how beliefs in traditional African healing may deter individuals from an HIV vaccine. The vaccine was categorized as a “western medicine,” and was not viewed to be compatible with the traditional African healing paradigm by some participants. Those who had experience with traditional healers expressed skepticism and mistrust of western medicine, “We have to stick to our tradition...our culture, our socialization ‘cause if I was taught not to get pills because pills are associated to bombs, or to wherever they are manufactured...it would not be easy to accept the vaccine.”
Motivators Of HIV Vaccine Uptake
Protection against HIV transmission risks outside of one's control
The most frequently discussed motivator for HIV vaccine uptake was the ability to be protected from HIV when the transmission risk was out of an individual's control. Over half of the participants perceived non-sexual modes of HIV transmission to be a significant threat, including injuries from car accidents, sewing needles, nail cutters, and injections received at the hospital. For example one female participant asked, “What if you use a condom and get HIV in a car accident? Why don't you just take the prevention [vaccine] and be safe forever if you are negative?” Some believed that non-sexual HIV transmission was their only risk of contracting HIV, “I will use it for safety in car accidents, not in sex.”
Sexual modes of transmission that were out of an individuals control, such as partner infidelity and rape, were also described as strong motivators for using an HIV vaccine in all six groups. One woman explained, “If I have taken that [vaccine] ...if my partner cheats on me I will be able to have prevention.” Similar benefits of being vaccinated, specifically in the context of marriage were also discussed, “One day I would like to get married, I don't know what my husband will be like, so I'm just preventing myself from getting the disease...I know I can trust him, but maybe things will change and I won't.” A young man expressed the benefits of a vaccine for men in the context of rape in prisons:
For me, in a prison scenario...you might get raped and get HIV, so having the vaccine available there is a great place to start. It should become a protocol in prison, after you get your prison number you get a vaccine, ‘cause they don't know whose gonna rape you in there...so at least your chance of getting HIV is less.”
Desire to raise a family
Female participants described the desire to live to parent their child, as well as the ability to have a family with an HIV-positive partner as two important reasons they would consider taking an HIV vaccine. With regard to parenting one woman said, “I am a parent myself...and here is the vaccine, it's available, and I think I would use it just for me to raise my child.” Another participant explained the role an HIV vaccine could play in allowing her to start a family with an HIV-positive partner. “I support the vaccine because if I'm not married and I meet someone who is HIV-positive, and I'm negative ...if I love that person and I want to have a baby...it is better to go and get the vaccine.”
Unprotected sex and multiple partners
Whereas women described the desire to raise a family as a central motivator of vaccine use, the majority of men cited the ability to have sex without a condom and having multiple sexual partners as advantages of taking the HIV vaccine. Several men in each group stated that if a vaccine were available they would not need to worry about HIV prevention, and therefore would not need to use a condom or limit the number of sexual partners they had. In the words of one male participant, “with the vaccine...one advantage is people would enjoy sex without condoms, because now many do not enjoy with a condom.” Another stated “I won't have stress about HIV anymore, I can just go for it like nobody's business...”
Male participants also described advantages of the vaccine in the context of a primary relationship: “If the HIV vaccine becomes available, you can have more than one partner... [B]ut if there's a partner that you would want to spend the rest of your life with, you can secretly cheat as long as HIV is not there.” It is important to mention that four of the men in the focus groups reacted strongly to the discussion about increased promiscuity, stating their sexual behavior would not change significantly if a vaccine was available. However, all male participants were in agreement that these factors would be seen as a motivator for vaccine uptake among many of their peers.
Among female participants, reduced condom use and multiple sexual partners in the setting of a HIV vaccine was described as a concern as opposed to a motivator. Several women in each group felt that decreased condom use would not be an advantage of the vaccine because it didn't protect against pregnancy and other STDs. In addition, several female participants expressed concern that fidelity and “moral” sexual behavior would be compromised by an effective vaccine, “If a vaccine is available people will not fear HIV anymore. Now the fear of HIV keeps people's moral behavior under control.”
Community, government, and media
Individual communities, the government, and the media were all described as having the potential to improve vaccine uptake through education, influencing social norms, and providing incentives to use HIV vaccines. In describing his community's attitude toward an HIV vaccine, one man said, “Discrimination will end. People would just say its better to do this [vaccine] because they are parents themselves. In their community they see people related to them [get sick], they also lose people, so they would just say it's a go!” Another participant described the importance of considering social inequities in society when addressing HIV prevention and vaccine use:
If we say why is this virus spreading a lot I would code issues of poverty, war, conflict, violence...rape...refugee camps...sex work because there are no jobs. As much as we want the vaccine we need to see other ways of improving it [prevention], like reducing unemployment and attacking those problems.
Participants also believed the government could play a significant role in improving HIV vaccine uptake through the use of incentives, mandates, and outreach. One male participant suggested, “Those who come for injections, maybe they will give one hundred [Rand/ZAR; $20 USD] for groceries to each...they [government] should give them incentives so they can be vaccinated.” Another female participant believed that the vaccine should be mandated, “If this vaccine was to be available, I would personally suggest to the government that everybody should be injected.” Participants also believed vaccine dissemination and uptake could be enhanced by outreach to rural and high risk communities, “Access to mobile visiting cars to get it [vaccine]...outreach to rural areas, supermarkets...even the bar with sex workers, so before you buy [sex] at least there is someone who has the vaccine” (male participant).
In all six groups the media was cited as another important facilitator of vaccine uptake, both through education and community mobilization. One female participant explained:
I think it is different in rural areas, some people don't have that knowledge so...I think the government should do a drama ...like Generations [a soap opera]...so at least people have enough knowledge to know [the vaccine] is saving lives.
The role of the media in mobilizing the community through newspapers, TV, radio, billboards and advertising was also emphasized. One male participant describes the importance of a collaborative approach, “ Like we did with HIV when people didn't actually believe it is here and killing people...the government went in, and the youth went in, the media, everybody went in...so that is how we have to do it...we must show people that here is someone who does not have AIDS who took it [vaccine]...and slept with somebody who had AIDS but he didn't get infected.”
DISCUSSION
Few studies have examined future HIV vaccine acceptability in the setting of high prevalence African countries. In this study, we use a conceptual model grounded in value expectancy theory and social marketing to study the behavioral intentions of young adults in South Africa with regard to acceptability of a future HIV vaccine, and barriers and motivators to future HIV vaccine uptake. Aspects of our conceptual model that were particularly relevant to the study sample were the role of behavioral and normative beliefs, social norms, and perceived risk as barriers and motivators to future HIV vaccine uptake. We found these beliefs, norms and perceptions to be most powerful in shaping the acceptability of a future HIV vaccine in our sample, relative to the more tangible hypothetical vaccine characteristics. Knowledge of vaccines in general and HIV vaccines specifically was low in the sample, and our model suggests utility in efforts to improve knowledge about HIV prevention overall, including testing, behavioral change, and vaccines when developing dissemination plans for a future HIV vaccine.
While our participants differ in many ways from the US populations that have been previously studied, we found several barriers to HIV vaccine uptake common to both groups, suggesting these factors may be important in the context of both the developed and developing world. These included fear of side effects, high cost, HIV stigma and discrimination, as well as mistrust of health care professionals and government as barriers to vaccine uptake (Newman et al., 2006; Rudy et al., 2005). Similar to the findings of Rudy et al., our participants also identified a role for the health care system and government to promote positive subjective norms that encourage HIV vaccination for the public.
One newly identified and commonly mentioned barrier to HIV uptake in our sample of South African young adults was HIV testing in the setting of vaccination. Fear of HIV testing was frequently mentioned in both female and male groups, and many participants believed that a requirement for testing prior to receiving vaccination would be a barrier to dissemination efforts. Fear of HIV stigma and discrimination continues to discourage testing among South African youth, despite free access to HIV treatment (Macphail et al., 2006). Participants in clinical trials of vaccines have also expressed concerns about having to first learn of their HIV status before enrolling in trials (Smit et al., 2006). Attitudes about HIV testing, fueled by the pervasive stigma of HIV, have the potential to hinder dissemination efforts. There will be a continuing need to study and address these issues in order to optimize uptake of a future post-trial HIV vaccine in contexts such as South Africa where fear of stigma and discrimination are widespread barriers to testing.
We found that knowledge about vaccines generally, and HIV vaccines specifically, were low for the majority of participants, with the exception of those who were parents or caretakers and had experience vaccinating a child. This is despite a publicized HIV vaccine trial in a neighboring community in Johannesburg that was ongoing during the study period. Our findings are consistent with research from the KwaZulu-Natal region of South Africa, which reported that 48% of participants had never heard of HIV vaccines (Lindegger, Quayle, & Ndlovu, 2007). This is in contrast to the levels of knowledge in communities in Uganda, where good access to childhood immunization programs is thought to contribute to knowledge and familiarity with vaccines (Kiwanuka et al., 2004). Confusion about the role of vaccines as preventive agents rather than treatment, and the mechanism of action that delineates vaccines from other types of prevention (microbicides, condoms) was also present in our sample, and has been previously documented in South African populations (Lindegger et al., 2007) as well as among military conscripts in Uganda (McGrath et al., 2001). Our results suggest that education about vaccines in general, and the specific protection provided by HIV vaccines will be an important component of community preparedness efforts in populations that do not have high penetration of childhood or other adult vaccines.
Mistrust of information about an HIV vaccine provided by the government, scientists, or the media was another potential barrier to vaccine uptake, which has been described in ethnic minority and low socioeconomic US populations (Newman et al., 2006; Roberts, Newman, Duan, & Rudy, 2005). In our study, this mistrust arose in the context of recent highly publicized South African microbicide trials that may have put trial participants at increased risk of contracting HIV, and a government that many felt was slow to act to stem the HIV epidemic, denied that the HIV virus caused AIDS, and whose Minister of Health has consistently endorsed nutritional supplements over antiretroviral therapy for the treatment of AIDS. While mistrust may be intensified by the specific political economy of South Africa, previous studies suggest that the lack of transparency and false information that has fostered mistrust of the government, science, and health care are not unique to South Africa (Newman et al., 2006; Roberts et al., 2005), and have the potential to interfere with dissemination efforts around the world. A smaller number of participants also felt that mistrust of western medicine and a preference for traditional African remedies may also limit uptake of an HIV vaccine. The practices of traditional medicine and “western” medicine were largely viewed as mutually exclusive, reflecting contrasting illness paradigms. Our findings suggest a great need for discussion and collaboration between traditional practitioners and “western medicine” if biomedical HIV prevention efforts are to be successful in countries where both types of practice are prevalent.
Overall, motivators for vaccination differed by gender. Women's discussions tended to focus on the normative beliefs of family members and friends as strong motivators for vaccine uptake, while men were more likely to see vaccines as an opportunity to stop using HIV prevention strategies such as condoms and partner reductions. The potential for sexual disinhibition in the context of an approved HIV vaccine is suggested by our findings; however, women were primarily concerned about disinhibition among men rather than changes in their own behavior. This suggests that education and risk reduction counseling for other sexually transmitted infections and pregnancy are likely to be critical components of any post-trial HIV vaccine dissemination campaign and that interventions may need to be tailored by gender.
Study Limitations
We chose the focus group method to explore acceptability of a future HIV vaccine. The limitations of focus groups include overrepresentation of specific participant contributions, as certain individuals may dominate the conversation or influence the overall dynamics in the group (Kreuger, 2000). However, we did take steps in coding to track and account for comments at the individual participant level. While we did not engage participants in formal member checking, our study included several methods for improving validity of qualitative studies, including triangulation, collaboration, researcher reflexivity, and rich description. Because the focus groups included mixed IsiZulu, SeTswana, and English words/passages, we used a modified translation protocol that did not involve transcribing all text into one African language, followed by translation and back translation. This means there may have been errors in translation/interpretation that were not identified by the investigators. We chose to purposively sample participants from an inner city clinic serving large numbers of patients with sexually transmitted infections, as it allows us to identify key barriers to vaccine uptake among young women and men who are engaging in HIV risk behaviors and would most benefit from an HIV vaccine. However, our goal was not to recruit a representative sample, thus our results may not generalize to all South African youth. Because participants were already seeking medical care, our sample may be biased toward participants who view biomedical prevention more favorably than those recruited from other venues, for whom HIV vaccine acceptability may be more challenging. Additionally, the majority of our participants have had at least some high school education, and results may differ among youth with lower levels of education and literacy. Despite these limitations, we were able gain important new knowledge about key factors that may influence behavioral intentions to accept an HIV vaccine, once it becomes available. Future studies that include representative samples in areas with high HIV prevalence, and examine the role of HIV vaccines on sexual risk behavior are needed to prepare for future post-trial dissemination campaigns.
Implications for Practice
This study identifies a range of perceived barriers and motivators to uptake of a future HIV vaccine, including mistrust of the government and scientific community, HIV/AIDS stigma, as well as concerns about cost and equitable distribution. These barriers mirror many of the challenges faced by practitioners in behavioral HIV prevention efforts, HIV testing, and HIV treatment in many parts of the world, and may play a role in fueling the existing health disparities for persons living with HIV/AIDS (Newman, Williams, Massaquoi, Brown, & Logie, 2008; Tsai, Chopra, Pronyk, & Martinson, 2008). Partnerships between practitioners and communities to improve rates and acceptance of HIV testing as well as sustained efforts to destigmatize HIV/AIDS are of critical importance to effectively address disparities in HIV/AIDS today, and to prevent further disparities in future HIV vaccine dissemination efforts. In our study, participants articulated the need to challenge moralistic and polarizing views of HIV in order to facilitate open discussion and enable individuals to make informed decisions about future HIV vaccine uptake. In this context, a discussion of biomedical prevention may provide the health educator opportunities to reframe HIV risk and prevention, and to move beyond moral codes of behavior. Discussions of biomedical prevention also may serve as a vehicle to encourage community dialogue between younger and older generations that address stigma and social norms, which are impediments to the success of existing HIV prevention and treatment.
ACKNOWLEDGEMENTS
This research was funded by the Center for HIV Identification, Prevention and Treatment Services (CHIPTS), University of California, Los Angeles (NIMH grant # P3058107). Dr. Sayles received support from an NIH National Research Service Award. Dr. Cunningham received partial support from UCLA/ DREW Project EXPORT, NCMHD, P20MD000148/P20MD000182 and UCLA RCMAR/CHIME, NIA grant #2P30AG021684. Thanks to Prudence Ngoako who conducted and managed the focus group discussions. Thanks to staff at the Esselin Street clinic for their assistance in recruiting and conducting the study, as well the clinic patients who participated in this study.
REFERENCES
- Ajzen I. In: From intentions to actions: A theory of planned behavior. Kuhl J, Beckmann J, editors. Springer-Verlag; Berlin: 1985. pp. 11–39. [Google Scholar]
- Bateman C. HIV/AIDS pandemic--a legacy of conquest and mistrust. S Afr Med J. 2005;95(7):464–465. [PubMed] [Google Scholar]
- Becker MH, Joseph JG. AIDS and behavioral change to reduce risk: a review. Am J Public Health. 1988;78(4):394–410. doi: 10.2105/ajph.78.4.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell J, Miller D. Determining Validity in Qualitative Inquiry. Theory Into Practice. 2000;39(3):124–130. [Google Scholar]
- Daftary A, Padayatchi N, Padilla M. HIV testing and disclosure: a qualitative analysis of TB patients in South Africa. AIDS Care. 2007;19(4):572–577. doi: 10.1080/09540120701203931. [DOI] [PubMed] [Google Scholar]
- Dahl V, Mellhammar L, Bajunirwe F, Bjorkman P. Acceptance of HIV testing among women attending antenatal care in south-western Uganda: risk factors and reasons for test refusal. AIDS Care. 2008;20(6):746–752. doi: 10.1080/09540120701693990. [DOI] [PubMed] [Google Scholar]
- Esparza J, Osmanov S, Pattou-Markovic C, Toure C, Chang ML, Nixon S. Past, present and future of HIV vaccine trials in developing countries. Vaccine. 2002;20(15):1897–1898. doi: 10.1016/s0264-410x(02)00062-2. [DOI] [PubMed] [Google Scholar]
- Excler JL, Kochhar S, Kapoor S, Das S, Bahri J, Ghosh MD, et al. Preparedness for AIDS vaccine trials in India. Indian J Med Res. 2008;127(6):531–538. [PubMed] [Google Scholar]
- Fishbein M, Azjen I. Belief, Attitude, Intention, and Behavior: An Introduction to Theory and Research. Addison-Wesley; Reading, Mass.: 1975. [Google Scholar]
- International AIDS Vaccine Initiative (IAVI) The Futures Group Estimating the Global Impact of an AIDS Vaccine - IAVI Policy Brief. Policy Research Working Paper. 2005:4. from http://www.iavi.org/file.cfm?fid=35123.
- Johnson LF, Bekker LG, Dorrington RE. HIV/AIDS vaccination in adolescents would be efficient and practical when vaccine supplies are limited. Vaccine. 2007;25(43):7502–7509. doi: 10.1016/j.vaccine.2007.08.047. [DOI] [PubMed] [Google Scholar]
- Kiwanuka N, Robb M, Kigozi G, Birx D, Philips J, Wabwire-Mangen F, et al. Knowledge about vaccines and willingness to participate in preventive HIV vaccine trials: A population-based study, Rakai, Uganda. Journal of Acquired Immune Deficiency Syndromes. 2004;36(2):721–725. doi: 10.1097/00126334-200406010-00009. [DOI] [PubMed] [Google Scholar]
- Kreuger RA. Focus Groups--a practical guide for applied research. Sage Publication; Thousand Oaks: 2000. [Google Scholar]
- Lindegger G, Quayle M, Ndlovu M. Local knowledge and experiences of vaccination: Implications for HIV-preventive vaccine trials in South Africa. Health Education & Behavior. 2007;34(1):108–123. doi: 10.1177/1090198105277852. [DOI] [PubMed] [Google Scholar]
- Macphail CL, Pettifor A, Coates T, Rees H. “You Must Do the Test to Know Your Status”: Attitudes to HIV Voluntary Counseling and Testing for Adolescents Among South African Youth and Parents. Health Education & Behavior. 2006 doi: 10.1177/1090198106286442. [DOI] [PubMed] [Google Scholar]
- McGrath JW, George K, Svilar G, Ihler E, Mafigiri D, Kabugo M, et al. Knowledge about vaccine trials and willingness to participate in an HIV/AIDS vaccine study in the Ugandan military. Journal of Acquired Immune Deficiency Syndromes. 2001;27(4):381–388. doi: 10.1097/00126334-200108010-00009. [DOI] [PubMed] [Google Scholar]
- Morrison D, Gillmore M, Baker S, et al. Determinants of condom use among high-risk heterosexual adults: A test of the Theory of Reasoned Action. Journal of Applied Social Psychology. 1995;25:651–676. [Google Scholar]
- Ncama BP, McInerney PA, Bhengu BR, Corless IB, Wantland DJ, Nicholas PK, et al. Social support and medication adherence in HIV disease in KwaZulu-Natal, South Africa. Int J Nurs Stud. 2008 doi: 10.1016/j.ijnurstu.2008.06.006. [DOI] [PubMed] [Google Scholar]
- Newman PA, Duan N, Roberts KJ, Seiden D, Rudy ET, Swendeman D, et al. HIV vaccine trial participation among ethnic minority communities: Barriers, motivators, and implications for recruitment. Journal of Acquired Immune Deficiency Syndromes. 2006;41(2):210–217. doi: 10.1097/01.qai.0000179454.93443.60. [DOI] [PubMed] [Google Scholar]
- Newman PA, Williams CC, Massaquoi N, Brown M, Logie C. HIV prevention for Black women: structural barriers and opportunities. J Health Care Poor Underserved. 2008;19(3):829–841. doi: 10.1353/hpu.0.0043. [DOI] [PubMed] [Google Scholar]
- Pope S, Ziebland S, Mays N. Qualitative research in health care: analysis of qualitative data. British Medical Journal. 2000;320:114–116. doi: 10.1136/bmj.320.7227.114. (Clinical Research Ed) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Republic of South Africa: Department of Health . HIV and AIDS and STI Strategic Plan for South Africa 2007-2011. Pretoria: 2007. [Google Scholar]
- Roberts KJ, Newman PA, Duan N, Rudy ET. HIV vaccine knowledge and beliefs among communities at elevated risk: Conspiracies, questions and confusion. Journal of the National Medical Association. 2005;97(12):1662–1671. [PMC free article] [PubMed] [Google Scholar]
- Rudy ET, Newman PA, Duan N, Kelly EM, Roberts KJ, Seiden DS. HIV vaccine acceptability among women at risk: perceived barriers and facilitators to future HIV vaccine uptake. AIDS Education and Prevention. 2005;17(3):253–267. doi: 10.1521/aeap.17.4.253.66529. [DOI] [PubMed] [Google Scholar]
- SAAVI (South African AIDS Vaccine Initiative) Meeting on Social and Behavioural Research Issues Related to AIDS Vaccines; Stellenbosch: Social-behavioural Research Group. Durban, South Africa. 2005. [Google Scholar]
- Schutten M, de Wit JB, van Steenbergen JE. Why do gay men want to be vaccinated against hepatitis B? An assessment of psychosocial determinants of vaccination intention. Int J STD AIDS. 2002;13(2):86–90. doi: 10.1258/0956462021924703. [DOI] [PubMed] [Google Scholar]
- Smit J, Middelkoop K, Myer L, Seedat S, Bekker LG, Stein DJ. Willingness to participate in HIV vaccine research in a peri-urban South African community. International Journal of STD & AIDS. 2006;17(3):176–179. doi: 10.1258/095646206775809259. [DOI] [PubMed] [Google Scholar]
- Strauss A, Corbin J. Basics of Qualitative Research. Sage Publications; Thousand Oaks: 1998. [Google Scholar]
- Tsai AC, Chopra M, Pronyk PM, Martinson NA. Socioeconomic disparities in access to HIV/AIDS treatment programs in resource-limited settings. AIDS Care. 2008:1–5. doi: 10.1080/09540120802068811. [DOI] [PubMed] [Google Scholar]
- UNAIDS 2006 Report on global HIV/AIDS Epidemic. 2006.
- Wang Y, Li B, Zheng J, Sengupta S, Emrick CB, Cohen MS, et al. Factors Related to Female Sex Workers’ Willingness to Utilize VCT Service: A Qualitative Study in Jinan City, Northern China. AIDS Behav. 2008 doi: 10.1007/s10461-008-9446-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiser S WW, Bangsberg D, et al. Barriers to antiretroviral adherence for patients living with HIV infection and AIDS in Botswana. JAIDS. 2003;34(3):281–288. doi: 10.1097/00126334-200311010-00004. [DOI] [PubMed] [Google Scholar]