Abstract
Background
Mindfulness-Based Cognitive Therapy (MBCT) is a group intervention that integrates elements of Cognitive Behavioural Therapy (CBT) with components of mindfulness training to prevent depressive relapse. The efficacy of MBCT compared to Treatment As Usual (TAU), shown in two randomized controlled trials indicates a significant decrease in 1-year relapse rates for patients with at least three past depressive episodes. The present study is the first independent replication trial comparing MBCT + TAU to TAU alone across both language and culture (Swiss health care system).
Methods
Sixty unmedicated patients in remission from recurrent depression (≥ 3 episodes) were randomly assigned to MBCT + TAU or TAU. Relapse rate and time to relapse were measured over a 60 week observation period. The frequency of mindfulness practices during the study was also evaluated.
Results
Over a 14-month prospective follow-up period, time to relapse was significantly longer with MBCT + TAU than TAU alone (median 204 and 69 days, respectively), although both groups relapsed at similar rates. Analyses of homework adherence revealed that following treatment termination, the frequency of brief and informal mindfulness practice remained unchanged over 14 months, whereas the use of longer formal meditation decreased over time.
Limitations
Relapse monitoring was 14 months in duration and prospective reporting of mindfulness practice would have yielded more precise frequency estimates compared to the retrospective methods we utilized.
Conclusions
Further studies are required to determine which patient characteristics, beyond the number of past depressive episodes, may predict differential benefits from this therapeutic approach.
Keywords: Depressive relapse prophylaxis, Mindfulness, MBCT, Remission, Mindfulness practice
1. Introduction
Relapse and recurrence following remission and recovery from a major depressive episode are common and debilitating outcomes that carry enormous social costs (Judd et al., 2000; Paykel et al., 2005). Since routine clinical management of depressed patients targets symptom reduction during the acute episode as its primary goal, little attention has been paid to strategies for maintaining treatment benefits over time. One approach that has recently shown promise involves sequencing antidepressant pharmacotherapy with a prophylactic intervention that teaches prevention skills to patients in pharmacologically-induced remission. Mindfulness-Based Cognitive Therapy (MBCT; Segal et al., 2002b) consists of 8 weekly sessions comprising a group intervention that integrates elements of Cognitive Behavioural Therapy (CBT; Beck et al., 1979) with components of the Mindfulness-Based Stress Reduction program (MBSR; Kabat-Zinn, 1990) to prevent depressive relapse.
The theoretical background of MBCT is based on the differential activation hypothesis developed by Teasdale (1988) who suggests that individuals who have experienced several depressive episodes are vulnerable to recurrences as even a mild dysphoric state may reactivate the depressive thinking patterns present during previous depressive episodes, thus precipitating a full-blown new episode. In this context, a treatment manual was developed (MBCT – Segal et al., 2002b) describing a preventive group protocol that teaches recovered depressed patients how to disengage from automatic, cognitive processing patterns linked to relapse. Teasdale et al. (1995) proposed that attentional control skills taught in mindfulness meditation could be helpful in preventing relapse by enabling formerly depressed individuals to observe their thoughts and feelings non-judgementally and to view them simply as passing mental events rather than as aspects of themselves or as accurate reflections of reality.
To date, two randomized controlled trials (Ma and Teasdale, 2004; Teasdale et al., 2000) explored the efficacy of MBCT compared to Treatment As Usual (TAU). More precisely, Teasdale et al. (2000) examined the effects of MBCT on rates of depressive relapse in a large multicenter sample of patients having remitted from major depressive episode and off antidepressant medication (N = 145). All participants had discontinued their medication at least 12 weeks before the study began. Patients were randomly assigned to either TAU or MBCT + TAU conditions and then followed for 1 year. For patients with three or more previous depressive episodes (77% of the study sample), results showed much lower relapse rates for MBCT + TAU patients (40% of patients relapsed) than for the TAU group (66% of patients relapsed) during the 1-year follow-up period. However, relapse rates did not differ between MBCT + TAU and TAU conditions for patients having experienced only one or two previous episodes. These results were later confirmed in a single site replication study (N = 75) of the efficacy of MBCT + TAU versus TAU (Ma and Teasdale, 2004) in preventing depressive relapse. A significant reduction in the relapse rate during the 1-year follow-up period was observed in MBCT + TAU patients compared to the TAU group (36% vs. 78%), again only for patients with three or more past episodes of depression.
More recently, it has also been shown, that in people with three or more past episodes of depression, MBCT produces comparable relapse/recurrence rates over 15-month follow-up (47%) to maintenance antidepressant medication (60%) (Kuyken et al., 2008). Additionally, preliminary results on MBCT for patients currently actively symptomatic are very encouraging (Eisendrath et al., 2008; Kenny and Williams, 2007; Kingston et al., 2007).
Still, there are a number of questions that remain to be answered. Chief among these is the fact that the prevention effects reported in studies comparing MBCT + TAU to TAU come from trials in which MBCT groups were conducted by the developers of this treatment approach. This makes it difficult to determine the MBCT's generalizability and to rule out allegiance effects (Luborsky and Luborsky, 2006). The major emphasis on efficacy in these early studies has also left questions such as the patient's experience while learning mindfulness practices largely unanswered (Mason and Hargreaves, 2001). For example, little is known about which mindfulness practices patients continue to use or abandon once the 8-session treatment has ended (Carmody and Baer, 2008).
In the present study, we tested the hypothesis that MBCT in addition to TAU would reduce the risk of depressive relapse when compared with TAU alone in the context of the Swiss health care system in a sample of remitted depressed patients with three or more past depressive episodes. Moreover, we investigated whether a regular degree of practice was associated with diminished relapse rates.
2. Methods
2.1. Inclusion/exclusion criteria
As the present study aims to be a replication trial of the two previous MBCT trials (Ma and Teasdale, 2004; Teasdale et al., 2000), inclusion/exclusion criteria and treatment framework were identical. The only difference between these studies and the present trial was the number of previous depressive episodes. Whereas a portion of the sample in the former studies (appx 20%) had 1–2 past episodes, we limited the inclusion to patients with 3 or more previous episodes. The rationale for this was based on previous findings (Ma and Teasdale, 2004; Teasdale et al., 2000) showing that MBCT reduces relapse rate specifically in people with 3 or more previous episodes.
Inclusion criteria were as follows: history of recurrent major depression according to DSM-IV (Diagnostic and Statistical Manual of Mental Disorders; American Psychiatric Association, 1994) assessed with the Structured Clinical Interview for DSM-IV (First et al., 1996); at least three past depressive episodes (2 episodes in the past 5 years and at least one in the past 2 years); remission for at least 3 months at time of enrolment. The Montgomery–Asberg Depression Rating Scale score (MADRS; Montgomery and Asberg, 1979) had to be ≤ 13, corresponding to the baseline score of 10 (Zimmerman et al., 2004) on the Hamilton Rating Scale for Depression 17-items (HRSD; Hamilton, 1960), which was the cut-off score used as inclusion criterion in the two previous MBCT trials (Ma and Teasdale, 2004; Teasdale et al., 2000). Participants were required to have a history of treatment with antidepressants but to currently be off medication for at least 3 months before enrolment. As it was not possible to determine the adequacy of treatment by antidepressant medication this criterion was used as an indicator that in the naturalistic course of service delivery patients had been judged as appropriate for pharmacotherapy by their treating physician.
Patients with the following conditions were excluded: history of schizophrenia or schizoaffective disorder; current substance abuse, eating disorder, or obsessive compulsive disorder; organic mental disorder, pervasive developmental disorder or borderline personality disorder; dysthymia with onset before age 20; more than four sessions of CBT ever; current psychotherapy or counselling more frequently than once per month; current practice of meditation more than once per week or yoga more than twice per week.
The study protocol and the informed consent form received approval from the ethics committee of the Geneva University Hospitals.
2.2. Sample size
Sample size was estimated on the basis of previously reported relapse rates of 35% with MBCT and 70% with TAU (Ma and Teasdale, 2004; Teasdale et al., 2000). In order to have 80% power to detect such a difference (chi-square test for proportions, two-sided, significance level at .05), fifty-six patients (28 per group) were required.
2.3. Study procedure
The study was conducted by a single research team at two different sites separated by 60 km (Geneva and Lausanne University Hospitals) to enable people living within a large geographic area to participate. Participants were recruited through media announcements and mailings to psychiatrists and general practitioners in the French speaking region of Switzerland. After a telephone screening, potential participants were scheduled for an in person selection interview. Participants who met inclusion criteria during the selection interview and who were not taking an antidepressant medication were entered into a 3-month run-in phase during which remission was to remain stable. Participants who met inclusion criteria during the selection interview but were still taking antidepressant medication started, in agreement with their medical doctor, to taper and then discontinue the antidepressant medication. Once they stopped the pharmacological treatment, they entered the 3-month run-in phase during which remission was to remain stable. Phone contact with the investigators was maintained on a monthly basis. After the run-in phase, an enrolment interview aimed at insuring that inclusion criteria were still met took place. Each participant provided written informed consent before being enrolled. Participants were randomly assigned to two groups: A) TAU, participants were told to seek help from their family doctor of other sources as they normally would, should they encounter symptomatic deterioration or other difficulties over the course of the study. The treatment that patients received was monitored at each follow-up interview and is described in the Results section; or B) MBCT plus TAU, with eight weekly 2-hour training sessions. The French translation of the MBCT manual was used in this study (Segal et al., 2006). At least four MBCT sessions were considered as the minimal dose of MBCT in accordance with previous MBCT trials (Ma and Teasdale, 2004; Teasdale et al., 2000). Four MBCT groups were instructed by three senior CBT psychologists and a senior CBT psychiatrist. All therapists had undergone at least one training program taught and supervised by one of the developers of MBCT (Z. Segal) and two instructors attended 9 day professional trainings in Mindfulness-Based Stress Reduction at the University of Massachusetts Medical School (UMASS). Prior to this trial, they had all led at least three supervised MBCT groups. All instructors had an ongoing personal mindfulness practice. All trial groups were audiotaped in order to enable an independent rating of adherence to the program. Twenty-one audiotaped MBCT sessions were evaluated using the MBCT adherence scale (MBCT-AS; Segal et al., 2002a), by two psychologists who were familiar with MBCT but independent from the research team. Ratings indicated that there was a high degree of adherence of the instructors to the MBCT protocol (mean ratings indicated that 93.33% of items were rated as meeting “definite evidence of adherence”, 4.29% showing “slight evidence” and 2.38% showing “no evidence” of adherence across sessions).
Randomization was performed by the last author (GBe) independently from the research team. A stratified block randomization procedure was implemented. Stratification variables were site (Geneva vs. Lausanne), number of previous depressive episodes (3 vs. > 3 episodes) and duration since remission from last episode (0–12 vs. 13–24 months). After checking for inclusion and exclusion criteria and informed consent had been obtained, intervention was assigned to patients through sealed envelopes. Patients were instructed not to inform the research team about group assignment to insure that blind outcome assessment could be performed. The observation period was 60 weeks for all patients (corresponding to 8-week MBCT treatment and 52-week follow-up). Four MBCT booster-sessions were provided at regular 3-month intervals during follow-up. Recruitment lasted from October 2005 to December 2005, followed by enrolment from January 2006 to March 2006. The MBCT groups were conducted between February 2006 and May 2006. Follow-up lasted from April 2006 to June 2007. All patients were assessed at 3-month intervals by the research team to monitor their mood, as well as any possible initiation of medication and/or possible contact with medical staff (contact with general practitioner or mental health practitioner) over this time period.
2.4. Measures
Our primary dependent measure, the occurrence of relapse or recurrence meeting DSM-IV criteria for major depressive episode, was assessed with the depression module of the Structured Clinical Interview for DSM-IV (First et al., 1996) by raters blind to group assignment (FJ, PhD psychologist, 2nd author and CG clinical research nurse, 8th author). An experienced clinical psychologist with formal training in the use of the SCID trained the two research staff. To ensure accuracy, all the assessments were audiotaped. A senior psychiatrist, blind to group assignment, then rated all actual, borderline or probable relapse/recurrences. When disagreement occurred between the interviewer and the senior psychiatrist's assessments, consensus was reached through discussion. Twenty-two probable relapses were identified by the research staff. Four interviews could not be audiotaped due to either dysfunction of the audiotape or participants' refusal. Eighteen were submitted to the senior psychiatrist who confirmed 15 of them (83%). Time to relapse was calculated in terms of number of days separating the enrolment date from the relapse date. Patients were interviewed at baseline, 2 months later (end of therapy sessions for participants allocated to MBCT + TAU) and at 3-month intervals during follow-up (months 5, 8, 11 and 14). Depression severity was assessed with the MADRS (Montgomery and Asberg, 1979). The severity of the subjects' depressive symptoms was also measured with a self-rating questionnaire, the Beck Depression Inventory II (BDI-II, Beck et al., 1996; Editions du Centre de Psychologie Appliquée, 1998).
Regarding the mindfulness practice, participants were given two CDs containing the standard practices proposed in the program (body scan, sitting meditation, mindful movements, and 3-minute breathing space) and recorded by the instructors of this trial. This audio material is available on http://www.ecsa.ucl.ac.be/mindfulness/. The frequency of mindfulness practices during the study was measured with an ad hoc questionnaire developed for the purpose of this study. Patients in the MBCT + TAU group were asked to perform a retrospective assessment of their degree of practice across three study periods – during the group sessions (period 1), over the next 6 months (period 2) and during the last 6 months of follow-up (period 3). Patients rated the frequency of their practice of the body scan (lying down meditation), sitting meditation, 3-minute breathing space (a short meditation exercise allowing to bring formal practice into daily life) and informal practice (performing an everyday activity mindfully) on a 4-point Likert scale (from 1 = never to 4 = almost every day). Scores 1–2 and 3–4 were considered as “low” and “regular” levels of practice, respectively.
2.5. Statistical analysis
Groups were compared with the Fisher's exact test for proportions and the Mann–Whitney U-test for continuous and ordinal variables. Cox proportional hazards models were used to investigate predictors of relapse. Differences over time regarding the amount of practice were investigated with the McNemar test. Significance level was set at .05.
3. Results
3.1. Patients flow
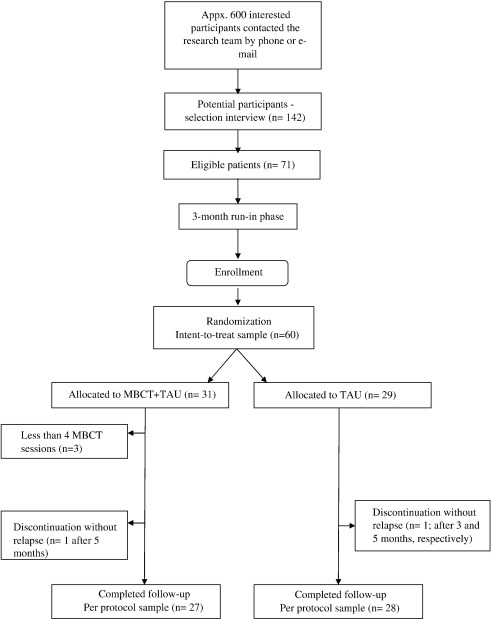
The patient flow chart is provided in Fig. 1.
Fig. 1.
Patient flow through each stage of the study.
More than 600 interested participants contacted the research team by phone or e-mail and a preliminary semi-structured phone screening was performed prior to an in person selection interview. The main reasons for exclusion from the phone screening interview were that participants presented with an ongoing acute depressive episode, they had less than three previous depressive episodes, they were older than 65 or younger than 18, they could not discontinue the antidepressant medication, they met diagnostic criteria for a bipolar mood disorder, they called only to report about their experience of recurrent depression and were not interested in being a research participant.
After this preliminary phone screening, one hundred forty two potential eligible patients completed an in person selection interview. Seventy-one were excluded because they didn't meet the inclusion criteria as follow: less than 3 past depressive episodes (n = 8), not having had 2 episodes in the past 5 years and at least one in the past 2 years (n = 10), MADRS score > 13 (n = 16), not having received an antidepressant for the last episode (n = 3), antidepressant medication couldn't be discontinued (n = 8), diagnosis of bipolar disorder (n = 10), presence of another psychiatric disorder such as alcohol abuse, borderline personality disorder, eating disorder, dysthymia (n = 15), refused to participate (n = 1).
Seventy-one eligible patients entered a 3-month run-in phase during which mood had to remain stable. Among them, 11 were excluded (7 no longer met the inclusion criteria as they had relapsed, 2 refused to participate and the staff team was unable to contact with 2 patients). The intent to treat sample (ITT) consisted of 60 patients who were randomized to either TAU (n = 29) or MBCT + TAU (n = 31) group. Regarding the MBCT + TAU group, the average number of MBCT sessions completed was 7.00 ± 1.09 and 90% (28/31) of the MBCT participants completed the 2-month program. Complete data on 14-month relapse or recurrence were available for 55 patients (per-protocol sample, PP).
3.2. Patient characteristics
Table 1 shows patient characteristics of the ITT sample. The TAU and MBCT + TAU groups did not differ statistically with respect to socio-demographic variables (age, gender, and education) or clinical history (age at onset of depression, number of past episodes, and number of hospitalizations). Baseline MADRS did not differ between the groups.
Table 1.
Characteristics of participants in the TAU and MBCT + TAU groups.
| Variable | MBCT + TAU (n = 31) | TAU (n = 29) | pa |
|---|---|---|---|
| Female (%) | 74 | 69 | .78 |
| Age, median (min–max) | 46 (27–63) | 49 (24–66) | .74 |
| Marital status (%) | .94 | ||
| Married/cohabiting | 48 | 44 | |
| Single | 20 | 17 | |
| Divorced/separated/widowed | 32 | 38 | |
| Years of education, median (min–max) | 15 (9–21) | 15 (10–28) | .53 |
| Social class (%)b | .52 | ||
| Class 1 | 10 | 7 | |
| Class 2 | 58 | 69 | |
| Class 3 | 32 | 21 | |
| Class 4 | 0 | 3 | |
| Class 5 | 0 | 0 | |
| Depression | |||
| MADRS score, median (min–max) | 4 (0–13) | 3 (0–13) | .77 |
| BDI-II score | 8.0 (0–32) | 8.0 (0–38) | .88 |
| Number of previous episodes, median (min–max) | 4 (3–14) | 4 (3–8) | .77 |
| Age of first onset, median (min–max) | 24 (14–54) | 25 (8–55) | .63 |
| Number of hospitalisations for depression, median (min–max) | 0 (0–3) | 0 (0–3) | .54 |
| Antidepressant medication at time of selection (%) with discontinuation in order to enter the run-in phase | 29 | 31 | .87 |
Fisher's exact test for proportions and Mann–Whitney U-test for continuous and ordinal variables.
Social class data are from the Office of Population Censuses and Surveys (1991) (Class 1, e.g., general manager; Class 5, e.g., road sweepers).
There was also no difference between groups regarding the use of antidepressant and non-pharmacological treatment during the study. Antidepressant medication was reinstated in 36% of the MBCT + TAU participants and in 31% of the TAU participants (Fisher's exact test, p = .78). Delay until onset of antidepressant medication was similar in both groups (median in days (min–max); MBCT + TAU: 204 (19–437); TAU: 111 (30–385); Mann–Whitney U-test, p = .40). One or more visit for counselling, psychotherapy or support from professional mental health staff was undertaken for 46% of the MBCT + TAU group and for 55% of the TAU group (Fisher's exact test, p = .60). One or more visit to general practitioner were undertaken for 29% of the MBCT + TAU group and for 24% of the TAU group (Fisher's exact test, p = .77).
In the ITT sample, 29% (9/31) of MBCT + TAU participants and 34% (10/29) of TAU participants relapsed over the 14-month study period (Fisher's exact test, p = .78). In the PP sample, corresponding figures were 33% (9/27) and 36% (10/28) (Fisher's exact test, p = 1). Among patients who relapsed (n = 19), relapse occurred significantly earlier in the TAU than in the MBCT + TAU group (median [range] time to relapse 69 days [15–191] with TAU and 204 [35–330] with MBCT + TAU, Mann–Whitney U-test, p = .006).
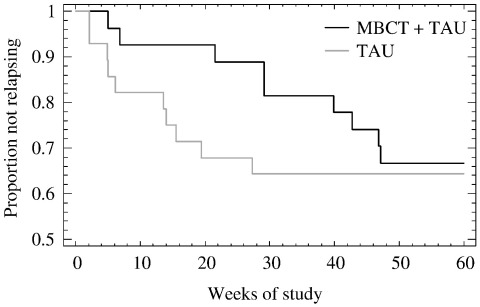
Cox regression models indicated that hazard of relapse did not significantly differ between MBCT + TAU and TAU participants, neither in the ITT sample nor in the PP sample (p = .58 and .60, respectively). Survival curves in Fig. 2 illustrate the cumulative proportion of patients not relapsing with MBCT + TAU and TAU in the PP sample.
Fig. 2.
Survival (non-relapse/non-recurrence) curves comparing relapse/recurrence to major depression (Diagnostic and Statistical Manual of Mental Disorders 4th ed.; APA, 1994) for MBCT + TAU and TAU groups (per-protocol sample, n = 55).
Treatment group remained non-significant after adjusting for age, gender, baseline MADRS, baseline BDI-II, time since remission and number of past depressive episodes, both in the ITT and PP samples. No significant interaction between these variables and treatment condition was detected.
3.3. Mindfulness practice over time
In the MBCT + TAU group (n = 26, data missing for 2 participants), the proportion of patients with a regular practice (at least once per week) is presented in Table 2 for each type of practice (body scan, sitting meditation, 3-minute breathing space, informal practice) across 3 periods of time (during group sessions, first 6 months and last 6 months of follow-up).
Table 2.
Formal and informal practice during and after MBCT sessions (n = 26).
| Proportion of MBCT participants who reported at least practicing once per week |
|||||
|---|---|---|---|---|---|
| Period 1 |
Period 2 |
Period 3 |
pa |
||
| During the 8-week MBCT treatment | 1–6 months follow-up | 7–12 months follow-up | Comparing Periods 1 and 2 | Comparing Periods 2 and 3 | |
| Body scan | 65.4% | 38.5% | 11.5% | .039 | .016 |
| Sitting meditation | 88.0% | 61.5% | 46.2% | .031 | .22 |
| 3-minute breathing space | 91.7% | 68.0% | 60.0% | .063 | .50 |
| Informal practice | 76.0% | 65.4% | 61.5% | .25 | 1.0 |
McNemar test.
While frequency of the body scan practice decreased from periods 1 to 2 and 2 to 3, and reduction of sitting meditation was observed between periods 1 and 2, patients kept practicing both the 3-minute breathing space and informal mindfulness with little change over 14 months.
The amount of practice did not significantly differ between relapsers (n = 9) and non-relapsers (n = 17) at any time for sitting meditation, 3-minute breathing space and informal practice (Fisher's exact test, N.S.). For body scan practice, no significant difference was observed during period 1 (p = 1) and period 2 (p = .69), while patients who relapsed practiced significantly more during period 3 (p = .032).
4. Discussion
To our knowledge, the present study is the first replication trial comparing MBCT + TAU to TAU performed without direct involvement of the MBCT developers, considered as a frequent bias in psychotherapy research (Chambless and Hollon, 1998). In remitted patients with three or more previous depressive episodes who relapsed, time to relapse was significantly delayed in the MBCT + TAU group (median 29 weeks) compared with TAU (10 weeks), in line with findings showing that MBCT increases the average time to relapse by at least 18 weeks (Williams et al., 2008). As in the two original MBCT trials, lack of an active control treatment does not allow us to attribute MBCT's effect on delaying time to relapse as due to specific training in mindfulness and CBT. Generic components of group-based therapy, such as support, destigmatization and therapeutic attention may well also play a role. In contrast to previous studies, however, 14-month relapse rates did not significantly differ between MBCT + TAU and TAU.
Whereas the 33% relapse rate following MBCT in our study is in line with those found in the two previous studies (40% and 36%), the 36% relapse rate in the TAU group was much lower than in earlier publications (66% and 78% – Ma and Teasdale, 2004; Teasdale et al., 2000). The high survival rate in the TAU condition, compared to the two former studies, is important to consider. First, no group differences appeared, neither on baseline clinical history or demographic variables, nor on the degree of adjunctive treatment, either psychological or pharmacological, accessed over the follow-up. The baseline clinical history and demographic variables were also similar to those of the past studies. A possible important difference, however, concerns the health care system in which these several studies were conducted. Indeed, the present trial was conducted within the Swiss mental health system. In Switzerland, there is high availability of mental health care and relatively easy access. The number of psychiatrists per 100,000 habitants is of 23, compared to 11 in the United Kingdom or 12 in Canada (World Health Organization, 2005). Moreover, in the United Kingdom and Canada, psychiatric patients have easy access to primary care general practitioners (‘gatekeeper system’) who work in collaboration with psychiatrists, whereas in Switzerland patients have direct access to psychiatrists as the first point of contact for mental health issues (World Health Organization, 2005). This high availability and accessibility may impact on the global management of recurrent depression. Studies comparing 1-year relapse rates after acute treatment of depression with CBT versus pharmacotherapy suggest relapse rates after discontinuing pharmacotherapy in the 60 to 80% range, thus much higher than the 35% rate found in our study (Simons et al., 1986; Dobson et al., 2008). It is interesting to note that in a recent study performed by our group, about a third of remitted depressed patients (37.5%) experienced a relapse during a 12-month follow-up period (Aubry et al., 2007). This relapse rate is similar to that evidenced in the present study and, noteworthy, both trials were performed in the same geographic area and Swiss health care system.
In other health care contexts, studies that have focused specifically on relapse prevention following psychological intervention, suggest that TAU relapse is higher than 35%. Howell et al. (2008) reported a 1-year relapse rate of 54% in a TAU group in their study of the prevention benefits from the “Keeping the Blues Away” program. Similarly, Bockting et al. (2005) found that 59% of patients in TAU relapsed over a 2-year period in their study of preventative CBT in Holland. However, it should be noted that it is rather difficult to compare relapse rates in patients with recurrent depression as the majority of relapse estimates are based on patients still receiving antidepressant treatment or placebo.
Regarding rates of mindfulness practice in the present study, MBCT patients who relapsed did not differ in their frequency of mindfulness practice compared to non-relapsers. The literature on this point is still unclear, as some studies have found associations between amount of practice and treatment outcome while others have not (Carmody and Baer, 2008). This could be due to the fact that most studies examine frequency of practice during the 8-session treatment period (Ramel et al., 2004; Speca et al., 2000) with only few reporting data beyond the program's end. When this latest period has been considered findings are equivocal. For example, Davidson et al. (2003) found that participants report a low rate of mindfulness practice (a mean of 1.7 on a Likert scale from 0 to 6) 4 months after MBSR classes. Reibel et al. (2001), on the other hand, reported that 1 year following a MBSR program 70% of participants practiced formal meditation more than three times per week and 91% practiced meditation informally. Our findings indicated that MBCT participants practiced regularly during the 8-session treatment, suggesting good initial adherence to the method. Formal practice decreased significantly between the end of the group and the 6-month follow-up for body scan and sitting meditation, whereas level of informal practice and the 3-minute breathing space decreased to a lesser extent, with more than 60% of participants still practicing regularly after 12 months.
Limitations of the present study should be acknowledged. Firstly, relapse was monitored over 14 months only, whereas a longer follow-up period, also taking into account more delayed relapses and recurrences, might have allowed better distinction between both study conditions. Another limitation is the retrospective estimation of mindfulness practice frequency over the 3 periods of time. While such an approach provides a global measure for each time period and helps avoiding missing data, day-to-day monitoring during would have yielded more precise information (e.g. minutes of practice per day). Moreover, it should be kept in mind that the secondary analyses were conducted on a relatively small sample (only on the MBCT + TAU group) and that this could limit statistical power.
In conclusion, MBCT significantly delayed time to relapse in recurrently depressed patients in remission. Considering the contrasting rates of relapse in the TAU condition found in this present study compared to earlier MBCT trials, further study is required to determine characteristics, beyond the number of past episodes that might predict differential benefit from this therapeutic approach. Recent publications (e.g. Eisendrath et al., 2008; Kuyken et al., 2008) and forthcoming studies of different research groups should progressively disentangle these questions.
Role of funding source
This study was supported by a grant of the Swiss National Science Foundation (Grant no. 3200BO-108432 to Guido Bondolfi, Gilles Bertschy, Jean-Michel Aubry and Martial Van der Linden).
Conflict of interest
There is no conflict of interest in this research.
Acknowledgments
This study was supported by a grant of the Swiss National Science Foundation (Grant no. 3200BO-108432 to Guido Bondolfi, Gilles Bertschy, Jean-Michel Aubry and Martial Van der Linden). Zindel Segal, PhD was consulted on the clinical competencies of the Swiss instructors and MBCT treatment fidelity. The authors thank Jean-Nicolas Despland from the Department of Psychiatry of the University Hospital in Lausanne for putting offices at the disposal of the research team. We also thank Sandra Ter Pelle for her expert technical support in the preparation of this manuscript.
References
- American Psychiatric Association . American Psychiatric Association; Washington, DC: 1994. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV. [Google Scholar]
- Aubry J.M., Gervasoni N., Osiek C., Perret G., Rossier M.F., Bertschy G., Bondolfi G. The DEX/CRH neuroendocrine test and the prediction of depressive relapse in remitted depressed outpatients. J. Psychiatr. Res. 2007;41:290–294. doi: 10.1016/j.jpsychires.2006.07.007. [DOI] [PubMed] [Google Scholar]
- Beck A.T., Rush A.J., Shaw B.F., Emery G. Guilford Press; New York: 1979. Cognitive Therapy of Depression. [Google Scholar]
- Beck A.T., Steer R.A., Brown G.K. The Psychological Corporation; San Antonio, TX: 1996. Beck Depression Inventory-II. [Google Scholar]
- Bockting C.L., Schene A.H., Spinhoven P., Koeter M.W., Wouters L.F., Huyser J., Kamphuis J.H. Preventing relapse/recurrence in recurrent depression with cognitive therapy: a randomized controlled trial. J. Consult. Clin. Psychol. 2005;73:647–657. doi: 10.1037/0022-006X.73.4.647. [DOI] [PubMed] [Google Scholar]
- Carmody J., Baer R.A. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. J. Behav. Med. 2008;31:23–33. doi: 10.1007/s10865-007-9130-7. [DOI] [PubMed] [Google Scholar]
- Chambless D.L., Hollon S.D. Defining empirically supported therapies. J. Consult. Clin. Psychol. 1998;66:7–18. doi: 10.1037//0022-006x.66.1.7. [DOI] [PubMed] [Google Scholar]
- Davidson R.J., Kabat-Zinn J., Schumacher J., Rosenkranz M., Muller D., Santorelli S.F., Urbanowski F., Harrington A., Bonus K., Sheridan J.F. Alterations in brain and immune function produced by mindfulness meditation. Psychosom. Med. 2003;65:564–570. doi: 10.1097/01.psy.0000077505.67574.e3. [DOI] [PubMed] [Google Scholar]
- Dobson K.S., Hollon S.D., Dimidjian S., Schmaling K.B., Kohlenberg R.J., Gallop R.J., Rizvi S.L., Gollan J.K., Dunner D.L., Jacobson N.S. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the prevention of relapse and recurrence in major depression. J. Consult. Clin. Psychol. 2008;76:468–477. doi: 10.1037/0022-006X.76.3.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Editions du Centre de Psychologie Appliquée . Editions du Centre de Psychologie Appliquée; Paris: 1998. Inventaire de Dépression de Beck, BDI-II. [Google Scholar]
- Eisendrath S.J., Delucchi K., Bitner R., Fenimore P., Smit M., McLane M. Mindfulness-based cognitive therapy for treatment-resistant depression: a pilot study. Psychother. Psychosom. 2008;77:319–320. doi: 10.1159/000142525. [DOI] [PubMed] [Google Scholar]
- First M.B., Spitzer R.L., Gibbon M., Williams J.B.W. New York State Psychiatric Institute, Biometrics Research Department; New York: 1996. Structured Clinical Interview for DSM-IV Axis I Disorders – Patient Edition (SCID-I/P, Version 2.0. [Google Scholar]
- Hamilton M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howell C.A., Turnbull D.A., Beilby J.J., Marshall C.A., Briggs N., Newbury W.L. Preventing relapse of depression in primary care: a pilot study of the “Keeping the Blues Away” program. Med. J. Aust. 2008;188:S138–141. doi: 10.5694/j.1326-5377.2008.tb01878.x. [DOI] [PubMed] [Google Scholar]
- Judd L.L., Akiskal H.S., Zeller P.J., Paulus M., Leon A.C., Maser J.D., Endicott J., Coryell W., Kunovac J.L., Mueller T.I., Rice J.P., Keller M.B. Psychosocial disability during the long-term course of unipolar major depressive disorder. Arch. Gen. Psychiatry. 2000;57:375–380. doi: 10.1001/archpsyc.57.4.375. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Delta; New York: 1990. Full catastrophe living: using the wisdom of your body and mind to face stress, pain, and illness. [Google Scholar]
- Kenny M.A., Williams J.M. Treatment-resistant depressed patients show a good response to mindfulness-based cognitive therapy. Behav. Res. Ther. 2007;45:617–625. doi: 10.1016/j.brat.2006.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kingston T., Dooley B., Bates A., Lawlor E., Malone K. Mindfulness-based cognitive therapy for residual depressive symptoms. Psychol. Psychother. 2007;80:193–203. doi: 10.1348/147608306X116016. [DOI] [PubMed] [Google Scholar]
- Kuyken W., Byford S., Taylor R.S., Watkins E., Holden E., White K., Barrett B., Byng R., Evans A., Mullan E., Teasdale J.D. Mindfulness-based cognitive therapy to prevent relapse in recurrent depression. J. Consult. Clin. Psychol. 2008;76:966–978. doi: 10.1037/a0013786. [DOI] [PubMed] [Google Scholar]
- Luborsky L., Luborsky E. Jason Aronson; Lanham, MD: 2006. Research and Psychotherapy: The Vital Link. [Google Scholar]
- Ma S., Teasdale J.D. Mindfulness-based cognitive therapy for depression: replication and exploration of differential relapse prevention effects. J. Consult. Clin. Psychol. 2004;72:31–40. doi: 10.1037/0022-006X.72.1.31. [DOI] [PubMed] [Google Scholar]
- Mason O., Hargreaves I. A qualitative study of mindfulness-based cognitive therapy for depression. Br. J. Med. Psychol. 2001;74(Part 2):197–212. [PubMed] [Google Scholar]
- Montgomery S.A., Asberg M. A new depression scale designed to be sensitive to change. Br. J. Psychiatry. 1979;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- Office of Population Censuses and Surveys . Her Majesty's Stationery Office; London: 1991. Standard Occupational Classification (Vol. 3) [Google Scholar]
- Paykel E.S., Brugha T., Fryers T. Size and burden of depressive disorders in Europe. Eur. Neuropsychopharmacol. 2005;15:411–423. doi: 10.1016/j.euroneuro.2005.04.008. [DOI] [PubMed] [Google Scholar]
- Ramel W., Goldin P.R., Carmona P.E., McQuaid J.R. The effects of mindfulness meditation on cognitive processes and affect in patients with past depression. Cogn. Ther. Res. 2004;28:433–455. [Google Scholar]
- Reibel D.K., Greeson J.M., Brainard G.C., Rosenzweig S. Mindfulness-based stress reduction and health-related quality of life in a heterogeneous patient population. Gen. Hosp. Psych. 2001;23:183–192. doi: 10.1016/s0163-8343(01)00149-9. [DOI] [PubMed] [Google Scholar]
- Segal Z.V., Teasdale J.D., Williams J.M., Gemar M.C. The mindfulness-based cognitive therapy adherence scale: inter-rater reliability, adherence to protocol and treatment distinctiveness. Clin. Psychol. Psychother. 2002;9:131–138. [Google Scholar]
- Segal Z.V., Williams J.M.G., Teasdale J.D. Guilford Press; New York: 2002. Mindfulness-based cognitive therapy for depression: a new approach to preventing relapse. [Google Scholar]
- Segal Z.V., Williams J.M.G., Teasdale J.D. Bruxelles; De Boeck: 2006. La thérapie cognitive basée sur la pleine conscience pour la dépression: Une nouvelle approche pour prévenir la rechute. [Google Scholar]
- Simons A.D., Murphy G.E., Levine J.L., Wetzel R.D. Cognitive therapy and pharmacotherapy for depression: sustained improvement over one year. Arch. Gen. Psychiatry. 1986;43:43–48. doi: 10.1001/archpsyc.1986.01800010045006. [DOI] [PubMed] [Google Scholar]
- Speca M., Carlson L.E., Goodey E., Angen M. A randomized, wait-list controlled clinical trial: the effect of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients. Psychosom. Med. 2000;62:613–622. doi: 10.1097/00006842-200009000-00004. [DOI] [PubMed] [Google Scholar]
- Teasdale J.D. Cognitive vulnerability to persistent depression. Cogn. Emot. 1988;2:247–274. [Google Scholar]
- Teasdale J.D., Segal Z., Williams J.M. How does cognitive therapy prevent depressive relapse and why should attentional control (mindfulness) training help? Behav. Res. Ther. 1995;33:25–39. doi: 10.1016/0005-7967(94)e0011-7. [DOI] [PubMed] [Google Scholar]
- Teasdale J.D., Segal Z.V., Williams J.M.G., Ridgeway V.A., Soulsby J.M., Lau M.A. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J. Consult. Clin. Psychol. 2000;68:615–623. doi: 10.1037//0022-006x.68.4.615. [DOI] [PubMed] [Google Scholar]
- Williams J.M., Russell I., Russell D. Mindfulness-based cognitive therapy: further issues in current evidence and future research. J. Consult. Clin. Psychol. 2008;76:524–529. doi: 10.1037/0022-006X.76.3.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . World Health Organization; Geneva: 2005. Mental Health Atlas – 2005. [Google Scholar]
- Zimmerman M., Posternak M.A., Chelminski I. Derivation of a definition of remission on the Montgomery–Asberg depression rating scale corresponding to the definition of remission on the Hamilton rating scale for depression. J. Psychiatr. Res. 2004;38:577–582. doi: 10.1016/j.jpsychires.2004.03.007. [DOI] [PubMed] [Google Scholar]