Abstract
Objective
To examine the initial efficacy of parent-child interaction therapy (PCIT) for treating behavior problems in young children who were born premature.
Method
In this randomized, controlled trial, 28 children between the ages of 18 and 60 months, who were born <37 weeks gestation and presented with clinically significant externalizing behavior problems, were randomly assigned to an immediate treatment (IT) or waitlist (WL) control group.
Results
After 4 months, children who received PCIT were reported by their mother to have less attention problems, aggressive behaviors, and externalizing and internalizing behavior problems, and they were observed to be more compliant to maternal commands than children in the WL group. In addition, mothers in the IT group interacted more positively with their child, reported lower parenting stress related to difficult child behavior and demonstrated improved parenting practices compared with WL mothers. Behavior change maintained for 80% of the IT children 4 months after treatment completion.
Conclusions
This study demonstrates preliminary efficacy of PCIT for the treatment of behavior problems in young children who were born premature.
Index terms: parent-child interaction therapy, behavior problems, prematurity
The prevalence of preterm birth has increased to 12.5% of all births in the United States and constitutes a significant public health concern.1 As a result, developmental pediatricians and other child development professionals see a growing number of children born premature, who present with a variety of medical and behavioral concerns. Specifically, follow-up studies of children born premature demonstrate an increased risk for developing externalizing behavior problems.2 These negative behavioral outcomes worsen with increased age3 and have been shown to result in a higher prevalence of behavior disorders (e.g., attention-deficit hyperactivity disorder) by early school age.4 These findings highlight the necessity for early identification of behavior problems and subsequent intervention with this population.
Mothers of preterm infants experience considerable distress during the newborn period,5 which may have implications for the development of later behavior problems. For example, it has been reported that maternal stress increased as a function of difficult preterm infant behavioral characteristics and strict child rearing attitudes.6 Alternatively, mothers who encouraged more autonomy and age-appropriate behaviors reported fewer behavior problems in their preterm children.7 However, promoting increased autonomy can be especially difficult for mothers of preterm children because of perceptions of increased vulnerability and the propensity to use a lax parenting style.8 Therefore, interventions promoting more effective parenting styles may help improve the behavioral outcomes among children born preterm.
Early intervention programs combining developmental and support services for preterm infants and their parents have been used and found to be successful in reducing developmental problems, and programs involving both parents and children have been the most efficacious.9 For example, mothers randomized to a family-based intervention in the neonatal intensive care unit showed more contingent and sensitive parent-infant interactions and less maternal stress compared with control mothers who did not receive an intervention.10 Another randomized trial, examining the efficacy of the Mother-Infant Transaction Program, resulted in a decrease in parental stress but did not yield treatment effects on cognitive, motor, or behavioral child outcomes at 2 years.11 To date, however, research examining psychosocial interventions for children born preterm is limited in that most interventions are implemented during the infancy period, address a broad range of problems, and do not link comprehensive assessment with the intervention.12 Furthermore, no study has examined a psychosocial intervention specifically targeting behavior problems in young children who were born premature.
The purpose of this study was to evaluate the efficacy of parent-child interaction therapy (PCIT) for treating externalizing behavior problems in children born premature. PCIT is an evidence-based parent-training intervention for treatment of disruptive behavior in young children,13 but the efficacy of this treatment for children born premature has not previously been examined in a randomized, controlled trial. PCIT can be particularly therapeutic for children born premature because of its focus on teaching parents to use an authoritative parenting style with their child (i.e., a combination of nurturance, good communication, and firm control). We hypothesized that in comparison with families in a waitlist (WL) control group, families in the PCIT group would show the following after treatment: (a) fewer parent-rated child behavior problems, (b) greater child compliance during observed parent-child interactions, (c) more positive and effective parenting behaviors during parent-child interactions, and (d) reductions in parenting stress and improved parenting practices.
METHODS
Participants
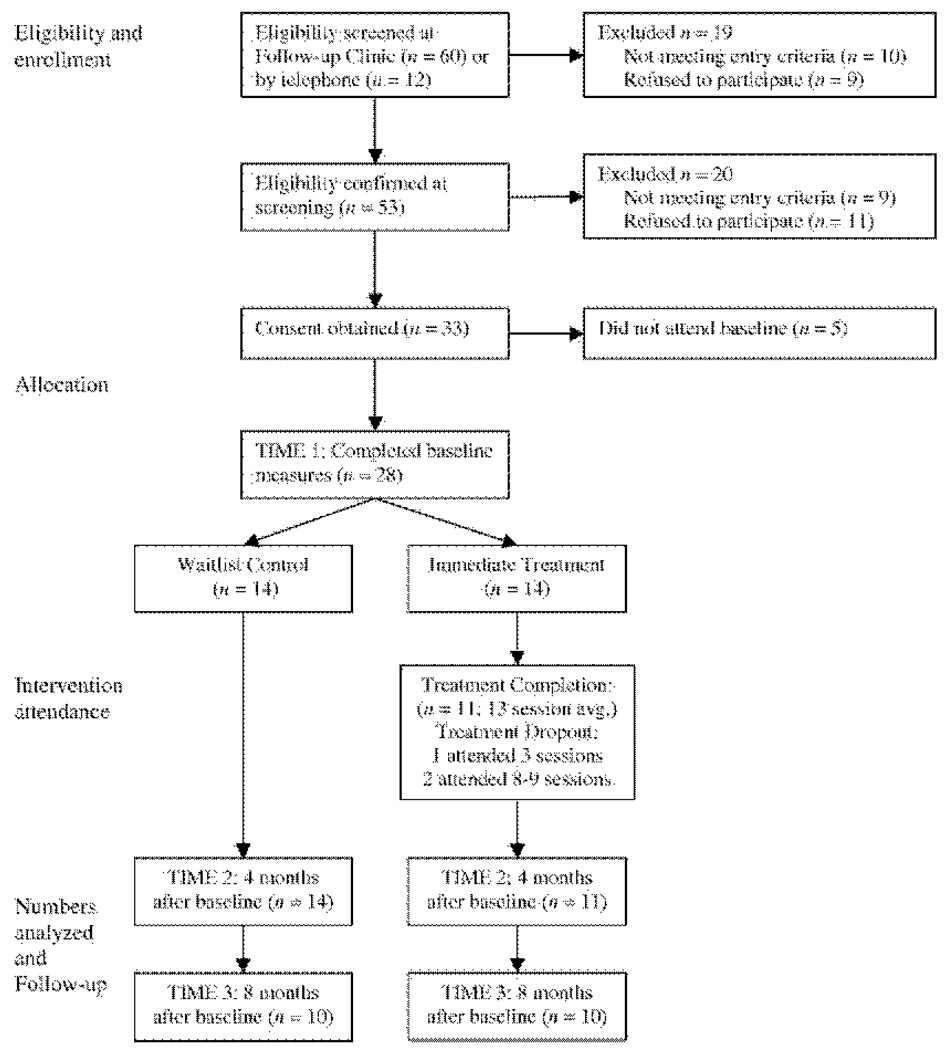
Participants were 28 mothers and their 18- to 60-month-old child who was born <37 weeks gestation. Children were referred between August 2007 and December 2008 by the director (Dr. Vohr) of a neonatal follow-up clinic (79%), health professionals at other pediatric sites (9%), staff at state-funded early intervention programs (6%), or self-referred by their mother after seeing a study brochure (6%). For study inclusion, mothers had to rate their child above the clinically significant range (T score ≥60) on the externalizing problems scale of the Child Behavior Checklist (CBCL) and be able to speak and understand English. Exclusion criteria for children included major sensory impairments (e.g., deafness and blindness), motor impairments (e.g., cerebral palsy significantly affecting mobility), and oxygen dependence for chronic lung disease. None of the 53 children attending the screening assessment were excluded based on these criteria. Children with symptoms of autism spectrum disorder, assessed by the Modified Checklist for Autism in Toddlers were excluded at the screening evaluation (n = 2). Although mother scores <75 on the Wechsler Abbreviated Scale of Intelligence was an exclusion criterion, no mother was excluded based on this criterion. The remaining 7 children who did not meet entry criteria at the screening evaluation had scores <60 on the CBCL externalizing problems scale (Fig. 1).
Figure 1.
Participant flowchart.
Study Design and Procedure
A randomized, controlled trial was used to determine the efficacy of parent-child interaction therapy (PCIT) compared with a waitlist control (WL) comparison group. Two computer-generated random numbers lists, one for boys and one for girls, were maintained by a statistician uninvolved in recruitment, intervention delivery, and data collection. After a family met eligibility and provided written informed consent with an assessor, the statistician assigned the family to the immediate treatment (IT) group if the number was even and to the WL group if the number was odd. All families participated in a baseline assessment (Time 1) and were informed of their group status at that time. Four months after the Time 1 assessment, all families were seen for the Time 2 assessment, which included the same measures completed at Time 1. Families participated in a Time 3 follow-up assessment 4 months after the Time 2 assessment, which was a follow-up assessment for IT families and the posttreatment assessment for WL families. All assessments were conducted in the clinic.
Intervention Description
PCIT is a manualized parent-training intervention with extensive research demonstrating its efficacy and long-term maintenance in treating young children with disruptive behavior disorders13 and showing promise with other at-risk populations, such as children with chronic illness14 and mental retardation.15 With foundations in attachment and social learning theories, PCIT was designed to change parent-child interaction patterns and thereby change child disruptive behavior. Treatment progresses through 2 distinct phases: child-directed interaction (CDI) resembles traditional play therapy and parent-directed interaction (PDI) resembles clinical behavior therapy.
During CDI, the parents follow their child’s lead in play by using the nondirective PRIDE skills: Praising the child, Reflecting the child’s statements, Imitating the child’s play, Describing the child’s behavior, and using Enthusiasm. They learn to direct the PRIDE skills to the child’s appropriate play and ignore undesirable behaviors. During PDI, the parents set limits to reduce child noncompliance and negative behavior. They learn to use effective commands and consistently follow through with timeout for noncompliance. The PDI procedure is only used at times when it is important that the child obeys a specific command. The parents are also taught variations of the PDI procedure to deal with aggressive behavior and public misbehavior. During all sessions, the therapist coaches each parent in vivo through a 1-way mirror (using a wireless headset) in their use of the CDI and PDI skills with their child.
PCIT sessions were conducted once a week for ~1 hour in length. In both phases of treatment, therapists actively coach parents toward mastery of the interaction skills as assessed during a 5-min parent-child observation at the start of each session. For this study, CDI was limited to 5 coaching sessions before beginning the PDI phase of treatment. However, CDI continues to be assessed and coached along with PDI skills in the PDI phase of treatment. Treatment is not time limited and continues until parents demonstrate mastery of the interaction skills. In addition, successful treatment completion requires the child’s behavior to be within ½ SD of the normative mean on a measure of child disruptive behavior, the Eyberg Child Behavior Inventory (ECBI; described later in detail). Parents complete the ECBI (taking ~5–10 min) at the beginning of each session to assess weekly treatment progress. In addition to helping parents master the CDI and PDI skills, additional procedures are used in PCIT to help reduce attrition, such as providing support to parents about concerns other than child management and making weekly reminder calls.
All therapy sessions were videotaped, and 50% were randomly selected and coded for integrity by a research assistant uninvolved in coding behavioral observations. Accuracy, defined as the percent with which the therapist adhered to key elements of each session detailed in the treatment manual, was 94% (range = 89–99%).
Demographic/Screening Measures
Socioeconomic status was measured using the Hollingshead Index of Social Position.16
The Modified Checklist for Autism in Toddlers is a 23-item parent-rating scale designed to identify children at risk for autism17 and is considered appropriate for children aged 18–48 months.18 The Modified Checklist for Autism in Toddlers was used for children between the ages of 18 and 48 months to exclude children with symptoms of autism spectrum disorder. For identification of children older than 48 months, parent report in conjunction with clinical judgment was used.
The Wechsler Abbreviated Scale of Intelligence19 is a short and reliable measure of intelligence that has high reliability and validity with other tests of intelligence.20 The Wechsler Abbreviated Scale of Intelligence was used to exclude mothers with cognitive impairment.
Clinical Outcomes/Measures
The CBCL21 is a 99-item parent-rating scale designed to measure the frequency of children’s behavioral and emotional problems with excellent psychometric properties. A T score ≥60 on the externalizing problems scale was required for study inclusion. The aggressive behavior, attention problems, and externalizing and internalizing scales were used as child behavior outcome measures. In this sample, internal consistency estimates for these scales ranged from 0.54 to 0.81.
The ECBI22 is a 36-item parent-rating scale of child disruptive behavior. The ECBI intensity scale measures the frequency with which disruptive behavior occurs, and the problem scale measures how problematic the child’s behavior is for the parent. Both scales yield excellent 12-week test-retest reliability coefficients.23 In this study, the ECBI was used as a measure of treatment outcome. Mothers receiving treatment also completed the ECBI weekly to assess treatment progress. The internal consistency estimates for the intensity and problem scales were 0.90 and 0.85, respectively.
The Dyadic Parent-Child Interaction Coding System24 is a behavioral coding system with documented reliability and validity that measures the quality of parent-child interactions.24 Several categories of parent and child behaviors may be selected for coding and include verbalizations, vocalizations, and physical behaviors. Behaviors are coded by recording the frequency of each occurrence in real time using a video coding system. For this study, we chose the categories that are most relevant to treatment outcome. We created a composite category of “do skills” (behavior descriptions, reflections, and praises) and “don’t skills” (questions, commands, and negative talk) reflecting behaviors parents are taught during treatment to use and not to use during a child-led play.
At the Time 1 and Time 2 assessments, the do and don’t skills were assessed during a 5-min child-led play in which the mother was instructed to follow her child’s lead in play. Child compliance was measured during a 5-min cleanup situation in which the mother was instructed to have her child clean up all the toys without helping. The mother was not prompted to use skills learned in treatment to objectively measure mother skill acquisition and child compliance during the assessments. Undergraduate student coders were trained to 80% agreement with a criterion tape and were uninformed of group status. Half of the observations (28) were coded a second time for reliability. Percent agreement ranged from 68% (negative talk and noncomply) to 91% (praise), and kappas ranged from 0.50 (noncomply) to 0.78 (praise).
The Parenting Stress Index-Short Form25 is a 36-item parent self-report instrument containing 3 scales (Parental Distress, Parent-Child Dysfunctional Interaction, and Difficult Child) with high 6-month test-retest reliability coefficients. The Parenting Stress Index-Short Form scales were used to assess the effects of PCIT on parenting stress, and the internal consistency estimates in this study ranged from 0.75 to 0.89.
The Parenting Scale is a 30-item self-report measure with strong validity that assesses parental discipline practices.26 The effectiveness of discipline techniques is measured based on 3 scales: laxness, overreactivity, and verbosity. The Parenting Scale was used to assess the effects of PCIT on parenting practices, and the internal consistency estimates in this study ranged from 0.53 to 0.84.
Sample Size
Power calculations were based on changes in CBCL externalizing problem T scores in a previous study of PCIT for children with comorbid mental retardation and disruptive behavior.15 Although the effect size in this study was large (d = 1.05), it was relatively low in comparison with subsequent efficacy trials of PCIT (d = 1.40–1.60)27,28 and, therefore, was a conservative estimate of power. Testing the hypothesis that the IT group will have a better outcome (i.e., lower scores) than the WL group at posttreatment, and using power = 0.80 and a 2-sided comparison with alpha = .05, a minimum sample of 9 per group was sufficient to detect expected differences.
Statistical Analyses
The IT and WL groups were compared on each dependent variable to evaluate posttreatment effects at the Time 2 assessment. Outcomes were analyzed using analysis of covariance with baseline scores as the covariate, which is a more statistically powerful analytic method than repeated-measures analysis of variance for randomized, controlled trials.29 Effect sizes were calculated using Cohen’s d, which was calculated by dividing the difference in magnitude between the IT and WL groups at Time 2 by the standard deviation of the WL group Time 2 scores. To determine clinical significance, we calculated the Reliable Change Index for each child by dividing the magnitude of change on the CBCL externalizing problems scale between Time 1 and Time 2 and between Time 1 and Time 3 (follow-up) by the standard error of the difference score.
RESULTS
Children were mostly boys (71%), with a mean age of 38.1 months (SD = 13.4). Racial composition was 82% white, 10% biracial, 4% African-American, and 4% Asian, and 21% of children were Hispanic. Families had a mean socioeconomic status score of 43.4 (SD = 13.2), which falls in the middle range of socioeconomic status. There were no significant differences between immediate treatment (IT) and waitlist control (WL) groups on any demographic variables (Table 1) and baseline measures. All 14 families randomized to the WL group completed the Time 2 assessment, conducted 4 months after baseline. Of the 14 IT families receiving parent-child interaction therapy (PCIT), 11 completed treatment (average of 13 sessions) and the Time 2 assessment, which was also scheduled 4 months after the Time 1 assessment. Three families (21%) withdrew from treatment and did not complete the Time 2 assessment but were included in the intent-to-treat analysis. Among the families that completed treatment, all mothers but one met mastery criteria of the child-directed interaction and parent-directed interaction skills and completed treatment before the Time 2 assessment. One mother mastered criteria and completed treatment 1 month after the Time 2 assessment. A follow-up assessment was completed 4 months after the Time 2 assessment. This follow-up assessment (Time 3) was completed by 10 of the 11 IT families that had completed treatment and the Time 2 assessment. Of the 14 WL families receiving PCIT after the Time 2 assessment, 10 completed treatment and the Time 3 assessment (Fig. 1).
Table 1.
Demographic Characteristics of Groups
| Mean (SD), Median (Range), or Percent |
||||||
|---|---|---|---|---|---|---|
| Characteristic | IT (n = 14) | WL (n = 14) | t(26) | U | χ2(1) | p |
| Child age (mo) | 39.7 (14.2) | 36.5 (13.0) | −0.6 | — | — | .537 |
| Birthweight (g) | 1157.0 (651.5) | 1246.1 (563.2) | 0.4 | — | — | .702 |
| Gestational age (wk) | 28 (23–35) | 28.5 (25–34) | 1.0 | — | — | .335 |
| Apgar 1 mina | 3 (1–8) | 5 (1–10) | — | 35.5 | — | .103 |
| Apgar 5 mina | 6 (1–10) | 7 (4–9) | — | 40.0 | — | .181 |
| Perinatal morbidity (%)b | 85.7 | 92.9 | — | — | 0.4 | .541 |
| Child sex (% male) | 71.4 | 71.4 | — | — | 0.0 | 1.00 |
| Child ethnicity (% minority) | 35.7 | 21.4 | — | — | 0.7 | .403 |
| Hollingshead | 40.0 (12.9) | 46.8 (13.2) | 1.4 | — | — | .184 |
IT, immediate treatment; WL, waitlist control.
APGAR scores were only available from 22 of the 28 children, and the Mann-Whitney U test was used to compare groups for this ordinal measure.
Perinatal morbidity, dummy coded as a dichotomous variable (1 = yes, 2 = no), was based on maternal report of respiratory distress, intraventricular bleeding, and other neonatal complications. All but 1 child (IT group) were admitted to the neonatal intensive care unit.
Child Outcome
At the Time 2 assessment, children in the IT group had significantly less attention problems and aggressive behaviors, as well as less externalizing and internalizing problems on the Child Behavior Checklist (CBCL) than children in the WL group (Table 2). On the Eyberg Child Behavior Inventory (ECBI), children in the IT group had significantly fewer disruptive and problematic behaviors than children in the WL group (Table 2). In addition, children’s compliance to maternal commands during cleanup was significantly higher at the Time 2 assessment in the IT than WL group (Table 2).
Table 2.
Mean Scores for Measures of Child and Parent Outcome
| Scale | Group | n | Time 1 Mean (SD) |
Time 2 Mean (SD) |
p | da |
|---|---|---|---|---|---|---|
| Child outcome | ||||||
| Child Behavior Checklist | ||||||
| Attention problems | IT | 11 | 64.7 (7.4) | 54.3 (5.6) | .011 | 1.1 |
| WL | 14 | 68.1 (8.2) | 62.6 (7.4) | |||
| Aggressive behavior | IT | 11 | 70.1 (10.9) | 51.1 (1.6) | .000 | 1.6 |
| WL | 14 | 75.8 (11.1) | 67.7 (10.2) | |||
| Externalizing problems | IT | 11 | 69.4 (9.1) | 47.9 (6.1) | .000 | 2.3 |
| WL | 14 | 74.2 (8.9) | 66.9 (8.4) | |||
| Internalizing problems | IT | 11 | 57.1 (10.5) | 44.8 (7.1) | .000 | 1.4 |
| WL | 14 | 58.5 (9.3) | 56.5 (8.4) | |||
| Eyberg Child Behavior Inventory | ||||||
| Intensity | IT | 11 | 63.4 (12.2) | 43.0 (4.3) | .000 | 2.3 |
| WL | 14 | 64.1 (8.1) | 64.6 (9.5) | |||
| Problem | IT | 11 | 61.8 (9.3) | 45.6 (5.5) | .000 | 1.4 |
| WL | 14 | 65.1 (7.9) | 61.1 (10.8) | |||
| Dyadic Parent-Child Coding System—Third Edition | ||||||
| % Child complianceb | IT | 11 | 54.7 (25.4) | 76.6 (20.0) | .039 | 0.9 |
| WL | 14 | 47.2 (25.9) | 55.9 (22.6) | |||
| Parent outcome | ||||||
| CDI do skillsc | IT | 11 | 5.4 (5.2) | 16.8 (11.8) | .003 | 1.3 |
| WL | 14 | 7.8 (4.0) | 7.5 (7.5) | |||
| CDI don’t skillsc | IT | 11 | 36.9 (14.7) | 11.6 (7.4) | .000 | 1.3 |
| WL | 14 | 34.7 (14.7) | 36.0 (18.4) | |||
| Parenting Stress Index-Short Form | ||||||
| Parental distress | IT | 11 | 26.8 (9.7) | 23.0 (9.0) | .078 | 0.8 |
| WL | 14 | 30.1 (9.7) | 30.1 (8.9) | |||
| Parent-child DI | IT | 11 | 23.9 (8.5) | 19.2 (5.4) | .186 | 0.4 |
| WL | 14 | 22.1 (5.8) | 21.1 (4.8) | |||
| Difficult Child | IT | 11 | 36.8 (6.1) | 24.3 (8.1) | .004 | 1.3 |
| WL | 14 | 40.6 (7.4) | 36.6 (9.4) | |||
| Parenting Scale | ||||||
| Laxness | IT | 11 | 31.6 (10.1) | 23.0 (9.5) | .004 | 1.1 |
| WL | 14 | 33.7 (10.8) | 32.0 (8.4) | |||
| Overreactivity | IT | 11 | 27.6 (6.2) | 21.6 (6.3) | .029 | 0.8 |
| WL | 14 | 29.9 (7.4) | 29.0 (9.1) | |||
| Verbosity | IT | 11 | 24.2 (3.1) | 20.3 (7.5) | .041 | 0.8 |
| WL | 14 | 24.6 (6.2) | 25.8 (7.0) |
IT, immediate treatment; WL, waitlist control; CDI, child-directed interaction; DI, dysfunction interaction; SES, socioeconomic status. Time 1 scores did not differ between groups (p > .19); analysis and covariance including child age, child minority status, and SES as covariates did not differ from the above analyses.
Cohen’s d = effect size between IT and WL group at the Time 2 assessment.
Child compliance was coded during the cleanup situation.
CDI skills were coded during the child-led play.
Parent Outcome
During the child-led play, mothers in the IT group used significantly more do skills and fewer don’t skills at the Time 2 assessment than mothers in the WL group (Table 2). Mothers in the IT group reported significantly less stress about their child’s behavior on the Parenting Stress Index-Short Form and reported less laxness, overreactivity, and verbosity in their parenting style on the Parenting Scale than mothers in the WL group (Table 2).
Intent to Treat
In addition to the comparisons with the treatment completers, we conducted an intent-to-treat analysis including the 3 families that dropped out of treatment. The ECBI intensity scale was completed weekly by mothers in treatment to assess treatment progress, so the last weekly score before dropping out was used as the best estimate of child disruptive behavior outcome at Time 2. All 14 children randomized to treatment had fewer disruptive behaviors on the ECBI than children in the WL group at the Time 2 assessment, F(1,25) = 24.2, p = .000, d = 1.8.
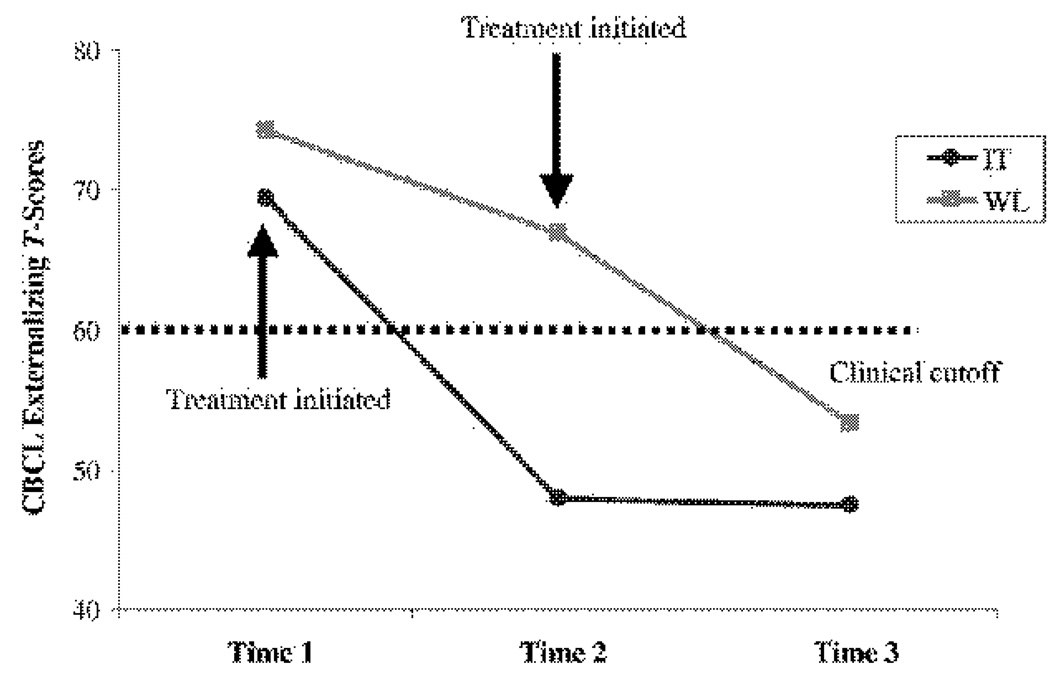
Clinical Significance and Follow-Up
To determine whether the changes in children’s behavior were clinically significant, we used established criteria.30 First, we considered Reliable Change Index scores >1.96 sufficient in magnitude (described in Statistical Analyses section). Second, we required the child’s CBCL externalizing T score to be <60 at Time 2. Using these stringent criteria, all 11 children in the IT group (100%) compared with 4 children in the WL group (29%) made clinically significant changes from Time 1 to Time 2. Using the same criteria for the 10 IT families that completed the Time 3 assessment 8 months after baseline, 8 children (80%) maintained clinical significant changes. Of the 10 WL families that completed treatment (i.e., between Time 2 and Time 3), 9 (90%) made clinically significant changes from Time 1 to Time 3. The mean changes in CBCL externalizing T scores associated with immediate and delayed treatment illustrate these clinically significant changes and are depicted in Figure 2.
Figure 2.
Clinically significant mean changes.
DISCUSSION
This study is the first randomized, controlled trial examining the initial efficacy of a parenting intervention for the treatment of behavior problems in young children born premature. The results indicate that mothers of children receiving parent-child interaction therapy (PCIT) reported significant decreases in internalizing, externalizing, and disruptive behavior problems compared with children in a waitlist control (WL) group. The reported behavioral improvements from clinically significant to normative levels were maintained among the treated children 4 months after completing treatment. Children receiving PCIT were also observed to be significantly more compliant to maternal commands during a cleanup situation, comparable with behavioral changes of other PCIT studies.15,27,28 Therefore, findings were consistent when examining both maternal report of behavior problems and objectively coded behavioral data.
In addition to the statistical analysis of study findings, we examined clinical significance to provide information about individual child behavior change within groups. Although 29% of untreated children showed clinically significant improvements of behavior problems during the 4-month waiting period, 100% of treated children showed reliable behavior change after treatment. The clinically significant improvements were also maintained for 80% of the treated children 4 months after completing treatment, suggesting behavioral treatment effects last in the short term. In addition, 90% of the WL children demonstrated clinically significant behavior change after receiving treatment, indicating the WL and immediate treatment (IT) children displayed similar treatment responses.
Observations of mother-child interactions during the child-led play suggested mothers receiving PCIT interacted more positively with their children than untreated mothers. In addition, treated mothers reported significantly lower levels of ineffective parenting practices, including lack of discipline, harshness, and long windedness, as well as parenting stress related to the child’s challenging behavior. There were no significant differences on the parental distress scale and parenting stress related to dysfunctional parent-child interactions. However, most mothers in the IT and WL groups did not report clinically significant stress on either scale at baseline (64% and 72%, respectively), suggesting change on these scales may not be clinically important.
One limitation of this study is the small sample size. Although the effect sizes in PCIT are very large and do not necessitate large samples to find significant effects, the small sample may have reduced power to detect some effects, such as parental distress and parenting stress related to dysfunctional parent-child interactions. In addition, the small sample reduces the generalizability of our findings. For example, there was large variability in birth weight (range, 420–3000 g), gestational age (range, 23–35 wks etiology), and neonatal course, and the of behavior problems can differ as a function of these demographic variables. The small sample size of this study limits conclusions that we can make about the impact of these variables on treatment, and future research should examine these variables as potential moderators of treatment outcome using larger samples.
Children with severe medical and neurodevelopmental disorders and mothers with cognitive impairment were excluded from this study further limiting generalizability. In addition, the number of children from racial and ethnic minority backgrounds was relatively small (29%), all mothers spoke and understood English, and the majority of families participating in the study were in the middle-class range. Examination of the effectiveness of PCIT for families from more culturally and socioeconomically diverse samples is warranted.
A second limitation is differential attrition. Although not statistically significant, attrition at the Time 2 assessment was higher for families in the IT group (21%) than the WL group (0%). We conducted an intent-to-treat analysis to determine whether findings would be similar when including all families assigned to the treatment group. Results suggested that significant between-group differences were likely not due to differential attrition. In addition, the treatment dropout rate for this study was considerably lower than other child psychosocial treatments (40–60%)31 and may be due to unique features of PCIT that encourage consistent participation (e.g., discussion of family stressors and weekly reminder calls). Nonetheless, attrition is a problem in parenting interventions, particularly with at-risk populations, and may be a function of the intensity of PCIT. Therefore, the prevention of externalizing behavior problems in shorter and more focused interventions is an important area of future research.
Finally, the use of a WL control group did not control for nonspecific therapy effects for families in the IT group (e.g., weekly contact with a supportive therapist), and maternal report of changes may have been subject to rater bias. However, findings from the behavioral observations conducted by coders unaware of the group status provide more objective data of behavior changes after treatment. Although treatment effects from PCIT have been shown to generalize to the school setting based on teacher report and school observations,32,33 data in the school setting were not collected for this particular study. PCIT was also not compared with other treatments of behavior problems (e.g., alternative parenting interventions and medication), and mothers were not masked to treatment status. It is important to first examine the efficacy of PCIT with a new population before conducting larger scale and more costly studies of treatment. The results of this study provide useful information on feasibility and power for future research examining interventions for children born premature. In addition, future research should examine the cost effectiveness of PCIT over other parenting interventions.
CONCLUSIONS
The findings of this randomized, controlled trial demonstrate the initial efficacy and feasibility of implementing a parenting intervention for young children with behavior problems who were born premature. Given the increased risk of behavior problems and importance of follow-up care with this population, parent-child interaction therapy (PCIT) is a helpful and safe treatment option that may have public health implications. Promoting the use of an authoritative parenting style was particularly relevant for mothers of children born premature who often have difficulty setting firm limits because of concerns about the physical well-being of their child. Future research should examine PCIT with children born premature in a larger, multisite trial to increase generalizability of the current findings.
ACKNOWLEDGMENTS
We thank Drs. James Jaccard and Wendy Silverman for their consultation and feedback on this manuscript.
Supported by the National Institute of Child Health and Human Development (F32 HD056748).
Footnotes
Portions of the data were previously presented at the 2008 Kansas Conference in Clinical Child and Adolescent Psychology in Lawrence, KS and at the 12th annual Research Symposium on Mental Health Sciences at the Warren Alpert Medical School of Brown University in Providence, RI.
REFERENCES
- 1.Berman RE, Butler AS. Preterm Birth: Causes, consequences, and Prevention. Washington, DC: National Academies; 2006. [PubMed] [Google Scholar]
- 2.Bhutta AT, Cleves MA, Casey PH, Cradock MM, Anand KJ. Cognitive and behavioral outcomes of school-aged children who were born preterm: a meta-analysis. JAMA. 2002;288:728–737. doi: 10.1001/jama.288.6.728. [DOI] [PubMed] [Google Scholar]
- 3.Aylward GP. Cognitive and neuropsychological outcomes: more than IQ scores. Ment Retard Dev Disabil Res Rev. 2002;8:234–240. doi: 10.1002/mrdd.10043. [DOI] [PubMed] [Google Scholar]
- 4.Hack M, Taylor HG, Schluchter M, Andreias L, Drotar D, Klein N. Behavioral outcomes of extremely low birth weight children at age 8 years. J Dev Behav Pediatr. 2009;30:122–130. doi: 10.1097/DBP.0b013e31819e6a16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singer LT, Danviller M, Bruening P, Hawkins S, Yamashita TS. Social support, psychological distress, and parenting strains in mothers of very low birthweight infants. Fam Relat. 1996;45:343–350. doi: 10.2307/585507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Halpern LF, Brand KL, Malone AF. Parenting stress in mothers of very-low-birth-weight (VLBW) and full-term infants: a function of infant behavioral characteristics and child-rearing attitudes. J Pediatr Psychol. 2001;26:93–104. doi: 10.1093/jpepsy/26.2.93. [DOI] [PubMed] [Google Scholar]
- 7.Eiser C, Eiser JR, Mayhew AG, Gibson AT. Parenting the premature infant: balancing vulnerability and quality of life. J Child Psychol Psychiatry. 2005;46:1169–1177. doi: 10.1111/j.1469-7610.2005.00415.x. [DOI] [PubMed] [Google Scholar]
- 8.Singer LT, Fulton S, Kirchner HL, et al. Parenting very low birth weight children at school age: maternal stress and coping. J Pediatr. 2007;151:463–469. doi: 10.1016/j.jpeds.2007.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McCarton CM, Wallace IF, Bennett FC. Early intervention for low-birth-weight premature infants: what can we achieve? Ann Med. 1996;28:221–225. doi: 10.3109/07853899609033123. [DOI] [PubMed] [Google Scholar]
- 10.Browne JV, Talmi A. Family-based intervention to enhance infant-parent relationships in the neonatal intensive care unit. J Pediatr Psychol. 2005;30:667–677. doi: 10.1093/jpepsy/jsi053. [DOI] [PubMed] [Google Scholar]
- 11.Kaaresen PI, Ronning JA, Tunby J, Nordhov SM, Ulvund SE, Dahl LB. A randomized controlled trial of an early intervention program in low birth weight children: outcome at 2 years. Early Hum Dev. 2008;84:201–209. doi: 10.1016/j.earlhumdev.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 12.Xu Y, Filler JW. Linking assessment and intervention for developmental/functional outcomes of premature, low-birth-weight children. Early Child Educ. 2005;32:383–389. [Google Scholar]
- 13.Eyberg SM, Nelson MM, Boggs SR. Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. J Clin Child Adolesc Psychol. 2008;37:1–23. doi: 10.1080/15374410701820117. [DOI] [PubMed] [Google Scholar]
- 14.Bagner DM, Fernandez MA, Eyberg SM. Parent-child interaction therapy and chronic illness: a case study. J Clin Psychol Med Set. 2004;11:1–6. [Google Scholar]
- 15.Bagner DM, Eyberg SM. Parent-child interaction therapy for disruptive behavior in children with mental retardation: a randomized controlled trial. J Clin Child Adolesc Psychol. 2007;36:418–429. doi: 10.1080/15374410701448448. [DOI] [PubMed] [Google Scholar]
- 16.Holingshead A. A Four Factor Index of Social Status. New Haven, CT: Yale University; 1975. [Google Scholar]
- 17.Robins DL, Fein D, Barton ML, Green JA. The Modified Checklist for Autism in Toddlers: an initial study investigating the early detection of autism and pervasive developmental disorders. J Autism Dev Disord. 2001;31:131–144. doi: 10.1023/a:1010738829569. [DOI] [PubMed] [Google Scholar]
- 18.Snow AV, Lecavalier L. Sensitivity and specificity of the Modified Checklist for Autism in Toddlers and the Social Communication Questionnaire in preschoolers suspected of having pervasive developmental disorders. Autism. 2008;12:627–644. doi: 10.1177/1362361308097116. [DOI] [PubMed] [Google Scholar]
- 19.Wechsler D. Wechsler Abbreviated Scale of Intelligence. San Antonio, TX: Pychological Corportation; 1999. [Google Scholar]
- 20.Hays JR, Reas DL, Shaw JB. Concurrent validity of the Wechsler abbreviated scale of intelligence and the Kaufman brief intelligence test among psychiatric inpatients. Psychol Rep. 2002;90:355–359. doi: 10.2466/pr0.2002.90.2.355. [DOI] [PubMed] [Google Scholar]
- 21.Achenbach TM, Rescorla LA. Manual for the ASEBA Preschool Forms and Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families; 2001. [Google Scholar]
- 22.Eyberg SM, Pincus D. Eyberg Child Behavior Inventory and Sutter-Eyberg Student Behavior Inventory: Professional Manual. Odessa, FL: Psychological Assessment Resources; 1999. [Google Scholar]
- 23.Funderburk BW, Eyberg SM, Rich BA, Behar L. Further psychometric evaluation of the Eyberg and Behar rating scales for parents and teachers of preschoolers. Early Educ Dev. 2003;14:67–81. [Google Scholar]
- 24.Eyberg SM, Nelson MM, Duke M, Boggs SR. Manual for the Dyadic Parent-Child Interaction Coding System. 3rd ed. 2004. [Google Scholar]
- 25.Abidin RR. Parenting Stress Index, Third Edition Professional Manual. Odessa, FL: Psychological Assessment Resources, Inc.; 1995. [Google Scholar]
- 26.Arnold DS, O’Leary SG, Wolff LS, Acker MM. The parenting scale: a measure of dysfunctional parenting in discipline situations. Psychol Assess. 1993;5:137–144. [Google Scholar]
- 27.Eisenstadt TH, Eyberg SM, McNeil CB, Newcomb K, Funderburk BW. Parent-child interaction therapy: interim report of a randomized trial with short-term maintenance. J Clin Child Psychol. 1993;22:42–51. doi: 10.1207/s15374424jccp2701_4. [DOI] [PubMed] [Google Scholar]
- 28.Schuhmann EM, Foote RC, Eyberg SM, Boggs SR, Algina J. Efficacy of parent-child interaction therapy: interim report of a randomized trial with short-term maintenance. J Clin Child Psychol. 1998;27:34–45. doi: 10.1207/s15374424jccp2701_4. [DOI] [PubMed] [Google Scholar]
- 29.Rausch JR, Maxwell SE, Kelley K. Analytic methods for questions pertaining to a randomized pretest, posttest, follow-up design. J Clin Child Adolesc Psychol. 2003;32:467–486. doi: 10.1207/S15374424JCCP3203_15. [DOI] [PubMed] [Google Scholar]
- 30.Jacobson NS, Roberts LJ, Berns SB, McGlinchey JB. Methods for defining and determining the clinical significance of treatment effects: description, application, and alternatives. J Consult Clin Psychol. 1999;67:300–307. doi: 10.1037//0022-006x.67.3.300. [DOI] [PubMed] [Google Scholar]
- 31.Wierzbicki M, Pekarik G. A meta-analysis of psychotherapy dropout. Prof Psychol Res Pract. 1993;24:190–195. [Google Scholar]
- 32.Bagner DM, Boggs SR, Eyberg SM. Evidence-based school behavior assessment of externalizing behavior in young children. Educ Treat Child. 2010;33:65–83. doi: 10.1353/etc.0.0084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McNeil C, Eyberg SM, Eisenstadt T, Newcomb K, Funderburk BW. Parent-child interaction therapy with behavior problem children: generalization of treatment effects to the school setting. J Clin Child Psychol. 1991;20:140–151. [Google Scholar]